A Comprehensive Guide to Input-Output Transformation Validation Methods for Robust Drug Development
This article provides a complete framework for validating input-output transformations, tailored for researchers and professionals in drug development.
A Comprehensive Guide to Input-Output Transformation Validation Methods for Robust Drug Development
Abstract
This article provides a complete framework for validating input-output transformations, tailored for researchers and professionals in drug development. It covers foundational principles, practical methodologies for application, strategies for troubleshooting and optimization, and rigorous validation and comparative techniques. The content is designed to help scientific teams ensure the accuracy, reliability, and regulatory compliance of their data pipelines and AI models, which are critical for accelerating discovery and securing regulatory approval.
Laying the Groundwork: Core Principles and Regulatory Imperatives for Data Validation
Defining Input-Output Validation in the Drug Development Context
Input-output validation is a critical process in drug development that ensures computational and experimental systems reliably transform input data into accurate, meaningful outputs. This process provides the foundational confidence in the data and models that drive decision-making, from early discovery to clinical application. It confirms that a system, whether a biochemical assay, a AI model, or a physiological simulation, performs as intended within its specific context of use [1] [2].
The pharmaceutical industry faces a pressing need for robust validation frameworks. Despite technological advancements, drug development remains hampered by high attrition rates, often linked to irreproducible data and a lack of standardized validation practices. It is reported that 80-90% of published biomedical literature may be unreproducible, contributing to program delays and failures [2]. Input-output validation serves as a crucial countermeasure to this problem, establishing a framework for generating reliable, actionable evidence.
Theoretical Foundations and Regulatory Framework
Core Principles of Input-Output Validation
At its core, input-output validation is the experimental confirmation that an analytical or computational procedure consistently provides reliable information about the object of analysis [1]. This involves a comprehensive assessment of multiple performance characteristics, which together ensure the system's outputs are a faithful representation of the underlying biological or chemical reality.
The validation process is governed by a "learn and confirm" paradigm, where experimental findings are systematically integrated to generate testable hypotheses, which are then refined through further experimentation [3]. This iterative process ensures models and methods remain grounded in empirical evidence throughout the drug development pipeline.
Key Validation Parameters
Guidelines from the International Council for Harmonisation (ICH), USP, and other regulatory bodies specify essential validation parameters that must be evaluated for analytical procedures [1]. The specific parameters required depend on the type of test being validated, as summarized in Table 1.
Table 1: Validation Parameters for Different Types of Analytical Procedures
| Validation Parameter | Identification | Testing for Impurities | Assay (Quantification) |
|---|---|---|---|
| Accuracy | - | Yes | Yes |
| Precision | - | Yes | Yes |
| Specificity | Yes | Yes | Yes |
| Detection Limit | - | Yes | - |
| Quantitation Limit | - | Yes | - |
| Linearity | - | Yes | Yes |
| Range | - | Yes | Yes |
| Robustness | Yes | Yes | Yes |
Source: Adapted from ICH Q2(R1) guidelines, as referenced in [1]
Accuracy represents the closeness between the test result and the true value, indicating freedom from systematic error (bias). Precision describes the scatter of results around the average value and is assessed at three levels: repeatability (same conditions), intermediate precision (different days, analysts, equipment), and reproducibility (between laboratories) [1].
Specificity is the ability to assess the analyte unequivocally in the presence of other components, while Linearity and Range establish that the method produces results directly proportional to analyte concentration within a specified range. Robustness measures the method's capacity to remain unaffected by small, deliberate variations in procedural parameters [1].
Validation Approaches Across the Drug Development Pipeline
Traditional Analytical Method Validation
In pharmaceutical quality control, validation of analytical procedures is mandatory according to pharmacopoeial and Good Manufacturing Practice (GMP) requirements. All quantitative tests must be validated, including assays and impurity tests, while identification tests require validation specifically for specificity [1].
The validation process involves extensive experimental testing against recognized standards. For accuracy assessment, this typically involves analysis using Reference Standards (RS) or model mixtures with known quantities of the drug substance. The procedure is considered accurate if the conventionally true values fall within the confidence intervals of the results obtained by the method [1].
Revalidation is required when changes occur in the drug manufacturing process, composition, or the analytical procedure itself. This ensures the validated state is maintained throughout the product lifecycle [1].
AI and Computational Model Validation
The emergence of artificial intelligence (AI) and machine learning (ML) in drug discovery has introduced new dimensions to input-output validation. A systematic review of AI validation methods identified four primary approaches: trials, simulations, model-centred validation, and expert opinion [4].
For AI systems, validation must ensure the model reliably transforms input data into accurate predictions or decisions. This is particularly challenging given the "black box" nature of some complex algorithms. The taxonomy of AI validation methods includes failure monitors, safety channels, redundancy, voting, and input and output restrictions to continuously validate systems after deployment [4].
A notable example is the development of an autonomous AI agent for clinical decision-making in oncology. The system integrated GPT-4 with specialized precision oncology tools, including vision transformers for detecting microsatellite instability and KRAS/BRAF mutations from histopathology slides, MedSAM for radiological image segmentation, and access to knowledge bases including OncoKB and PubMed [5]. The validation process evaluated the system's ability to autonomously select and use appropriate tools (87.5% accuracy), reach correct clinical conclusions (91.0% of cases), and cite relevant oncology guidelines (75.5% accuracy) [5].
Table 2: Performance Metrics of Validated AI Systems in Drug Development
| AI System/Application | Validation Metric | Performance Result | Comparison Baseline |
|---|---|---|---|
| Oncology AI Agent [5] | Correct clinical conclusions | 91.0% | - |
| Oncology AI Agent [5] | Appropriate tool use | 87.5% | - |
| Oncology AI Agent [5] | Guideline citation accuracy | 75.5% | - |
| Oncology AI Agent [5] | Treatment plan completeness | 87.2% | GPT-4 alone: 30.3% |
| In-silico Trials [6] | Resource requirements | ~33% of conventional trial | - |
| In-silico Trials [6] | Development timeline | 1.75 years vs. 4 years | Conventional trial: 4 years |
The validation demonstrated that integrating language models with precision oncology tools substantially enhanced clinical accuracy compared to GPT-4 alone, which achieved only 30.3% completeness in treatment planning [5].
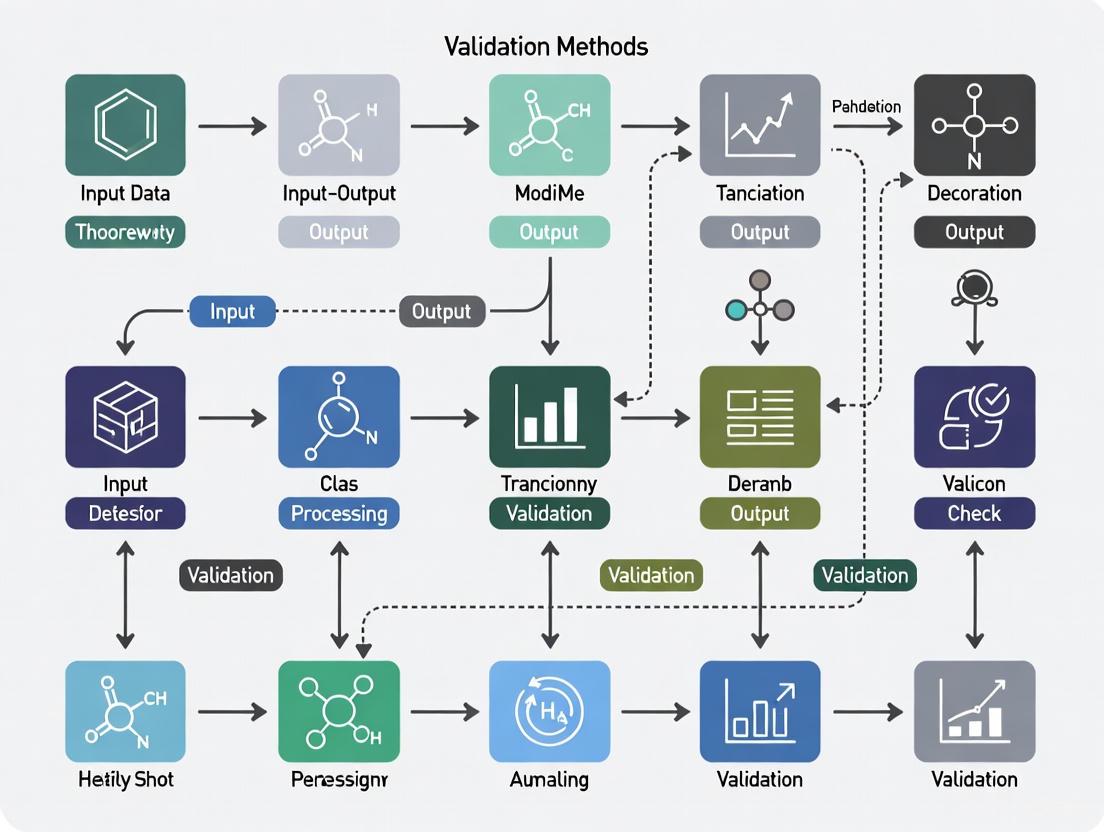
Figure 1: Input-Output Validation Framework for Clinical AI Systems in Oncology, demonstrating the transformation of multimodal medical data into validated clinical decisions through specialized tool integration [5].
In-silico Trial and Virtual Cohort Validation
In-silico trials using virtual cohorts represent another frontier where input-output validation is crucial. These computer simulations are used in the development and regulatory evaluation of medicinal products, devices, or interventions [6]. The European Union's SIMCor project developed a comprehensive framework for validating cardiovascular virtual cohorts, resulting in an open-source statistical web application for validation and analysis [6].
The SIMCor validation environment implements statistical techniques to compare virtual cohorts with real datasets, supporting both the validation of virtual cohorts and the application of validated cohorts in in-silico trials [6]. This approach demonstrates how input-output validation enables the acceptance of in-silico methods as reliable alternatives to traditional clinical trials, with reported potential to reduce development time from 4 years to 1.75 years while requiring approximately one-third of the resources [6].
Practical Implementation: Protocols and Methodologies
Protocol for Validating an Autonomous AI Clinical Agent
The development and validation of the autonomous AI agent for oncology decision-making followed a rigorous protocol [5]:
Step 1: System Architecture Integration
- Base LLM (GPT-4) integrated with specialized unimodal deep learning models
- Tool suite implementation: vision transformers for histopathology analysis, MedSAM for radiological image segmentation, knowledge search tools (OncoKB, PubMed, Google), and calculator functions
- Compilation of evidence repository with ~6,800 medical documents and clinical scores from six oncology-specific sources
Step 2: Benchmark Development
- Creation of 20 realistic, multimodal patient cases focusing on gastrointestinal oncology
- Each case included clinical vignettes with corresponding questions requiring tool use and evidence retrieval
- Simulation of complete patient journeys with multimodal data integration
Step 3: Validation Methodology
- Two-stage process: autonomous tool selection and application followed by document retrieval for evidence-based responses
- Blinded manual evaluation by four human experts across three domains: tool use effectiveness, quality and completeness of textual outputs, and precision of relevant citations
- Evaluation against 109 predefined statements for treatment plan completeness across the 20 cases
Step 4: Performance Benchmarking
- Comparison against GPT-4 alone and other state-of-the-art models (Llama-3 70B, Mixtral 8x7B)
- Quantitative assessment of tool invocation success rate (56 of 64 required tools correctly used)
- Evaluation of sequential tool chaining capability for multistep reasoning
Protocol for Quantitative Systems Pharmacology (QSP) Model Validation
Quantitative and Systems Pharmacology employs a distinct validation approach for its mathematical models [3]:
Step 1: Project Objective and Scope Definition
- Define clear context of use and model purpose
- Establish minimal physiological aspects necessary to achieve goals
- Identify crucial "states" to be tracked (e.g., plasma insulin, glucose in diabetes models)
Step 2: Biological Mechanism Formalization
- Develop diagrams visualizing relationships between different biological states
- Translate biological knowledge into mathematical representations (typically Ordinary Differential Equations)
- Integrate "top-down" clinical perspective with "bottom-up" physiological mechanisms
Step 3: Model Calibration and Verification
- Implement "learn and confirm" paradigm integrating experimental findings
- Calibrate parameters using available preclinical and clinical data
- Verify mathematical consistency and numerical stability
Step 4: Predictive Capability Assessment
- Execute "what-if" experiments to predict clinical trial outcomes
- Determine optimal minimum effective dosage based on preclinical data
- Evaluate combination therapies with different mechanisms of action
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Solutions for Input-Output Validation
| Reagent/Solution | Function in Validation | Application Context |
|---|---|---|
| Reference Standards (RS) [1] | Provide conventionally true values for accuracy assessment | Analytical method validation for drug quantification |
| Model Mixtures [1] | Simulate complex biological matrices for specificity testing | Impurity testing, method selectivity validation |
| Virtual Cohort Datasets [6] | Serve as reference for in-silico model validation | Cardiovascular device development, physiological simulations |
| Validated Histopathology Slides [5] | Ground truth for AI vision model validation | Oncology AI agent for MSI, KRAS, BRAF detection |
| Radiological Image Archives [5] | Reference standard for image segmentation algorithms | MedSAM tool validation in clinical AI systems |
| OncoKB Database [5] | Curated knowledge base for clinical decision validation | Precision oncology AI agent benchmarking |
| Clinical Data Repositories [2] | Provide real-world data for model benchmarking | FAIR data principles implementation, AI/ML training |
Data Standards and FAIR Principles
The critical importance of data standards in input-output validation cannot be overstated. The value of data generated from physiologically relevant cell-based assays and AI/ML approaches is limited without properly implemented data standards [2]. The FAIR Principles (Findable, Accessible, Interoperable, Reusable) provide a guiding framework for standardization efforts.
The biomedical community's lack of standardized experimental processes creates significant obstacles. For example, the development of microphysiological systems (MPS) as advanced in vitro models has been hampered by insufficient harmonized characterization and validation between different technologies, creating uncertainty about their added value [2].
Successful standardization requires attention to three main areas: (1) experimental standards to establish scientific relevance and clinical predictability; (2) information standards to ensure dataset comparability across institutions; and (3) dissemination standards to enable proper data communication and reuse [2].
Figure 2: Comprehensive Data Standardization Framework for Input-Output Validation, showing the three pillars of standardization guided by FAIR principles to ensure reliable and reproducible results in drug development [2].
Input-output validation represents a cornerstone of modern drug development, ensuring the reliability of data and models that drive critical decisions from discovery through clinical application. As the field increasingly adopts complex AI systems, in-silico trials, and sophisticated analytical methods, robust validation frameworks become increasingly essential.
The protocols and examples presented demonstrate that successful validation requires meticulous attention to defined performance parameters, appropriate statistical methodologies, and adherence to standardized practices. The integration of FAIR data principles throughout the validation process further enhances reproducibility and reliability.
As drug development continues to evolve toward more computational and AI-driven approaches, input-output validation will play an increasingly central role in ensuring these advanced methods generate trustworthy, actionable evidence. This will require ongoing refinement of validation methodologies, development of new standards, and cross-disciplinary collaboration among researchers, regulators, and technology developers.
In research and development, particularly in regulated industries like pharmaceuticals, the integrity of data and processes is paramount. Validation serves as the foundational layer ensuring that all inputs to a system and the resulting outputs are correct, consistent, and secure. It is defined as the confirmation by objective evidence that the previously established requirements for a specific intended use are met [7]. For researchers and drug development professionals, robust validation protocols are not merely a regulatory checkbox but a critical scientific discipline that underpins the trustworthiness of all experimental data and subsequent decisions [8]. A failure in validation can lead to catastrophic outcomes, including compromised product quality, erroneous research conclusions, and significant security vulnerabilities [9] [10].
This document frames validation within the broader context of input-output transformation methods, providing a detailed examination of its role as the first line of defense. We will explore essential data validation techniques, present experimental protocols for method validation, and outline the lifecycle approach for process validation, all tailored to the needs of scientific research.
Essential Data Validation Techniques
Data validation encompasses a suite of techniques designed to check data for correctness, meaningfulness, and security before it is processed [10]. Implementing these techniques at the point of entry prevents erroneous data from contaminating systems and ensures the integrity of downstream analysis.
The following table summarizes the core data validation techniques critical for research data integrity:
Table 1: Core Data Validation Techniques for Scientific Data Integrity
| Technique | Core Function | Common Research Applications |
|---|---|---|
| Type Validation [11] [10] | Verifies data matches the expected type (integer, float, string, date). | Ensuring instrument readings are numeric before statistical analysis; confirming date formats in patient data. |
| Range & Constraint Validation [11] [10] | Confirms data falls within a predefined minimum/maximum range or meets a logical constraint. | Checking pH values are between 0-14; verifying patient age in a clinical trial is plausible (e.g., 18-120). |
| Format & Pattern Validation [11] [10] | Ensures data adheres to a specific structural pattern, often using regular expressions. | Validating email addresses, sample IDs against a naming convention, or genomic sequences against an expected pattern. |
| Constraint & Business Logic Validation [11] | Enforces complex rules and relationships between different data points. | Ensuring a clinical trial's end date does not precede its start date; preventing duplicate patient enrollments (uniqueness check). |
| Code & Cross-Reference Validation [10] | Verifies data against a known list of allowed values or external reference data. | Ensuring a provided country code is valid; confirming a reagent lot number exists in an inventory database. |
| Consistency Validation [10] | Ensures data is logically consistent across related fields or systems. | Prohibiting a sample's analysis date from preceding its collection date. |
The Critical Role of Output Validation
While input validation is often emphasized, output validation is an equally critical defense mechanism. It involves sanitizing data before it leaves an API or system to prevent accidental exposure of sensitive information [9]. This includes:
- Preventing Data Leakage: Removing sensitive internal metadata, debugging information, or Personally Identifiable Information (PII) from API responses [9].
- Ensuring Response Consistency: Applying data minimization principles to return only necessary information to the client, using standardized and secure response formats [9].
Validating the Validator: Test Method Validation (TMV)
In medical device and pharmaceutical development, the integrity of test data depends on a fundamental principle—the test method itself must be validated [8]. Test Method Validation (TMV) ensures that both hardware and software test methods produce accurate, consistent, and reproducible results, independent of the operator, location, or time of execution [8].
TMV Experimental Protocol Framework
The following protocol provides a generalized framework for validating a test method, adaptable for both hardware and software contexts in a research environment.
Table 2: Experimental Protocol for Test Method Validation
| Protocol Step | Objective | Key Activities & Measured Outcomes |
|---|---|---|
| 1. Define Objective | To clearly state the purpose of the test method and what it intends to measure. | Define the Measurement Variable (e.g., bond strength, concentration, software response time). Document acceptance criteria based on regulatory standards and product requirements [8]. |
| 2. Develop Method | To establish a detailed, reproducible test procedure. | Select and calibrate equipment. Write a step-by-step test procedure. For software, this includes developing automated test scripts [8]. |
| 3. Perform Gage R&R (Hardware Focus) | To quantify the measurement system's variation (repeatability and reproducibility). | Multiple operators repeatedly measure a set of representative samples. Calculate %GR&R; a value below 10% is generally considered acceptable, indicating the method is capable [8]. |
| 4. Verify Test Code (Software Focus) | To ensure automated test scripts are functionally correct and maintainable. | Perform code review. Establish traceability from test scripts to software requirements (e.g., via a Requirements Traceability Matrix). Validate script output for known inputs [8]. |
| 5. Assess Accuracy & Linearity | To evaluate the method's trueness (bias) and performance across the operating range. | Measure certified reference materials across the intended range. Calculate bias and linear regression statistics (R², slope) [12] [8]. |
| 6. Evaluate Robustness | To determine the method's resilience to small, deliberate changes in parameters. | Vary key parameters (e.g., temperature, humidity, input voltage) within a expected operating range and monitor the impact on results [8]. |
| 7. Document & Approve | To generate objective evidence that the method is fit for its intended use. | Compile a TMV Report including protocol, raw data, analysis, and conclusion. Obtain formal approval before releasing the method for use [8]. |
The workflow for establishing a validated test method, from definition to documentation, is systematized as follows:
The Validation Lifecycle: Process Validation in Six Sigma
For processes that are consistently executed, such as manufacturing a drug substance, a lifecycle approach to validation is required. Process validation is defined as the collection and evaluation of data, from the process design stage through commercial production, which establishes scientific evidence that a process is capable of consistently delivering a quality product [13]. This aligns with the FDA's guidance and is effectively implemented using the DMAIC (Define, Measure, Analyze, Improve, Control) framework from Six Sigma [13].
The Three Stages of Process Validation
The lifecycle model consists of three integrated stages:
- Process Design: Building quality into the process through development and scale-up. Critical Quality Attributes (CQAs) and Critical Process Parameters (CPPs) are identified. Tools like Design of Experiments (DOE) and Failure Mode and Effects Analysis (FMEA) are used to understand and mitigate risks [13].
- Process Qualification: Confirming the process design is effective during commercial manufacturing. This includes equipment qualification (IQ/OQ/PQ) and Process Performance Qualification (PPQ) to demonstrate consistency [13].
- Continued Process Verification: Maintaining the validated state through ongoing monitoring. Statistical Process Control (SPC) charts are used to detect process shifts, ensuring long-term control and enabling continuous improvement [13].
The following diagram illustrates the interconnected, lifecycle nature of process validation:
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential "reagents" or tools in the validation scientist's toolkit, which are critical for executing the protocols and techniques described in this document.
Table 3: Essential Research Reagent Solutions for Validation
| Tool / Solution | Function in Validation | Application Context |
|---|---|---|
| GAMP 5 Framework [7] | A risk-based framework for classifying and validating computerized systems, crucial for regulatory compliance. | Categorizing software from infrastructure (Cat. 1) to custom (Cat. 5) and defining appropriate validation rigor for each [7]. |
| Statistical Analysis Software (e.g., JMP, R) | Used for conducting Gage R&R studies, regression analysis, capability analysis (Cp, Cpk), and creating control charts. | Analyzing measurement system variation in TMV and monitoring process performance in Continued Process Verification [13] [12]. |
| JSON Schema / XML Schema | A declarative language for defining the expected structure, data types, and constraints of data payloads. | Implementing automated input validation for APIs and web services to ensure data quality and security [9]. |
| Validation Manager Software [12] | A specialized platform for planning, executing, and documenting analytical method comparisons and instrument verifications. | Automating data management and report generation for quantitative comparisons, such as bias estimation using Bland-Altman plots [12]. |
| Pydantic / Joi Libraries [9] | Programming libraries for implementing type and constraint validation logic within application code. | Ensuring data integrity in Python (Pydantic) or Node.js (Joi) applications by validating data types, ranges, and custom business rules [9]. |
| Electronic Lab Notebook (ELN) | A system for digitally capturing and managing experimental data and metadata, supporting data integrity principles. | Providing an audit trail for TMV protocols and storing raw validation data, ensuring ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate) [7]. |
The integration of Artificial Intelligence (AI) and machine learning (ML) into healthcare is transforming drug development, medical device innovation, and patient care. These technologies can derive novel insights from the vast amounts of data generated daily within healthcare systems [14]. However, their adaptive, complex, and often opaque nature challenges traditional regulatory paradigms. Consequently, major regulatory bodies, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), have developed specific frameworks and guidelines to ensure that AI/ML technologies used in medical products and drug development are safe, effective, and reliable [14] [15]. For researchers and scientists, understanding these perspectives is crucial for navigating the path from innovation to regulatory approval. This document outlines the core regulatory principles, summarizes them for easy comparison, and provides actionable experimental protocols for validating AI systems within this evolving landscape, with a specific focus on input-output transformation validation methods.
United States Food and Drug Administration (FDA) Approach
The FDA's approach to AI has evolved significantly, moving from a traditional medical device regulatory model to one that accommodates the unique lifecycle of AI/ML technologies. The agency recognizes that the greatest potential of AI lies in its ability to learn from real-world use and improve its performance over time [14]. A key development was the 2019 discussion paper and subsequent "Artificial Intelligence and Machine Learning Software as a Medical Device (SaMD) Action Plan" published in January 2021, which laid the groundwork for a more adaptive regulatory pathway [14].
The FDA's current strategy is articulated through several key guidance documents and principles:
- Good Machine Learning Practice (GMLP): The FDA, in collaboration with other partners, has outlined guiding principles for Good Machine Learning Practice in medical device development [14].
- Predetermined Change Control Plans (PCCP): A pivotal concept introduced by the FDA is the Predetermined Change Control Plan, which allows manufacturers to pre-specify certain types of modifications to an AI-enabled device—such as performance enhancements or bias mitigation—and the protocols for implementing them, without necessitating a new marketing submission for each change [14] [16]. A final guidance on marketing submission recommendations for a PCCP was issued in December 2024 [14].
- Lifecycle Management: In January 2025, the FDA released a draft guidance titled "Artificial Intelligence-Enabled Device Software Functions: Lifecycle Management and Marketing Submission Recommendations." This document provides comprehensive recommendations for the total product life cycle of AI-enabled devices, from pre-market development to post-market monitoring [14] [16]. It emphasizes a risk-based approach, transparency, and the management of issues like bias and data drift [16].
- Cross-Center Coordination: The FDA has adopted a coordinated approach across its centers—CBER, CDER, CDRH, and OCP—to drive alignment and share learnings on AI applicable to all medical products [14] [17].
For drug development specifically, the FDA's CDER has established a CDER AI Council to oversee and coordinate activities related to AI, reflecting the significant increase in drug application submissions using AI components [17]. In January 2025, the FDA also released a separate draft guidance, "Considerations for the Use of Artificial Intelligence to Support Regulatory Decision-Making for Drug and Biological Products," which provides a risk-based credibility assessment framework for AI models used in this context [18] [17].
European Medicines Agency (EMA) Approach
The EMA views AI as a key tool for leveraging large volumes of health data to encourage research, innovation, and support regulatory decision-making [15]. The agency's strategy is articulated through the workplan of the Network Data Steering Group for 2025-2028, which focuses on four key AI-related areas: guidance and policy, tools and technology, collaboration and change management, and structured experimentation [15].
Key EMA outputs include:
- Reflection Paper on AI: In September 2024, the CHMP and CVMP adopted a reflection paper on the use of AI in the medicinal product lifecycle. This paper provides considerations for medicine developers to use AI and ML in a safe and effective way at different stages of a medicine's life [15].
- Annex 22 on AI in GxP: In a landmark move in July 2025, the EMA, via the GMDP Inspectors Working Group, published a draft of Annex 22 as part of the updates to EudraLex Volume 4. This is the first dedicated GxP framework for AI and ML systems used in the manufacture of active substances and medicinal products [19] [20]. Annex 22 sets clear expectations for intended use documentation, performance validation, independent testing, explainability, and qualified human oversight [19]. It explicitly excludes dynamic or generative AI models from critical applications, emphasizing consistency and accountability [19].
- Large Language Model (LLM) Guiding Principles: The EMA and HMA have also published guiding principles for the use of large language models by regulatory network staff, promoting safe, responsible, and effective use of this technology [15].
- AI Observatory: The EMA has established an AI Observatory to capture and share experiences and trends in AI, which includes horizon scanning and an annual report [15].
The EMA's approach, particularly with Annex 22, integrates AI regulation into the existing GxP framework, requiring that AI systems be governed by the same principles of quality, validation, and accountable human oversight that apply to other computerized systems and processes [19] [20].
Comparative Analysis of FDA and EMA Guidelines
The following tables provide a structured comparison of the regulatory approaches and technical requirements of the FDA and EMA regarding AI in healthcare and drug development.
Table 1: Core Regulatory Focus and Application Scope
| Aspect | U.S. Food and Drug Administration (FDA) | European Medicines Agency (EMA) |
|---|---|---|
| Primary Focus | Safety & effectiveness of AI as a medical product or tool supporting drug development [14] [18]. | Use of AI within the medicinal product lifecycle & GxP processes [15] [20]. |
| Governing Documents | AI/ML SaMD Action Plan; Good MLP Principles; Draft & Final Guidances on PCCP & Lifecycle Management (2023-2025) [14] [16]. | Reflection Paper on AI (2024); Draft Annex 22 to GMP (2025); Revised Annex 11 & Chapter 4 [15] [19] [20]. |
| Regulatory Scope | AI-enabled medical devices (SaMD, SiMD); AI to support regulatory decisions for drugs & biologics [14] [18]. | AI used in drug manufacturing (GxP environments); AI in the broader medicinal product lifecycle [15] [20]. |
| Core Paradigm | Risk-based, Total Product Life Cycle (TPLC) approach [16]. | Risk-based, integrated within existing GxP quality systems [19] [20]. |
| Key Mechanism for Adaptation | Predetermined Change Control Plan (PCCP) [14] [16]. | Formal change control under quality management system (QMS) [20]. |
Table 2: Technical and Validation Requirements for Input-Output Transformation
| Requirement | FDA Perspective | EMA Perspective |
|---|---|---|
| Validation | Confirmation through objective evidence that device meets intended use [16]. Must reflect real-world conditions [21]. | Validation against predefined metrics; integrated into computerized system validation [19] [20]. |
| Data Management | Data diversity & representativeness; prevention of data leakage; ALCOA+ principles for data integrity [21] [16]. | GxP standards for data accuracy, integrity, and traceability [19] [20]. |
| Transparency & Explainability | Critical information must be understandable/accessible; "black-box" nature must be addressed [16]. | Decisions must be subject to qualified human review; explainability required [19] [20]. |
| Bias Control & Management | Address throughout lifecycle; ensure data reflects intended population; proactive identification of disparities [16]. | Implied through requirements for data quality, representativeness, and validation [19]. |
| Lifecycle Monitoring | Ongoing performance monitoring for drift; continuous validation [21] [16]. | Continuous oversight to detect performance drift; formal change control for updates [20]. |
| Human Oversight | "Human-AI team" performance evaluation encouraged (e.g., reader studies) [16]. | Qualified human review mandatory for critical decisions; accountability cannot be transferred to AI [19] [20]. |
Experimental Protocols for Regulatory Validation
This section provides detailed methodological protocols for key experiments and studies required to demonstrate the safety and effectiveness of AI systems, aligning with FDA and EMA expectations for input-output transformation validation.
Protocol 1: Model Validation and Performance Benchmarking
1. Objective: To rigorously assess the performance, robustness, and generalizability of an AI model using independent datasets, ensuring it meets predefined performance criteria for its intended use.
2. Background: Regulatory agencies require that AI models be validated on datasets that are independent from the training data to provide an unbiased estimate of real-world performance and to ensure the model is generalizable across relevant patient demographics and clinical settings [16].
3. Materials and Reagents: Table 3: Research Reagent Solutions for AI Validation
| Item | Function |
|---|---|
| Curated Training Dataset | Used for initial model development and parameter tuning. Must be well-characterized and documented. |
| Independent Validation Dataset | A held-aside dataset used for unbiased performance estimation. Must be statistically independent from the training set. |
| External Test Dataset | Data collected from a different source or site than the training data, used to assess generalizability. |
| Data Annotation Protocol | Standardized procedure for labeling data, ensuring consistency and quality of ground truth labels. |
| Performance Metric Suite | A set of quantitative measures (e.g., AUC, accuracy, sensitivity, specificity, F1-score) to evaluate model performance. |
4. Methodology:
- 4.1. Data Segmentation: Partition available data into three distinct sets: Training Set (~70%), Validation Set (~15%), and Hold-out Test Set (~15%). Ensure stratification to maintain distribution of key variables (e.g., disease severity, demographics) across sets.
- 4.2. Subgroup Analysis: Define and analyze performance metrics for critical subgroups based on age, sex, ethnicity, disease subtype, and imaging equipment to identify potential performance disparities and bias [16].
- 4.3. Statistical Analysis:
- Calculate all predefined performance metrics with 95% confidence intervals.
- Perform statistical significance testing (e.g., McNemar's test) to compare model performance against a baseline or comparator, if applicable.
- For diagnostic tools, conduct a reader study to evaluate the "human-AI team" performance compared to either alone [16].
5. Data Analysis: The model is deemed to have passed validation if all primary performance metrics meet or exceed the pre-specified success criteria on the independent test set and across all major subgroups, demonstrating robustness and lack of significant bias.
Protocol 2: Monitoring for Data and Concept Drift
1. Objective: To establish a continuous, post-market surveillance system for detecting and quantifying data drift and concept drift that may degrade AI model performance in real-world use.
2. Background: AI models are sensitive to changes in input data distribution (data drift) and changes in the relationship between input and output data (concept drift) [22] [16]. The FDA and EMA expect ongoing lifecycle monitoring to ensure sustained safety and effectiveness [22] [21].
3. Materials and Reagents:
- Incoming Real-World Data Stream: Data from the deployed clinical environment.
- Baseline Data Statistical Profile: The statistical properties (e.g., mean, variance, distribution) of the data used for model training and initial validation.
- Automated Monitoring Dashboard: A tool for visualizing key drift metrics and triggering alerts.
4. Methodology:
- 4.1. Establish Baseline: Characterize the reference training data by calculating feature distributions, summary statistics, and correlation matrices to create a baseline profile.
- 4.2. Define Drift Thresholds: Set statistically driven thresholds for triggering alerts. For example, a significant change in a feature's distribution using the Population Stability Index (PSI) or Kolmogorov-Smirnov (KS) test.
- 4.3. Implement Monitoring:
- 4.4. Root Cause Analysis: Upon triggering a drift alert, initiate an investigation to identify the cause (e.g., change in clinical protocol, new patient population, shift in data acquisition hardware/software).
5. Data Analysis: Regularly report drift metrics and performance KPIs. A confirmed, significant drift that negatively impacts performance should trigger the model's retraining protocol, which is governed by the Predetermined Change Control Plan (for FDA) or formal change control process (for EMA) [16] [20].
Protocol 3: Human Factors and Usability Validation
1. Objective: To evaluate the usability of the AI system's interface and ensure that the intended users can interact with the system safely and effectively to achieve the intended clinical outcome.
2. Background: The FDA requires human factors and usability studies for medical devices to minimize use errors [16]. The EMA's Annex 22 mandates that decisions made or proposed by AI must be subject to qualified human review, making the human-AI interaction critical [20].
3. Methodology:
- 4.1. Formative Studies: Conduct early-stage testing with a small group of representative users (e.g., clinicians, radiologists) to identify and rectify usability issues in the design phase.
- 4.2. Summative Validation Study: Perform a simulated-use study with a larger group of participants. Provide them with realistic clinical tasks that involve using the AI system's output to make a decision.
- 4.3. Data Collection: Record all use errors, near misses, and subjective feedback. Measure task success rate, time-on-task, and the user's mental workload (e.g., using NASA-TLX scale).
- 4.4. "Human-AI Team" Performance Assessment: As encouraged by the FDA, compare the diagnostic or decision-making accuracy of the user alone, the AI system alone, and the user assisted by the AI system [16].
5. Data Analysis: The validation is successful if all critical tasks are completed without recurring, unmitigated use errors that could harm the patient, and the "human-AI team" demonstrates non-inferiority or superiority to the human alone.
Visualization of Regulatory Workflows
The following diagrams illustrate the core workflows for navigating the FDA and EMA regulatory pathways for AI-enabled technologies, highlighting the parallel processes and key decision points.
Diagram 1: AI Regulatory Pathways
Diagram 2: AI Validation Lifecycle
In pharmaceutical research and development, the principles of verification and validation (V&V) are foundational to ensuring product quality and regulatory compliance. These processes represent a systematic approach to input-output transformation, where user needs are transformed into a final product that is both high-quality and fit for its intended use. Verification confirms that each transformation step correctly implements the specified inputs, while validation demonstrates that the final output meets the original user needs and intended uses in a real-world environment [23] [24]. This framework is crucial for drug development professionals who must navigate complex regulatory landscapes while bringing safe and effective products to market.
Core Concepts and Definitions
Verification: Building it Right
Design verification is defined as "confirmation by examination and provision of objective evidence that specified requirements have been fulfilled" [23] [24]. In essence, verification answers the question: "Did we build the product right?" by ensuring that design outputs match the design inputs specified during development [24]. This process involves checking whether the product conforms to technical specifications, standards, and regulations through rigorous testing at the subsystem level.
Verification activities typically include:
- Reviewing design documents and specifications
- Conducting technical inspections
- Performing bench testing and static analysis
- Executing component-level functional tests [24]
Validation: Building the Right Thing
Design validation is defined as "establishing by objective evidence that device specifications conform with user needs and intended use(s)" [23] [24]. Validation answers the question: "Did we build the right product?" by demonstrating that the final product meets the user requirements and is suitable for its intended purpose in actual use conditions [24]. This process focuses on the user's interaction with the complete system in real-world environments.
Validation activities typically include:
- Conducting functional and performance testing
- Executing usability studies and clinical evaluations
- Performing real-world environment testing
- Assessing biocompatibility and safety [24]
Table 1: Fundamental Differences Between Verification and Validation
| Aspect | Verification | Validation |
|---|---|---|
| Primary Question | Did we build it right? | Did we build the right thing? |
| Focus | Design outputs vs. design inputs | Device specifications vs. user needs |
| Timing | During development | Typically at development completion |
| Methods | Reviews, inspections, bench testing | Real-world testing, clinical trials, usability studies |
| Scope | Sub-system level components | Complete system in operational environment |
| Output | Review reports, inspection records | Test reports, acceptance documentation [23] [24] |
Regulatory Context in Pharmaceutical Development
Analytical Methodology Framework
In pharmaceutical development, the V&V framework extends to analytical methods with precise regulatory definitions:
Validation: Formal demonstration that an analytical method is suitable for its intended use, producing reliable, accurate, and reproducible results across a defined range. Required for methods used in routine quality control testing of drug substances, raw materials, or finished products [25].
Verification: Confirmation that a previously validated method works as expected in a new laboratory or under modified conditions. This is typically required for compendial methods (USP, Ph. Eur.) adopted by a new facility [25].
Qualification: Early-stage evaluation of an analytical method's performance during development phases (preclinical or Phase I trials) to demonstrate the method is likely reliable before full validation [25].
FDA and ICH Requirements
Regulatory bodies including the FDA and EMA require well-documented V&V plans, test protocols, and results to ensure devices meet requirements and are fit for use [23]. For analytical methods, the ICH Q2(R1) guideline provides the definitive framework for validation parameters, which must be thoroughly documented to support regulatory submissions and internal audits [25].
Table 2: Analytical Method V&V Approaches in Pharmaceutical Development
| Approach | When Used | Key Parameters | Regulatory Basis |
|---|---|---|---|
| Method Validation | For release testing, stability studies, batch quality assessment | Accuracy, precision, specificity, linearity, range, LOD, LOQ, robustness | ICH Q2(R1), FDA requirements for decision-making |
| Method Verification | Adopting established methods in new labs or for similar products | Limited assessment of accuracy, precision, specificity | Confirmation of compendial method performance |
| Method Qualification | Early development when full validation not yet required | Specificity, linearity, precision optimization | Supports development decisions before validation |
Experimental Protocols and Application Notes
Protocol 1: Design Verification Process
Objective: To confirm that design outputs meet all specified design input requirements.
Materials and Reagents:
- Complete set of design input specifications
- Design history file including all outputs
- Verification test equipment and instrumentation
- Documented verification protocol
Methodology:
- Requirements Mapping: Trace each design input to corresponding design outputs
- Inspection Protocol: Examine components against technical specifications
- Bench Testing: Perform functional tests on subsystems
- Analysis: Compare test results against acceptance criteria
- Documentation: Record all verification activities and results
Acceptance Criteria: All design outputs must conform to design input requirements with objective evidence documented for each requirement [24].
Protocol 2: Design Validation Process
Objective: To establish by objective evidence that device specifications conform to user needs and intended uses.
Materials and Reagents:
- Defined user needs and intended use statements
- Final device specification document
- Validation test protocol approved by quality unit
- Real-world simulated use environment
Methodology:
- User Needs Assessment: Confirm traceability from user needs to design specifications
- Real-World Testing: Evaluate device in simulated use environment
- Performance Testing: Assess device under actual use conditions
- Usability Evaluation: Conduct studies with intended users
- Data Analysis: Compare results against user need requirements
Acceptance Criteria: Device must perform as intended for its defined use with all user needs met under actual use conditions [24].
Protocol 3: Analytical Method Verification
Objective: To verify that a compendial method performs as expected when implemented in a new laboratory.
Materials and Reagents:
- Reference standards with documented purity
- Compendial method documentation (USP, Ph. Eur.)
- Qualified instrumentation and equipment
- Appropriate chemical reagents and solvents
Methodology:
- System Suitability: Confirm the system meets compendial requirements
- Precision Assessment: Perform six replicate injections of standard preparation
- Accuracy Evaluation: Spike placebo with known analyte quantities (80%, 100%, 120%)
- Specificity Verification: Demonstrate analytical response is from analyte alone
- Report Results: Compare obtained values against acceptance criteria
Acceptance Criteria: Method performance must meet predefined acceptance criteria for accuracy, precision, and specificity as defined in the verification protocol [25].
Visualization of V&V Workflows
Input-Output Transformation Model
Input-Output Transformation V&V Model: This diagram illustrates the sequential transformation from user needs to final product, with verification and validation checkpoints ensuring correctness and appropriateness at each stage.
Pharmaceutical Analytical Method Decision Framework
Analytical Method Decision Framework: This workflow provides a systematic approach for drug development professionals to determine the appropriate methodology pathway based on method novelty, regulatory status, and development phase.
Research Reagent Solutions and Materials
Table 3: Essential Research Materials for V&V Activities
| Material/Reagent | Function in V&V | Application Context |
|---|---|---|
| Reference Standards | Provide known purity materials for method accuracy determination | Analytical method validation and verification |
| System Suitability Test Materials | Verify chromatographic system performance before analysis | HPLC/UPLC method validation and verification |
| Placebo Formulation | Assess method specificity and interference | Analytical method validation for drug products |
| Certified Calibration Equipment | Ensure measurement accuracy and traceability | Device performance verification |
| Biocompatibility Test Materials | Evaluate biological safety of device materials | Medical device validation for regulatory submission |
| Stability Study Materials | Assess method and product stability under various conditions | Forced degradation and shelf-life studies |
The distinction between verification and validation is fundamental to successful pharmaceutical development and regulatory compliance. Verification ensures that products are built correctly according to specifications, while validation confirms that the right product has been built to meet user needs. The input-output transformation framework provides a systematic approach for researchers and drug development professionals to implement these processes effectively throughout the product lifecycle. By adhering to the detailed protocols and decision frameworks outlined in these application notes, organizations can enhance product quality, reduce development risks, and streamline regulatory approvals.
In the landscape of modern drug development, the validation of input-output transformations is a cornerstone of scientific and regulatory credibility. This process ensures that the data entering analytical systems emerges as reliable, actionable knowledge. At the heart of this validation lie three critical data quality dimensions: Completeness, Consistency, and Integrity. These are not isolated attributes but interconnected pillars that collectively determine whether a dataset is fit-for-purpose, especially within highly regulated pharmaceutical research and development [26] [27]. For researchers and scientists, mastering these dimensions is fundamental to reconstructing the data lineage from raw inputs to polished outputs, thereby safeguarding patient safety and the efficacy of therapeutic interventions [28].
The consequences of neglecting data quality are severe, ranging from financial losses and regulatory actions to direct risks to patient safety [27]. Furthermore, with the increasing integration of Artificial Intelligence (AI) in drug discovery and manufacturing, the adage "garbage in, garbage out" becomes ever more critical. The efficacy of AI models is entirely contingent on the quality of the data on which they are trained and operated, making rigorous data quality practices a prerequisite for trustworthy AI-driven innovation [29]. This application note details the protocols and best practices for ensuring these foundational data quality dimensions within the context of input-output transformation validation.
Core Data Quality Dimensions in Pharmaceutical Research
For data to be considered high-quality in a regulatory and research context, it must excel across multiple dimensions. The following table summarizes the six core dimensions of data quality, with a focus on the three pillars of this discussion [27]:
Table 1: Core Data Quality Dimensions for Drug Development
| Dimension | Definition | Impact on Drug Development & Research |
|---|---|---|
| Completeness | The presence of all necessary data required to address the study question, design, and analysis [26]. | Prevents bias in study populations and outcomes; ensures sufficient data for robust statistical analysis [26]. |
| Consistency | The stability and uniformity of data across sites, over time, and across linked datasets [26]. | Ensures that analytics correctly capture the value of data; discrepancies can indicate systemic errors [27]. |
| Integrity | The maintenance of accuracy, consistency, and traceability of data over its entire lifecycle, including correct attribute relationships across systems [28] [27]. | Ensures that all enterprise data can be traced and connected; foundational for audit trails and regulatory compliance [28]. |
| Accuracy | The level to which data correctly represents the real-world scenario it is intended to depict and confirms to a verifiable source [27]. | Powers factually correct reporting and trusted business decisions; critical for patient safety and dosing [27]. |
| Uniqueness | A measure that the data represents a single, non-duplicated instance within a dataset [27]. | Ensures no duplication or overlaps, which is critical for accurate patient counts and inventory management. |
| Validity | The degree to which data conforms to the specific syntax (format, type, range) of its definition [27]. | Guarantees that data values align with the expected domain, such as valid ZIP codes or standard medical terminologies. |
The ALCOA+ framework, mandated by regulators, provides a practical set of principles for achieving data integrity, which encompasses completeness, consistency, and accuracy. It stipulates that data must be Attributable, Legible, Contemporaneous, Original, and Accurate, with the "plus" adding that it must also be Complete, Consistent, Enduring, and Available [28] [30]. Adherence to ALCOA+ is a primary method for ensuring data quality throughout the drug development lifecycle.
Experimental Protocols for Data Quality Validation
Validating data quality requires a multi-layered testing strategy. The following protocols can be integrated into data pipeline development to verify and validate transformations.
Protocol for Schema and Metadata Validation
This protocol ensures the structural integrity of data before and after transformations.
- Objective: To enforce that incoming and transformed data conform to expected schemas, data types, and constraints [31].
- Materials:
- JSON Schema or Apache Avro: For defining and enforcing expected data structures.
- Validation Framework: Such as Great Expectations or Pydantic in Python.
- Business Rules Document: A pre-defined list of domain-specific constraints (e.g., value ranges, mandatory fields).
- Methodology:
- Schema Definition: Formally define the expected schema for input data, including data types (string, integer), formats (email, date), and nullability.
- Validation Checkpoint: Implement a validation step early in the data pipeline, ideally as middleware or a pre-processing hook [9].
- Rule Execution: The system checks all incoming data against the defined schema and business rules.
- Exception Handling: Data that fails validation is routed to a quarantine area for review, and an error is logged. The process should not proceed until the data is corrected or its rejection is confirmed [9].
- Output: A validation report detailing the number of records processed, records failed, and specific errors for each failed record (e.g., "Field 'patient_age': value '-5' is less than minimum (0)") [9].
Protocol for Unit and Integration Testing of Data Transformations
This protocol verifies the correctness of the transformation logic itself.
- Objective: To validate specific transformation functions (unit tests) and several transformations working together (integration tests) using known input-output pairs [31].
- Materials:
- Testing Framework: PyTest (Python), JUnit (Java).
- Test Harness: A controlled environment, potentially using Docker, to mimic pipeline steps.
- Golden Datasets: Small, curated datasets with known inputs and expected outputs.
- Methodology:
- Unit Test Creation: For each discrete transformation function (e.g., a function that normalizes laboratory unit names), write tests with known inputs and expected outputs.
- Parameterized Testing: Use the testing framework to run the same test logic with multiple input-output pairs from the golden dataset.
- Integration Test Creation: Construct tests that execute a sequence of transformations, simulating a segment of the full pipeline.
- Test Execution and Regression: Integrate tests into a continuous integration (CI) system to run automatically, ensuring that new code changes do not break existing transformation logic (regression testing) [31].
- Output: A test execution report showing pass/fail status for all tests. Failed tests indicate a logic error in the transformation code that must be investigated.
Protocol for Data Integrity and Consistency Auditing
This protocol ensures the ongoing integrity and consistency of data throughout its lifecycle.
- Objective: To verify that data remains accurate, consistent, and traceable after storage and across systems, in line with ALCOA+ principles [28].
- Materials:
- Automated Audit Trail System: A secure, time-stamped electronic record that tracks the creation, modification, or deletion of any data [28].
- Data Comparison Tools: Scripts or software (e.g., custom Python/R scripts, Diff utilities) to compare data across systems.
- Access to Source Systems: The ability to trace data back to its original source.
- Methodology:
- Audit Trail Review: Periodically sample records and use the audit trail to reconstruct their entire history, verifying that all changes are attributable and justified.
- Cross-System Consistency Check: For data stored in multiple locations (e.g., a clinical database and a data warehouse), run scripts to compare key records and ensure values match.
- Traceability Verification: Select a final analysis result (output) and trace it backward through the transformation pipelines to the original source data (input), ensuring no breaks in lineage.
- Output: An audit report confirming data integrity or highlighting discrepancies found in the audit trail, cross-system checks, or traceability verification.
The logical workflow for implementing these validation protocols is summarized in the following diagram:
The Researcher's Toolkit: Essential Reagents for Data Quality
Table 2: Key Research Reagent Solutions for Data Quality Assurance
| Category / Tool | Specific Examples | Function & Application in Data Quality |
|---|---|---|
| Schema Enforcement | JSON Schema, Apache Avro, XML Schema | Defines the expected structure, format, and data types for input and output data, enabling automated validation of completeness and validity [9] [31]. |
| Testing Frameworks | PyTest (Python), JUnit (Java), NUnit (.NET) | Provides the infrastructure to build and run unit and integration tests, verifying the correctness of data transformation logic against known inputs and outputs [31]. |
| Data Profiling & Validation | Great Expectations, Pandas Profiling, Deequ | Libraries that automatically profile datasets to generate summaries and validate data against defined expectations, checking for accuracy, consistency, and uniqueness [31]. |
| Audit Trail Systems | Electronic Lab Notebook (ELN) systems, Database triggers, Version control (e.g., Git) | Creates a secure, time-stamped record of all data-related actions, ensuring integrity by making data changes attributable and traceable, a core requirement of ALCOA+ [28]. |
| Reference Data | Golden Datasets, Standardized terminologies (e.g., CDISC, IDMP) | A trusted, curated set of data used as a baseline to compare transformation outputs, serving as a benchmark for accuracy and a tool for regression testing [31]. |
In the rigorous world of drug development, where decisions directly impact human health, there is no room for ambiguous or unreliable data. The principles of Completeness, Consistency, and Integrity form an indissoluble chain that protects the validity of input-output transformations from the laboratory bench to regulatory submission. By implementing the structured protocols and tools outlined in this application note—from schema validation and unit testing to comprehensive integrity auditing—researchers and scientists can build a robust defense against data corruption and bias.
This disciplined approach to data quality is the bedrock upon which trustworthy analytics, credible AI models, and ultimately, safe and effective medicines are built. As regulatory bodies like the FDA and EMA increasingly focus on data governance, mastering these fundamentals is not just a scientific best practice but a regulatory imperative for bringing new therapies to market [29] [32].
From Theory to Pipeline: A Practical Toolkit for Implementation
In the context of input-output transformation validation methods research, structural validation refers to the systematic enforcement of predefined rules governing the organization, format, and relationships within data. This process ensures that data adheres to consistent structural patterns, which is a critical prerequisite for reliable data transformation and analysis. For researchers and scientists, particularly in drug development where data integrity is paramount, implementing robust structural validation frameworks guarantees that input data quality is maintained throughout complex processing pipelines, leading to trustworthy, reproducible outputs.
Structural metadata serves as the foundational blueprint for this validation process. It defines the organizational elements that describe how data is structured within a dataset or system, including data relationships, formats, hierarchical organization, and integrity constraints [33]. In scientific computing and data analysis, this translates to enforcing consistent structures in instrument data outputs, experimental metadata, and clinical trial data, ensuring all downstream consumers—whether automated algorithms or research professionals—can correctly interpret and utilize the information.
Core Principles of Structural Validation
Schema Validation Fundamentals
Schema validation ensures incoming data structures match expected patterns before processing. Using JSON Schema, XML Schema, or Protocol Buffer schemas, researchers can define exact specifications for their API communications or data file formats [9]. This preemptive validation prevents malformed data from entering analytical systems, protecting the integrity of scientific computations.
A typical JSON schema for an experimental metadata might define:
Type Checking and Data Coercion
Type checking verifies data matches expected formats, preventing critical errors such as numerical calculations on string data or inserting text into numeric database fields [9]. In scientific contexts, where data may originate from multiple instrument sources, explicit type validation with clear error messages is essential for maintaining data quality.
Content Validation Strategies
Content validation ensures actual data values are acceptable through:
- Pattern matching (using regular expressions for identifier formats)
- Format validation (ensuring dates, numerical values fall within expected ranges)
- Range checking (verifying numerical values adhere to physiological or instrument limits)
- Business logic validation (ensuring data relationships make scientific sense)
The most effective approach is whitelisting (allowlisting), which defines exactly what's permitted and rejects everything else, as recommended by OWASP security guidelines [9].
Contextual and Semantic Validation
Contextual validation applies domain-specific business logic rules beyond basic syntax checking. In drug development, this might include verifying that clinical trial start dates precede end dates, that dosage values fall within established safety ranges, or that patient identifier codes follow institutional formatting standards [9].
Validation Methodologies and Experimental Protocols
Protocol Buffer Schema Validation
For high-performance scientific data exchange, Protocol Buffer schema validation ensures encoded messages conform to expected structures. The validation process follows a rigorous methodology [34]:
- Message Descriptor Lookup: The schema registry retrieves Key and Value message descriptors by name
- Record Iteration: Each record in a data batch undergoes validation
- Key Validation: Validates key bytes against the key descriptor if present
- Value Validation: Validates value bytes against the value descriptor if present
- Deserialization: Uses
CodedInputStreamto parse bytes into message instances - Error Handling: Any deserialization failure returns
ErrorCode::InvalidRecord
Table 1: Protocol Buffer Validation Behavior Matrix
| Scenario | Key Schema | Value Schema | Record Key | Record Value | Validation Result |
|---|---|---|---|---|---|
| Complete validation | Present | Present | Must match | Must match | Validated |
| Value-only validation | Absent | Present | Any bytes | Must match | Validated |
| Key-only validation | Present | Absent | Must match | Any bytes | Validated |
| No schema defined | Absent | Absent | Any bytes | Any bytes | Passes (no-op) |
| Missing required key | Present | - | None | - | InvalidRecord |
| Corrupted value data | - | Present | - | Invalid | InvalidRecord |
Implementation code for Protocol Buffer validation follows this pattern [34]:
JSON Schema Validation Protocol
For research data management, JSON schema validation enforces consistent structure for experimental metadata. The implementation protocol involves [35]:
- Schema Definition: Create a JSON schema defining required metadata structure
- Schema Registration: Apply the schema to the project or data system
- Validation Enforcement: Configure data upload processes to validate against schema
- Error Handling: Capture and report validation failures with specific field-level details
A typical experimental workflow implements this as:
Input/Output Validation Security Protocol
Input/output validation serves as a critical security measure in research data pipelines, protecting against data corruption and injection attacks. The security validation protocol includes [9]:
- Schema Validation: Apply JSON Schema or similar validation early in request processing
- Type Checking: Verify data types match expected formats
- Size and Range Validation: Prevent resource exhaustion attacks with appropriate limits
- Content Sanitization: Remove or escape potentially harmful content
- Output Encoding: Ensure safe data rendering in outputs
Table 2: Input Validation Techniques for Scientific Data Systems
| Technique | Implementation | Security Benefit | Research Application |
|---|---|---|---|
| Schema Validation | JSON Schema, Protobuf | Rejects malformed data | Ensures instrument data conformity |
| Type Checking | Runtime type verification | Prevents type confusion errors | Maintains data type integrity |
| Range Checking | Minimum/maximum values | Prevents logical errors | Validates physiologically plausible values |
| Content Whitelisting | Allow-only approach | Blocks unexpected formats | Ensures data domain compliance |
| Output Encoding | Context-aware escaping | Prevents injection attacks | Secures data visualization |
Quantitative Validation Metrics and Performance
Validation systems require comprehensive metrics and observability to ensure performance and reliability. The Tansu validation framework implements these key metrics [34]:
registry_validation_duration: Histogram tracking latency of validation operations in millisecondsregistry_validation_error: Counter tracking validation failures with reason labels
Table 3: Validation Performance Metrics
| Metric Name | Type | Unit | Labels | Description |
|---|---|---|---|---|
| validation_duration | Histogram | milliseconds | topic, schema_type | Latency of validation operations |
| validation_success | Counter | count | topic, schema_type | Count of successful validations |
| validation_error | Counter | count | topic, reason | Count of validation failures by cause |
| batch_size | Histogram | records | topic | Distribution of validated batch sizes |
Performance optimization strategies include:
- Schema Caching: Reduces latency by caching compiled schemas in memory [35]
- Batch Validation: Processes multiple records simultaneously for throughput [34]
- Early Rejection: Fails fast on first validation error to conserve resources [9]
Research Reagent Solutions
Table 4: Essential Research Reagents for Validation Methodology Implementation
| Reagent Solution | Function | Implementation Example |
|---|---|---|
| JSON Schema Validator | Validates JSON document structure against schema definitions | ajv (JavaScript), jsonschema (Python) [9] |
| Protocol Buffer Compiler | Generates data access classes from .proto definitions | protoc with language-specific plugins [36] |
| Avro Schema Validator | Validates binary Avro data against JSON-defined schemas | Apache Avro library for JVM/Python/C++ [34] |
| XML Schema Processor | Validates XML documents against W3C XSD schemas | Xerces (C++/Java), lxml (Python) |
| Data Type Enforcement Library | Runtime type checking for dynamic languages | Joi (JavaScript), Pydantic (Python) [9] |
Validation Workflow Architecture
The following diagram illustrates the complete validation workflow for scientific data processing, from input through transformation to output:
Scientific Data Validation Workflow
Error Handling and Quality Assurance
Robust error handling is essential for maintaining research data quality. Validation failures should be reported through standardized error systems with specific error codes [34]:
InvalidRecord: Message fails schema validationSchemaValidation: Generic validation failureProtobufJsonMapping: JSON-to-Protobuf conversion failsAvro: Avro schema or encoding error
Error responses should follow consistent formats that help researchers identify and resolve issues without exposing system internals [9]:
Quality assurance protocols for validation systems include:
- Schema Versioning: Track changes to validation rules over time
- Backward Compatibility Testing: Ensure new schemas don't break existing valid data
- Validation Test Coverage: Verify validation rules with comprehensive test suites
- Performance Monitoring: Track validation latency and failure rates
- Error Analytics: Categorize and analyze validation failures to improve data quality
Schema and metadata validation provides the critical foundation for ensuring structural consistency in scientific data systems. By implementing the methodologies and protocols outlined in this document, research organizations can establish robust frameworks for maintaining data quality throughout complex input-output transformation pipelines. The rigorous application of structural validation principles enables drug development professionals and researchers to trust their analytical outputs, supporting reproducible science and regulatory compliance while preventing data corruption and misinterpretation. As research data systems grow in complexity and scale, these validation methodologies will become increasingly essential components of the scientific computing infrastructure.
Unit and Integration Testing for Isolated and Combined Transformation Logic
In the pharmaceutical and medical device industries, the validation of input-output transformation logic is a critical pillar of quality assurance. This process ensures that every unit operation, whether examined in isolation or as part of an integrated system, consistently produces outputs that meet predetermined specifications and quality attributes. The methodology is foundational to demonstrating that manufacturing processes consistently deliver products that are safe, effective, and of high quality, thereby satisfying stringent regulatory requirements from bodies like the FDA and EMA [13] [37]. The approach is bifurcated: unit testing verifies the logic of individual components in isolation, while integration testing confirms that these components interact correctly to transform inputs into the desired final output [38] [39]. Adopting this structured, layered testing strategy is not merely a regulatory checkbox but a scientific imperative for building quality into products from the ground up [40].
Quantitative Comparison of Testing Methodologies
A clear understanding of the distinct yet complementary roles of unit and integration testing is essential for designing a robust validation strategy. The following table summarizes their key characteristics, providing a framework for their strategic application.
Table 1: Strategic Comparison of Unit and Integration Testing for Transformation Logic
| Characteristic | Unit Testing | Integration Testing |
|---|---|---|
| Scope & Objective | Individual components/functions in isolation; validates internal logic and algorithmic correctness [38] [41]. | Multiple connected components; validates data flow, interfaces, and collaborative behavior [42] [38]. |
| Dependencies | Uses mocked or stubbed dependencies to achieve complete isolation of the unit under test [38] [39]. | Uses actual dependencies (e.g., databases, APIs) or highly realistic simulations [38] [41]. |
| Primary Focus | Functional accuracy of a single unit, including edge cases and error handling [39]. | Interaction defects, data format mismatches, and communication failures between modules [43] [39]. |
| Execution Speed | Very fast (milliseconds per test), enabling a rapid developer feedback loop [39] [41]. | Slower (seconds to minutes) due to the overhead of coordinating multiple components and systems [38] [39]. |
| Error Detection | Catches logic errors, boundary value issues, and algorithmic flaws within a single component [39]. | Identifies interface incompatibilities, data corruption in flow, and misconfigured service connections [43] [38]. |
| Ideal Proportion in Test Suite | ~70% (Forms the broad base of the test pyramid) [41]. | ~20% (The supportive middle layer of the test pyramid) [41]. |
Experimental Protocols for Validation
This section delineates the detailed, actionable protocols for implementing unit and integration tests, providing a clear roadmap for researchers and validation scientists.
Protocol for Unit Testing
Objective: To verify the internal transformation logic of a single, isolated function or method, ensuring it produces the correct output for a given set of inputs, independent of any external systems [39].
Methodology: The unit testing protocol follows a precise, multi-stage process to ensure thoroughness and reliability.
Table 2: Unit Testing Protocol Steps and Requirements
| Step | Description | Requirements & Acceptance Criteria |
|---|---|---|
| 1. Test Identification | Identify the smallest testable unit (e.g., a pure function for dose calculation, a method for column clearance modeling) [39]. | A uniquely identified unit with defined input parameters and an expected output. |
| 2. Environment Setup | Create an isolated test environment. All external dependencies (database calls, API calls, file I/O) must be replaced with mocks or stubs [38] [39]. | A testing framework (e.g., pytest, JUnit) and mocking library (e.g., unittest.mock). Verification that no real external systems are called. |
| 3. Input Definition | Define test input data, including standard use cases, boundary values, and invalid inputs designed to trigger error conditions [42]. | Documented input sets covering valid and invalid ranges. Boundary values must include minimum, maximum, and just beyond these limits. |
| 4. Test Execution | Execute the unit with the predefined inputs. | The test harness runs the unit and captures the output. |
| 5. Output Validation | Compare the actual output against the pre-defined expected output [41]. | For valid inputs: actual output must exactly match expected output. For invalid inputs: the unit must throw the expected exception or error message. |
| 6. Result Documentation | Document the test results, including pass/fail status, any deviations, and the exact inputs/outputs involved. | A generated test report that provides documented evidence of the unit's behavior for regulatory scrutiny [44]. |
Example: A unit test for a function that calculates the percentage of protein monomer from chromatogram data would provide specific peak area inputs and assert that the output matches the expected percentage. All calls to the chromatogram data service would be mocked [41].
Protocol for Integration Testing
Objective: To verify that multiple, individually validated units work together correctly, ensuring the combined transformation logic and data flow across component interfaces function as intended [42] [43].
Methodology: Integration testing requires a controlled environment that mirrors the production system architecture to validate interactions realistically.
Table 3: Integration Testing Protocol Steps and Requirements
| Step | Description | Requirements & Acceptance Criteria |
|---|---|---|
| 1. Scope Definition | Define the integration scope by selecting the specific modules, services, or systems to be tested together (e.g., a bioreactor controller integrated with a temperature logging service) [42]. | A defined test scope document listing all components and their interfaces under test. |
| 2. Test Environment Construction | Construct a stable, production-like test environment. This includes access to real or realistically simulated databases, APIs, and network configurations [42] [43]. | An environment that mirrors production architecture. Entry criteria must be met, including completed unit tests and environment readiness [43]. |
| 3. Test Scenario Generation | Generate end-to-end test scenarios that reflect real-world business processes or scientific workflows [42]. | Scenarios that exercise the entire data flow between integrated components, including "happy paths" and error paths (e.g., sensor failure). |
| 4. Test Data Generation | Prepare and load test data that mimics real-world data, including valid and invalid datasets [42]. | Data that is representative of production data but isolated for testing purposes. Must be clearly documented and version-controlled. |
| 5. Test Execution & Monitoring | Execute the test scenarios and meticulously monitor the interactions, data flow, and system responses [42]. | Monitoring tools to track API calls, database transactions, and message queues. Logs must be detailed for debugging purposes. |
| 6. Result Analysis & Defect Reporting | Analyze results to identify interface mismatches, data corruption, or timing issues. Report all defects with high fidelity [42]. | A documented report of all failures, traced back to the specific interface or component interaction that caused the issue. |
| 7. Exit Criteria Verification | Verify that all critical integration paths have been tested, all critical defects resolved, and coverage metrics achieved before proceeding to system-level testing [43]. | Formal sign-off based on pre-defined exit criteria, confirming the integrated system is ready for the next validation stage [43]. |
Example: An integration test for a drug substance purification process would involve the sequential interaction of the harvest, purification, and bulk fill modules. The test would verify that the output (drug substance) from one module correctly serves as the input to the next, and that critical quality attributes (CQAs) are maintained throughout the data flow [37].
Visualization of Testing Workflows
The following diagrams illustrate the logical relationships and workflows for the unit and integration testing strategies described in the protocols.
Unit Testing Isolation Logic
Integration Testing Data Flow
The Testing Pyramid Strategy
The Scientist's Toolkit: Research Reagent Solutions
This section catalogs the essential tools, frameworks, and materials required to effectively implement the described validation protocols for transformation logic.
Table 4: Essential Research Reagent Solutions for Test Implementation
| Tool/Reagent | Category | Primary Function in Validation |
|---|---|---|
| pytest / JUnit | Unit Testing Framework | Provides the structure and runner for organizing and executing isolated unit tests. Offers assertions, fixtures, and parameterization [42] [41]. |
| Postman / SoapUI | API Testing Tool | Enables the design, execution, and automation of tests for RESTful and SOAP APIs, which are critical for integration testing between services [42] [38]. |
| TestContainers | Integration Testing Library | Allows for lightweight, disposable instances of real dependencies (e.g., databases, message brokers) to be run in Docker containers, making integration tests more realistic and reliable [41]. |
| Selenium / Playwright | End-to-End Testing Framework | Automates user interactions with a web-based UI, validating complete workflows from the user's perspective, which often relies on underlying integration points [42] [41]. |
| Mocking Library | Test Double Framework | Isolates the unit under test by replacing complex, slow, or non-deterministic dependencies (e.g., databases, APIs) with simulated objects that return predefined responses [39]. |
| Validation Master Plan (VMP) | Documentation | A top-level document that outlines the entire validation strategy for a project or system, defining policies, protocols, and responsibilities [44] [40]. |
| IQ/OQ/PQ Protocol | Qualification Framework | A structured approach for equipment and system validation in regulated environments. Installation (IQ) and Operational (OQ) Qualification are forms of integration testing, while Performance Qualification (PQ) validates overall output [13] [44]. |
Statistical Validation and Cross-Verification Techniques
Statistical validation and cross-verification techniques form the cornerstone of robust scientific research and development, particularly within the highly regulated pharmaceutical industry. These methodologies provide the critical framework for ensuring that analytical methods, computational models, and manufacturing processes consistently produce reliable, accurate, and reproducible results. The fundamental principle underpinning these techniques is the rigorous assessment of input-output transformations, where raw data or materials are systematically converted into meaningful information or qualified products. Within the context of drug development, statistical validation transcends mere regulatory compliance, emerging as a strategic asset that accelerates time-to-market, enhances product quality, and mitigates risks across the product lifecycle [45].
The current regulatory landscape, governed by guidelines such as ICH Q2(R1) and the forthcoming ICH Q2(R2) and Q14, emphasizes a lifecycle approach to analytical procedures [45]. This paradigm shift moves beyond one-time validation events toward continuous verification, leveraging advanced statistical tools and real-time monitoring to maintain a state of control. Furthermore, the increasing complexity of novel therapeutic modalities—including biologics, cell therapies, and personalized medicines—demands more sophisticated validation approaches capable of handling multi-dimensional data streams and ensuring product consistency and patient safety [45] [46].
Statistical cross-verification, particularly through methodologies like cross validation, addresses the critical need for method transfer and data comparability across multiple laboratories or computational environments. As demonstrated in recent research, refined statistical assessment frameworks for cross validation significantly enhance the integrity and comparability of pharmacokinetic data in clinical trials, directly impacting the reliability of trial endpoints and subsequent regulatory decisions [47]. This document provides comprehensive application notes and detailed experimental protocols to guide researchers, scientists, and drug development professionals in implementing these vital statistical techniques within their input-output transformation validation activities.
The quantitative assessment of validation methodologies relies on specific performance metrics that gauge accuracy, precision, and robustness. The following tables summarize key statistical parameters and comparative performance data essential for evaluating validation and cross-verification techniques.
Table 1: Key Statistical Parameters for Method Validation
| Parameter | Definition | Typical Acceptance Criteria | Assessment Method |
|---|---|---|---|
| Accuracy | Closeness of agreement between measured and true value | Recovery of 98-102% | Comparison against reference standard or spike recovery [45] |
| Precision | Closeness of agreement between a series of measurements | RSD ≤ 2% for repeatability; RSD ≤ 3% for intermediate precision | Repeated measurements of homogeneous sample [45] |
| Specificity | Ability to assess analyte unequivocally in presence of components | No interference observed | Analysis of samples with and without potential interferents [45] |
| Linearity | Ability to obtain results proportional to analyte concentration | R² ≥ 0.990 | Calibration curve across specified range [45] |
| Range | Interval between upper and lower analyte concentrations | Meets linearity, accuracy, and precision criteria | Verified by testing samples across the claimed range [45] |
| Robustness | Capacity to remain unaffected by small, deliberate variations | System suitability parameters met | Deliberate variation of method parameters (e.g., temperature, pH) [45] |
Table 2: Comparative Performance of Cross-Validation Statistical Tools
| Statistical Tool | Primary Function | Key Output Metrics | Application Context | Reported Performance/Outcome |
|---|---|---|---|---|
| Bland-Altman Plot with Equivalence Testing [47] | Assess agreement between two analytical methods | Mean difference (bias); 95% Limits of Agreement (LoA) | Cross-lab method transfer | Provides consistent, credible outcomes in real-world scenarios by accommodating practical assay variability [47] |
| Deming Regression [47] | Model relationship between two methods with measurement error | Slope; Intercept; Standard Error | Comparing new method vs. reference standard | Recognized limitations for interpreting cross-validation results alone [47] |
| Lin's Concordance [47] | Measure of agreement and precision | Concordance Correlation Coefficient (ρc) | Method comparison studies | Recognized limitations for interpreting cross-validation results alone [47] |
| Attentional Factorization Machines (AFM) [48] | Model complex feature interactions in prediction models | AUC (Area Under ROC Curve); AUPR (Area Under Precision-Recall Curve) | Drug repositioning predictions | AUC > 0.95; AUPR > 0.96; superior stability with low coefficient of variation [48] |
Experimental Protocols
Protocol 1: Cross-Laboratory Analytical Method Validation
This protocol outlines a standardized procedure for validating an analytical method across multiple laboratories, utilizing a combined Bland-Altman and equivalence testing approach to ensure data comparability and integrity [47].
Scope and Application
This protocol applies to the cross-validation of bioanalytical methods (e.g., HPLC, LC-MS/MS) used for quantifying drug substances or biomarkers in clinical trial samples when methods are transferred between primary and secondary testing sites.
Pre-Validation Requirements
- Method Documentation: The originating laboratory must provide a fully validated method package, including standard operating procedures (SOPs), validation report, and known limitations.
- Reagent and Standard Alignment: All participating laboratories must use the same lot of critical reagents, reference standards, and consumables to minimize inter-lab variability.
- Instrument Qualification: All instruments used in the study must have current Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ) records.
- Analyst Training: Analysts at the receiving laboratory must demonstrate proficiency with the method by successfully analyzing a predefined set of quality control (QC) samples prior to the formal cross-validation study.
Experimental Procedure
Sample Preparation:
- Prepare a minimum of 15 independent samples for each QC level (Low, Medium, High). The samples should be blinded to the analysts.
- The matrix of the samples should be identical to the intended study samples (e.g., human plasma, serum).
- Samples are split and distributed to both Laboratory A (originating) and Laboratory B (receiving).
Sample Analysis:
- Both laboratories analyze the entire set of blinded samples in a single batch within their respective validated environments.
- The analytical run must include appropriate system suitability tests and calibration standards as per the method SOP.
Data Collection:
- Record the measured concentration for each sample from both laboratories.
- Data should be recorded in a structured format (e.g., CSV) indicating Sample ID, Laboratory, Nominal Concentration, and Measured Concentration.
Statistical Analysis and Acceptance Criteria
Bland-Altman Analysis:
- Calculate the differences between measurements (Lab B - Lab A) for each sample pair.
- Calculate the mean difference (bias) and the 95% Limits of Agreement (LoA = mean difference ± 1.96 * SD of the differences).
- Plot the differences against the average of the two measurements for each sample.
Equivalence Testing:
- Log10-transform the measured concentrations from both laboratories to stabilize variance.
- Calculate the mean log10 difference (bias) and its 95% confidence interval (CI).
- Acceptance Criterion: The 95% CI of the mean log10 difference must fall entirely within pre-defined equivalence boundaries (e.g., ± 0.04 log10 units, derived from method validation criteria for accuracy) [47].
Protocol 2: Validation of AI/ML-Based Predictive Models for Drug Repositioning
This protocol describes the statistical validation of a deep learning model, such as the Unified Knowledge-Enhanced deep learning framework for Drug Repositioning (UKEDR), designed to predict novel drug-disease associations [48].
Scope and Application
This protocol is for validating computational models that leverage knowledge graphs and machine learning to transform input biological data (e.g., molecular structures, disease semantics) into output predictions of therapeutic utility.
Model and Data Preparation
- Model Architecture: Specify the model configuration, including the knowledge graph embedding method (e.g., PairRE), the recommendation system (e.g., Attentional Factorization Machines - AFM), and pre-training strategies for drugs and diseases [48].
- Datasets: Use standardized benchmark datasets such as RepoAPP for evaluation. Data must be partitioned into training, validation, and hold-out test sets strictly to prevent data leakage.
- Evaluation Metrics: Define primary (e.g., AUC, AUPR) and secondary (e.g., F1-Score, Precision@K) metrics prior to validation.
Experimental Procedure for Performance Evaluation
Standard Performance Validation:
- Train the model on the training set.
- Tune hyperparameters using the validation set.
- Evaluate the final model on the hold-out test set to calculate AUC and AUPR.
- Performance Benchmark: Compare results against classical ML (e.g., Random Forest), network-based (e.g., NBI), and other deep learning baselines (e.g., KGCNH) [48].
Cold-Start Scenario Validation:
- Simulation: Create a test set containing drugs or diseases that are completely absent from the knowledge graph used for training.
- Procedure: Leverage the model's pre-trained attribute representations (e.g., DisBERT for diseases, CReSS for drugs) to generate features for these unseen entities.
- Evaluation: Assess the model's prediction performance (AUC) on this cold-start test set. The model should demonstrate a significant performance advantage (e.g., 39.3% improvement in AUC) over models incapable of handling cold starts [48].
Robustness Validation on Imbalanced Data:
- Artificially unbalance the training data to reflect real-world sparsity of known drug-disease associations.
- Monitor the model's performance on a balanced test set, paying particular attention to metrics like AUPR that are sensitive to class imbalance.
Acceptance Criteria
- The model must demonstrate statistically superior performance (p < 0.05) in AUC and AUPR compared to established baseline methods on standard benchmarks.
- In cold-start scenarios, the model must maintain predictive capability, with a predefined minimum performance threshold (e.g., AUC > 0.80) to be considered valid for real-world application.
Visualization of Workflows
The following diagrams, generated using Graphviz DOT language, illustrate the core logical workflows and signaling pathways described in the application notes and protocols.
Cross-Lab Method Validation Workflow
This diagram outlines the step-by-step procedure for Protocol 1, from sample preparation to statistical assessment and the final acceptance decision.
AI Model Validation Pathway
This diagram depicts the multi-faceted validation pathway for AI/ML models as detailed in Protocol 2, covering standard, cold-start, and robustness testing.
The Scientist's Toolkit: Research Reagent Solutions
The successful implementation of statistical validation and cross-verification protocols depends on the use of specific, high-quality reagents and materials. The following table details essential solutions for the experiments cited in this document.
Table 3: Essential Research Reagents and Materials for Validation Studies
| Item Name | Function/Application | Critical Specifications | Validation Context |
|---|---|---|---|
| Certified Reference Standard | Serves as the primary benchmark for quantifying the analyte of interest. | Purity ≥ 98.5%; Certificate of Analysis (CoA) from qualified supplier (e.g., USP, EP). | Method Validation & Cross-Lab Transfer [45] [47] |
| Stable Isotope-Labeled Internal Standard (SIL-IS) | Corrects for variability in sample preparation and ionization efficiency in mass spectrometry. | Isotopic purity ≥ 95%; Chemically identical to analyte; CoA available. | Bioanalytical Method Cross-Validation (LC-MS/MS) [47] |
| Matrix-Free (Surrogate) Blank | Used for preparing calibration standards and validating assay specificity. | Confirmed absence of analyte and potential interferents. | Specificity & Selectivity Testing [45] |
| Quality Control (QC) Materials | Used to monitor the accuracy and precision of the analytical run. | Prepared at Low, Mid, and High concentrations in biological matrix; Pre-assigned target values. | Cross-Lab Validation & Continued Verification [45] [47] |
| Structured Biomedical Knowledge Graph | Provides the relational data (drugs, targets, diseases) for AI model training and validation. | Comprehensiveness (e.g., RepoAPP); Data provenance; Standardized identifiers (e.g., InChI, MeSH). | AI/ML Model Validation for Drug Repositioning [48] |
| Pre-Trained Language Model (e.g., DisBERT) | Generates intrinsic attribute representations for diseases from textual descriptions. | Domain-specific fine-tuning (e.g., on 400,000+ disease texts); High semantic capture capability. | Handling Cold-Start Scenarios in AI Models [48] |
| Molecular Representation Model (e.g., CReSS) | Generates intrinsic attribute representations for drugs from structural data (e.g., SMILES). | Capable of contrastive learning from SMILES and spectral data. | Handling Cold-Start Scenarios in AI Models [48] |
Golden Dataset and Ground Truth Validation for Benchmarking
In the methodological framework of input-output transformation validation, golden datasets and ground truth validation serve as the foundational reference point for evaluating the performance, reliability, and accuracy of computational models, including those used in AI and biotechnology [49] [50]. A golden dataset is a curated, high-quality collection of data that has been meticulously validated by human experts to represent the expected, correct outcome for a given task. This dataset acts as the "north star" or benchmark against which a model's predictions are compared [50]. The closely related concept of ground truth data encompasses not just the dataset itself, but the broader definition of correctness, including verified labels, decision rules, scoring guides, and acceptance criteria that collectively define successful task completion for a system [49]. In essence, ground truth is the definitive, accurate interpretation of a task, based on domain knowledge and verified context [49]. In scientific research, particularly in computational biology, the traditional concept of "experimental validation" is being re-evaluated, with a shift towards viewing orthogonal experimental methods as a form of "corroboration" or "calibration" that increases confidence in computational findings, rather than serving as an absolute validator [51].
Core Characteristics and Importance
Defining Characteristics of a High-Quality Golden Dataset
For a golden dataset to effectively serve as a benchmark, it must possess several key characteristics [50]:
- Accuracy: The data must be obtained from qualified sources and be free from errors, inconsistencies, and inaccuracies.
- Completeness: It must cover all aspects of the real-world phenomenon the model intends to capture, including edge cases, with sufficient examples for effective evaluation.
- Consistency: The data should be organized in a uniform format and structure, with standardized labels to avoid ambiguities.
- Bias-free: The dataset should represent a diverse range of perspectives and avoid biases that could negatively impact the model's performance.
- Timely: The data must be up-to-date and relevant to the domain's current state, requiring regular updates to reflect real-world changes.
The Role of Golden Datasets in Validation Research
Golden datasets are indispensable for the rigorous evaluation of computational models, especially fine-tuned large language models (LLMs) and AI agents deployed in sensitive domains like drug development [50] [52]. Their primary roles include:
- Establishing a Performance Baseline: They provide a solid foundation for measuring model performance. By comparing a model's output to the human-verified ground truth, researchers can quantitatively assess accuracy, coherence, and relevance [50].
- Identifying Biases and Limitations: Evaluation against a golden dataset helps uncover discrepancies, revealing underlying biases and limitations in the model. This information is critical for making iterative improvements [50].
- Ensuring Domain-Specific Task Performance: They are crucial for evaluating models tailored to specific scientific domains (e.g., healthcare, toxicology, biomarker discovery) or tasks (e.g., medical diagnosis, protein folding prediction). Subject matter experts (SMEs) are often involved in annotating these datasets to ensure they reflect the necessary nuances [50].
- Enabling Trust and Reproducibility: A well-constructed golden dataset acts as institutional memory, preserving consistency across research teams and over time. It prevents "model drift by optimism" and ensures that performance gains are genuine and reproducible [49] [50].
Table 1: Characteristics of a High-Quality Golden Dataset
| Characteristic | Description | Impact on Model Evaluation |
|---|---|---|
| Accuracy | Free from errors and inconsistencies, sourced from qualified experts. | Ensures models are learning correct patterns, not noise. |
| Completeness | Covers core scenarios and edge cases relevant to the domain. | Provides a comprehensive test, revealing model weaknesses. |
| Consistency | Uniform format and standardized labeling. | Enables fair, reproducible comparisons between model versions. |
| Bias-free | Represents diverse perspectives and demographic groups. | Helps identify and mitigate algorithmic bias, promoting fairness. |
| Timely | Updated regularly to reflect current domain knowledge. | Ensures the model remains relevant and effective in a changing environment. |
Protocol for Golden Dataset Creation
Creating a high-quality golden dataset is a resource-intensive process that requires careful planning and execution. The following protocol outlines the key steps.
Step 1: Goal Identification and Scoping
Objective: Define the specific purpose and scope of the golden dataset. Methodology:
- Clearly articulate the primary objective of the model being evaluated (e.g., "to accurately identify drug-protein interactions from scientific literature").
- Define the specific tasks the golden dataset will be used to benchmark.
- Establish the criteria for success and the key performance indicators (KPIs) that will be measured [50].
Step 2: Data Collection and Sourcing
Objective: Gather a diverse and representative pool of raw data. Methodology:
- Identify Sources: Collect data from relevant sources, which may include public datasets (e.g., from government agencies or research institutions), proprietary data, and real user data [50] [53].
- Ensure Representativeness: The collected data must cover multiple scenarios, perspectives, and edge cases. The dataset should have a balanced distribution of different classes or categories to avoid skewing the model's learning [50].
- Determine Volume: The number of examples required depends on the task's complexity, the desired level of accuracy, and the quality of the available data. High-quality, clean data can sometimes reduce the required dataset size [50].
Step 3: Data Preparation and Annotation
Objective: Transform raw data into a clean, structured, and labeled format. Methodology:
- Data Cleaning: Clean the dataset to remove noise, inconsistencies, and errors. Normalize the data into a uniform and consistent format, such as JSON or CSV [50].
- Develop Annotation Guidelines: Create clear, detailed guidelines for human annotators to ensure consistency and minimize ambiguity throughout the labeling process [50] [54].
- Leverage Human Expertise: Engage a team of human annotators, ideally with domain expertise (SMEs), to label the data accurately. SMEs can interpret ambiguous data points and handle complex, domain-specific concepts [50]. For example, in a biomedical context, this could involve radiologists labeling medical images or bioinformaticians annotating genomic sequences.
Step 4: Validation and Quality Control
Objective: Ensure the annotated dataset meets the highest standards of quality. Methodology:
- Implement Quality Control Procedures: This includes cross-validation (e.g., having multiple annotators label the same data to measure inter-annotator agreement), involving external experts for audit, and using statistical methods to review annotations [50].
- Audit for Fairness and Bias: Apply fairness metrics to assess the dataset's performance across different demographic groups and identify potential biases [50].
- Human-in-the-Loop (HITL) Review: Institute a HITL process where SMEs review a sample of the generated ground truth, especially for high-risk or critical applications. The level of review is determined by the potential impact of incorrect ground truth [54].
Step 5: Maintenance and Iteration
Objective: Treat the golden dataset as a living document that evolves. Methodology:
- Regular Revision: Continuously refine and update the dataset to ensure it remains relevant as models evolve and new scientific insights emerge [50].
- Incorporate Production Feedback: Sample model outputs from real-world use (production data) and score them using the same evaluation framework. New failure modes should be fed back into the golden dataset to create a continuous feedback loop: data → model → evaluation → data [49].
Experimental Protocols for Validation
Protocol A: Building a Ground Truth Pipeline for Question-Answering
This protocol is adapted for evaluating generative AI models, such as those used in retrieving scientific literature or clinical data.
1. Application: Validating the output of a Retrieval Augmented Generation (RAG) system or a question-answering assistant for technical or scientific domains [54].
2. Experimental Steps:
- Step 1: Create High-Quality Supervised Fine-Tuning (SFT) Data.
- Begin with a small set of domain-representative prompts and ideal responses, written with real context (e.g., policy references, scientific nuances).
- Each example should encode clear reasoning and be reviewed by experts to turn a text corpus into true ground truth [49].
- Step 2: Assemble Question-Answer-Fact Triplets.
- For each piece of source data (e.g., a chunk of a scientific document), generate a
(question, ground_truth_answer, fact)triplet. - The "fact" is a minimal representation of the ground truth answer, comprising one or more subject entities of the question. This structure is crucial for deterministic evaluation [54].
- For each piece of source data (e.g., a chunk of a scientific document), generate a
- Step 3: Scale Generation with an LLM Pipeline.
- Use a structured prompt with an LLM (e.g., Anthropic's Claude, GPT-4) to generate the triplets from source data chunks automatically.
- The prompt should assign a persona to the LLM and instruct it to use a fact-based, chain-of-thought approach to interpret the source chunk and generate relevant questions and answers [54].
- Step 4: Implement a Serverless Batch Pipeline.
- Automate the process using a pipeline architecture (e.g., with AWS Step Functions and Lambda).
- The pipeline ingests source data from cloud storage, chunks it, processes each chunk through the LLM to generate JSONLines records of triplets, and finally aggregates them into a single golden dataset output file [54].
- Step 5: Human-in-the-Loop (HITL) Review.
- Flag a randomly selected percentage of the generated records for review by SMEs.
- SMEs verify that critical business or scientific logic is correctly represented, providing the final stamp of approval [54].
Protocol B: Benchmarking AI Agents with a Golden Dataset
This protocol is for evaluating the performance of autonomous or semi-autonomous AI agents, which are increasingly used in research simulation and data analysis workflows.
1. Application: Evaluating AI agents on tasks such as tool use, reasoning, planning, and task completion in dynamic environments [52].
2. Experimental Steps:
- Step 1: Define the Evaluation Objectives.
- Agent Behavior (Black-Box): Focus on outcome-oriented aspects like task completion rate (e.g., Success Rate - SR) and output quality (e.g., accuracy, relevance) as perceived by the end-user [52].
- Agent Capabilities (White-Box): Focus on process-oriented competencies like tool use, planning and reasoning, memory, and multi-agent collaboration [52].
- Step 2: Construct a Task-Specific Evaluation Set.
- Build a golden dataset that mirrors real-world goals, covering both routine and high-risk edge cases. This dataset acts as a private evaluation set, distinct from public benchmarks [49].
- Use stratified sampling to balance easy and hard samples, preventing inflated metrics or obscured improvement [49].
- Step 3: Employ LLM-as-a-Judge with Calibration.
- Use an LLM to evaluate the agent's outputs at scale. However, the LLM judge must be calibrated against human judgment to ensure alignment.
- Start with a human-reviewed benchmark where experts have scored responses using clear rubrics. Run the LLM judge on the same set and measure agreement. If below 80-85%, refine the evaluation prompts [49].
- Step 4: Execute Benchmarking and Analyze Results.
- Run the agent through the golden dataset of tasks.
- Calculate key metrics (see Table 2) and compare them against the established ground truth to identify strengths and failure modes.
Table 2: Key Metrics for Benchmarking AI Agents against Golden Datasets
| Metric Category | Specific Metric | Description | How it's Measured |
|---|---|---|---|
| Task Completion | Success Rate (SR) / Pass Rate | Measures whether the agent successfully achieves the predefined goal. | Binary (1/0) or average over multiple trials (pass@k) [52]. |
| Output Quality | Factual Accuracy, Relevance, Coherence | Assesses the quality of the agent's final response. | Comparison to ground truth answer using quantitative scores or qualitative LLM/Human judgment [52]. |
| Capabilities | Tool Use Accuracy, Reasoning Depth | Evaluates the correctness of the process and use of external tools. | Analysis of the agent's intermediate steps and reasoning chain against an expected process [52]. |
| Reliability & Safety | Robustness, Fairness, Toxicity | Measures consistency and ethical alignment of the agent. | Testing with adversarial inputs and checking for biased or harmful outputs against safety guidelines [55] [52]. |
The Scientist's Toolkit: Research Reagent Solutions
The following table details key resources and tools used in the creation and validation of golden datasets.
Table 3: Essential Research Reagents and Tools for Golden Dataset Creation
| Tool / Resource | Category | Function in Golden Dataset Creation |
|---|---|---|
| Subject Matter Experts (SMEs) | Human Resource | Provide domain-specific knowledge for accurate data annotation, validation, and review of edge cases [50] [54]. |
| LLM Judges (e.g., GPT-4, Claude) | Software Tool | Automate the large-scale evaluation of model outputs against ground truth; must be calibrated with human judgment [49] [56]. |
| Data Annotation Platforms (e.g., SuperAnnotate) | Software Platform | Provide specialized environments for designing labeling interfaces, managing annotators, and ensuring quality control during dataset creation [49]. |
| Evaluation Suites (e.g., FMEval) | Software Library | Offer standardized implementations of evaluation metrics (e.g., factual accuracy) to systematically measure performance against the golden dataset [54]. |
| Benchmarking Suites (e.g., AgentBench, WebArena) | Software Framework | Provide pre-built environments and tasks for systematically evaluating specific model capabilities, such as AI agent tool use and reasoning [57] [52]. |
| Step Functions / Pipeline Orchestrators | Infrastructure | Automate and scale the end-to-end ground truth generation process, from data ingestion and chunking to LLM processing and aggregation [54]. |
Validation Framework and Metrics Interpretation
A robust validation framework integrates the golden dataset into a continuous cycle of model assessment and improvement. The diagram below illustrates this ecosystem and the relationships between its core components.
Interpreting Validation Outcomes:
- High Performance on Golden Dataset: Indicates the model has learned the desired patterns and performs well on the curated test cases. It is a necessary but not sufficient condition for real-world deployment.
- Performance Gaps and Failure Modes: Discrepancies between model output and ground truth are not failures of the evaluation, but successes of the methodology. They precisely identify areas for model improvement, data augmentation, or potential bias in the dataset itself.
- The Role of Production Feedback: The ultimate test of a model is its performance on real, unseen user data. Continuously sampling and scoring production outputs and feeding them back into the golden dataset is what transforms a static benchmark into a dynamic, evolving system that ensures long-term model reliability and relevance [49]. This closed-loop validation is the cornerstone of a mature input-output transformation research pipeline.
End-to-End Testing in Staging Environments with Production-like Data
End-to-end (E2E) testing is a critical software testing methodology that validates an application's complete workflow from start to finish, replicating real user scenarios to verify system integration and data integrity [58]. Within the context of input-output transformation validation methods research, E2E testing in staging environments serves as the ultimate validation layer, ensuring that all system components—from front-end interfaces to backend services and databases—interact correctly to transform user inputs into expected outputs [59] [60]. This holistic approach is particularly crucial for drug development applications where accurate data processing and system reliability directly impact research outcomes and patient safety.
Staging environments provide the foundational infrastructure for meaningful E2E testing by replicating production systems in a controlled setting [61]. These environments enable researchers to validate complete scientific workflows, data processing pipelines, and system integrations before deployment to live production environments. The precision of these testing environments directly correlates with the validity of the test results, making environment parity a critical consideration for research and drug development professionals [59].
Staging Environment Architecture for Validation Research
Core Environmental Requirements
A staging environment must be a near-perfect replica of the production environment to serve as a valid platform for input-output transformation research [61]. The environment requires careful configuration across multiple dimensions to ensure testing accuracy.
Table: Staging Environment Parity Specifications
| Component | Production Parity Requirement | Research Validation Purpose |
|---|---|---|
| Infrastructure | Matching hardware, OS, and resource allocation [61] | Eliminates infrastructure-induced variability in test results |
| Data Architecture | Realistic or sanitized production data snapshots [61] | Ensures data processing transformations mirror real-world behavior |
| Network Configuration | Replicated load balancers, CDNs, and service integrations [61] | Validates performance under realistic network conditions |
| Security & Access Controls | Mirror production security policies and IAM configurations [61] | Tests authentication and authorization flows without exposing real systems |
Data Management Protocols
Test data management presents significant challenges for E2E testing, particularly in research contexts where data integrity is paramount [59]. Effective strategies include:
- Production Data Snapshots: Utilizing anonymized or masked production data that maintains statistical properties while protecting sensitive information [61]
- Synthetic Data Generation: Creating programmatically generated datasets that mimic production data characteristics when real data cannot be used
- Test Data Isolation: Implementing isolated data stores for different testing activities to prevent cross-contamination of results [59]
- Automated Data Refresh: Establishing regular data synchronization schedules to prevent environmental drift [61]
E2E Testing Framework and Methodologies
Test Design and Planning
E2E testing design follows a structured approach to ensure comprehensive validation coverage [60] [58]. The process begins with requirement analysis and proceeds through test execution and closure phases.
E2E Testing Methodology Workflow
Test Validation Metrics
Quantitative metrics are essential for assessing E2E testing effectiveness and tracking validation progress throughout the research lifecycle [60] [58].
Table: E2E Testing Validation Metrics
| Metric Category | Measurement Parameters | Research Application |
|---|---|---|
| Test Coverage | Percentage of critical user journeys validated; requirements coverage [60] | Ensures comprehensive validation of scientific workflows |
| Test Progress | Test cases executed vs. planned; weekly completion rates [60] [58] | Tracks research validation timeline adherence |
| Defect Analysis | Defects identified/closed; severity distribution; fix verification rates [60] | Quantifies system stability and issue resolution effectiveness |
| Environment Reliability | Scheduled vs. actual availability; setup/teardown efficiency [60] | Measures infrastructure stability for consistent testing |
Experimental Protocols for Input-Output Transformation Validation
Core Validation Protocol
The following protocol provides a systematic methodology for validating input-output transformations through E2E testing in staging environments.
Input-Output Validation Protocol
Protocol Steps:
- Input Parameter Definition: Establish baseline input conditions, including data formats, value ranges, and boundary conditions based on production usage patterns [9]
- Test Scenario Execution: Implement automated test execution through frameworks such as Selenium, Cypress, or Playwright to ensure consistent, repeatable testing conditions [59]
- Output Capture Mechanism: Deploy monitoring tools to capture system outputs, including data transformations, API responses, database changes, and user interface states
- Expected vs. Actual Validation: Compare captured outputs against predefined expected results using schema validation, data comparison tools, and statistical analysis methods [9]
- Transformation Analysis: Trace data flow through system components to identify transformation points where discrepancies may occur
- Variance Documentation: Record all deviations from expected outcomes with sufficient context to support root cause analysis
- Validation Model Update: Refine validation criteria and testing methodologies based on variance analysis to improve future testing accuracy
The Researcher's Toolkit: Essential Testing Solutions
Table: E2E Testing Research Reagent Solutions
| Tool Category | Specific Solutions | Research Application |
|---|---|---|
| Test Automation Frameworks | Selenium, Cypress, Playwright, Gauge [59] [60] | Automated execution of user interactions and workflow validation |
| Environment Management | Docker, Kubernetes, Northflank, Bunnyshell [59] [61] | Containerized, consistent environment replication and management |
| Data Validation Tools | JSON Schema, Pydantic, Joi [9] | Structural validation of data formats and content integrity |
| Performance Monitoring | Application Performance Monitoring (APM) tools, custom metrics collectors | Response time measurement and system behavior under load |
| Visual Testing Tools | Percy, Applitools, Screenshot comparisons | UI/UX consistency validation across platforms and devices |
Advanced Implementation: Staging Environment Architecture
Modern staging environments leverage cloud-native technologies to achieve high-fidelity production replication while maintaining cost efficiency [61].
Staging Environment Architecture
Environment Synchronization Protocol
Maintaining parity between staging and production environments requires systematic synchronization:
- Infrastructure as Code (IaC): Define all environment specifications in code to ensure consistent, repeatable deployments [61]
- Automated Provisioning: Implement automated pipelines for environment creation and destruction to ensure fresh, consistent testing conditions [59]
- Data Synchronization: Establish secure processes for refreshing staging data with recent production snapshots, applying appropriate anonymization where necessary [61]
- Configuration Management: Version control all environment configurations and synchronize changes between production and staging environments
- Monitoring Implementation: Deploy identical monitoring, logging, and observability tools in both environments to enable accurate comparison [61]
Validation and Uncertainty Quantification
In precision research applications, particularly those involving clinical or drug development contexts, formal Verification, Validation, and Uncertainty Quantification (VVUQ) processes are essential for establishing trust in digital systems and their outputs [62].
VVUQ Framework Implementation
- Verification: Ensure that software implementations correctly solve their intended mathematical models through code solution verification and software quality engineering practices [62]
- Validation: Test models for applicability to specific scenarios and use cases, understanding where predictions can be trusted through continuous validation as systems evolve [62]
- Uncertainty Quantification: formally track uncertainties throughout model calibration, simulation, and prediction, identifying both epistemic (incomplete knowledge) and aleatoric (natural variability) uncertainties [62]
For research applications, documenting the VVUQ process provides critical context for interpreting E2E testing results and understanding system limitations, particularly when research outcomes inform clinical or regulatory decisions [62].
Beyond Basics: Advanced Strategies for Error Detection and Process Improvement
Within the framework of input-output transformation validation methods research, quantifying the discrepancy between predicted and observed values is a fundamental activity. This process of error rate analysis is critical for evaluating model performance, ensuring reliability, and supporting regulatory decision-making. In scientific and industrial contexts, such as drug development, accurate validation is indispensable for assessing the safety, effectiveness, and quality of new products [17]. This document provides detailed application notes and protocols for calculating and interpreting three key error metrics—Mean Absolute Error (MAE), Root Mean Square Error (RMSE), and Mean Absolute Percentage Error (MAPE)—to standardize and enhance validation practices for researchers and scientists.
Theoretical Foundation of Error Metrics
The choice of an error metric is not arbitrary but is rooted in statistical theory concerning the distribution of errors. The fundamental justification for these metrics stems from maximum likelihood estimation (MLE), which seeks the model parameters that are most likely to have generated the observed data [63].
- RMSE and Normal Errors: The Root Mean Square Error (RMSE) is derived from the L2 norm (Euclidean distance) and is optimal when model errors are independent and identically distributed (iid) and follow a normal (Gaussian) distribution. For normal errors, the model that minimizes the RMSE is the most likely model [63].
- MAE and Laplacian Errors: The Mean Absolute Error (MAE) is derived from the L1 norm (Manhattan distance) and is optimal when errors follow a Laplacian distribution. This distribution is characterized by stronger peakness around the mean (positive kurtosis) and is often encountered with variables that are approximately exponential, such as daily precipitation or certain biological processes [63].
- MAPE for Relative Error: The Mean Absolute Percentage Error (MAPE) provides a scale-independent measure by expressing the error as a percentage. This makes it useful for understanding the relative size of errors across different datasets or units of measurement [64].
Presenting multiple metrics, such as both RMSE and MAE, is a common practice that allows researchers to understand different facets of model performance. However, this should not be a substitute for selecting a primary metric based on the expected error distribution for a specific application [63].
Metric Definitions and Quantitative Comparison
The following table summarizes the core definitions, properties, and ideal use cases for each key metric.
Table 1: Comparison of Key Error Metrics for Model Validation
| Metric | Mathematical Formula | Units | Sensitivity to Outliers | Primary Use Case / Justification | ||
|---|---|---|---|---|---|---|
| Mean Absolute Error (MAE) | ( \text{MAE} = \frac{1}{n}\sum_{i=1}^{n} | yi - \hat{y}i | ) | Same as the dependent variable | Robust (low sensitivity) [64] | Optimal for Laplacian error distributions; when all errors should be weighted equally [63]. |
| Root Mean Square Error (RMSE) | ( \text{RMSE} = \sqrt{\frac{1}{n}\sum{i=1}^{n} (yi - \hat{y}_i)^2 } ) | Same as the dependent variable | High sensitivity [65] | Optimal for normal (Gaussian) error distributions; when large errors are particularly undesirable [63]. | ||
| Mean Absolute Percentage Error (MAPE) | ( \text{MAPE} = \frac{100\%}{n}\sum_{i=1}^{n} \left | \frac{yi - \hat{y}i}{y_i} \right | ) | Percentage (%) | Affected, but provides context | Understanding error relative to the actual value; communicating results in an intuitive, scale-free percentage [64]. |
Workflow for Error Rate Analysis
The following diagram illustrates the logical workflow for selecting, calculating, and interpreting error metrics within an input-output validation study.
Diagram 1: Workflow for error metric selection and calculation in model validation.
Experimental Protocols for Error Calculation
This section provides a detailed, step-by-step methodology for calculating error rates, using a hypothetical dataset for clarity. The example is inspired by a retail sales scenario but is directly analogous to experimental data, such as predicted versus observed compound potency in drug screening [66].
Example Dataset
Table 2: Sample Observational Data for Error Calculation
| Observation (i) | Actual Value (yᵢ) | Predicted Value (ŷᵢ) |
|---|---|---|
| 1 | 2 | 2 |
| 2 | 0 | 2 |
| 3 | 4 | 2 |
| 4 | 1 | 2 |
| 5 | 1 | 2 |
Protocol 1: Calculation of Mean Absolute Error (MAE)
Purpose: To compute the average magnitude of errors, ignoring their direction. Procedure:
- For each observation i, calculate the absolute error: |yᵢ - ŷᵢ|.
- Sum all absolute errors: Σ|yᵢ - ŷᵢ|.
- Divide the sum by the total number of observations (n).
Sample Calculation:
- Absolute Errors: |0|, |-2|, |2|, |-1|, |-1| = 0, 2, 2, 1, 1
- Sum of Absolute Errors: 0 + 2 + 2 + 1 + 1 = 6
- MAE: 6 / 5 = 1.2
Protocol 2: Calculation of Root Mean Square Error (RMSE)
Purpose: To compute a measure of error that is sensitive to large outliers. Procedure:
- For each observation i, calculate the squared error: (yᵢ - ŷᵢ)².
- Sum all squared errors: Σ(yᵢ - ŷᵢ)².
- Divide the sum by the total number of observations (n) to get the Mean Squared Error (MSE).
- Take the square root of the MSE.
Sample Calculation:
- Squared Errors: (0)², (-2)², (2)², (-1)², (-1)² = 0, 4, 4, 1, 1
- Sum of Squared Errors: 0 + 4 + 4 + 1 + 1 = 10
- MSE: 10 / 5 = 2
- RMSE: √2 ≈ 1.414
Protocol 3: Calculation of Mean Absolute Percentage Error (MAPE)
Purpose: To compute the average error as a percentage of the actual values. Procedure:
- For each observation i, calculate the absolute percentage error: |(yᵢ - ŷᵢ) / yᵢ| × 100%.
- Sum all absolute percentage errors: Σ |(yᵢ - ŷᵢ) / yᵢ| × 100%.
- Divide the sum by the total number of observations (n).
Sample Calculation:
- Percentage Errors: |0/2|×100%, |-2/0|×100%, |2/4|×100%, |-1/1|×100%, |-1/1|×100%
- Note: The second term involves division by zero and must be handled (e.g., excluded or imputed). For this example, we exclude it.
- Sum of Percentage Errors (for valid points): 0% + 50% + 100% + 100% = 250%
- MAPE: 250% / 4 = 62.5% (Calculation based on 4 valid data points)
Application in Pharmaceutical Development and Beyond
Error rate analysis is critical across numerous domains. In drug development, the FDA's Center for Drug Evaluation and Research (CDER) has observed a significant increase in regulatory submissions incorporating AI/ML components, where robust model validation is paramount [17]. A study on medication errors in Malaysia, which analyzed over 265,000 reports, highlights the importance of error tracking and analysis for improving pharmacy practices and patient safety, though it focused on clinical errors rather than statistical metrics [67].
Beyond healthcare, these metrics are essential in:
- Finance and Economics: Evaluating the accuracy of stock market or economic forecasting models [65] [64].
- Energy Sector: Assessing models for energy demand forecasting to optimize power generation and resource management [65].
- Climate Science: Comparing climate model predictions against observed data to refine projections of temperature and precipitation [65].
- Retail and Logistics: Forecasting product demand and sales to optimize inventory and supply chains [65] [64].
Advanced Considerations: Scaled Error Metrics
A significant limitation of MAE and RMSE is that their values are scale-dependent, making it difficult to compare model performance across different datasets or units (e.g., sales of individual screws vs. boxes of 100 screws) [66]. To address this, scaled metrics like Mean Absolute Scaled Error (MASE) and Root Mean Square Scaled Error (RMSSE) were developed.
Protocol 4: Calculation of Scaled Metrics (MASE and RMSSE)
Purpose: To create scale-independent error metrics for comparing forecasts across different series. Procedure for MASE:
- Calculate the MAE of your model's forecasts (as in Protocol 1).
- Calculate the MAE of a naive one-step forecast (using the previous period's actual value as the forecast) on the training data.
- Divide the model's MAE by the naive model's MAE.
Procedure for RMSSE:
- Calculate the MSE of your model's forecasts.
- Calculate the MSE of a naive one-step forecast on the training data.
- Divide the model's MSE by the naive model's MSE and take the square root.
Using the sample data from [66], scaling the data by a factor of 100 changes the MAE from 1.2 to 120, but the MASE remains constant at 0.8, confirming its scale-independence. Similarly, the RMSSE provides a consistent, comparable value regardless of the data's scale.
The Scientist's Toolkit: Essential Reagents for Error Analysis
Table 3: Key Research Reagent Solutions for Computational Validation
| Item / Tool | Function in Error Analysis |
|---|---|
| Python with scikit-learn | A programming language and library that provides built-in functions for calculating MAE, RMSE, and other metrics, streamlining the validation process [65]. |
| Statistical Software (R, SAS) | Specialized environments for statistical computing that offer comprehensive packages for error analysis and model diagnostics. |
| Validation Dataset | A subset of data not used during model training, reserved for the final calculation of error metrics to provide an unbiased estimate of model performance. |
| Naive Forecast Model | A simple benchmark model (e.g., predicting the last observed value) used to calculate scaled metrics like MASE and RMSSE, providing a baseline for comparison [66]. |
| Error Distribution Analyzer | Tools (e.g., statistical tests, Q-Q plots) to assess the distribution of residuals, guiding the selection of the most appropriate error metric (RMSE for normal, MAE for Laplacian) [63]. |
Conducting Capability Studies to Assess Process Stability and Variation
Process capability studies are fundamental statistical tools used within input-output transformation validation methods to quantify a process's ability to produce output that consistently meets customer specifications or internal tolerances [68] [69]. In regulated environments like drug development, demonstrating that a manufacturing process is both stable and capable is critical for ensuring product quality, safety, and efficacy. These studies translate process performance into quantitative indices, providing researchers and scientists with a common language for evaluating and comparing the capability of diverse processes [70].
A foundational principle is that process capability can only be meaningfully assessed after a process has been demonstrated to be stable [71] [72]. Process stability, defined as the state where a process exhibits only random, common-cause variation with constant mean and constant variance over time, is a prerequisite [71] [73]. A stable process is predictable, while an unstable process, affected by special-cause variation, is not [72]. Attempting to calculate capability for an unstable process leads to misleading predictions about future performance [73].
Theoretical Foundation: Capability Indices
Process capability is communicated through standardized indices that compare the natural variation of the process to the width of the specification limits.
Key Capability Indices
The most commonly used indices are Cp and Cpk. Their calculations and interpretations are summarized in the table below.
Table 1: Key Process Capability Indices (Cp and Cpk)
| Index | Calculation | Interpretation | Focus |
|---|---|---|---|
| Cp (Process Capability Ratio) | ( Cp = \frac{USL - LSL}{6\sigma} ) [69] | Measures the potential capability of the process, assuming it is perfectly centered. It is a ratio of the specification width to the process spread [70] [73]. | Process Spread (Variation) |
| Cpk (Process Capability Index) | ( Cpk = \min\left( \frac{USL - \mu}{3\sigma}, \frac{\mu - LSL}{3\sigma} \right) ) [70] [69] | Measures the actual capability, accounting for both process spread and the centering of the process mean (μ) relative to the specification limits [70] [73]. | Process Spread & Centering |
Where:
- USL & LSL: Upper and Lower Specification Limits.
- σ (Sigma): The standard deviation of the process, representing its inherent variability.
- μ (Mu): The process mean.
The "3σ" in the denominator for Cpk arises because each index looks at one side of the distribution at a time, and ±3σ represents one half of the natural process spread of 6σ [70].
Process Performance Indices (Pp, Ppk)
It is crucial to distinguish between capability indices (Cp, Cpk) and performance indices (Pp, Ppk). Cp and Cpk are used when a process is under statistical control and are calculated using an estimate of short-term standard deviation (σ), making them predictive of future potential [70] [73]. In contrast, Pp and Ppk are used for new or unstable processes and are calculated using the overall, or long-term, standard deviation of all collected data, making them descriptive of past actual performance [70] [73]. When a process is stable, the values of Cpk and Ppk will converge [70].
Interpreting Index Values
The following table provides general guidelines for interpreting Cp and Cpk values. In critical applications like drug development, higher thresholds are often required.
Table 2: Interpretation of Cp and Cpk Values
| Cpk Value | Sigma Level | Interpretation | Long-Term Defect Rate |
|---|---|---|---|
| < 1.0 | < 3σ | Incapable. Process produces non-conforming product [73]. | > 2,700 ppm |
| 1.0 - 1.33 | 3σ - 4σ | Barely Capable. Requires tight control [73]. | ~ 66 - 2,700 ppm |
| ≥ 1.33 | ≥ 4σ | Capable. Standard minimum requirement for many industries [69] [73]. | ~ 63 ppm |
| ≥ 1.67 | ≥ 5σ | Good Capability. A common target for robust processes [73]. | ~ 0.6 ppm |
| ≥ 2.00 | ≥ 6σ | Excellent Capability. Utilizes only 50% of the spec width, significantly reducing risk [73]. | ~ 0.002 ppm |
A process can have an acceptable Cp but a poor Cpk if the process mean is shifted significantly toward one specification limit, highlighting the importance of evaluating both indices [70].
Diagram 1: Capability Study Workflow
Pre-Study Requirements: Assessing Process Stability
Before calculating capability indices, the mandatory first step is to verify that the process is stable [71] [72].
Protocol for Stability Assessment
Objective: To determine if the process exhibits a constant mean and constant variance over time, with only common-cause variation.
Method: The primary tool for assessing stability is the Control Chart [71] [72].
Data Collection:
Chart Selection & Plotting:
- For continuous data (e.g., weight, concentration, pH), commonly used charts are the X-bar and R chart (for subgrouped data) or the Individuals (I-MR) chart [69].
- Plot the individual data points or subgroup means on the chart in the order they were produced.
Analysis & Interpretation:
- A process is considered stable if the control chart shows no non-random patterns (e.g., trends, cycles, shifts) and all points fall within the calculated control limits, indicating only common-cause variation [72].
- The presence of any points outside the control limits or non-random patterns indicates an unstable process due to special-cause variation [72]. These causes must be identified and eliminated before proceeding with capability analysis.
Experimental Protocol: Conducting a Capability Study
This protocol provides a detailed methodology for executing a process capability study, from planning to interpretation.
Phase 1: Pre-Study Planning and Data Collection
Objective: To establish the study's foundation and collect high-integrity data.
Define Scope and Specifications:
- Clearly define the Critical-to-Qality (CTQ) characteristic to be measured.
- Document the Upper and Lower Specification Limits (USL/LSL) based on patient safety, efficacy, or regulatory requirements.
Verify Measurement System:
Sampling Strategy:
- Use a rational sampling scheme to ensure data is representative of the entire process run. For example, collect small subgroups (e.g., 3-5 consecutive units) at regular intervals throughout a production batch [68] [69].
- Sample size must be adequate for statistical validity; typically, 100-125 individual measurements are considered a minimum [71].
Phase 2: Data Analysis and Calculation
Objective: To compute process capability indices and visualize process performance.
Verify Stability:
- Construct a control chart with the collected data as described in Section 3.1. If the process is unstable, pause the study and investigate special causes.
Check Normality:
- Generate a histogram of the data with the specification limits overlaid.
- Perform a statistical test for normality (e.g., Anderson-Darling). Cp and Cpk are highly sensitive to the normality assumption. If data is non-normal, transformation or alternative indices (e.g., Cpm) may be required [68] [69].
Calculate Baseline Statistics:
- Calculate the process mean (μ) and standard deviation (σ).
- For a stable process, the within-subgroup standard deviation is often used to estimate σ for Cp/Cpk, as it represents the inherent, short-term process variation [73].
Compute Capability Indices:
- Calculate Cp and Cpk using the formulas in Table 1.
- For a comprehensive view, also calculate Pp and Ppk using the overall (long-term) standard deviation.
Phase 3: Interpretation and Reporting
Objective: To translate numerical results into actionable insights.
- Interpret Values: Refer to Table 2 to interpret the calculated Cp and Cpk values. A Cpk ≥ 1.33 is often the minimum target for a capable process [73].
- Analyze the Histogram: Visually assess the distribution relative to the specification limits. Look for adequate "white space" between the process spread and the specs [73].
- Report Findings: Report the capability indices and their associated Z-scores (Z = 3 × Cpk) [70]. Use confidence intervals for the true capability values if possible, as point estimates are subject to sampling error [68].
The Scientist's Toolkit: Essential Reagents and Solutions
This table details key resources required for conducting rigorous process capability studies.
Table 3: Essential "Research Reagent Solutions" for Capability Studies
| Item / Solution | Function / Purpose | Critical Considerations |
|---|---|---|
| Statistical Software (e.g., Minitab, JMP, R) [69] | Automates calculation of capability indices, creation of control charts, and normality tests. Reduces human error and increases efficiency. | Software must be validated for use in regulated environments. Choose packages with comprehensive statistical tools. |
| Calibrated Measurement Gage [73] | Provides the raw data for the study by measuring the CTQ characteristic. The foundation of all subsequent analysis. | Resolution must be ≤ 1/10th of tolerance. Requires regular calibration and a successful Gage R&R study. |
| Standard Operating Procedure (SOP) | Provides a controlled, standardized methodology for how to conduct the study, ensuring consistency and compliance. | Must define sampling plans, data recording formats, and analysis methods. |
| Control Chart [71] [72] | The primary tool for distinguishing common-cause from special-cause variation, thereby assessing process stability. | Correct chart type must be selected based on data type (e.g., I-MR, X-bar R). Control limits must be calculated from process data. |
| Reference Data Set (for software verification) | Used to verify that statistical software algorithms are calculating indices correctly, a form of verification. | Can be a known data set with published benchmark results (e.g., from NIST). |
Diagram 2: Input-Output Validation Logic
Identifying Root Causes with Failure Modes and Effects Analysis (FMEA)
Failure Modes and Effects Analysis (FMEA) serves as a systematic, proactive framework for identifying potential failures within systems, processes, or products before they occur. Within the context of input-output transformation validation methods, FMEA provides a critical mechanism for analyzing how process inputs (e.g., materials, information, actions) can deviatate and lead to undesirable outputs (e.g., defects, errors, failures). Originally developed by the U.S. military in the 1940s and later adopted by NASA and various industries, this methodology enables researchers and drug development professionals to enhance reliability, safety, and quality by preemptively addressing system vulnerabilities [74] [75]. This paper presents structured protocols, quantitative risk assessment tools, and practical applications of FMEA, with particular emphasis on pharmaceutical and healthcare settings where validation of process transformations is paramount.
In validation methodologies, the "input-output transformation" model represents any process that converts specific inputs into desired outputs. FMEA strengthens this model by providing a structured framework to identify where and how the transformation process might fail, the potential effects of those failures, and their root causes [74] [76]. This is particularly crucial in drug development, where the inputs (e.g., raw materials, experimental protocols, manufacturing procedures) must consistently transform into safe, effective, and high-quality outputs (e.g., finished pharmaceuticals, reliable research data) [77] [78].
FMEA functions as a prospective risk assessment tool, contrasting with retrospective methods like Root Cause Analysis (RCA). By assembling cross-functional teams and systematically analyzing each process step, FMEA identifies potential failure modes, their effects on the system, and their underlying causes [74] [79]. The method prioritizes risks through quantitative scoring, enabling organizations to focus resources on the most critical vulnerabilities [80]. The application of FMEA in healthcare and pharmaceutical settings has grown significantly, with regulatory bodies like The Joint Commission recommending its use for proactive risk assessment [79].
Core Principles and Quantitative Framework
Fundamental FMEA Concepts
The FMEA methodology rests on several key concepts that align directly with input-output validation [80]:
- Systematic Approach: FMEA follows a structured methodology for identifying potential failure modes, analyzing their causes and effects, and developing preventive actions.
- Proactive Risk Management: It identifies and addresses potential failures before they occur, preventing costly failures and enhancing performance.
- Cross-functional Collaboration: It involves multidisciplinary teams with diverse expertise, ensuring comprehensive analysis of various factors contributing to failure modes.
- Quantitative Analysis: It incorporates numerical assessment of severity, occurrence probability, and detection capability to facilitate prioritization and decision-making.
Risk Priority Number (RPN) Calculation
The core quantitative metric in traditional FMEA is the Risk Priority Number (RPN), calculated as follows [77] [76]:
RPN = Severity (S) × Occurrence (O) × Detection (D)
Table 1: Traditional FMEA Risk Scoring Criteria
| Dimension | Score Range | Description | Quantitative Guidance |
|---|---|---|---|
| Severity (S) | 1-10 | Importance of effect on critical quality parameters | 1 = Not severe; 10 = Very severe/Catastrophic [76] |
| Occurrence (O) | 1-10 | Frequency with which a cause occurs | 1 = Not likely; 10 = Very likely [76] |
| Detection (D) | 1-10 | Ability of current controls to detect the cause | 1 = Likely to detect; 10 = Not likely to detect [76] |
Table 2: Risk Priority Number (RPN) Intervention Thresholds [78]
| RPN Range | Priority Level | Required Action |
|---|---|---|
| > 30 | Very High | Immediate corrective actions required |
| 20-29 | High | Corrective actions needed within specified timeframe |
| 10-19 | Medium | Corrective actions recommended |
| < 10 | Low | Actions optional; monitor periodically |
Advanced Quantitative Criticality Analysis
For higher-precision applications, particularly in defense, aerospace, or critical pharmaceutical manufacturing, Quantitative Criticality Analysis (QMECA) provides a more rigorous approach. This method calculates Mode Criticality using the formula [75]:
Mode Criticality = Expected Failures × Mode Ratio of Unreliability × Probability of Loss
Where:
- Expected Failures: Number of failures estimated based on item reliability at a given time (e.g., λt for exponential distribution)
- Mode Ratio of Unreliability: Percentage of item failures attributable to a specific failure mode
- Probability of Loss: Likelihood that the failure mode will cause system failure (100% for actual loss, >10-100% for probable loss, >0-10% for possible loss) [75]
FMEA Experimental Protocol and Methodology
Standard FMEA Protocol
The following protocol provides a systematic approach for conducting FMEA studies in research and drug development environments:
Step 1: Team Assembly
- Assemble a multidisciplinary team including representatives from design, manufacturing, quality, testing, reliability, maintenance, purchasing, and customer service [74].
- In pharmaceutical contexts, include pharmacists, physicians, nurses, quality control personnel, and information engineers as applicable [77] [78].
- Designate a team leader with FMEA expertise to facilitate the process.
Step 2: Process Mapping and Scope Definition
- Define the FMEA's scope and boundaries clearly [74].
- Create detailed process flowcharts identifying all transformation steps from input to output.
- For medication dispensing processes, map sub-processes including prescription issuance, verification, dispensing, and documentation [77].
- Validate the process map with all stakeholders to ensure completeness.
Step 3: Function and Failure Mode Identification
- For each process step, identify the intended function or transformation [74].
- Brainstorm all potential failure modes (ways the process could fail to achieve its intended transformation).
- Document failure modes using clear, specific descriptions.
- In pharmaceutical applications, identify potential failures in drug storage, preparation, dispensing, and administration [77] [78].
Step 4: Effects and Causes Analysis
- For each failure mode, identify all potential consequences (effects) on the system, related processes, products, services, customers, or regulations [74].
- Determine all potential root causes for each failure mode using techniques like the "5 Whys" or fishbone diagrams [80].
- Focus on identifying the fundamental process or system flaws rather than individual human errors.
Step 5: Risk Assessment and Prioritization
- For each failure mode, assign Severity (S), Occurrence (O), and Detection (D) ratings using standardized criteria [74].
- Calculate Risk Priority Numbers (RPN) for each failure mode.
- Prioritize failure modes for intervention based on RPN scores and threshold values.
Step 6: Action Plan Development and Implementation
- Develop specific corrective actions to address high-priority failure modes [80].
- Assign responsibility and timelines for implementation.
- Focus on eliminating root causes rather than symptoms.
- Implement mistake-proofing (poka-yoke) solutions where possible.
Step 7: Monitoring and Control
- Track effectiveness of implemented actions.
- Recalculate RPNs after improvements to verify risk reduction.
- Update FMEA documentation to reflect changes.
- Incorporate FMEA findings into standard operating procedures and training materials.
Diagram 1: FMEA Methodology Workflow. This diagram illustrates the sequential process for conducting a complete FMEA study, highlighting the critical risk assessment and improvement phases.
Application in Pharmaceutical Dispensing: Case Protocol
Based on research by Anjalee et al. (2021), the following protocol specifics apply to medication dispensing processes [77]:
Team Structure:
- Two independent teams of 5-7 pharmacists each
- Teams conduct parallel analyses to enhance validity
- 4-6 meetings of 2 hours each per team
Data Collection Methods:
- Extract prescription data from Hospital Information System (HIS)
- Review paper prescriptions for completeness
- Verify signature registration books
- Cross-reference dispensing records with inventory data
Failure Mode Identification:
- Teams identified 48 and 42 failure modes respectively
- 69 failure modes were common to both teams
- Overcrowded dispensing counters contributed to 57 failure modes
Intervention Strategies:
- Redesign dispensing tables and labels
- Modify medication re-packing processes
- Establish patient counseling units
- Implement regular process audits
Table 3: Research Reagent Solutions for FMEA Implementation
| Tool/Resource | Function | Application Context |
|---|---|---|
| Cross-functional Team | Provides diverse expertise and perspectives for comprehensive failure analysis | Essential for all FMEA types; multidisciplinary input critical for pharmaceutical applications [74] [77] |
| Process Mapping Software | Documents and visualizes process flows from input to output | Critical for understanding transformation processes and identifying failure points [74] |
| FMEA Worksheet/Template | Standardized documentation tool for recording failure modes, causes, effects, and actions | Required for consistent application across projects; customizable for specific organizational needs [74] [81] |
| Risk Assessment Matrix | Tool for evaluating and prioritizing risks based on Severity, Occurrence, and Detection | Enables quantitative risk prioritization; can be customized to organizational risk tolerance [81] |
| Root Cause Analysis Tools | Methods like 5 Whys, Fishbone Diagrams for identifying fundamental causes | Essential for moving beyond symptoms to address underlying process flaws [80] |
| Statistical Reliability Data | Historical failure rates, mode distributions, and reliability metrics | Critical for Quantitative Criticality Analysis; enhances objectivity of occurrence estimates [75] |
| FMEA Software Solutions | Automated tools for managing FMEA data, calculations, and reporting | Streamlines complex analyses; maintains historical data for continuous improvement [80] [81] |
Case Study: FMEA in Anesthetic Drug Management
A 2024 study applied FMEA to manage anesthetic drugs and Class I psychotropic medications in a hospital setting, identifying 15 failure modes with RPN values ranging from 4.21 to 38.09 [78]. The study demonstrates FMEA's application in high-stakes pharmaceutical environments.
Table 4: High-Priority Failure Modes in Anesthetic Drug Management [78]
| Failure Mode | Process Stage | RPN Score | Priority | Corrective Actions |
|---|---|---|---|---|
| Discrepancies between empty ampule collection and dispensing quantities | Recovery | 38.09 | Very High | Enhanced documentation procedures; automated reconciliation systems |
| Patients' inability to receive medications in a timely manner | Dispensing | 32.15 | Very High | Process redesign; staffing adjustments; queue management |
| Incomplete prescription information | Prescription Issuance | 24.67 | High | Standardized prescription templates; mandatory field requirements |
| Incorrect dosage verification | Prescription Verification | 21.43 | High | Independent double-check protocols; decision support systems |
The study employed a multidisciplinary team including doctors, pharmacists, nurses, and information engineers. Data sources included Hospital Information System (HIS) records, paper prescriptions, and verification signature registration books. The team established specific intervention thresholds: RPN > 30 (very high priority), 20-29 (high priority), 10-19 (medium priority), and RPN < 10 (low priority) [78].
Diagram 2: FMEA Risk Assessment Logic. This diagram illustrates the logical relationship between risk assessment components and how they integrate to determine priority classifications and action plans.
Customization and Implementation Considerations
Adapting FMEA for Specific Research Contexts
FMEA methodology can be customized for different applications within drug development and research:
Design FMEA (DFMEA)
- Focuses on identifying potential failure modes during the design phase of products, systems, or processes
- Aims to prevent design-related failures before they occur [80]
- Particularly relevant for pharmaceutical device development and experimental design
Process FMEA (PFMEA)
- Evaluates potential failure modes in manufacturing or operational processes
- Identifies process weaknesses and error-prone areas [80]
- Essential for drug manufacturing process validation and quality control
Healthcare FMEA (HFMEA)
- Adapted for healthcare environments with specific considerations for patient safety
- Incorporates elements from FMEA, hazard analysis, and root cause analysis [79]
- Appropriate for clinical trial management and healthcare service delivery
Customization of Risk Criteria
Risk assessment criteria can be tailored to specific organizational needs and risk tolerance:
- Severity Criteria: Can include multiple dimensions such as patient impact, regulatory compliance, financial consequences, and reputational damage [81]
- Occurrence Ratings: Can be calibrated using historical data, reliability predictions, or expert consensus [81]
- Detection Capabilities: Should reflect the organization's current control systems and monitoring capabilities [81]
- Action Priority (AP): Alternative prioritization approach that uses predetermined rules rather than simple RPN thresholds [81]
Failure Modes and Effects Analysis provides a robust, systematic framework for identifying root causes within input-output transformation systems, particularly in pharmaceutical research and drug development. By employing structured protocols, quantitative risk assessment, and cross-functional expertise, FMEA enables organizations to proactively identify and mitigate potential failures before they impact product quality, patient safety, or research validity. The methodology's flexibility allows customization across various applications, from drug design and manufacturing to clinical trial management and healthcare delivery. When properly implemented and integrated into quality management systems, FMEA serves as a powerful validation tool for ensuring the reliability and safety of critical transformation processes in highly regulated environments.
Reducing Variation and Achieving Robust Design
In both manufacturing and drug development, variation is an inherent property where every unit of product or result differs to some small degree from all others [82]. Robust Design is an engineering methodology developed by Genichi Taguchi that aims to create products and processes that are insensitive to the effects of variation, particularly variation from uncontrollable factors or "noise" [83]. For researchers and scientists in drug development, implementing robust design principles means that therapeutic products will maintain consistent quality, safety, and efficacy despite normal fluctuations in raw materials, manufacturing parameters, environmental conditions, and patient characteristics.
The fundamental principle of variation transmission states that variation in process inputs (materials, parameters, environment) is transmitted to process outputs (product characteristics) [84] [82]. Understanding and controlling this transmission represents the core challenge in achieving robust design. This relationship can be mathematically modeled to predict how input variations affect critical quality attributes, enabling scientists to proactively design robustness into their processes rather than attempting to inspect quality into finished products.
Table 1: Key Terminology in Variation Reduction and Robust Design
| Term | Definition | Application in Drug Development |
|---|---|---|
| Controllable Factors | Process parameters that can be precisely set and maintained | Reaction temperature, mixing speed, catalyst concentration |
| Uncontrollable Factors (Noise) | Sources of variation that are difficult or expensive to control | Raw material impurity profiles, environmental humidity, operator technique |
| Variation Transmission | Mathematical relationship describing how input variation affects outputs [84] | Modeling how API particle size distribution affects dissolution rate |
| Robust Optimization | Selecting parameter targets that minimize output sensitivity to noise [84] | Identifying optimal buffer pH that minimizes degradation across storage temperatures |
| Process Capability (Cp, Cpk) | Statistical measures of a process's ability to meet specifications [82] | Quantifying ability to consistently achieve tablet potency within 95-105% label claim |
Fundamental Principles of Variation Transmission
Variation transmission analysis provides the mathematical foundation for robust design. This approach uses quantitative relationships between input variables and output responses to predict how input variation affects final product characteristics [84]. For a pharmaceutical process with output Y that depends on several input variables (X₁, X₂, ..., Xₙ), the relationship can be expressed as Y = f(X₁, X₂, ..., Xₙ). The variation in Y (σᵧ²) can be approximated using the following equation based on partial derivatives:
This equation demonstrates that the contribution of each input variable to the total output variation depends on both its own variation (σᵢ²) and the sensitivity of the output to that input (∂f/∂Xᵢ) [84]. Robust design addresses both components: reducing the sensitivity through parameter optimization, and controlling the input variation through appropriate tolerances.
A pump design example illustrates this principle effectively. The pump flow rate (F) depends on piston radius (R), stroke length (L), motor speed (S), and valve backflow (B) according to the equation: F = S × [16.388 × πR²L - B] [84]. Through variation transmission analysis, researchers determined that backflow variation contributed most significantly to flow rate variation, informing the strategic decision to specify a higher-cost valve with tighter tolerances to achieve the required flow rate consistency [84].
Figure 1: Variation Transmission Framework - This diagram illustrates how input variation is transmitted through a process to create output variation, with robust design strategies providing control through continuous feedback and optimization.
Experimental Protocols for Robust Design
Protocol 1: Variation Transmission Analysis
Objective: To quantify the relationship between input variables and critical quality attributes, identifying which parameters require tighter control and which can be targeted for robust optimization.
Materials and Methods:
- Experimental System: Pharmaceutical blending process with multiple controllable parameters
- Response Variables: Blend uniformity (RSD), dissolution rate (% at 30 min), tablet hardness
- Input Variables: Mixing speed (rpm), mixing time (min), blender load level (%), excipient particle size (μm)
Procedure:
- Define Mathematical Model: Establish theoretical relationships between inputs and outputs based on first principles. For a blending process, this may include mass balance equations and powder flow dynamics.
- Characterize Input Variation: Collect historical data or conduct capability studies to determine the natural variation of each input variable under normal operating conditions [82].
- Calculate Sensitivity Coefficients: Determine partial derivatives (∂Y/∂Xᵢ) either analytically from first principles or empirically through controlled experimentation.
- Predict Output Variation: Apply the variation transmission equation to calculate the expected variation in each critical quality attribute.
- Identify Key Contributors: Rank input variables by their contribution to total output variation (sensitivity² × input variation).
Data Analysis: Table 2: Variation Transmission Analysis for Pharmaceutical Blending Process
| Input Variable | Nominal Value | Natural Variation (±3σ) | Sensitivity (∂Y/∂X) | Contribution to Output Variation (%) |
|---|---|---|---|---|
| Mixing Speed | 45 rpm | ±5 rpm | 0.15 RSD/rpm | 18% |
| Mixing Time | 20 min | ±2 min | 0.25 RSD/min | 32% |
| Blender Load | 75% | ±8% | 0.08 RSD/% | 12% |
| Excipient Particle Size | 150 μm | ±25 μm | 0.12 RSD/μm | 38% |
Protocol 2: Robust Optimization Using Response Surface Methodology
Objective: To identify optimal parameter settings that minimize the sensitivity of critical quality attributes to uncontrollable noise factors.
Materials and Methods:
- Experimental Design: Central Composite Design (CCD) with 3 controllable factors and 2 noise factors
- Controllable Factors: Binder concentration, granulation time, compression force
- Noise Factors: Environmental humidity, API particle size distribution
- Response Variables: Tablet tensile strength, dissolution efficiency
Procedure:
- Experimental Design: Structure a response surface methodology (RSM) experiment that systematically varies both controllable and noise factors. A combined array approach places noise factors in the outer array and controllable factors in the inner array.
- Execute Experimental Runs: Conduct all experimental runs in randomized order to avoid systematic bias. Replicate center points to estimate pure error.
- Model Development: Fit response surface models for each critical quality attribute, including both main effects and interactions between controllable and noise factors.
- Robustness Optimization: Use mathematical programming or graphical optimization to identify settings of controllable factors that minimize the transmission of noise variation to the responses.
- Verification: Confirm optimal settings through additional verification experiments and compare predicted versus actual performance.
Data Analysis: Table 3: Robust Optimization Results for Tablet Formulation
| Controllable Factor | Original Setting | Robust Optimal Setting | Sensitivity Reduction | Performance Improvement |
|---|---|---|---|---|
| Binder Concentration | 3.5% w/w | 4.2% w/w | 42% | Tensile strength Cpk improved from 1.2 to 1.8 |
| Granulation Time | 8 min | 10.5 min | 28% | Dissolution Cpk improved from 1.1 to 1.6 |
| Compression Force | 12 kN | 14 kN | 35% | Reduced sensitivity to API lot variation by 52% |
Figure 2: Robust Design Optimization Workflow - This methodology systematically identifies parameter settings that minimize sensitivity to uncontrollable variation, creating more reliable pharmaceutical processes.
Research Reagent Solutions and Materials
Implementing robust design principles requires specific statistical, computational, and experimental tools. The following reagents and solutions enable researchers to effectively characterize and optimize their processes for reduced variation.
Table 4: Essential Research Reagent Solutions for Robust Design Implementation
| Research Reagent | Function | Application Example |
|---|---|---|
| Statistical Analysis Software | Enables variation transmission analysis and modeling of input-output relationships [84] | JMP, Minitab, or R for designing experiments and analyzing process capability |
| Design of Experiments (DOE) | Structured approach for efficiently exploring factor effects and interactions [82] | Screening designs to identify critical process parameters affecting drug product CQAs |
| Process Capability Indices | Quantitative measures of process performance relative to specifications [82] | Cp/Cpk analysis to assess ability to consistently meet potency specifications |
| Response Surface Methodology | Optimization technique for finding robust operating conditions [84] | Central composite designs to map the design space for a granulation process |
| Failure Mode and Effects Analysis | Systematic risk assessment tool for identifying potential variation sources [82] | Assessing risks to product quality from material and process variability |
| Measurement System Analysis | Quantifies contribution of measurement error to total variation [82] | Gage R&R studies to validate analytical methods for content uniformity testing |
Implementation Framework for Pharmaceutical Development
Successful implementation of robust design in pharmaceutical development requires a structured framework that integrates with existing quality systems and regulatory expectations. The following protocol outlines a comprehensive approach for implementing variation reduction strategies throughout the product lifecycle.
Objective: To establish a systematic framework for implementing robust design principles that ensures consistent drug product quality and facilitates regulatory compliance.
Materials and Methods:
- Quality by Design Framework: ICH Q8-Q11 guidelines
- Statistical Tools: Design of Experiments, Process Capability Analysis, Control Charts
- Documentation System: Electronic Quality Management System (eQMS)
- Risk Management Tools: FMEA, Risk Assessment Matrices
Procedure:
- Define Target Product Profile: Identify Critical Quality Attributes (CQAs) that impact therapeutic performance, safety, and efficacy.
- Link CQAs to Process Parameters: Through small-scale experiments and prior knowledge, identify Critical Process Parameters (CPPs) that significantly affect CQAs.
- Characterize Variation Transmission: Quantify how variation in CPPs and material attributes propagates to affect CQAs using the principles outlined in Protocol 1.
- Establish Design Space: Through comprehensive experimentation (Protocol 2), define the multidimensional combination of input variables that consistently produce material meeting CQA requirements.
- Implement Control Strategy: Define appropriate controls for CPPs and material attributes based on their impact on CQAs and variation transmission characteristics.
- Monitor Continuously: Implement statistical process control and continued process verification to ensure the process remains in a state of control.
Data Analysis: Table 5: Robust Design Implementation Metrics for Pharmaceutical Development
| Implementation Phase | Key Activities | Success Metrics | Regulatory Documentation |
|---|---|---|---|
| Process Design | Identify CQAs, CPPs, and noise factors | Risk prioritization of parameters | Quality Target Product Profile |
| Process Characterization | Design space exploration via DOE | Establishment of proven acceptable ranges | Process Characterization Report |
| Robust Optimization | Response surface methodology | Reduced sensitivity to noise factors | Design Space Definition |
| Control Strategy | Control plans for critical parameters | Cp/Cpk > 1.33 for all CQAs | Control Strategy Document |
| Lifecycle Management | Continued process verification | Stable capability over product lifecycle | Annual Product Reviews |
The integration of robust design principles with the pharmaceutical quality by design framework creates a powerful approach for developing robust manufacturing processes that consistently produce high-quality drug products. By systematically applying variation transmission analysis and robust optimization techniques, pharmaceutical scientists can significantly reduce the risk of quality issues while maintaining efficiency and regulatory compliance.
Implementing Automated Testing Frameworks and Continuous Monitoring
Within the broader research on input-output transformation validation methods, the implementation of automated testing frameworks and continuous monitoring represents a critical paradigm for ensuring the reliability, safety, and efficacy of complex systems. In the high-stakes context of drug development, these methodologies provide the essential infrastructure for validating that software-controlled processes and data transformations consistently produce outputs that meet predetermined quality attributes and regulatory specifications [13]. This document details the application notes and experimental protocols for integrating these practices, framing them as applied instances of rigorous input-output validation.
The lifecycle of a pharmaceutical product, from discovery through post-market surveillance, is a series of interconnected input-output systems. Process validation, as defined by regulatory bodies, is "the collection and evaluation of data, from the process design stage through commercial production, which establishes scientific evidence that a process is capable of consistently delivering quality product" [13]. Automated testing and continuous monitoring are the operational mechanisms that enable this evidence-based assurance, transforming raw data into validated knowledge for researchers, scientists, and drug development professionals.
Automated Testing Frameworks: Structured Assurance for Input-Output Consistency
Automated testing frameworks provide a structured set of rules, tools, and practices that offer a systematic approach to validating software behavior [85]. They are foundational to building quality into digital products rather than inspecting it afterward, directly supporting the Process Design stage of validation [13]. These frameworks organize test code, increase test accuracy and reliability, and simplify maintenance, which is crucial for the long-term viability of research and production software [85].
Quantitative Comparison of Prevalent Testing Frameworks
The selection of an appropriate framework depends on the specific validation requirements, the system under test, and the technical context of the team. The following table summarizes key quantitative and functional data for popular frameworks relevant to scientific applications.
Table 1: Comparative Analysis of Automated Testing Frameworks for 2025
| Framework | Primary Testing Type | Key Feature | Supported Languages | Key Advantage for Research |
|---|---|---|---|---|
| Selenium [85] [86] | Web Application | Cross-browser compatibility | Java, Python, C#, Ruby, JavaScript | Industry standard; extensive community support & integration |
| Playwright [85] [86] | End-to-End Web | Reliability for modern web apps, built-in debugging | JavaScript, TypeScript, Python, C#, Java | Robust API for complex scenarios (e.g., iframes, pop-ups) |
| Cucumber [85] | Behavior-Driven Development (BDD) | Plain language Gherkin syntax | Underlying step definitions in multiple languages | Bridges communication between technical and non-technical stakeholders |
| Appium [85] [86] | Mobile Application | Cross-platform (iOS, Android) | Java, Python, JavaScript | Extends Selenium's principles to mobile environments |
| TestCafe [85] | End-to-End Web | Plugin-free execution | JavaScript, TypeScript | Simplified setup and operation, no external dependencies |
| Robot Framework [85] | Acceptance Testing | Keyword-driven, plain-text syntax | Primarily Python, extensible | Highly accessible for non-programmers; clear, concise test cases |
The Emergence of AI in Test Automation
The field is experiencing a significant shift with the integration of Artificial Intelligence (AI), marking a "Third Wave" of test automation [87]. This wave is characterized by capabilities that directly enhance input-output validation efforts:
- Self-healing tests: Tests that autonomously adapt to changes in the application's user interface, reducing maintenance overhead and preventing false negatives [87].
- Natural language processing: Enables the creation of test cases from plain English requirements, democratizing test creation and aligning with BDD principles [87].
- Autonomous agents: AI systems that can reason and make decisions, going beyond script execution to actively explore and test applications [87].
- Visual intelligence: Validates the visual presentation of an application, a critical output often missed by traditional functional testing [87].
Tools like BlinqIO, testers.ai, and Mabl exemplify this trend, offering AI-powered capabilities that can dramatically accelerate test creation and execution while improving robustness [87].
Continuous Monitoring: The Persistent Validation Feedback Loop
Continuous monitoring represents the ongoing, real-world application of output validation. In the context of drug development, it is the mechanism for Continued Process Verification, ensuring a process remains in a state of control during commercial manufacturing [13]. More broadly, it enables the early detection of deviations, tracks system health, and provides a feedback loop for continuous improvement.
Application in Post-Marketing Drug Surveillance
Post-marketing surveillance (PMS) is a critical domain where continuous monitoring is paramount. It serves as the safety net that protects patients after a pharmaceutical product reaches the market, systematically collecting and evaluating safety data to identify previously unknown adverse effects or confirm known risks in broader populations [88] [89]. This process validates the real-world safety and efficacy of a drug—a crucial output—against the expectations set during clinical trials.
Table 2: Data Sources and Analytical Methods for Continuous Monitoring in Pharmacovigilance
| Method/Data Source | Core Function | Key Strengths | Key Limitations |
|---|---|---|---|
| Spontaneous Reporting Systems (e.g., FAERS) [88] [89] | Passive surveillance; voluntary reporting of adverse events. | Early signal detection; global coverage; detailed case narratives. | Significant underreporting; reporting bias; lack of denominator data. |
| Active Surveillance (e.g., Patient Registries) [88] [89] | Proactive, longitudinal follow-up of specific patient populations. | Detailed clinical data; ideal for long-term safety and rare diseases. | Resource-intensive; potential for selection bias; limited generalizability. |
| Electronic Health Records (EHRs) [90] [89] | Data mining of routine clinical care data for trends and risks. | Large-scale data; rich clinical context; real-world evidence. | Data quality variability; interoperability challenges; privacy concerns. |
| Wastewater Analysis [90] | Population-level biomonitoring for pathogen or substance prevalence. | Cost-effective; anonymous; provides community-level insight. | Cannot attribute use to individuals; ethical concerns; complex logistics. |
| Digital Health Technologies [90] [89] | Continuous patient monitoring via wearables and mobile apps. | Continuous, objective data; high patient engagement; real-time feedback. | Requires data validation; introduces technology access barriers. |
The Role of AI and Technology in Advanced Monitoring
Artificial intelligence and machine learning are revolutionizing continuous monitoring by enhancing signal detection and analysis. Machine learning algorithms can identify potential safety signals from complex, multi-source datasets, detecting subtle associations that traditional statistical methods might miss [90] [89]. Furthermore, Natural Language Processing (NLP) transforms unstructured data from clinical notes, social media, and case report narratives into structured, analyzable information, unlocking previously inaccessible data sources for validation [89].
Experimental Protocols for Validation
This section provides detailed, executable protocols for establishing automated testing and continuous monitoring as part of a comprehensive input-output validation strategy.
Protocol: Implementing a Hybrid Test Automation Framework
Objective: To establish a robust, maintainable, and scalable test automation framework that validates the functionality, integration, and business logic of a software application.
Research Reagent Solutions:
- Selenium WebDriver/Playwright: Core library for driving browser interaction and validating web-based user interfaces [85] [86].
- Cucumber/Gherkin: Behavior-Driven Development (BDD) tool for defining test scenarios in natural language, ensuring alignment with business requirements [85].
- JUnit/TestNG: Test runner for organizing and executing test suites and generating reports.
- CI/CD Server (e.g., Jenkins): Orchestration tool for integrating test execution into the development pipeline.
- Programming Language (e.g., Java, Python): The underlying language for implementing test logic and step definitions.
Methodology:
- Framework Architecture Design (Define): Adopt a hybrid framework combining a BDD layer for business-facing tests with a page object model for technical implementation. This separates the "what" (test scenario) from the "how" (interaction with the application).
- Test Data Strategy (Define): Implement a data-driven approach. Externalize test inputs and expected outputs into files (e.g., CSV, JSON) to allow the same test logic to be validated against multiple datasets [86].
- Implementation of Validation Layers (Improve):
- Unit Tests: Developers write and execute these tests to validate individual code units (e.g., functions, methods) in isolation.
- API/Service Tests: Validate business logic and data contracts at the service layer, independent of the user interface.
- End-to-End (E2E) Tests: Using Selenium or Playwright, automate critical user journeys that traverse multiple system components to validate integrated functionality [85].
- Integration with CI/CD (Control): Configure the CI/CD server to automatically trigger the relevant test suite upon events like a code commit or pull request. This shift-left practice validates changes continuously [86].
- Reporting and Analysis (Control): Configure the framework to generate detailed test reports after each run, including pass/fail status, logs, and screenshots of failures for root cause analysis.
Protocol: Establishing Continuous Monitoring for Process Validation
Objective: To implement a continuous monitoring system that provides ongoing verification of a manufacturing or data processing workflow, ensuring it remains in a validated state.
Research Reagent Solutions:
- Process Analytical Technology (PAT) Sensors: Hardware for real-time measurement of Critical Process Parameters (CPPs).
- Statistical Process Control (SPC) Software: Tool for statistical analysis of process data and generation of control charts [13].
- Electronic Health Record (EHR) or Data Warehouse: Centralized repository for aggregating real-world performance and safety data [90] [89].
- Signal Detection Algorithms (e.g., Machine Learning Models): Computational methods for identifying patterns and anomalies in large datasets [90] [89].
Methodology:
- Identify Critical Quality Attributes (CQAs) & CPPs (Define): Define the measurable outputs (CQAs) critical to product quality and the process inputs (CPPs) that impact them. This is the foundation of the input-output model [13].
- Define Control Strategy and Data Collection Points (Define): Establish a control plan specifying how each CPP will be controlled and monitored. Identify where in the process data will be collected.
- Implement Real-Time Data Acquisition (Measure): Deploy sensors and data logging systems to automatically collect data on CPPs and CQAs at the defined frequencies.
- Statistical Monitoring and Alerting (Analyze/Control):
- Implement control charts (e.g., X-bar, R charts) to monitor process stability over time. Calculate and monitor process capability indices (Cp, Cpk) [13].
- Set thresholds and configure automated alerts to trigger when data indicates the process is trending out of control.
- Signal Triage and Investigation (Control): Establish a formal procedure for investigating alerts. Use root cause analysis (RCA) techniques to determine the source of the variation.
- Feedback Loop for Process Improvement (Control): Use insights from monitoring and investigations to make informed, documented adjustments to the process, followed by appropriate re-validation activities.
The Scientist's Toolkit: Essential Research Reagents and Solutions
This table catalogs key technologies and methodologies that constitute the essential "reagents" for experiments in automated testing and continuous monitoring.
Table 3: Essential Research Reagents for Validation Frameworks
| Category | Item | Function in Validation Context |
|---|---|---|
| Testing Frameworks | Selenium WebDriver [85] | Core engine for automating and validating web browser interactions. |
| Playwright [85] | Reliable framework for end-to-end testing of modern web applications. | |
| Cucumber [85] | BDD tool for expressing test cases in natural language (Gherkin). | |
| Appium [85] | Extends automation principles to mobile (iOS/Android) applications. | |
| Validation & Analysis Tools | Joi / Pydantic [9] | Libraries for input-output data schema validation in API development. |
| Statistical Process Control (SPC) [13] | Method for monitoring and controlling a process via control charts. | |
| Data Sources | EHR & Claims Databases [90] [89] | Provide large-scale, real-world data for outcomes monitoring and safety surveillance. |
| Spontaneous Reporting Systems (e.g., FAERS) [88] [89] | Foundation for passive pharmacovigilance and adverse event signal detection. | |
| Methodologies | Behavior-Driven Development (BDD) [85] [86] | Collaborative practice to define requirements and tests using ubiquitous language. |
| Risk Management Planning [89] | Proactive process for identifying potential failures and defining mitigation strategies. |
Demonstrating Efficacy: Rigorous Validation and Comparative Analysis for Regulatory Success
Artificial intelligence has emerged as a transformative force in drug development, demonstrating significant capabilities across target identification, biomarker discovery, and clinical trial optimization [91]. The synergy between machine learning and high-dimensional biomedical data has fueled growing optimism about AI's potential to accelerate and enhance the therapeutic development pipeline. Despite this promise, AI's clinical impact remains limited, with many systems confined to retrospective validations and pre-clinical settings, seldom advancing to prospective evaluation or integration into critical decision-making workflows [91].
This gap reflects systemic issues within both the technological ecosystem and the regulatory framework. A recent study examining 950 AI medical devices authorized by the FDA revealed that 60 devices were associated with 182 recall events, with approximately 43% of all recalls occurring within one year of authorization [92]. The most common causes were diagnostic or measurement errors, followed by functionality delay or loss. Significantly, the "vast majority" of recalled devices had not undergone clinical trials, highlighting the critical need for more rigorous validation standards [92].
Prospective clinical validation serves as the essential bridge between algorithmic development and clinical implementation, assessing how AI systems perform when making forward-looking predictions rather than identifying patterns in historical data [91]. This approach addresses potential issues of data leakage and overfitting while evaluating performance in actual clinical workflows and measuring impact on clinical decision-making and patient outcomes.
Core Principles and Quantitative Framework
Defining Prospective Clinical Validation
Prospective clinical validation refers to the rigorous assessment of an AI system's performance and clinical utility through planned evaluation in intended clinical settings before routine deployment. Unlike retrospective validation on historical datasets, prospective validation involves testing the AI system on consecutively enrolled patients in real-time or near-real-time clinical workflows, with pre-specified endpoints and statistical analysis plans.
This validation paradigm requires AI systems to demonstrate not only technical accuracy but also clinical effectiveness—measuring how the system impacts diagnostic accuracy, therapeutic decisions, workflow efficiency, and ultimately patient outcomes when integrated into clinical practice.
Key Performance Metrics for AI Clinical Validation
Table 1: Essential Quantitative Metrics for AI System Clinical Validation
| Metric Category | Specific Metrics | Target Threshold | Clinical Significance |
|---|---|---|---|
| Diagnostic Accuracy | Sensitivity, Specificity, AUC-ROC | >0.90 (High-stakes) >0.80 (Moderate) | Diagnostic reliability compared to gold standard |
| Clinical Utility | Diagnostic Time Reduction, Treatment Change Rate, Error Reduction | ≥20% improvement | Tangible clinical workflow benefits |
| Safety Profile | Adverse Event Rate, False Positive/Negative Rate | Non-inferior to standard care | Patient safety assurance |
| Technical Robustness | Failure Rate, Downtime, Processing Speed | <5% failure rate | System reliability in clinical settings |
The validation framework must establish minimum performance thresholds based on the intended use case and clinical context. For high-risk applications such as oncology diagnostics or intensive care monitoring, more stringent criteria apply, often requiring performance that exceeds current clinical standards or demonstrates substantial clinical improvement [91] [93].
Experimental Design and Methodological Protocols
Randomized Controlled Trial Designs for AI Validation
The need for rigorous validation through randomized controlled trials (RCTs) presents a significant hurdle for technology developers, yet AI-powered healthcare solutions promising clinical benefit must meet the same evidence standards as therapeutic interventions [91]. Adaptive trial designs that allow for continuous model updates while preserving statistical rigor represent viable approaches for evaluating AI technologies in clinical settings.
Table 2: RCT Design Options for AI System Validation
| Trial Design | Implementation Approach | Use Case Scenarios |
|---|---|---|
| Parallel Group RCT | Patients randomized to AI-assisted care vs. standard care | Diagnostic applications, treatment recommendation systems |
| Cluster Randomized | Clinical sites randomized to implement AI tool or not | Workflow optimization tools, clinical decision support systems |
| Stepped-Wedge | Sequential rollout of AI intervention across sites | Implementation science studies, health system adoption |
| Adaptive Enrichment | Modification of enrollment criteria based on interim results | Personalized medicine applications, biomarker-defined subgroups |
Traditional RCTs are often perceived as impractical for AI models due to rapid technological evolution; however, this view must be challenged [91]. Adaptive trial designs, digitized workflows for more efficient data collection and analysis, and pragmatic trial designs all represent viable approaches for evaluating AI technologies in clinical settings.
Technical Validation Protocol: Source-to-Target Data Integrity
Robust technical validation forms the foundation for credible clinical validation. The ETL (Extract, Transform, Load) framework provides a structured approach to data validation throughout the AI pipeline [94].
Figure 1: Technical validation workflow ensuring data integrity throughout AI pipeline.
Effective data validation employs several techniques to maintain quality throughout the pipeline [94]:
- Syntactic Validation: Verifies data follows expected formats (dates, email addresses, phone numbers)
- Semantic Validation: Ensures data makes logical sense within business rules
- Referential Integrity: Confirms relationships between data elements are maintained
- Range Validation: Checks if numeric values fall within acceptable boundaries
Implementation requires both automated and manual validation techniques. Automated components include scheduled validation jobs, comparison scripts that match source and target data counts and values, and notification systems that alert teams when validation failures occur [94].
Clinical Validation Protocol: Prospective Trial Implementation
The clinical validation protocol establishes the methodology for evaluating AI system performance in real-world clinical settings.
Figure 2: Clinical validation protocol for prospective AI system evaluation.
Protocol Development Specifications
- Primary Endpoints: Define clinically meaningful endpoints (e.g., diagnostic accuracy, time to correct diagnosis, treatment change rate)
- Statistical Power Calculation: Determine sample size based on expected effect size and variability
- Inclusion/Exclusion Criteria: Establish patient selection criteria reflecting intended use population
- Randomization Procedure: Implement allocation concealment and balanced randomization
- Blinding Procedures: Maintain blinding of clinicians and outcome assessors where feasible
Implementation Guidelines
Clinical sites should represent diverse care settings to ensure generalizability. The protocol must specify procedures for handling AI system failures, missing data, and protocol deviations. Additionally, predefined statistical analysis plans should include both intention-to-treat and per-protocol analyses.
Regulatory and Compliance Framework
AI Act Compliance Checklist for Clinical Validation
The European Union's Artificial Intelligence Act establishes comprehensive legal requirements for AI systems in healthcare, classifying many medical AI applications as high-risk [93]. Compliance requires systematic assessment and documentation.
Table 3: AI Act Compliance Checklist for Clinical Validation
| Compliance Domain | Validation Requirement | Documentation Evidence |
|---|---|---|
| Technical Documentation | Detailed system specifications, design decisions | Technical file, algorithm description |
| Data Governance | Training data quality, representativeness | Data provenance, preprocessing documentation |
| Clinical Evidence | Prospective clinical validation results | Clinical study report, statistical analysis |
| Human Oversight | Clinician interaction design, override mechanisms | Human-AI interaction protocol, training materials |
| Transparency | Interpretability, decision logic explanation | Model interpretability analysis, output documentation |
| Accuracy and Robustness | Performance metrics, error analysis | Validation report, failure mode analysis |
| Cybersecurity | Data protection, system security | Security testing report, vulnerability assessment |
The AI Act mandates specific transparency obligations for AI systems that interact with humans or generate synthetic content [93]. For high-risk AI systems, which include many medical devices, the regulation introduces requirements for data governance, technical documentation, human oversight, and post-market monitoring.
Regulatory Pathway Selection Strategy
The appropriate regulatory pathway depends on the AI system's intended use, risk classification, and claimed indications. The FDA's 510(k) pathway, which does not always require prospective human testing, has been associated with higher recall rates for AI-enabled devices [92]. For novel AI systems with significant algorithmic claims, the Premarket Approval (PMA) pathway with prospective clinical trials provides more robust evidence generation.
The INFORMED (Information Exchange and Data Transformation) initiative at the FDA serves as a blueprint for regulatory innovation, functioning as a multidisciplinary incubator for deploying advanced analytics across regulatory functions [91]. This model demonstrates the value of creating protected spaces for experimentation within regulatory agencies to address the complexity of modern biomedical data and AI-enabled innovation.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Platforms for AI Clinical Validation
| Tool Category | Specific Solutions | Research Application |
|---|---|---|
| Data Validation Frameworks | Great Expectations, dbt (data build tool), Apache NiFi | Automated data quality checking, pipeline validation |
| Clinical Trial Management | REDCap, Medidata Rave, OpenClinica | Patient recruitment, data collection, protocol management |
| Statistical Analysis | R Statistical Software, Python SciPy, SAS | Power calculation, interim analysis, endpoint evaluation |
| Regulatory Documentation | eCTD Submission Systems, DocuSign | Protocol submission, safety reporting, approval tracking |
| AI Literacy Platforms | Custom LMS, Coursera, edX | Staff training, competency documentation, compliance tracking |
Implementation of these tools requires integration with existing clinical workflows and EHR systems. The selection process should prioritize solutions with robust validation features, audit trails, and regulatory compliance capabilities [94] [93].
Prospective clinical validation represents the unequivocal standard for establishing AI system efficacy and safety in clinical practice. The framework presented in this document provides a structured approach to designing, implementing, and documenting robust validation studies that meet evolving regulatory requirements and clinical evidence standards. As the field matures, successful adoption will depend on interdisciplinary collaboration between data scientists, clinical researchers, regulatory affairs specialists, and healthcare providers. By embracing rigorous prospective validation methodologies, the drug development community can fully realize AI's potential to transform therapeutic development while ensuring patient safety and regulatory compliance.
Designing Randomized Controlled Trials (RCTs) for AI Model Validation
The integration of Artificial Intelligence (AI) into drug development and clinical practice represents a transformative shift, yet its full potential remains constrained by a significant validation gap. While AI demonstrates promising technical capabilities in target identification, biomarker discovery, and clinical trial optimization, most systems remain confined to retrospective validations and pre-clinical settings, seldom advancing to prospective evaluation or integration into critical decision-making workflows [91]. This gap is not merely technological but reflects deeper systemic issues within the validation ecosystem and regulatory framework governing AI technologies.
The validation of AI models demands a paradigm shift from traditional software testing toward evidence generation methodologies that account for AI's unique characteristics—adaptability, complexity, and data-dependence. Randomized Controlled Trials (RCTs) represent the gold standard for demonstrating clinical efficacy and have become an imperative for AI systems impacting clinical decisions or patient outcomes [91]. For AI models claiming transformative or disruptive clinical impact, comprehensive validation through prospective RCTs is essential to justify healthcare integration, mirroring the evidence standards required for therapeutic interventions [91]. This document provides detailed application notes and protocols for designing rigorous RCTs specifically for AI model validation, framed within the broader context of input-output transformation validation methods research.
Experimental Design Principles for AI RCTs
Core Methodological Considerations
Designing RCTs for AI validation requires careful consideration of several methodological factors that distinguish them from conventional therapeutic trials. The fundamental principle involves comparing outcomes between patient groups managed with versus without the AI intervention, with random allocation serving to minimize confounding [95].
Randomization and Blinding: Cluster randomization is often preferable to individual-level randomization when the AI intervention operates at an institutional level or when there is high risk of contamination between study arms. For instance, randomizing clinical sites rather than individual patients to AI-assisted diagnosis versus standard care prevents cross-group influence that could bias results [96]. Blinding presents unique challenges in AI trials, particularly when the intervention involves noticeable human-AI interaction. While patients can often be blinded to their allocation group, clinician users typically cannot. This necessitates robust objective endpoint assessment by blinded independent endpoint committees to maintain trial integrity [97].
Control Group Design: Selection of appropriate controls must reflect the AI's intended use case. Placebo-controlled designs are suitable when no effective alternative exists, while superiority or non-inferiority designs against active comparators are appropriate when benchmarking against established standards of care [96]. The control should represent current best practice rather than a theoretical baseline, ensuring the trial assesses incremental clinical value rather than just technical performance [91].
Endpoint Selection: AI validation trials should employ endpoints that capture both technical efficacy and clinical utility. Traditional performance metrics (accuracy, precision, recall) must be supplemented with clinically meaningful endpoints relevant to patients, clinicians, and healthcare systems [98]. Composite endpoints may be necessary to capture the multidimensional impact of AI interventions on diagnostic accuracy, treatment decisions, and ultimately patient outcomes [97].
Table 1: Key Considerations for AI RCT Endpoint Selection
| Endpoint Category | Examples | Use Case | Regulatory Significance |
|---|---|---|---|
| Technical Performance | AUC-ROC, F1-score, Mean Absolute Error | Early-phase validation, Algorithm refinement | Necessary but insufficient for clinical claims |
| Clinical Workflow | Time to diagnosis, Resource utilization, Adherence to guidelines | Process optimization, Decision support | Demonstrates operational value |
| Patient-Centered Outcomes | Mortality, Morbidity, Quality of Life, Hospital readmission | Therapeutic efficacy, Prognostication | Highest regulatory evidence for clinical benefit |
Specialized Trial Designs for AI Validation
Adaptive trial designs enhanced by AI methodologies offer efficient approaches to validation, particularly valuable when rapid iteration is required or patient populations are limited [95]. These designs allow pre-planned, real-time modifications to trial protocols based on interim results, ensuring resources focus on the most promising applications.
Bayesian Adaptive Designs: These incorporate accumulating evidence to update probabilities of treatment effects, potentially reducing sample size requirements and enabling more efficient resource allocation. Reinforcement learning algorithms can be aligned with Bayesian statistical thresholds by incorporating posterior probability distributions into learning loops, maintaining type I error control while adapting allocation ratios [95].
Digital Twin Applications: Digital twins (DTs)—dynamic virtual representations of individual patients created through integration of real-world data and computational modeling—enable innovative trial architectures including synthetic control arms [95]. By simulating patient-specific responses, DTs can enhance treatment precision while addressing ethical concerns about randomization to control groups. Validation of DT approaches requires quantitative comparison between predicted and actual patient outcomes using survival concordance indices, RMSE, or calibration curves [95].
Table 2: Adaptive Trial Designs for AI Validation
| Design Type | Key Features | AI Applications | Implementation Considerations |
|---|---|---|---|
| Group Sequential | Pre-specified interim analyses with stopping rules for efficacy/futility | Early validation of AI diagnostic accuracy | Requires careful alpha-spending function planning |
| Platform Trials | Master protocol with multiple simultaneous interventions against shared control | Comparing multiple AI algorithms or versions | Complex operational logistics but efficient for iterative AI development |
| Bucket Trials | Modular protocol structure with interchangeable components | Testing AI across different patient subgroups or clinical contexts | Flexible but requires sophisticated statistical oversight |
Implementation Protocols: SPIRIT-AI Extension Framework
The SPIRIT-AI (Standard Protocol Items: Recommendations for Interventional Trials–Artificial Intelligence) extension provides evidence-based recommendations for clinical trial protocols evaluating interventions with an AI component [97]. Developed through international consensus involving multiple stakeholders, SPIRIT-AI includes 15 new items that should be routinely reported in addition to the core SPIRIT 2013 items.
AI Intervention Specification
Complete Software Description: The trial protocol must provide a complete description of the AI intervention, including the algorithm name, version, and type (e.g., deep learning, random forest). Investigators should specify the data used for training and tuning the model, including details on the dataset composition, preprocessing steps, and any data augmentation techniques employed [97]. The intended use and indications, including intended user(s), should be explicitly defined, along with the necessary hardware requirements for deployment.
Instructions for Use and Interaction: Detailed instructions for using the AI system are essential, including the necessary input data, steps for operation, and interpretation of outputs [97]. The nature of the human-AI interaction must be clearly described—specifying whether the system provides autonomous decisions or supportive recommendations, and delineating how disagreements between AI and clinician judgments should be handled during the trial.
Setting and Integration: The clinical setting in which the AI intervention will be implemented should be described, including the necessary infrastructure and workflow modifications required [97]. Protocol developers should outline plans for handling input data quality issues and output data interpretation, including safety monitoring procedures for erroneous predictions and contingency plans for system failures.
Validation and Error Analysis Framework
Prospective validation is essential for assessing how AI systems perform when making forward-looking predictions rather than identifying patterns in historical data [91]. This process addresses potential issues of data leakage or overfitting that may not be apparent in controlled retrospective evaluations.
Error Case Analysis: The trial protocol should pre-specify plans for analyzing incorrect AI outputs and performance variations across participant subgroups [97]. This includes statistical methods for assessing robustness across different clinical environments and patient populations, with particular attention to underrepresented groups in the training data.
Continuous Learning Protocols: For AI systems with adaptive capabilities, the protocol must detail the conditions and processes for model updates during the trial, including methods for preserving internal validity while allowing for system improvement [97]. This includes specifying the frequency of updates, validation procedures for modified algorithms, and statistical adjustments for performance assessment.
The following workflow diagram illustrates the key stages in implementing an AI RCT according to SPIRIT-AI guidelines:
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of AI RCTs requires specialized methodological resources and analytical tools. The following table details key "research reagent solutions" essential for implementing robust validation frameworks.
Table 3: Essential Research Reagents for AI RCTs
| Category | Specific Tools/Resources | Function in AI Validation | Implementation Notes |
|---|---|---|---|
| Reporting Guidelines | SPIRIT-AI & CONSORT-AI [97] | Ensure complete and transparent reporting of AI-specific trial elements | Mandatory for high-impact journal submission; improves methodological rigor |
| Statistical Analysis Frameworks | Bayesian adaptive designs, Group sequential methods [95] | Maintain statistical power while allowing pre-planned modifications | Requires specialized statistical expertise; protects type I error |
| Bias Assessment Tools | Fairness metrics (demographic parity, equality of opportunity) [98] | Quantify performance disparities across patient subgroups | Essential for regulatory compliance; demonstrates generalizability |
| Digital Twin Technologies | Mechanistic models, Synthetic control arms [95] | Create virtual patients for simulation and control group generation | Reduces recruitment challenges; enables n-of-1 trial designs |
| Performance Monitoring Systems | Drift detection algorithms, Model performance dashboards [98] | Identify performance degradation during trial implementation | Enables continuous validation; alerts to data quality issues |
| AI Agent Frameworks | ClinicalAgent, MAKAR [95] | Autonomous coordination across clinical trial lifecycle | Improves trial efficiency; handles complex eligibility reasoning |
Regulatory and Implementation Considerations
Regulatory Innovation and Evidence Requirements
Regulatory frameworks for AI validation are evolving to accommodate the unique characteristics of software-based interventions. The FDA's Information Exchange and Data Transformation (INFORMED) initiative exemplified a novel approach to driving regulatory innovation, functioning as a multidisciplinary incubator for deploying advanced analytics across regulatory functions [91]. This model demonstrates the value of creating protected spaces for experimentation within regulatory agencies while maintaining rigorous oversight.
Evidence Generation Pathways: Regulatory acceptance of AI systems typically requires demonstration of both analytical validity (technical performance) and clinical validity (correlation with clinical endpoints) [91]. For systems influencing therapeutic decisions, clinical utility (improvement in health outcomes) represents the highest evidence standard. The required level of validation directly correlates with the proposed claims and intended use—with more comprehensive evidence needed for autonomous systems versus those providing supportive recommendations [97].
Real-World Performance Monitoring: Post-market surveillance and real-world performance monitoring are increasingly required components of AI validation frameworks [98]. Continuous validation protocols should establish triggers for model retraining or protocol modifications based on performance drift, with clearly defined thresholds for intervention [98].
Case Study: Autonomous AI Agent in Oncology
A recent development and validation of an autonomous AI agent for clinical decision-making in oncology demonstrates the application of rigorous validation methodologies [5]. The system integrated GPT-4 with multimodal precision oncology tools, including vision transformers for detecting microsatellite instability and KRAS/BRAF mutations from histopathology slides, MedSAM for radiological image segmentation, and web-based search tools including OncoKB, PubMed, and Google [5].
In validation against 20 realistic multimodal patient cases, the AI agent demonstrated 87.5% accuracy in autonomous tool selection, reached correct clinical conclusions in 91.0% of cases, and accurately cited relevant oncology guidelines 75.5% of the time [5]. Compared to GPT-4 alone, the integrated AI agent drastically improved decision-making accuracy from 30.3% to 87.2%, highlighting the importance of domain-specific tool integration beyond general-purpose language models [5].
This case study illustrates several key principles for AI RCT design: (1) the importance of multimodal data integration, (2) the value of benchmarking against both human performance and baseline algorithms, and (3) the necessity of real-world clinical simulation beyond technical metric evaluation.
Designing randomized controlled trials for AI model validation requires specialized methodologies that address the unique challenges of software-based interventions while maintaining the evidentiary standards expected in clinical research. The SPIRIT-AI and CONSORT-AI frameworks provide essential guidance for protocol development and reporting, emphasizing complete description of AI interventions, their integration into clinical workflows, and comprehensive error analysis [97]. As AI systems grow more sophisticated and autonomous, validation methodologies must similarly evolve—incorporating adaptive designs, digital twin technologies, and continuous monitoring approaches that maintain scientific rigor while accommodating rapid technological advancement [95]. Through rigorous validation frameworks that demonstrate both technical efficacy and clinical utility, AI systems can fulfill their potential to transform drug development and patient care.
- Introduction: Overview of input-output transformation validation and its importance in scientific research.
- Comparative Analysis: Tables comparing verification vs. validation and method validation techniques.
- Experimental Protocols: Detailed methodologies for comparison of methods and design validation.
- Visualization: Workflow diagrams for validation processes.
- Research Reagent Solutions: Table of essential materials and their functions.
Comparative Analysis of Validation Methods: Strengths, Weaknesses, and Use Cases
Input-output transformation validation represents a fundamental framework for ensuring the reliability and accuracy of scientific methods and systems across research and development industries. In regulated sectors such as drug development and medical device manufacturing, rigorous validation methodologies serve as critical gatekeepers for product safety, efficacy, and regulatory compliance. The core concept revolves around systematically verifying that specified inputs, when processed through a defined system or method, consistently produce outputs that meet predetermined requirements and specifications while fulfilling intended user needs. This approach encompasses both design verification (confirming that outputs meet input specifications) and design validation (confirming that the resulting product meets user needs and intended uses), forming a comprehensive validation strategy essential for scientific integrity and regulatory approval.
The input-process-output (IPO) model, first conceptualized by McGrath in 1964, provides a structured framework for understanding these transformations [99]. In this model, inputs represent the flow of data and materials into the process from outside sources, processing includes all tasks required to transform these inputs, and outputs constitute the data and materials flowing outward from the transformation process. Within life sciences and pharmaceutical development, validation methodologies must address increasingly complex analytical techniques, manufacturing processes, and product development pipelines while navigating stringent regulatory landscapes. This application note examines prominent validation methodologies, their comparative strengths and limitations, detailed experimental protocols, and essential research reagents, providing researchers and drug development professionals with practical guidance for implementing robust validation frameworks within their organizations.
Comparative Analysis of Validation Methods
Fundamental Validation Concepts: Verification vs. Validation
Design verification and design validation represent two distinct but complementary stages within design controls, often confused despite their different objectives and applications. Design verification answers the question "Did we design the device right?" by confirming that design outputs meet design inputs, while design validation addresses "Did we design the right device?" by proving the device's design meets specified user needs and intended uses [100]. For instance, a user need for one-handed device operation would generate multiple design inputs related to size, weight, and ergonomics. Verification would check that design outputs (drawings, specifications) meet these inputs, while validation would demonstrate that users can actually operate the device with one hand to fulfill its intended use. It is entirely possible to have design outputs perfectly meeting design inputs while resulting in a device that fails to meet user needs, necessitating both processes.
Table 1: Comparison of Design Verification vs. Design Validation
| Aspect | Design Verification | Design Validation |
|---|---|---|
| Primary Question | "Did we design the device right?" | "Did we design the right device?" |
| Focus | Design outputs meet design inputs | Device meets user needs and intended uses |
| Basis | Examination of objective evidence against specifications | Proof of device meeting user needs |
| Methods | Testing, inspection, analysis | Clinical evaluation, simulated/actual use |
| Timing | Throughout development process | Late stage with initial production units |
| Specimens | Prototypes, components | Initial production units from production environment |
Method Validation Techniques
Various analytical validation methods serve specific purposes in assessing method performance characteristics, each with distinct strengths, weaknesses, and optimal use cases. The comparison of methods experiment is particularly critical for assessing systematic errors that occur with real patient specimens, estimating inaccuracy by analyzing patient samples by both new and comparative methods [101]. This approach requires careful selection of a comparative method, with "reference methods" of documented correctness being preferred over routine methods whose correctness may not be thoroughly established. For methods expected to show one-to-one agreement, difference plots displaying test minus comparative results versus comparative results visually represent systematic errors, while comparison plots displaying test results versus comparison results illustrate relationships between methods not expected to show one-to-one agreement.
Table 2: Analytical Method Validation Techniques Comparison
| Method | Strengths | Weaknesses | Optimal Use Cases |
|---|---|---|---|
| Comparison of Methods | Estimates systematic error with real patient specimens, identifies constant/proportional errors | Dependent on quality of comparative method, requires minimum 40 specimens | Method comparisons against reference methods, assessing clinical acceptability |
| Regression Analysis | Quantifies relationships between variables, predicts outcomes based on relationships | Relies on linearity, independence, and normality assumptions; correlation doesn't prove causation | Forecasting outcomes, understanding variable influence in business, economics, biology |
| Monte Carlo Simulation | Quantifies uncertainty, assesses risks, provides outcome range, models complex systems | Computationally intensive, depends on input distribution accuracy | Financial modeling, system reliability, project risk analysis, environmental predictions |
| Factor Analysis | Data reduction, identifies underlying structures (latent variables), simplifies complex datasets | Subjective interpretation, assumes linearity and adequate sample size | Psychology (personality studies), marketing (consumer traits), finance (portfolio construction) |
| Cohort Analysis | Identifies group-specific trends/behaviors, more detailed than general analytics | Limited to groups with shared characteristics, requires longitudinal tracking | User behavior analysis, customer retention studies, lifecycle pattern identification |
For comparison of methods experiments, a minimum of 40 patient specimens carefully selected to cover the entire working range of the method is recommended, with the quality of specimens being more critical than quantity [101]. These specimens should represent the spectrum of diseases expected in routine method application. While single measurements are common practice, duplicate measurements provide a validity check by identifying problems from sample mix-ups, transposition errors, and other mistakes. The experiment should span multiple analytical runs on different days (minimum 5 days recommended) to minimize systematic errors that might occur in a single run, with specimens typically analyzed within two hours of each other unless stability data supports longer intervals.
Experimental Protocols
Protocol: Comparison of Methods Experiment
Purpose: This protocol estimates the systematic error or inaccuracy between a new test method and a comparative method through analysis of patient specimens. The systematic differences at critical medical decision concentrations constitute the primary errors of interest, with additional information about the constant or proportional nature of the systematic error derived from statistical calculations.
Materials and Equipment:
- Minimum 40 patient specimens covering entire analytical measurement range
- Test method instrumentation and reagents
- Comparative method instrumentation and reagents
- Data collection and analysis system (spreadsheet or statistical software)
Procedure:
- Specimen Selection: Select 40+ patient specimens representing the entire working range of the method and spectrum of diseases expected in routine application.
- Experimental Design: Analyze specimens by both test and comparative methods within 2 hours of each other to minimize stability issues. Include several analytical runs across different days (minimum 5 days).
- Data Collection: Record all results immediately, noting any discrepancies or unusual observations.
- Initial Data Review: Graph results using difference plots (for methods expected to show one-to-one agreement) or comparison plots (for methods not expected to show one-to-one agreement).
- Discrepant Result Handling: Identify and reanalyze specimens with large differences while specimens are still available to confirm differences are real.
- Statistical Analysis: Calculate appropriate statistics based on data characteristics:
- For wide analytical ranges: Linear regression statistics (slope, intercept, standard error of estimate)
- For narrow analytical ranges: Paired t-test calculations (average difference, standard deviation of differences)
- Systematic Error Estimation: For regression analysis, calculate systematic error at critical medical decision concentrations (Xc) using: Yc = a + bXc, then SE = Yc - Xc.
- Acceptability Assessment: Compare estimated systematic errors to established acceptability criteria based on clinical requirements.
Quality Control Considerations: Specimen handling must be carefully defined and systematized prior to beginning the study to ensure differences observed result from analytical errors rather than specimen handling variables. When using routine methods as comparative methods (rather than reference methods), additional experiments such as recovery and interference studies may be necessary to resolve discrepancies when differences are large and medically unacceptable [101].
Protocol: Design Validation for User Needs
Purpose: This protocol validates that a device's design meets specified user needs and intended uses under actual or simulated use conditions, proving that the right device has been designed rather than merely verifying that the device was designed right [100].
Materials and Equipment:
- Initial production units manufactured in production environment
- Production personnel, equipment, and specifications
- Actual or simulated use environment
- Representative end-users
- Documentation system for objective evidence
Procedure:
- Unit Selection: Utilize initial production units built in the production environment using approved drawings, specifications, and procedures by production personnel.
- End-user Involvement: Engage representative end-users who reflect the target user population, including relevant demographic and experience characteristics.
- Environmental Conditions: Conduct validation under specific intended environmental conditions, including any changing conditions the device might encounter during normal use.
- Testing Scope: Include the entire medical device system, including hardware, software, labeling, instructions for use, packaging, and all components within packaging.
- Clinical Evaluation: Perform testing under simulated use or actual use conditions, comparing device performance against appropriate benchmarks with similar purposes.
- Data Collection: Document all results, observations, and user feedback as objective evidence of validation.
- Analysis: Evaluate whether collected evidence demonstrates that user needs and intended uses are consistently fulfilled.
- Acceptance Criteria: Determine validation success based on predetermined criteria aligned with user needs specifications.
Quality Control Considerations: Design validation must be comprehensive, addressing all aspects of the device as used in the intended environment. When validation reveals deficiencies, design changes must be implemented and verified, followed by re-validation to ensure issues are resolved. This process applies throughout the product lifecycle, including post-market updates necessitated by feedback, nonconformances, or corrective and preventive actions (CAPA) [100].
Visualization
Input-Output Transformation Validation Workflow
Input-Output Transformation Validation Workflow Diagram
Comparison of Methods Experimental Protocol
Comparison of Methods Experimental Protocol
Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Validation Studies
| Research Reagent/Material | Function/Purpose in Validation |
|---|---|
| Patient Specimens | Provide real-world matrix for method comparison studies, assessing analytical performance across biological variation [101] |
| Reference Materials | Serve as certified standards with documented correctness for comparison studies, establishing traceability [101] |
| Quality Control Materials | Monitor analytical performance stability throughout validation studies, detecting systematic shifts or increased random error |
| Statistical Analysis Software | Perform regression analysis, difference plots, paired t-tests, and calculate systematic errors at decision points [101] |
| Production Equipment & Personnel | Generate initial production units using final specifications for design validation studies [100] |
| Contrast Checking Tools | Verify visual accessibility of interfaces, ensuring compliance with WCAG 2.1 contrast requirements (4.5:1 for normal text) [102] |
| Clinical Evaluation Platforms | Facilitate simulated or actual use testing with representative end-users for design validation studies [100] |
Statistical Hypothesis Testing for Model and System Performance
In the field of drug development, the validation of computer simulation models through statistical hypothesis testing is a critical process for ensuring model credibility and regulatory acceptance. Model validation is defined as the "substantiation that a computerized model within its domain of applicability possesses a satisfactory range of accuracy consistent with the intended application of the model" [103]. With the U.S. Food and Drug Administration (FDA) increasingly receiving submissions with AI components—over 500 from 2016 to 2023—the establishment of robust statistical frameworks for model validation has become paramount [17] [32]. The FDA's 2025 draft guidance on artificial intelligence emphasizes a risk-based credibility framework where a model's context of use (COU) determines the necessary level of evidence, with statistical hypothesis testing serving as a fundamental tool for demonstrating model accuracy [104] [105].
This document outlines application notes and experimental protocols for employing statistical hypothesis testing in the validation of model input-output transformations, particularly within the pharmaceutical and drug development sectors. The focus is on practical implementation of these statistical methods to determine whether a model's performance adequately represents the real-world system it imitates, thereby supporting regulatory decision-making for drug safety, effectiveness, and quality [103] [104].
Statistical Foundation of Hypothesis Testing for Validation
Statistical hypothesis testing provides a structured, probabilistic framework for deciding whether observed data provide sufficient evidence to reject a specific hypothesis about a population [106] [107]. In model validation, this methodology is applied to test the fundamental question: Does the simulation model adequately represent the real system? [103]
Core Hypotheses for Model Validation
For model validation, the typical null hypothesis ((H0)) and alternative hypothesis ((H1)) are formulated as follows [103]:
- (H0): The model's measure of performance equals the system's measure of performance ((μm = μ_s))
- (H1): The model's measure of performance does not equal the system's measure of performance ((μm ≠ μ_s))
The test statistic for this validation test, typically following a t-distribution, is calculated as [103]:
[ t0 = \frac{(E(Y) - μ0)}{(S / \sqrt{n})} ]
Where (E(Y)) is the expected value from the model output, (μ_0) is the observed system value, (S) is the sample standard deviation, and (n) is the number of independent model runs.
Decision Framework and Error Considerations
The calculated test statistic is compared against a critical value from the t-distribution with (n-1) degrees of freedom for a chosen significance level (\alpha) (typically 0.05). If (|t0| > t{\alpha/2,n-1}), the null hypothesis is rejected, indicating the model needs adjustment [103].
Two types of error must be considered in this decision process [103]:
- Type I Error ((\alpha)): Rejecting a valid model ("model builder's risk")
- Type II Error ((\beta)): Accepting an invalid model ("model user's risk")
The probability of correctly detecting an invalid model ((1-\beta)) is particularly important for patient safety in drug development applications [103].
Quantitative Data Presentation
Common Statistical Tests for Model Validation
Table 1: Statistical Tests for Model Validation
| Test Statistic | Type of Test | Common Application in Model Validation | Key Assumptions |
|---|---|---|---|
| t-statistic | t-test [106] | Comparing means of model output vs. system data [103] | Normally distributed data, independent observations |
| F-statistic | ANOVA [106] | Comparing multiple model configurations or scenarios | Normally distributed data, homogeneity of variance |
| χ²-statistic | Chi-square test [106] | Testing distribution assumptions or categorical data fit | Large sample size, independent observations |
Performance Metrics for AI/ML Models in Drug Development
Table 2: Essential Performance Metrics for AI Model Validation
| Metric Category | Specific Metrics | Target Values | Context of Use |
|---|---|---|---|
| Accuracy Metrics | MAE, RMSE, MAPE | COU-dependent [104] | Continuous output models |
| Classification Metrics | Sensitivity, Specificity, Precision, F1-score | >0.8 (high-risk) [105] | Binary classification models |
| Agreement Metrics | Cohen's Kappa, ICC | >0.6 (moderate) [103] | Inter-rater reliability |
| Bias & Fairness | Subgroup performance differences | <10% degradation [105] | All patient-facing models |
Experimental Protocols
Protocol 1: T-Test for Model-System Comparison
Purpose and Scope
This protocol describes the procedure for comparing model output to system data using a statistical t-test, suitable for validating continuous output measures in clinical trial simulations or pharmaceutical manufacturing models [103].
Materials and Equipment
- Independent validation dataset from real system
- Computational resources for model execution
- Statistical software (R, Python, or equivalent)
Procedure
- Define Performance Measure: Identify the specific model output variable of interest for validation (e.g., average patient wait time, drug response rate) [103]
- Collect System Data: Record corresponding output measures from the actual system under the same input conditions
- Execute Model Runs: Conduct (n) statistically independent runs of the model using the same input conditions as system data collection
- Calculate Test Statistic:
- Compute sample mean ((E(Y))) and standard deviation ((S)) from model outputs
- Calculate the observed system mean ((μ_0))
- Compute (t0 = \frac{(E(Y) - μ0)}{(S / \sqrt{n})}) [103]
- Determine Critical Value: Obtain (t_{\alpha/2,n-1}) from t-distribution tables
- Decision Rule: If (|t0| > t{\alpha/2,n-1}), reject (H_0) and conclude model needs adjustment
Data Analysis and Interpretation
For the memantine cognitive function example [108], with:
- Model mean ((E(Y))) = 0.0
- System mean ((μ_0)) = 0.87
- Standard deviation ((S)) = 3.19
- Sample size ((n)) = 45
The test statistic is calculated as (t_0 = -1.83), with a corresponding p-value of 0.0336. At (\alpha = 0.05), this statistically significant result suggests the model outputs differ from system data [108].
Protocol 2: Confidence Interval Approach for Model Accuracy
Purpose and Scope
This protocol uses confidence intervals to determine if a model is "close enough" to the real system, particularly useful when small, clinically insignificant differences are acceptable [103].
Procedure
- Define Acceptable Margin: Establish the acceptable difference ((\epsilon)) between model and system through subject matter expert input
- Generate Model Outputs: Conduct multiple independent model runs
- Construct Confidence Interval:
- Calculate sample mean ((E(Y))) and standard error ((S/\sqrt{n}))
- Determine (t_{\alpha/2,n-1}) from t-distribution
- Compute interval: ([E(Y) - t{\alpha/2,n-1}S/\sqrt{n}, E(Y) + t{\alpha/2,n-1}S/\sqrt{n}]) [103]
- Decision Rules:
- If entire interval falls within (\pm\epsilon) of system value: model acceptable
- If entire interval falls outside (\pm\epsilon): model requires calibration
- If interval straddles boundary: inconclusive; additional data needed
Workflow Visualization
Hypothesis Testing Validation Workflow
Risk-Based AI Validation Framework
The Scientist's Toolkit
Research Reagent Solutions for Model Validation
Table 3: Essential Resources for Statistical Validation of Models
| Tool Category | Specific Tool/Resource | Function | Implementation Example |
|---|---|---|---|
| Statistical Software | R Statistical Environment [107] | Comprehensive statistical analysis and hypothesis testing | t.test(high_sales, low_sales, alternative="greater") |
| Statistical Software | Python SciPy Library [107] | Statistical testing and numerical computations | stats.ttest_ind(perf4, perf1, equal_var=False) |
| Data Management | Versioned Dataset Registry [105] | Maintain data lineage and reproducibility | Immutable data storage with complete metadata |
| Validation Frameworks | FDA AI Validation Guidelines [104] | Risk-based credibility assessment | Context of Use (COU) mapping to evidence requirements |
| Bias Assessment | Subgroup Performance Analysis [105] | Detect and mitigate model bias | Performance comparison across demographic strata |
| Model Monitoring | Predetermined Change Control Plans [105] | Manage model updates and drift | Automated validation tests for model retraining |
Statistical hypothesis testing provides a rigorous, evidence-based framework for establishing the credibility of simulation models in drug development. By implementing the protocols and workflows outlined in this document, researchers and drug development professionals can generate the necessary evidence to demonstrate model validity to regulatory agencies. The integration of these statistical methods within a risk-based framework, as advocated in the FDA's 2025 draft guidance, ensures that models used in critical decision-making for drug safety, effectiveness, and quality are properly validated for their intended context of use [104] [105]. As AI and computational models continue to transform pharmaceutical development, robust statistical validation practices will remain essential for maintaining scientific rigor and regulatory compliance.
Benchmarking Against Known Datasets and Historical Data
Application Notes
The Critical Role of Benchmarking in Predictive Model Validation
In regulated industries such as drug development, benchmarking against known datasets and historical data provides the scientific evidence required to demonstrate that predictive models maintain performance when applied to new data sources. External validation is a crucial step in the model deployment lifecycle, as performance often deteriorates when models encounter data from different healthcare facilities, geographical regions, or patient populations [109]. This degradation has been demonstrated in widely implemented clinical models, including the Epic Sepsis Model and various stroke risk scores [109]. Benchmarking transforms model validation from a regulatory checkbox into a meaningful assessment of real-world reliability and transportability.
A significant innovation in benchmarking methodologies enables the estimation of external model performance using only external summary statistics without requiring access to patient-level data [109]. This approach assigns weights to the internal cohort units to reproduce a set of external statistics, then computes performance metrics using the labels and model predictions of the internally weighted units [109]. This methodology substantially reduces the overhead of external validation, as obtained statistics can be repeatedly used to estimate the external performance of multiple models, accelerating the deployment of robust predictive tools in pharmaceutical development and clinical practice.
Integration with Structured Quality Frameworks
Integrating benchmarking activities within established quality frameworks like Six Sigma's DMAIC (Define, Measure, Analyze, Improve, Control) enhances methodological rigor [13]. This integration ensures validation activities are data-driven and focused on parameters that genuinely impact product quality. The Control phase aligns perfectly with Continued Process Verification, where statistical process control (SPC) and routine monitoring of critical parameters maintain the validated state throughout the model's lifecycle [13]. This structured approach provides documented evidence that analytical processes operate consistently within established parameters, supporting both internal quality assurance and external regulatory inspections.
Performance Estimation Accuracy Across Metrics
Table 1: Accuracy of external performance estimation method across different metrics [109]
| Performance Metric | 95th Error Percentile | Median Estimation Error (IQR) | Median Internal-External Absolute Difference (IQR) |
|---|---|---|---|
| AUROC (Discrimination) | 0.03 | 0.011 (0.005–0.017) | 0.027 (0.013–0.055) |
| Calibration-in-the-large | 0.08 | 0.013 (0.003–0.050) | 0.329 (0.167–0.836) |
| Brier Score (Overall Accuracy) | 0.0002 | 3.2⋅10⁻⁵ (1.3⋅10⁻⁵–8.3⋅10⁻⁵) | 0.012 (0.0042–0.018) |
| Scaled Brier Score | 0.07 | 0.008 (0.001–0.022) | 0.308 (0.167–0.440) |
Impact of Sample Size on Estimation Accuracy
Table 2: Effect of internal and external sample sizes on estimation algorithm performance [109]
| Sample Size | Algorithm Convergence Rate | Estimation Error Variance | Key Observations |
|---|---|---|---|
| 1,000 units | Fails in most cases | N/A | Insufficient for reliable estimation |
| 2,000 units | Fails in some cases | High | Marginal reliability |
| ≥250,000 units | Consistent convergence | Low (optimal) | Stable and accurate estimations |
Experimental Protocols
Purpose: To estimate predictive model performance in external data sources using only limited descriptive statistics without accessing patient-level external data.
Materials:
- Internally trained predictive model
- Internal cohort with unit-level data (features and outcomes)
- External summary statistics (population characteristics, outcome prevalence)
Procedure:
- Define Target Cohort: Identify patients matching the model's intended use case in both internal and external data sources (e.g., patients with pharmaceutically-treated depression) [109].
- Train Internal Models: Develop prediction models for target outcomes (e.g., diarrhea, fracture, GI hemorrhage, insomnia, seizure) using the internal data source [109].
- Extract External Statistics: Obtain population-level statistics from external cohorts, focusing on features with non-negligible model importance [109].
- Calculate Weighting Scheme: Apply optimization algorithm to assign weights to internal cohort units that reproduce the external statistics.
- Success Criterion: External statistics must be representable as a weighted average of the internal cohort's features [109].
- Compute Estimated Metrics: Calculate performance metrics (AUROC, calibration, Brier scores) using the labels and model predictions of the weighted internal units [109].
- Validation: Compare estimated performance measures against actual performance obtained by testing models in external cohorts with full data access.
Technical Notes:
- Feature Selection: Use statistics of features with non-negligible model importance for weighting [109].
- Algorithm Failure: Occurs when certain external statistics cannot be represented in the internal cohort (e.g., missing demographic subgroups) [109].
- Sample Size Considerations: Internal sample size has more pronounced impact on estimation accuracy than external sample size [109].
Protocol: Process Validation Lifecycle for Predictive Models
Purpose: To establish scientific evidence that a predictive modeling process is capable of consistently delivering reliable performance throughout its operational lifecycle.
Materials:
- Process validation master plan
- Defined critical quality attributes (CQAs) and critical process parameters (CPPs)
- Statistical analysis software with capability analysis functions
- Design of Experiments (DOE) software
- Documentation system for validation protocols and reports
Procedure: Stage 1: Process Design
- Identify Critical Quality Attributes (CQAs) that directly impact model performance and safety [13].
- Determine Critical Process Parameters (CPPs) that affect these attributes using Design of Experiments (DOE) [13].
- Conduct risk assessment using Failure Mode and Effects Analysis (FMEA) to identify potential failure points [13].
- Develop preliminary control strategy based on risk management principles [13].
Stage 2: Process Qualification
- Develop detailed validation protocol specifying test conditions, sample sizes, and acceptance criteria [13].
- Execute validation runs under normal operating conditions [13].
- Apply statistical rigor through appropriate sample size determination and capability analysis (Cp/Cpk) [13].
- Document results in validation report demonstrating process consistency [13].
Stage 3: Continued Process Verification
- Implement ongoing monitoring of key parameters according to established control plan [13].
- Deploy Statistical Process Control (SPC) with control charts (X-bar, R, EWMA) to detect process shifts [13].
- Conduct formal investigations for deviations with root cause analysis and corrective actions [13].
- Perform annual reviews to evaluate overall process performance and validation status [13].
Visualization of Workflows
Performance Estimation Methodology
Process Validation Lifecycle
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential materials and computational tools for benchmarking experiments
| Research Reagent/Tool | Function in Benchmarking | Application Context |
|---|---|---|
| Statistical Characteristics | Enable performance estimation without unit-level data access | External validation when data sharing is restricted [109] |
| Weighting Algorithm | Assigns weights to internal cohort to reproduce external statistics | Core component of performance estimation methodology [109] |
| Harmonized Data Definitions | Standardize data structure, content, and semantics across sources | Reduces burden of redefining model elements for external validation [109] |
| Process Validation Protocol | Specifies test conditions, sample sizes, and acceptance criteria | Formalizes validation activities and ensures regulatory compliance [13] |
| Critical Quality Attributes (CQAs) | Define model characteristics that directly impact performance and safety | Risk-based approach to focus validation on most important aspects [13] |
| Critical Process Parameters (CPPs) | Identify process variables that affect critical quality attributes | Helps determine which parameters must be tightly controlled [13] |
| Statistical Process Control (SPC) | Monitor process stability and detect shifts through control charts | Continued Process Verification stage to maintain validated state [13] |
| Design of Experiments (DOE) | Efficiently explore parameter interactions and effects on quality | Process Design stage to understand parameter relationships [13] |
| Capability Analysis (Cp/Cpk) | Quantify how well a process meets specifications | Statistical rigor in validation activities [13] |
Conclusion
Mastering input-output transformation validation is not merely a technical exercise but a strategic imperative for modern drug development. A layered approach—combining foundational rigor, methodological diversity, proactive troubleshooting, and conclusive comparative validation—is essential for building trustworthy data pipelines and AI models. As the regulatory landscape evolves, exemplified by the EMA's structured framework and the FDA's flexible approach, the ability to generate robust, prospective clinical evidence will separate promising innovations from those that achieve real-world impact. Future success will depend on the pharmaceutical industry's commitment to these validation principles, fostering a culture of quality that accelerates the delivery of safe and effective therapies to patients.
References
- 1. Topic 2 Pharmaceutical analysis data treatment. Validation ... [https://med.libretexts.org/Under_Construction/Drugs_Quality_Control_(Theoretical_foundation_and_practical_application)%3A_The_Coursebook/PART_I._Theory/MODULE_1_GENERAL_QUESTIONS_OF_DRUG_ANALYSIS_AND_QUALITY_CONTROL/Topic_2_Pharmaceutical_analysis_data_treatment._Validation_of_analytical_procedures]
- 2. Data standards in drug discovery: A long way to go [https://www.sciencedirect.com/science/article/abs/pii/S1359644624000047]
- 3. Applying quantitative and systems pharmacology to drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11483046/]
- 4. Systematic literature review of validation methods for AI ... [https://www.sciencedirect.com/science/article/pii/S0164121221001473]
- 5. Development and validation of an autonomous artificial ... [https://www.nature.com/articles/s43018-025-00991-6]
- 6. An open source statistical web application for validation ... [https://www.nature.com/articles/s41598-025-99720-3]
- 7. A Complete Guide to Computer System Validation (CSV) [https://www.qbdgroup.com/en/a-complete-guide-to-computer-system-validation/]
- 8. Test Method Development and Validation in Software ... [https://www.linkedin.com/pulse/test-method-development-validation-software-hardware-medical-bhat-lve9c]
- 9. Input/Output Validation: Best Practices for API ... [https://zuplo.com/learning-center/input-output-validation-best-practices]
- 10. Data validation [https://en.wikipedia.org/wiki/Data_validation]
- 11. 8 Essential Data Validation Techniques for 2025 [https://osher.com.au/blog/data-validation-techniques/]
- 12. A step by step guide to quantitative comparisons in ... [https://finbiosoft.com/a-step-by-step-guide-to-quantitative-comparisons-in-validation-manager/]
- 13. Process Validation in Six Sigma: A Complete Guide [https://www.6sigma.us/process-improvement/process-validation/]
- 14. Artificial Intelligence in Software as a Medical Device [https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-software-medical-device]
- 15. Artificial intelligence | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/about-us/how-we-work/data-regulation-big-data-other-sources/artificial-intelligence]
- 16. Understanding FDA's 2025 Draft Guidance on AI-Enabled ... [https://www.orielstat.com/blog/fda-2025-guidance-ai-enabled-medical-devices/]
- 17. Artificial Intelligence for Drug Development [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 18. Considerations for the Use of Artificial Intelligence [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/considerations-use-artificial-intelligence-support-regulatory-decision-making-drug-and-biological]
- 19. EMA AI Data Integrity Guidelines in Clinical Research [https://justintimegcp.com/ema-ai-data-integrity-guidelines-in-clinical-research/]
- 20. EMA's Annex 22: AI in Pharma Gets a GxP Rulebook [https://www.rephine.com/resources/blog/emas-annex-22-ai-in-pharma-gets-a-gxp-rulebook/]
- 21. FDA AI Guidance 2025: What Life Sciences Must Do Now [https://usdm.com/resources/blogs/fda-ai-guidance-2025-life-sciences-compliance]
- 22. Evaluating AI-enabled Medical Device Performance in ... [https://www.fda.gov/medical-devices/digital-health-center-excellence/request-public-comment-measuring-and-evaluating-artificial-intelligence-enabled-medical-device]
- 23. The difference between verification & validation [https://vantagemedtech.com/do-you-know-the-difference-between-verification-and-validation/]
- 24. Verification Vs. Validation Of Medical Devices [https://synectic.net/verification-vs-validation/]
- 25. Analytical Methodology: Validation, Verification, or ... [https://vicihealthsciences.com/analytical-methodology-validation-verification-qualification/]
- 26. Data quality – The foundation of real-world studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10267987/]
- 27. The 6 Data Quality Dimensions with Examples [https://www.collibra.com/blog/the-6-dimensions-of-data-quality]
- 28. A critical path to safe medicines: Why data integrity matters ... [https://www.quotientsciences.com/blog/critical-path-safe-medicines-why-data-integrity-matters-drug-development]
- 29. PDA 2025: Data Governance and AI's Impact on Drug ... [https://www.biopharminternational.com/view/pda-2025-data-governance-and-ai-s-impact-on-drug-manufacturing]
- 30. Ensuring data integrity: Best practices and strategies in ... [https://www.sciencedirect.com/science/article/pii/S2949866X24001060]
- 31. From Raw Inputs to Polished Outputs: The Art of Testing ... [https://medium.com/@wyaddow/from-raw-inputs-to-polished-outputs-the-art-of-testing-data-transformations-534593f8bad7]
- 32. The future of AI regulation in drug development: a comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598624/]
- 33. Understanding Structural Metadata [https://www.actian.com/blog/data-management/structural-metadata/]
- 34. | tansu-io/tansu | DeepWiki Schema Validation [https://deepwiki.com/tansu-io/tansu/4.2-schema-validation]
- 35. Validation Schemas [https://docs.supervisely.com/data-organization/project-dataset/advanced/validation-schemas]
- 36. Proto File Validator - Validate Buffer Protocol Online Schema [https://jsontotable.org/proto-file-validator/]
- 37. Best Practices for Process Validation in the Pharmaceutical ... [https://www.valgenesis.com/blog/best-practices-for-process-validation-in-the-pharmaceutical-industry]
- 38. Unit Testing vs Integration Testing: Key Differences & ... [https://testlio.com/blog/differences-between-unit-testing-integration-testing/]
- 39. Unit Test vs Integration Test: Key Differences Explained ... [https://supatest.ai/blog/unit-testing-vs-integration-testing]
- 40. Understanding Validation and Technical Transfer, Part I [https://www.biopharminternational.com/view/understanding-validation-and-technical-transfer-part-i]
- 41. Unit Testing vs Integration Testing vs E2E Testing - Shift Asia [https://shiftasia.com/column/unit-integration-e2e-testing-guide/]
- 42. 2025 Integration Testing Handbook: Techniques, Tools, ... [https://dev.to/testwithtorin/2025-integration-testing-handbook-techniques-tools-and-trends-3ebc]
- 43. System Integration Testing: Ultimate Guide with Examples [https://aqua-cloud.io/system-integration-testing/]
- 44. A Basic Guide to IQ, OQ, PQ in FDA-Regulated Industries [https://www.thefdagroup.com/blog/a-basic-guide-to-iq-oq-pq-in-fda-regulated-industries]
- 45. 2025 Trends In Pharmaceutical Analytical Methods ... [https://agnopharma.com/blog/trends-in-pharmaceutical-analytical-methods-development-validation/]
- 46. How to be prepared for Pharmaceutical Validation in 2025 [https://www.gillsprocess.com/blog-1/2024/12/11/how-to-be-prepared-for-pharmaceutical-validation-in-2025]
- 47. Objective criteria for statistical assessments of cross ... [https://pubmed.ncbi.nlm.nih.gov/41147683/]
- 48. A fused deep learning approach to transform drug ... [https://www.nature.com/articles/s42004-025-01712-x]
- 49. Ground Truth Data for AI [https://www.superannotate.com/blog/ground-truth-data-for-ai]
- 50. Golden datasets: Evaluating fine-tuned large language ... [https://sigma.ai/golden-datasets/]
- 51. Re-evaluating experimental validation in the Big Data Era [https://pmc.ncbi.nlm.nih.gov/articles/PMC7903713/]
- 52. Evaluation and Benchmarking of LLM Agents: A Survey [https://arxiv.org/html/2507.21504v1]
- 53. LLM Benchmarking Decoded: Updates In May 2025 [https://empathyfirstmedia.com/llm-benchmarking-decoded-updates-in-may-2025/]
- 54. Ground truth generation and review best practices for ... [https://aws.amazon.com/blogs/machine-learning/ground-truth-generation-and-review-best-practices-for-evaluating-generative-ai-question-answering-with-fmeval/]
- 55. Benchmarking AI Agents in 2025: Top Tools, Metrics & ... [https://metadesignsolutions.com/benchmarking-ai-agents-in-2025-top-tools-metrics-performance-testing-strategies/]
- 56. Generative Benchmarking - Chroma Research [https://research.trychroma.com/generative-benchmarking]
- 57. Top 50 AI Model Benchmarks & Evaluation Metrics (2025 Guide) [https://o-mega.ai/articles/top-50-ai-model-evals-full-list-of-benchmarks-october-2025]
- 58. What is End To End (E2E) Testing: Tools & Example [https://www.browserstack.com/guide/end-to-end-testing]
- 59. Best Practices for End-to-End Testing in 2025 [https://www.bunnyshell.com/blog/best-practices-for-end-to-end-testing-in-2025/]
- 60. E2E Testing - Engineering Fundamentals Playbook [https://microsoft.github.io/code-with-engineering-playbook/automated-testing/e2e-testing/]
- 61. What is a staging environment? (and how to set one up) [https://northflank.com/blog/what-is-a-staging-environment-how-to-set-one-up]
- 62. Survey and perspective on verification, validation, and ... [https://www.nature.com/articles/s41746-025-01447-y]
- 63. Root-mean-square error (RMSE) or mean absolute error ... [https://gmd.copernicus.org/articles/15/5481/2022/]
- 64. Metrics Evaluation: MSE, RMSE, MAE and MAPE [https://medium.com/@jonatasv/metrics-evaluation-mse-rmse-mae-and-mape-317cab85a26b]
- 65. Root Mean Square Error (RMSE) In AI: What You Need To ... [https://arize.com/blog-course/root-mean-square-error-rmse-what-you-need-to-know/]
- 66. MAE, MAPE, MASE and the Scaled RMSE - Paul Morgan [https://www.pmorgan.com.au/tutorials/mae,-mape,-mase-and-the-scaled-rmse/]
- 67. analysis of data from the National Medication Error ... [https://pubmed.ncbi.nlm.nih.gov/40672148/]
- 68. What is Process Capability? Capability Estimates & Studies [https://asq.org/quality-resources/process-capability?srsltid=AfmBOopVCeqb9mkn4uxnA6JGtpXBHZJppq2kms2eyGw2K4Il2jWTfO2h]
- 69. Comprehensive Guide to Capability Analysis for Process ... [https://www.6sigma.us/process-improvement/capability-analysis-for-process-improvement/]
- 70. Process Capability (Cp & Cpk) [https://sixsigmastudyguide.com/process-capability-cp-cpk/]
- 71. 3.4.5. Assessing Process Stability [https://www.itl.nist.gov/div898/handbook/ppc/section4/ppc45.htm]
- 72. Assessing Process Stability: Techniques and Tools [https://www.isixsigma.com/dictionary/stability/]
- 73. Process Capability Analysis Cp, Cpk, Pp, Ppk - A Guide [https://www.1factory.com/quality-academy/guide-process-capability.html]
- 74. What is FMEA? Failure Mode & Effects Analysis [https://asq.org/quality-resources/fmea?srsltid=AfmBOorWk9D5v0omBr8qrijxxdHB3552anK6w_Bmmd15GVWh6rHH01bE]
- 75. Application of Quantitative Criticality Analysis in FMEA [https://accendoreliability.com/application-of-quantitative-criticality-analysis-in-fmea/]
- 76. FMEA in Six Sigma DMAIC Failure Mode and Effect Analysis [https://www.sixsigma-institute.org/Six_Sigma_DMAIC_Process_Improve_Phase_Failure_Mode_Effect_Analysis_FMEA.php]
- 77. Application of failure mode and effects analysis (FMEA) to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8293514/]
- 78. Using failure mode and effects analysis for risk ... [https://www.nature.com/articles/s41598-025-13377-6]
- 79. Overview of Failure Mode and Effects Analysis (FMEA) [https://pmc.ncbi.nlm.nih.gov/articles/PMC10229026/]
- 80. Comprehensive Guide to FMEA Analysis Techniques [https://www.scrut.io/post/guide-to-an-fmea-analysis]
- 81. Customizing FMEA Risk Criteria [https://relyence.com/help/user-guide/customizing-fmea-risk-criteria.html]
- 82. Methods and Tools for Process Validation - Taylor Enterprises [https://variation.com/methods-and-tools-for-process-validation/]
- 83. Design Inputs, Optimization & Reviews [https://cqeacademy.com/cqe-body-of-knowledge/product-process-design/design-inputs-review/]
- 84. Reducing Variation During Design [https://variation.com/reducing-variation-during-design/]
- 85. 10 Popular Test Automation Frameworks In 2025 | GAT [https://www.globalapptesting.com/blog/automation-testing-framework]
- 86. Ultimate Test Automation Tools & Frameworks for 2025 [https://www.techment.com/blog/test-automation-tools-guide-2025/]
- 87. 11 Best AI Test Automation Tools for 2025: The Third Wave [https://testguild.com/7-innovative-ai-test-automation-tools-future-third-wave/]
- 88. Post marketing drug surveillance: Critical for Safer ... [https://lifebit.ai/blog/post-marketing-drug-surveillance/]
- 89. Post-Marketing Surveillance in 2025: Evolving Strategies ... [https://www.vitrana.com/post-marketing-surveillance-in-2025-evolving-strategies-for-real-world-safety-monitoring/]
- 90. Barriers to translating continuous monitoring technologies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639493/]
- 91. AI in Drug Development: Clinical Validation and ... [https://globalforum.diaglobal.org/issue/june-2025/ai-in-drug-development-clinical-validation-and-regulatory-innovation-are-dual-imperatives/]
- 92. Keep an Eye on Clinical Validation Gaps in AI-Enabled ... [https://www.aha.org/aha-center-health-innovation-market-scan/2025-09-16-keep-eye-clinical-validation-gaps-ai-enabled-medical-devices]
- 93. AI policy in healthcare: a checklist-based methodology for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465464/]
- 94. Data Validation in ETL - 2025 Guide [https://www.integrate.io/blog/data-validation-etl/]
- 95. AI and innovation in clinical trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627430/]
- 96. CONSORT 2025 Statement - Reporting guideline [https://www.equator-network.org/reporting-guidelines/consort/]
- 97. Guidelines for clinical trial protocols for interventions ... [https://www.nature.com/articles/s41591-020-1037-7]
- 98. A Step-by-Step Guide to Effective AI Model Validation [https://galileo.ai/blog/ai-model-validation]
- 99. Must-have Input Process Output Diagram Templates ... [https://www.slideteam.net/blog/must-have-input-process-output-diagram-templates-with-examples-and-samples]
- 100. Design Verification & Validation for Medical Devices [Guide] [https://www.greenlight.guru/blog/design-verification-and-design-validation]
- 101. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 102. Contrast requirements for WCAG 2.2 Level AA [https://www.makethingsaccessible.com/guides/contrast-requirements-for-wcag-2-2-level-aa/]
- 103. Verification and validation of computer simulation models [https://en.wikipedia.org/wiki/Verification_and_validation_of_computer_simulation_models]
- 104. AI Drug Development: FDA Releases Draft Guidance [https://www.foley.com/insights/publications/2025/01/ai-drug-development-fda-releases-draft-guidance/]
- 105. What's new in the FDA's 2025 AI/ML draft guidance? [https://blogs.atlas-compliance.ai/whats-new-in-the-fdas-2025-ai-ml-draft-guidance/]
- 106. Statistical hypothesis test [https://en.wikipedia.org/wiki/Statistical_hypothesis_test]
- 107. The three most common statistical tests you should deeply ... [https://www.apadivisions.org/division-5/publications/score/2024/10/common-statistical-tests]
- 108. The nuts and bolts of hypothesis testing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6668281/]
- 109. Extensive benchmarking of a method that estimates ... [https://www.nature.com/articles/s41746-024-01414-z]