Beyond Accuracy: A Comprehensive Guide to Predictive Model Performance Metrics for Drug Development
This guide provides researchers, scientists, and drug development professionals with a comprehensive framework for evaluating predictive model performance.
Beyond Accuracy: A Comprehensive Guide to Predictive Model Performance Metrics for Drug Development
Abstract
This guide provides researchers, scientists, and drug development professionals with a comprehensive framework for evaluating predictive model performance. It covers foundational metrics, methodological application for clinical data, advanced troubleshooting and optimization techniques, and robust validation and comparative analysis strategies. The content is tailored to address the unique challenges in biomedical research, such as handling imbalanced data for rare diseases and meeting regulatory requirements for transparent and reliable model reporting.
Core Principles: Understanding the Essential Metrics for Model Evaluation
The Critical Role of Evaluation Metrics in Robust Model Development
The development of predictive models in machine learning operates on a constructive feedback principle where models are built, evaluated using metrics, and improved iteratively until desired performance is achieved [1]. Evaluation metrics are not merely performance indicators but form the fundamental basis for discriminating between model results and making critical decisions about model deployment [1]. Within the context of predictive model performance metrics research, this whitepaper establishes that proper metric selection and interpretation constitute a scientific discipline in itself, particularly for high-stakes fields like pharmaceutical development and drug discovery.
The performance of machine learning models is fundamentally governed by their ability to generalize to unseen data [1] [2]. As noted in analytical literature, "The ground truth is building a predictive model is not your motive. It's about creating and selecting a model which gives a high accuracy score on out-of-sample data" [1]. This principle underscores why a systematic approach to model evaluation—rather than ad-hoc metric selection—proves essential for research integrity and practical application in scientific domains.
Classification of Evaluation Metrics
Evaluation metrics are broadly categorized based on model output type (classification vs. regression) and the specific aspect of performance being measured [1] [3]. Understanding these categories enables researchers to select metrics aligned with their model's operational context and the cost of potential errors.
Core Classification Metrics
Table 1: Fundamental Classification Metrics and Their Applications
| Metric | Formula | Use Case | Advantages | Limitations |
|---|---|---|---|---|
| Accuracy | (TP+TN)/(TP+TN+FP+FN) [3] | Balanced datasets, equal error costs | Simple, intuitive interpretation | Misleading with class imbalance [2] |
| Precision | TP/(TP+FP) [3] | When false positives are costly (e.g., spam filtering) | Measures prediction quality | Does not account for false negatives |
| Recall (Sensitivity) | TP/(TP+FN) [3] | When false negatives are critical (e.g., medical diagnosis) | Identifies true positive coverage | Does not penalize false positives |
| F1-Score | 2×(Precision×Recall)/(Precision+Recall) [1] [3] | Imbalanced datasets, need for balance | Harmonic mean balances both concerns | May oversimplify in complex trade-offs |
| AUC-ROC | Area under ROC curve [2] | Model discrimination ability at various thresholds | Threshold-independent, comprehensive | Can be optimistic with severe imbalance |
Beyond these core metrics, the confusion matrix serves as the foundational table that visualizes all four possible prediction outcomes (True Positives, True Negatives, False Positives, False Negatives), enabling calculation of numerous derived metrics [1] [3]. For pharmaceutical applications, understanding the confusion matrix proves particularly valuable when different types of classification errors carry significantly different consequences.
Advanced Classification Assessment
The Kolmogorov-Smirnov (K-S) chart measures the degree of separation between positive and negative distributions, with values ranging from 0-100, where higher values indicate better separation [1]. Meanwhile, Gain and Lift charts provide rank-ordering capabilities essential for campaign targeting problems, indicating which population segments to prioritize for intervention [1].
Regression Metrics and Their Applications
Regression models require distinct evaluation metrics focused on the magnitude and distribution of prediction errors. Different regression metrics capture varying aspects of error behavior, with selection depending on the specific application context and error tolerance.
Table 2: Key Regression Metrics and Characteristics
| Metric | Formula | Sensitivity to Outliers | Interpretation | Best Use Cases |
|---|---|---|---|---|
| Mean Absolute Error (MAE) | (1/n)×∑|yi-ŷi| [3] | Robust | Average error magnitude | When all errors are equally important |
| Mean Squared Error (MSE) | (1/n)×∑(yi-ŷi)² [3] | High | Average squared error | When large errors are particularly undesirable |
| Root Mean Squared Error (RMSE) | √MSE [3] | High | Error in original units | When units matter and large errors are critical |
| R-squared (R²) | 1 - (SSE/SST) [3] | Moderate | Proportion of variance explained | Model explanatory power |
| Adjusted R-squared | 1 - [(1-R²)(n-1)/(n-k-1)] | Moderate | Variance explained adjusted for predictors | Comparing models with different predictors |
Recent research in wastewater quality prediction—a domain with parallels to pharmaceutical process optimization—suggests that "error metrics based on absolute differences are more favorable than squared ones" in noisy environments [4]. This finding has significant implications for drug development applications where sensor data and experimental measurements often contain substantial inherent variability.
Experimental Design and Validation Protocols
Robust model evaluation requires methodological rigor in experimental design beyond mere metric calculation. Proper validation techniques ensure that reported performance metrics reflect true generalization capability rather than idiosyncrasies of the data partitioning.
Holdout Validation
The dataset is split into two parts: a training set for model development and a test set for final evaluation [3]. This approach provides an unbiased assessment of model performance on unseen data. For example, in predicting customer subscription cancellations, a streaming company might use data from 800 customers for training and reserve 200 completely separate customers for testing [3].
Cross-Validation Techniques
k-Fold Cross-Validation divides the dataset into k equal parts (folds), using k-1 folds for training and the remaining fold for testing, repeating this process k times [3]. A financial institution predicting loan defaults might implement 5-fold cross-validation, ensuring the model's performance consistency across different data subsets [3]. The final performance is averaged across all folds:
Average Performance = (1/K) × ∑(Performance on Fold_i) [2]
For imbalanced datasets common in pharmaceutical applications (such as rare adverse event prediction), stratified cross-validation maintains the class distribution比例 in each fold, preventing biased evaluation [2].
The Bias-Variance Tradeoff
The bias-variance tradeoff represents a fundamental concept in model evaluation, balancing underfitting (high bias) against overfitting (high variance) [3]. Simple models with high bias fail to capture data patterns, while overly complex models with high variance fit training noise rather than underlying relationships [3]. Optimal model selection explicitly acknowledges and manages this tradeoff.
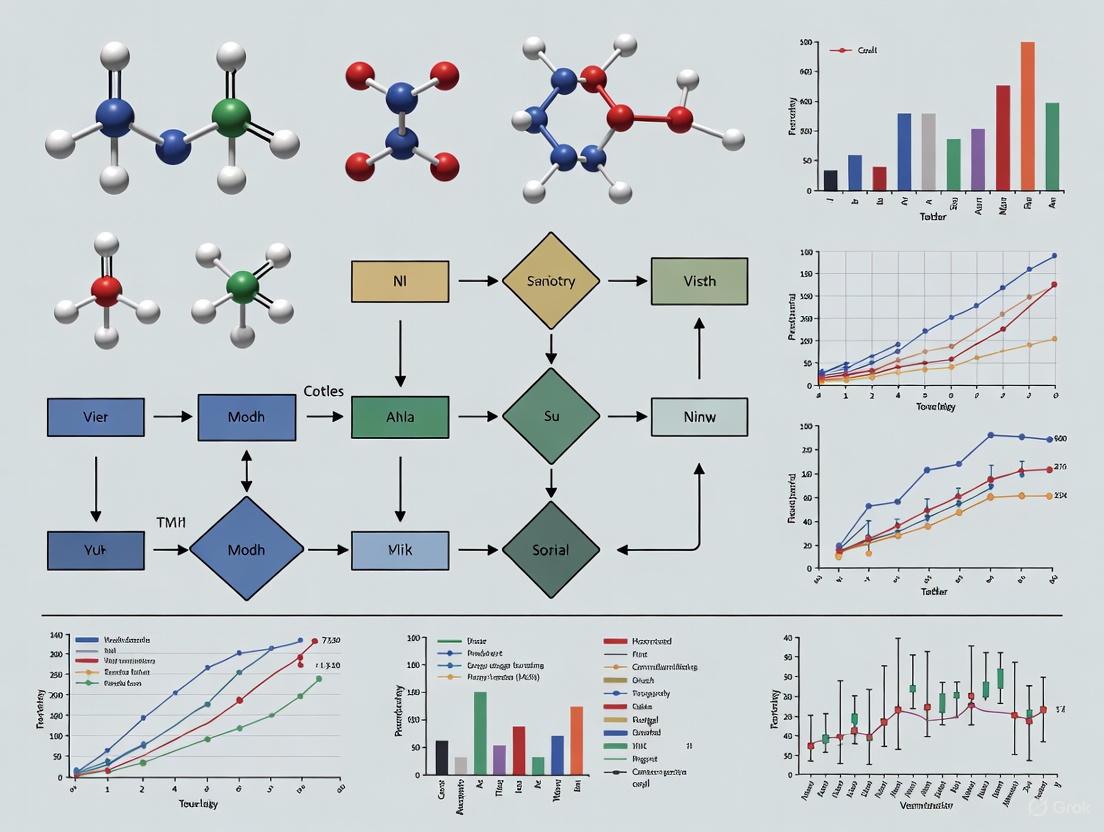
Methodological Workflows and Visualization
The process of model evaluation follows systematic workflows that ensure comprehensive assessment. The diagram below illustrates the integrated model validation workflow:
Integrated Model Validation Workflow
Selecting appropriate evaluation metrics requires understanding the research question and model objectives. The following diagram outlines the decision process for metric selection:
Metric Selection Decision Framework
Table 3: Essential Research Reagent Solutions for Model Evaluation
| Tool/Resource | Function | Application Context |
|---|---|---|
| Scikit-learn Metrics Module | Provides implementation of key metrics [5] | General-purpose model evaluation |
| Strictly Consistent Scoring Functions | Aligns metric with target functional (e.g., mean, quantile) [5] | Probabilistic forecasting and decision making |
| Cross-Validation Implementations | k-Fold, Leave-One-Out, Stratified variants [3] | Robust performance estimation |
| Confusion Matrix Analysis | Detailed breakdown of classification results [1] [3] | Binary and multi-class classification |
| AUC-ROC Calculation | Threshold-agnostic model discrimination assessment [1] [2] | Classification model selection |
| Multiple Metric Evaluation | Simultaneous assessment of different performance aspects [2] | Comprehensive model validation |
Emerging Trends and Future Directions
The landscape of model evaluation continues to evolve with increasing sophistication in metric development and application. Current research indicates several emerging trends that will influence future predictive model assessment in scientific domains.
Metric Selection Frameworks
Research in specialized domains like wastewater treatment has led to the development of "practical, decision-guiding flowchart[s] to assist researchers in selecting appropriate evaluation metrics based on dataset characteristics, modeling objectives, and project constraints" [4]. Similar frameworks are increasingly necessary for pharmaceutical applications where regulatory compliance and model interpretability requirements impose additional constraints on metric selection.
Evaluation of Generative AI Models
As generative AI models become more prevalent in scientific discovery, including drug candidate generation and molecular design, traditional evaluation metrics prove insufficient [2]. These models require "a more nuanced approach" beyond conventional metrics, incorporating human evaluation, domain-specific benchmarks, and specialized quality assessments [2].
Continuous Performance Monitoring
The concept of model evaluation is expanding beyond pre-deployment assessment to include continuous monitoring in production environments [2]. This recognizes that "model performance can degrade over time as the underlying data distribution changes, a phenomenon known as data drift" [2]. For pharmaceutical applications with longitudinal data, establishing continuous evaluation protocols becomes essential for maintaining model validity throughout its lifecycle.
Evaluation metrics form the scientific foundation for robust model development in predictive analytics, particularly in high-stakes fields like pharmaceutical research and drug development. The selection of appropriate metrics must be guided by domain knowledge, error cost analysis, and operational requirements rather than convention or convenience. As the field advances, researchers must remain abreast of both theoretical developments in metric design and practical frameworks for comprehensive model assessment. The integration of rigorous evaluation protocols throughout the model lifecycle ensures that predictive models deliver reliable, actionable insights for scientific advancement and public health improvement.
Within the rigorous field of predictive modeling, the performance of a classification algorithm is paramount. For researchers and scientists, particularly in high-stakes domains like drug development, a model's output must be quantifiable, interpretable, and trustworthy. The confusion matrix serves as this fundamental diagnostic tool, providing a granular breakdown of a model's predictions versus actual outcomes and forming the basis for a suite of critical performance metrics [6] [7]. This technical guide deconstructs the confusion matrix into its core components—True Positives (TP), True Negatives (TN), False Positives (FP), and False Negatives (FN)—and details the methodologies for deriving and interpreting key metrics essential for validating predictive models in scientific research.
Core Components of the Confusion Matrix
A confusion matrix is a specific table layout that allows for the visualization of a classification model's performance [7]. It compares the actual target values with those predicted by the machine learning model, creating a structured overview of its successes and failures.
The foundational structure for a binary classification problem is a 2x2 matrix, with rows representing the actual class and columns representing the predicted class [6] [8]. The four resulting quadrants are defined as follows:
- True Positive (TP): The model correctly predicts the positive class. In a medical context, this represents a patient with a disease who is correctly identified as having it [6] [9].
- True Negative (TN): The model correctly predicts the negative class. This represents a healthy patient correctly identified as not having the disease [6] [9].
- False Positive (FP): The model incorrectly predicts the positive class when the actual value is negative. Also known as a Type I error, this is a false alarm [6] [7]. For example, a diagnostic test incorrectly indicating that a healthy person has a disease [6].
- False Negative (FN): The model incorrectly predicts the negative class when the actual value is positive. Also known as a Type II error, this represents a missed detection [6] [7]. For example, a test failing to identify a sick person as having the disease [6].
The following diagram illustrates the logical relationship between these components and the process of creating a confusion matrix.
Metrics Derived from the Confusion Matrix
The raw counts of TP, TN, FP, and FN are used to calculate a suite of performance metrics, each offering a different perspective on model behavior [6] [7]. The choice of metric is critical and depends on the specific research objective and the cost associated with different types of errors.
Comprehensive Metric Formulae
The table below summarizes the key metrics derived from the confusion matrix, their formulas, and their core interpretation.
Table 1: Key Performance Metrics Derived from the Confusion Matrix
| Metric | Formula | Interpretation |
|---|---|---|
| Accuracy | (TP + TN) / (TP + TN + FP + FN) [6] [10] | The overall proportion of correct predictions among the total predictions. |
| Precision | TP / (TP + FP) [6] [10] | The proportion of correctly identified positives among all instances predicted as positive. Measures the model's reliability when it predicts the positive class. |
| Recall (Sensitivity) | TP / (TP + FN) [6] [10] | The proportion of actual positive cases that were correctly identified. Measures the model's ability to find all relevant positive cases. |
| Specificity | TN / (TN + FP) [6] | The proportion of actual negative cases that were correctly identified. |
| F1-Score | 2 * (Precision * Recall) / (Precision + Recall) [6] [10] | The harmonic mean of precision and recall, providing a single metric that balances both concerns. |
| False Positive Rate (FPR) | FP / (FP + TN) [10] | The proportion of actual negatives that were incorrectly classified as positive. Equal to 1 - Specificity. |
The Precision-Recall Trade-Off and Metric Selection
Precision and recall often have an inverse relationship; increasing one may decrease the other [10]. The F1-score is a single metric that balances this trade-off, but the choice to prioritize precision or recall is domain-specific.
- High-Recall Scenarios: Essential in contexts where the cost of missing a positive case is high. In medical diagnostics (e.g., cancer screening or identifying patients for drug trials), a false negative (missing a disease) is far more dangerous than a false positive (which can be ruled out by further tests) [10] [11]. Therefore, maximizing recall is the priority.
- High-Precision Scenarios: Critical when the cost of a false positive is high. For example, in spam email detection, incorrectly labeling a legitimate email as spam (false positive) is more problematic than letting a single spam email through (false negative) [6] [10].
- The Pitfall of Accuracy: For imbalanced datasets, where one class significantly outnumbers the other, accuracy can be a misleading metric [9] [10]. A model that simply predicts the majority class for all instances can achieve high accuracy while being useless for identifying the critical minority class (e.g., a rare disease).
Experimental Protocol for Model Evaluation
This section provides a detailed, step-by-step methodology for evaluating a classification model and constructing its confusion matrix, using a publicly available clinical dataset as an example.
Research Reagent Solutions and Essential Materials
Table 2: Essential Tools and Software for Model Evaluation
| Item | Function | Example / Justification |
|---|---|---|
| Labeled Dataset | Serves as the ground truth for training and evaluating the model. Requires expert annotation. | The Breast Cancer Wisconsin (Diagnostic) Dataset [11] [8]. |
| Programming Language | Provides the environment for data manipulation, model training, and evaluation. | Python, with its extensive data science ecosystem (e.g., scikit-learn, pandas, NumPy) [6] [11]. |
| Computational Library | Offers pre-implemented functions for metrics calculation and matrix visualization. | Scikit-learn's metrics module (confusion_matrix, classification_report) [6] [11]. |
| Visualization Library | Enables the creation of clear, interpretable plots of the confusion matrix. | Seaborn and Matplotlib for generating heatmaps [6] [11]. |
Step-by-Step Workflow
The following diagram outlines the end-to-end experimental workflow for training a model and evaluating its performance using a confusion matrix.
1. Data Preparation and Model Training: A common dataset used in medical ML research is the Breast Cancer Wisconsin dataset, which contains features computed from digitized images of fine-needle aspirates of breast masses, with the target variable being diagnosis (malignant or benign) [11] [8]. The dataset is first split into a training set (e.g., 70-80%) and a held-out test set (e.g., 20-30%) to ensure an unbiased evaluation [8]. A classification model, such as Logistic Regression or Support Vector Machine (SVM), is then trained on the training set [11] [8].
2. Prediction and Matrix Construction:
The trained model is used to predict labels for the test set. These predictions are compared against the ground truth labels. Using a function like confusion_matrix from scikit-learn, the counts for TP, TN, FP, and FN are computed [6].
Example Python Snippet:
3. Metric Derivation and Visualization: The counts from the confusion matrix are used to calculate the metrics outlined in Table 1. The matrix is best visualized as a heatmap to facilitate immediate interpretation.
Example Python Snippet for Visualization:
4. Threshold Tuning: The default threshold for classification is often 0.5. However, this threshold can be adjusted to better align with research goals [12] [11]. Lowering the classification threshold makes it easier to predict the positive class, which typically increases Recall (fewer false negatives) but decreases Precision (more false positives). Conversely, raising the threshold increases Precision but decreases Recall [11]. The optimal threshold is determined by analyzing metrics across a range of values, for instance, using ROC or Precision-Recall curves [12].
The confusion matrix is an indispensable, foundational tool in the evaluation of predictive models. Its components—TP, TN, FP, and FN—provide the raw data from which critical metrics like accuracy, precision, recall, and the F1-score are derived. For researchers in drug development and other scientific fields, a nuanced understanding of these metrics and the trade-offs between them is non-negotiable. It allows for the rigorous selection and deployment of models whose performance characteristics are aligned with the high-stakes costs of real-world decision-making, where a false negative or false positive can have significant consequences. Proper evaluation, as outlined in this guide, ensures that predictive models are not just mathematically sound but are also fit for their intended purpose.
In the rigorous field of predictive model performance metrics research, selecting appropriate evaluation criteria is paramount to validating a model's real-world utility. This is especially critical in high-stakes domains like drug development, where model performance directly impacts patient safety and therapeutic efficacy [13]. Metrics such as accuracy, precision, recall, and the F1-score provide a multifaceted view of model behavior, each illuminating a different aspect of performance. Their definitions, interrelationships, and the trade-offs they represent form the foundation of robust model evaluation [10] [14]. This guide provides an in-depth technical exploration of these core metrics, framing them within the specific context of pharmaceutical research and development to aid scientists and professionals in making informed, evidence-based decisions about their predictive models.
Core Metric Definitions and Mathematical Formulations
The evaluation of binary classification models is fundamentally based on four outcomes derived from the confusion matrix: True Positives (TP), True Negatives (TN), False Positives (FP), and False Negatives (FN) [1] [15]. These outcomes represent the simplest agreement or disagreement between model predictions and actual values.
The Confusion Matrix: A Foundational Tool
The confusion matrix is a 2x2 table that provides a detailed breakdown of a model's predictions against actual outcomes [14]. It is the cornerstone for calculating all subsequent metrics and is indispensable for diagnosing specific error patterns.
- True Positive (TP): The model correctly predicts the positive class. In drug discovery, this represents correctly identifying a compound that truly has a therapeutic effect [14].
- True Negative (TN): The model correctly predicts the negative class. For example, correctly identifying a drug candidate that does not cause a specific adverse reaction [15].
- False Positive (FP) (Type I Error): The model incorrectly predicts the positive class. This is a "false alarm," such as wrongly flagging a safe drug as potentially causing a severe side effect [10] [14].
- False Negative (FN) (Type II Error): The model incorrectly predicts the negative class. This is a "miss," such as failing to identify a drug that actually causes an adverse reaction, a critical error in pharmacovigilance [10] [14].
Derivation of Primary Metrics
From these four building blocks, the primary evaluation metrics are derived. The formulas below provide a quantitative framework for assessment.
Accuracy
Accuracy measures the overall correctness of the model across both positive and negative classes [10] [15].
Formula:
Accuracy = (TP + TN) / (TP + TN + FP + FN) [10]
Precision
Precision, also known as Positive Predictive Value (PPV), measures the reliability of a model's positive predictions [10] [14]. It answers the question: "When the model predicts positive, how often is it correct?"
Formula:
Precision = TP / (TP + FP) [10]
Recall
Recall, also known as Sensitivity or True Positive Rate (TPR), measures a model's ability to identify all relevant positive instances [10] [14]. It answers the question: "Of all the actual positives, how many did the model successfully find?"
Formula:
Recall = TP / (TP + FN) [10]
F1-Score
The F1-score is the harmonic mean of precision and recall, providing a single metric that balances both concerns [10] [16]. It is particularly useful when a balanced view of both false positives and false negatives is needed.
Formula:
F1 = 2 * (Precision * Recall) / (Precision + Recall) = 2TP / (2TP + FP + FN) [10] [16]
Table 1: Summary of Core Evaluation Metrics
| Metric | Formula | Interpretation | Focus |
|---|---|---|---|
| Accuracy | (TP + TN) / (TP + TN + FP + FN) | Overall correctness of the model | All predictions |
| Precision | TP / (TP + FP) | Correctness when it predicts positive | False Positives (Type I Error) |
| Recall | TP / (TP + FN) | Ability to find all positive instances | False Negatives (Type II Error) |
| F1-Score | 2TP / (2TP + FP + FN) | Balanced mean of precision and recall | Both FP and FN |
The Critical Role of Class Balance and Metric Selection
The distribution of classes in a dataset—whether it is balanced or imbalanced—profoundly influences the interpretation and choice of these metrics [10] [15].
The Accuracy Paradox in Imbalanced Data
Accuracy can be a dangerously misleading metric when dealing with imbalanced datasets, which are common in healthcare and drug safety applications [15]. For instance, if only 1% of patients in a study experience a serious adverse drug reaction (ADR), a model that simply predicts "no ADR" for every patient would achieve 99% accuracy, despite being entirely useless for the task of identifying the critical positive cases [10] [15]. This phenomenon is known as the accuracy paradox [15].
Strategic Metric Selection for Drug Development
The choice of which metric to prioritize is not a purely technical decision; it must be guided by the specific clinical or research context and the cost associated with different types of errors [10] [13].
Table 2: Metric Selection Guide for Pharmaceutical Use Cases
| Use Case Scenario | Primary Metric | Rationale and Cost-Benefit Analysis |
|---|---|---|
| Early-stage drug safety screening [13] | High Recall | Goal: Identify all potential ADRs.Cost of FN: Catastrophic. A missed toxic compound progresses, risking patient harm and costly late-stage trial failures.Cost of FP: Manageable. A safe compound flagged for further review incurs minor additional testing cost. |
| Validating a diagnostic assay | High Precision | Goal: Ensure positive test results are reliable.Cost of FP: High. A false diagnosis leads to patient anxiety, unnecessary confirmatory tests, and potential for incorrect treatment.Cost of FN: Lower but still important. A missed case may be caught through subsequent testing. |
| Post-market pharmacovigilance [17] | F1-Score | Goal: Balance the detection of true ADR signals with the operational cost of investigating false alerts.Context: Requires a balance; too many FPs overwhelm resources, while too many FNs mean missing safety signals. |
| Balanced dataset (e.g., drug-target interaction) [18] | Accuracy (with other metrics) | Goal: General model correctness.Context: When both classes are equally represented and important, accuracy provides a valid coarse-grained performance indicator. |
Experimental Protocols and Performance Benchmarking
To illustrate the practical application of these metrics, consider a typical experimental protocol for evaluating a model designed to predict adverse drug reactions (ADRs) from clinical trial data [17].
Experimental Workflow for ADR Prediction
The following diagram outlines a standardized methodology for building and evaluating a predictive model in this context.
Benchmarking Model Performance
A study on AI-driven pharmacovigilance provides concrete results from such an evaluation, comparing multiple machine learning models [17]. The performance metrics offer a clear, quantitative basis for model selection.
Table 3: Model Performance Comparison for ADR Detection [17]
| Model | Reported Accuracy | Precision | Recall | F1-Score |
|---|---|---|---|---|
| Logistic Regression (Benchmark) | 78% | Data not specified | Data not specified | Data not specified |
| Support Vector Machine (Benchmark) | 80% | Data not specified | Data not specified | Data not specified |
| Convolutional Neural Network (CNN) | 85% | Data not specified | Data not specified | Data not specified |
Experimental Insight: The CNN model's superior accuracy suggests it is better at overall correct classification of ADRs versus non-ADRs [17]. However, for a full assessment, the precision and recall values are critical. A model with high accuracy but low recall would be unsuitable, as it would miss too many actual ADRs.
Another study on drug-target interactions reported an accuracy of 98.6% for their proposed CA-HACO-LF model, highlighting the high performance achievable on specific prediction tasks within drug discovery [18].
Advanced Considerations: The Precision-Recall Trade-Off and Fβ-Score
In practice, it is often impossible to simultaneously improve both precision and recall. This inherent tension is known as the precision-recall trade-off [10] [14].
Visualizing the Trade-Off
Adjusting the classification threshold of a model directly impacts this trade-off. A higher threshold makes the model more conservative, increasing precision but decreasing recall. A lower threshold makes the model more aggressive, increasing recall but decreasing precision [14]. This relationship is best visualized with a Precision-Recall (PR) curve.
The Fβ-Score: A Flexible Combined Metric
While the F1-score assigns equal weight to precision and recall, there are scenarios where one is more important than the other. The generalized Fβ-score allows for this flexibility [1] [16].
Formula:
Fβ = (1 + β²) * (Precision * Recall) / (β² * Precision + Recall) [16]
The β parameter controls the weighting:
β = 1: Equally weights precision and recall (standard F1-score).β > 1: Favors recall (e.g.,β=2for F2-score, recall is twice as important as precision).β < 1: Favors precision (e.g.,β=0.5, precision is twice as important as recall).
This is crucial in drug development. For a screening model to identify potentially toxic compounds, a high β value (e.g., 2) would be appropriate to heavily penalize false negatives. Conversely, for a final confirmatory test, a low β value might be chosen to ensure positive results are highly reliable and minimize false alarms [16].
Implementing and evaluating these metrics requires a suite of methodological and computational tools. The following table details key components of the research toolkit for scientists working in predictive model evaluation for drug development.
Table 4: Essential Research Reagents and Computational Tools
| Tool / Technique | Function in Evaluation | Example Application in Drug Discovery |
|---|---|---|
| Confusion Matrix [1] [14] | Foundational diagnostic tool visualizing TP, TN, FP, FN. | First-step analysis to understand the specific error profile of a model predicting drug-target interactions [18]. |
| Precision-Recall (PR) Curve [14] | Illustrates the trade-off between precision and recall across different classification thresholds. | Essential for evaluating models on imbalanced datasets, such as predicting rare but serious adverse drug reactions [17]. |
| Fβ-Score [16] | A single metric that allows for weighting precision vs. recall based on a specific β parameter. | Formally incorporates the relative cost of false positives vs. false negatives into model selection for a given clinical task. |
| Cosine Similarity & N-Grams [18] | Feature extraction techniques for textual or structural data to assess semantic and syntactic proximity. | Used to process and extract meaningful features from scientific literature or drug description datasets to improve context-aware models [18]. |
| Cross-Validation [1] | A resampling technique used to assess model generalizability and reduce overfitting. | Critical for providing a robust estimate of model performance (e.g., accuracy, F1) before deployment in clinical trial data analysis [1]. |
| Context-Aware Hybrid Models (e.g., CA-HACO-LF) [18] | Advanced models combining optimization algorithms with classifiers for improved prediction. | Used in state-of-the-art research to enhance the accuracy of predicting complex endpoints like drug-target interactions [18]. |
Within the broader context of predictive model performance metrics research, the Receiver Operating Characteristic (ROC) curve and the Area Under this Curve (AUC) stand as critical tools for evaluating binary classification models. These metrics are indispensable for assessing a model's discriminative power—its ability to separate positive and negative classes—across all possible classification thresholds. Unlike metrics such as accuracy, which provide a single-threshold snapshot, the AUC-ROC offers a comprehensive, threshold-independent evaluation, making it particularly valuable for imbalanced datasets common in medical research and drug development [19] [20]. This technical guide details the principles, interpretation, and methodological application of AUC-ROC, providing researchers with the framework necessary for robust model evaluation.
Core Concepts and Definitions
The ROC Curve
The ROC curve is a graphical plot that illustrates the diagnostic ability of a binary classifier system. It is created by plotting the True Positive Rate (TPR) against the False Positive Rate (FPR) at various threshold settings [19] [21]. The curve visualizes the trade-off between sensitivity and specificity, enabling researchers to select an optimal threshold based on the relative costs of false positives and false negatives in their specific application.
Underlying Metrics
The construction and interpretation of the ROC curve rely on fundamental classification metrics derived from the confusion matrix:
- True Positive Rate (TPR/Sensitivity/Recall): Proportion of actual positives correctly identified: ( TPR = \frac{TP}{TP + FN} ) [22] [23]
- False Positive Rate (FPR): Proportion of actual negatives incorrectly classified as positive: ( FPR = \frac{FP}{FP + TN} = 1 - Specificity ) [22] [23]
- Specificity (True Negative Rate): Proportion of actual negatives correctly identified: ( Specificity = \frac{TN}{TN + FP} ) [21] [24]
Table 1: Classification Metrics from Confusion Matrix
| Metric | Formula | Interpretation |
|---|---|---|
| Sensitivity/Recall/TPR | ( \frac{TP}{TP + FN} ) | Ability to identify true positives |
| Specificity/TNR | ( \frac{TN}{TN + FP} ) | Ability to identify true negatives |
| False Positive Rate | ( \frac{FP}{FP + TN} ) | Proportion of false alarms |
| False Negative Rate | ( \frac{FN}{TP + FN} ) | Proportion of missed positives |
Area Under the Curve (AUC)
The AUC represents the probability that a randomly chosen positive example ranks higher than a randomly chosen negative example, based on the classifier's scoring function [19] [20]. This interpretation as a ranking metric is fundamental to understanding its value in model assessment. AUC values range from 0 to 1, where:
- AUC = 1.0: Perfect classifier that completely separates the classes
- AUC = 0.5: Classifier with no discriminative power (equivalent to random guessing)
- AUC < 0.5: Classifier performs worse than random guessing [19] [24]
Clinical and Diagnostic Applications
In medical research and drug development, ROC analysis is extensively used to evaluate diagnostic tests, biomarkers, and predictive models. The curve helps determine the clinical utility of index tests—including serum markers, radiological imaging, or clinical decision rules—by quantifying their ability to distinguish between diseased and non-diseased individuals [21] [25].
Table 2: Clinical Interpretation Guidelines for AUC Values
| AUC Value | Diagnostic Performance | Clinical Utility |
|---|---|---|
| 0.9 - 1.0 | Excellent | High clinical utility |
| 0.8 - 0.9 | Considerable | Good clinical utility |
| 0.7 - 0.8 | Fair | Moderate clinical utility |
| 0.6 - 0.7 | Poor | Limited clinical utility |
| 0.5 - 0.6 | Fail | No clinical utility [25] |
When interpreting AUC values, researchers should always consider the 95% confidence interval. A narrow confidence interval indicates greater reliability of the AUC estimate, while a wide interval suggests uncertainty, potentially due to insufficient sample size [25].
Methodological Considerations
ROC Curve Types
ROC curves can be generated using different statistical approaches, each with distinct advantages:
- Nonparametric (Empirical) ROC Curves: Constructed directly from observed data without distributional assumptions. These curves typically have a jagged, staircase appearance but provide unbiased estimates of sensitivity and specificity [21].
- Parametric ROC Curves: Assume data follows a specific distribution (often normal). These produce smooth curves but may yield improper ROC curves if distributional assumptions are violated [21].
- Semiparametric ROC Curves: Combine elements of both approaches to overcome limitations of each method [21].
Table 3: Comparison of ROC Curve Methodologies
| Characteristic | Nonparametric | Parametric |
|---|---|---|
| Assumptions | No distributional assumptions | Assumes normal distribution |
| Curve Appearance | Jagged, staircase | Smooth |
| Data Usage | Uses all observed data | May discard actual data points |
| Computation | Simple | Complex |
| Bias Potential | Unbiased estimates | Possibly biased |
Optimal Cutoff Selection
While ROC analysis evaluates performance across all thresholds, practical application often requires selecting a single operating point. The Youden Index (( J = Sensitivity + Specificity - 1 )) identifies the threshold that maximizes both sensitivity and specificity [25]. However, the optimal threshold ultimately depends on the clinical context and relative consequences of false positives versus false negatives [19] [21].
Performance Evaluation and Comparison with Other Metrics
Advantages of AUC-ROC
Research demonstrates that AUC provides the most consistent model evaluation across datasets with varying prevalence levels, maintaining stable performance when other metrics fluctuate significantly [20]. This stability arises because AUC evaluates the ranking capability of a model rather than its performance at a single threshold, making it particularly valuable for:
- Imbalanced datasets where positive and negative classes are unevenly distributed [20] [26]
- Threshold-independent evaluation of intrinsic model performance [20]
- Model comparison without presupposing a specific operating threshold [19] [20]
Limitations and Complementary Metrics
While powerful, AUC-ROC has limitations. In cases of extreme class imbalance, precision-recall curves may provide more meaningful evaluation [19] [22]. Additionally, AUC summarizes performance across all thresholds, which may include regions of little practical interest [20]. For comprehensive model assessment, researchers should consider AUC alongside metrics like precision, recall, and F1-score, particularly when the operational threshold is known.
Experimental Protocols and Implementation
ROC Curve Generation Protocol
The following methodology details the process for generating and evaluating ROC curves:
- Model Training: Train binary classification model using standardized procedures
- Probability Prediction: Generate predicted probabilities for the positive class on validation data
- Threshold Selection: Define a series of classification thresholds (typically 0-1 in increments of 0.01)
- Performance Calculation: At each threshold, calculate TPR and FPR using the confusion matrix
- Curve Plotting: Graph TPR (y-axis) against FPR (x-axis) for all thresholds
- AUC Calculation: Compute the area under the plotted curve using numerical integration methods (e.g., trapezoidal rule) [22] [23]
Statistical Comparison of ROC Curves
When comparing two independent ROC curves, researchers can test for statistically significant differences in AUC using methods such as the DeLong test [25] [27]. This evaluation should consider both the magnitude of difference between AUC values and their associated confidence intervals to draw meaningful conclusions about comparative model performance.
Multiclass Classification Extension
For problems with more than two classes, the One-vs-Rest (OvR) approach extends ROC analysis by treating each class as the positive class once while grouping all others as negative [24]. This generates multiple ROC curves (one per class), with the macro-average AUC providing an overall performance measure.
Research Reagent Solutions
Table 4: Essential Tools for ROC Analysis in Research
| Tool/Category | Examples | Function |
|---|---|---|
| Statistical Software | R, Python (scikit-learn), MedCalc, SPSS | Compute ROC curves, AUC, and confidence intervals |
| Programming Libraries | scikit-learn, pROC (R), statsmodels | Implement ROC analysis algorithms |
| Visualization Tools | matplotlib, ggplot2, seaborn | Generate publication-quality ROC curves |
| Statistical Tests | DeLong test, Hanley & McNeil method | Compare AUC values statistically |
Visualizations
ROC Curve Construction Logic
AUC Interpretation and Calculation
The AUC-ROC curve remains a fundamental tool for evaluating predictive model performance in research settings, particularly in medical science and drug development. Its capacity to measure discriminative power across all classification thresholds provides a comprehensive assessment of model quality that single-threshold metrics cannot match. While researchers should remain aware of its limitations—particularly in cases of extreme class imbalance—the AUC-ROC's consistency across varying prevalence levels and its intuitive interpretation as a ranking metric secure its position as an essential component of the model evaluation toolkit. Future work in predictive model performance metrics research should continue to refine ROC methodology while developing complementary approaches that address its limitations in specialized applications.
Gain, Lift, and Kolmogorov-Smirnov (K-S) Charts for Model Selection
Within the rigorous framework of predictive model performance metrics research, selecting an optimal classification model extends beyond mere accuracy. This technical guide provides an in-depth examination of three pivotal diagnostic tools—Gain, Lift, and Kolmogorov-Smirnov (K-S) charts—that empower researchers and drug development professionals to evaluate model efficacy based on probabilistic ranking and distributional separation. These metrics are particularly crucial in domains like pharmacovigilance and targeted therapy, where imbalanced data is prevalent and the cost of misclassification is high. By detailing their theoretical foundations, calculation methodologies, and interpretive protocols, this whitepaper establishes a standardized paradigm for model selection that prioritizes operational efficiency and robust discriminatory power.
The evaluation of predictive models in scientific research, particularly in drug development, necessitates metrics that align with strategic operational goals. While traditional metrics like accuracy and F1-score provide a snapshot of overall performance, they often fail to guide resource allocation efficiently [1] [2]. Gain, Lift, and K-S charts address this gap by focusing on the model's ability to rank-order instances by their probability of belonging to a target class, such as patients experiencing an adverse drug reaction or respondents to a specific treatment.
This approach is indispensable when dealing with imbalanced datasets, a common scenario in clinical trials and healthcare analytics, where the event of interest may be rare [28]. By quantifying the concentration of target events within top-ranked segments, these charts enable researchers to make data-driven decisions about where to apply a model's predictions for maximum impact, thereby optimizing experimental budgets and accelerating discovery cycles. This paper frames these tools within a broader thesis that advocates for context-sensitive, efficiency-oriented model evaluation.
Gain Chart: Quantifying Cumulative Model Effectiveness
Theoretical Foundation
A Gain Chart visualizes the effectiveness of a classification model by plotting the cumulative percentage of the target class captured against the cumulative percentage of the population sampled when sorted in descending order of predicted probability [28] [29]. Its core function is to answer the question: "If we target the top X% of a population based on the model's predictions, what percentage of all positive cases will we capture?" [30]. This makes it an invaluable tool for planning targeted interventions, such as identifying a sub-population for a high-cost therapeutic or selecting patients for a focused clinical study.
Construction Methodology
The construction of a Gain Chart follows a systematic protocol [28] [30]:
- Probability Prediction and Ranking: Use the model to assign a probability of being in the target class (e.g., "responder," "disease positive") to every instance in the validation dataset. Rank all instances from highest to lowest probability.
- Decile-Based Segmentation: Divide the ranked list into ten equal segments, or deciles (i.e., top 10%, next 10%, etc.).
- Cumulative Sum Calculation: For each decile, calculate the cumulative number of true positive instances (actual target class members) captured up to that point.
- Gain Calculation: The gain value for each decile is calculated as the ratio of the cumulative number of true positives up to that decile to the total number of true positives in the entire dataset [28].
- Plotting: The Gain Chart is plotted with the cumulative percentage of the population (deciles) on the X-axis and the cumulative percentage of true positives (Gain) on the Y-axis.
Table 1: Example Gain Chart Calculation for a Marketing Response Model (Total Positives = 3850)
| Decile | % Population | Number of Positives in Decile | Cumulative Positives | Gain (%) |
|---|---|---|---|---|
| 1 | 10% | 543 | 543 | 14.1% |
| 2 | 20% | 345 | 888 | 23.1% |
| 3 | 30% | 287 | 1175 | 30.5% |
| 4 | 40% | 222 | 1397 | 36.3% |
| 5 | 50% | 158 | 1555 | 40.4% |
| 6 | 60% | 127 | 1682 | 43.7% |
| 7 | 70% | 98 | 1780 | 46.2% |
| 8 | 80% | 75 | 1855 | 48.2% |
| 9 | 90% | 53 | 1908 | 49.6% |
| 10 | 100% | 42 | 1950 | 50.6% |
Interpretation and Analysis
The resulting chart features two key lines [29]:
- The Model Gain Curve: A curve that arches above the baseline. The steeper the initial ascent of this curve, the better the model is at concentrating positive cases at the top of the ranked list.
- The Baseline (Random Model): A diagonal line from (0,0) to (100,100), representing the expected performance if instances were selected randomly. For example, randomly selecting 20% of the population would be expected to capture 20% of the positive cases.
A superior model will show a gain curve that rises sharply towards the top-left corner. For instance, from Table 1, the model captures 36.3% of all positive cases by targeting only the top 40% of the population, a significant improvement over the 40% expected by random selection [30]. The point where the gain curve begins to flatten indicates the optimal operational cutoff for resource allocation.
Diagram 1: Workflow for constructing a Gain Chart
Lift Chart: Measuring Performance Improvement Over Random
Theoretical Foundation
While the Gain Chart shows cumulative coverage, the Lift Chart expresses the multiplicative improvement in target density achieved by using the model compared to a random selection [31] [29]. Lift answers the question: "How many times more likely are we to find a positive case by using the model compared to not using it?" A lift value of 3 at the top decile means the model is three times more effective than random selection in that segment. This metric is critical for communicating the tangible value and ROI of deploying a predictive model.
Construction Methodology
Lift is derived directly from the Gain Chart data [28] [30]:
- Calculate Cumulative Lift: For each decile, take the Gain value (the cumulative percentage of positives captured) and divide it by the cumulative percentage of the population sampled.
Cumulative Lift = (Cumulative % of Positives at Decile i) / (Cumulative % of Population at Decile i) - Plotting: The Lift Chart is plotted with the cumulative percentage of the population (deciles) on the X-axis and the Lift value on the Y-axis.
Table 2: Corresponding Lift Chart Calculations from Table 1 Data
| Decile | % Population | Gain (%) | Cumulative Lift |
|---|---|---|---|
| 1 | 10% | 14.1% | 1.41 |
| 2 | 20% | 23.1% | 1.16 |
| 3 | 30% | 30.5% | 1.02 |
| 4 | 40% | 36.3% | 0.91 |
| 5 | 50% | 40.4% | 0.81 |
| 6 | 60% | 43.7% | 0.73 |
| 7 | 70% | 46.2% | 0.66 |
| 8 | 80% | 48.2% | 0.60 |
| 9 | 90% | 49.6% | 0.55 |
| 10 | 100% | 50.6% | 0.51 |
Interpretation and Analysis
The Lift Chart also features two primary elements [32]:
- The Model Lift Curve: Typically starts high and decreases, showing that the model's superior performance is concentrated in the top deciles.
- The Baseline: A horizontal line at Lift = 1, which represents random performance.
A strong model will show a high lift (e.g., >3) in the first one or two deciles, indicating powerful discrimination at the top of the list [1]. The point where the lift curve drops to 1 is the point beyond which using the model provides no better than random performance, defining the practical limit of the model's utility. As shown in Table 2, the model's lift is 1.41 in the top decile, meaning it is 1.41 times better than random, but this lift quickly decays, a typical characteristic.
Diagram 2: Logical relationship for calculating Lift from Gain
Kolmogorov-Smirnov (K-S) Chart: Evaluating Distribution Separation
Theoretical Foundation
The Kolmogorov-Smirnov (K-S) chart is a powerful nonparametric tool used to measure the degree of separation between the cumulative distribution functions (CDFs) of two samples—typically the "positive" and "negative" classes as scored by a model [33] [1]. In model evaluation, the K-S statistic quantifies the maximum difference between the cumulative distributions of the two classes, providing a single value that indicates the model's discriminatory power. A higher K-S value (from 0 to 100) signifies a greater ability to distinguish between positive and negative events, which is fundamental for diagnostic and risk stratification models in healthcare.
Construction Methodology
The K-S statistic is calculated from the cumulative distributions of the two classes [33]:
- Score and Separate: Score all instances with the model and separate them into two groups based on their actual class: "Positive" and "Negative."
- Form Cumulative Distributions: For each possible score threshold, calculate the cumulative percentage of "Positive" instances that have a score at or above that threshold (Sensitivity) and the cumulative percentage of "Negative" instances that have a score at or above that threshold (1 - Specificity).
- Calculate K-S Statistic: The K-S statistic is the maximum vertical distance between these two cumulative distribution curves across all possible score thresholds [33] [34].
Table 3: Sample Data for K-S Statistic Calculation (Maximum Difference = 41.7%)
| Score Threshold | Cumulative % Positive | Cumulative % Negative | Difference (K-S) |
|---|---|---|---|
| 0.95 | 10% | 1% | 9% |
| 0.85 | 25% | 5% | 20% |
| 0.75 | 45% | 10% | 35% |
| 0.65 | 65% | 23.3% | 41.7% |
| 0.55 | 80% | 45% | 35% |
| 0.45 | 90% | 70% | 20% |
| 0.00 | 100% | 100% | 0% |
Interpretation and Analysis
The K-S chart plots the cumulative percentage of both positives and negatives against the model's score, visually highlighting the point of maximum separation.
- A high K-S statistic (e.g., >40) indicates that the model can effectively separate the two populations at an optimal cutoff, which is critical for applications like identifying high-risk patients [1].
- A K-S value of 0 suggests the model cannot differentiate between the two classes, while a value of 100 represents perfect separation.
- The optimal score cutoff for operational use is often the point where the K-S maximum occurs, as it balances the trade-off between correctly identifying positives and incorrectly classifying negatives [33].
It is crucial to note that the K-S test is distribution-free and robust to outliers, but it is most appropriate for continuous data and is more sensitive to differences near the center of the distribution than in the tails [33] [34].
Comparative Analysis and Application in Drug Development
Side-by-Side Metric Comparison
Table 4: Comparative Summary of Model Evaluation Charts
| Feature | Gain Chart | Lift Chart | K-S Chart |
|---|---|---|---|
| Primary Purpose | Shows cumulative coverage of targets [28] [30]. | Shows performance improvement over random [31] [29]. | Measures maximum separation between class distributions [33] [1]. |
| Key Question | What % of all positives will I find if I target X% of the population? | How many times better is the model than random at a given point? | How well does the model distinguish between positive and negative classes? |
| Optimal Value | Curve close to top-left corner. | High initial lift (e.g., >3) in top deciles. | High K-S statistic (closer to 100). |
| Interpretation | Guides resource allocation depth (e.g., how many to contact). | Quantifies model value and efficiency. | Identifies model's overall discriminatory power and optimal cutoff. |
| Best Use Case | Planning campaign reach or patient screening depth. | Justifying model deployment and comparing initial performance. | Risk stratification and diagnostic test evaluation. |
Application to Drug Development: A Protocol for Model Selection
In drug development, these charts guide critical decisions. For instance, when building a model to predict patients at high risk of a severe adverse event (AE) from a new therapy, the protocol would be:
- Data Preparation: Use a labeled dataset from Phase II trials, where the target variable is the occurrence of the severe AE. Split data into training (70%), validation (15%), and test (15%) sets, ensuring stratified sampling to preserve the imbalance of the AE rate [2].
- Model Training and Scoring: Train multiple candidate models (e.g., Logistic Regression, Random Forest, Gradient Boosting) on the training set. Use the validation set to generate predicted probabilities for the AE for each model.
- Chart Generation and Evaluation:
- Gain Analysis: For each model, generate a Gain Chart on the validation set. The model that captures the highest percentage of actual AE cases in the top two deciles (i.e., the top 20% of highest-risk patients) would be favored, as it allows for efficient monitoring of the most vulnerable subgroup.
- Lift Analysis: Compare the lift values of the models at the 10% population cutoff. A model with a lift of 4.0 means it is 4 times more effective at identifying AE cases in the top tier than random chart review, directly demonstrating resource efficiency.
- K-S Analysis: Calculate the K-S statistic for each model. A model with a higher K-S statistic (e.g., 60 vs. 45) demonstrates a superior ability to separate patients who will experience an AE from those who will not, which is fundamental for reliable risk stratification.
- Final Selection and Testing: The model that demonstrates a balanced excellence across all three charts—showing strong cumulative gain, high initial lift, and a high K-S statistic—is selected. Its performance is then conclusively validated on the held-out test set to ensure generalizability.
Essential Research Reagent Solutions for Implementation
Table 5: Key Computational Tools for Metric Implementation
| Tool / Reagent | Type | Primary Function in Analysis |
|---|---|---|
| Scikit-learn | Python Library | Core machine learning model training, prediction, and probability calibration [1]. |
| Pandas & NumPy | Python Library | Data manipulation, ranking, and aggregation required for decile analysis and metric calculation [28]. |
| Matplotlib/Seaborn | Python Library | Visualization and plotting of Gain, Lift, and K-S charts for interpretation and reporting. |
| R Language | Statistical Software | Comprehensive statistical environment with native packages for nonparametric tests and advanced plotting [34]. |
| Minitab | Commercial Software | Provides built-in procedures for generating and interpreting Gain and Lift charts [32]. |
| DataRobot | AI Platform | Automated model evaluation with integrated cumulative charts for performance comparison [29]. |
Gain, Lift, and Kolmogorov-Smirnov charts form a critical triad of diagnostics for the sophisticated selection of predictive models in research and drug development. Moving beyond monolithic accuracy metrics, they provide a dynamic view of model performance that is directly tied to strategic operational efficiency and robust statistical separation. By following the detailed methodologies and interpretive frameworks outlined in this guide, researchers can objectively compare models, identify the one that best concentrates the signal of interest, and justify its deployment with clear, quantitative evidence. Integrating these tools into the standard model selection workflow ensures that predictive analytics in high-stakes environments like drug development is not only statistically sound but also pragmatically optimal.
From Theory to Practice: Applying Metrics in Clinical and Biomarker Research
In the domain of supervised machine learning, the selection of an appropriate evaluation metric is a critical decision that extends far beyond technical implementation—it directly aligns model performance with fundamental research objectives and real-world consequences. This selection is primarily governed by the nature of the predictive task: classification for discrete outcomes and regression for continuous values [35] [36]. Within applied research fields such as drug development, this choice forms part of the "fit-for-purpose" modeling strategy, ensuring that quantitative tools are closely matched to the key questions of interest and the specific context of use [37].
The core distinction is intuitive: classification models predict discrete, categorical labels (such as "spam" or "not spam," "malignant" or "benign"), while regression models predict continuous, numerical values (such as house prices, patient survival time, or biochemical concentration levels) [35] [36]. This fundamental difference in output dictates not only the choice of algorithm but also the entire framework for evaluating model success. Despite the emergence of more complex AI methodologies, these foundational paradigms remain central to the practical application of machine learning in domains where interpretability, precision, and structured data are paramount [35].
This guide provides an in-depth examination of performance metrics for classification and regression, offering researchers a structured framework for selection based on problem type, data characteristics, and domain-specific costs of error.
Core Concepts: Classification vs. Regression
Problem Formalization and Objectives
In statistical learning theory, both classification and regression are framed as function approximation problems. The core assumption is that an underlying process maps input data X to outputs Y, expressed as Y = f(X) + ε, where f is the true function and ε represents irreducible error [35]. The machine learning model's goal is to learn a function f̂(X) that best approximates f.
- Classification is the task of learning a function that maps an input to a discrete categorical label [36]. The output is qualitative and can be binary (e.g., spam vs. non-spam), nominal (e.g., dog, cat, fish), or ordinal (e.g., low, medium, high risk) [35]. The model's goal is to find optimal decision boundaries that partition the feature space into distinct classes [36].
- Regression is the task of learning a function that maps an input to a continuous numerical value [36]. The output is quantitative, representing real-valued numbers like revenue, temperature, or drug concentration [35]. The model's objective is to find the best-fit line (or curve) that minimizes the discrepancy between predicted and actual values [36].
Illustrative Examples in Drug Development
The distinction becomes critically important in fields like pharmaceutical research, where the choice of model must align with the scientific question:
- A classification problem might involve diagnosing based on symptoms or predicting whether a compound will be toxic [35].
- A regression problem could involve predicting a continuous outcome like a patient's specific drug concentration level, the number of days a patient stays in hospital, or estimating disease risk [35].
Table 1: Fundamental Differences Between Classification and Regression
| Feature | Classification | Regression |
|---|---|---|
| Output Type | Discrete categories (e.g., "spam", "not spam") [36] | Continuous numerical value (e.g., price, temperature) [36] |
| Core Objective | Predict class membership [36] | Predict a precise numerical quantity [36] |
| Model Output | Decision boundary [36] | Best-fit line or curve [36] |
| Example Algorithms | Logistic Regression, Decision Trees, SVM [36] | Linear Regression, Polynomial Regression, Ridge Regression [35] |
Diagram 1: A decision workflow for selecting model type and evaluation metrics based on problem definition, data characteristics, and business goals.
Evaluation Metrics for Classification
Classification metrics are derived from the confusion matrix, a table that describes the performance of a classifier by comparing actual labels to predicted labels [10] [1]. The core components of a confusion matrix for binary classification are:
- True Positives (TP): Actual positives correctly identified.
- True Negatives (TN): Actual negatives correctly identified.
- False Positives (FP): Actual negatives incorrectly classified as positive (Type I error).
- False Negatives (FN): Actual positives incorrectly classified as negative (Type II error) [10] [15].
Key Metric Definitions and Interpretations
Accuracy: Measures the overall correctness of the model. It is the ratio of all correct predictions (both positive and negative) to the total number of predictions [10] [15]. Accuracy is a good initial metric for balanced datasets but becomes misleading when classes are imbalanced [10].
Accuracy = (TP + TN) / (TP + TN + FP + FN)Precision (Positive Predictive Value): Measures the accuracy of positive predictions. It answers the question: "When the model predicts positive, how often is it correct?" [10] [15]. High precision is critical when the cost of a false positive is high.
Precision = TP / (TP + FP)Recall (Sensitivity or True Positive Rate): Measures the model's ability to identify all actual positive instances. It answers the question: "What fraction of all actual positives did the model find?" [10] [15]. High recall is vital when missing a positive case (false negative) is very costly.
Recall = TP / (TP + FN)F1 Score: The harmonic mean of precision and recall, providing a single metric that balances both concerns [38] [10]. It is especially useful for imbalanced datasets where you need to find a trade-off between false positives and false negatives [10].
F1 Score = 2 * (Precision * Recall) / (Precision + Recall)ROC AUC (Receiver Operating Characteristic - Area Under the Curve): Represents the model's ability to distinguish between classes across all possible classification thresholds. The AUC score is the probability that a randomly chosen positive instance is ranked higher than a randomly chosen negative instance [38]. It is ideal when you care about ranking and when positive and negative classes are equally important.
PR AUC (Precision-Recall AUC): The area under the Precision-Recall curve. This metric is more informative than ROC AUC for highly imbalanced datasets, as it focuses primarily on the model's performance on the positive class [38].
Strategic Metric Selection for Classification
The choice of classification metric should be driven by the research objective and the cost associated with different types of errors [10] [15].
Table 2: A Guide to Selecting Classification Metrics
| Research Context & Goal | Recommended Metric(s) | Rationale |
|---|---|---|
| Balanced Classes, Equal Cost of Errors | Accuracy [10] | Provides a simple, overall measure of correctness. |
| High Cost of False Positives (FP)(e.g., spam classification) | Precision [10] [15] | Ensures that when a positive prediction is made, it is highly reliable. |
| High Cost of False Negatives (FN)(e.g., disease screening, fraud detection) | Recall [10] [15] | Ensures that most actual positive cases are captured, minimizing misses. |
| Imbalanced Data & Need for Balance between FP and FN | F1 Score [38] [10] | Harmonizes precision and recall into a single score to find a balance. |
| Need for Ranking & Overall Performance View | ROC AUC [38] | Evaluates the model's ranking capability across all thresholds. |
| Highly Imbalanced Data, Focus on Positive Class | PR AUC (Average Precision) [38] | Provides a more realistic view of performance on the rare class. |
Diagram 2: Logical relationships between the confusion matrix and key classification metrics, showing how core components feed into different calculations.
Evaluation Metrics for Regression
Regression metrics quantify the difference between the continuous values predicted by a model and the actual observed values. These differences are known as residuals (residual = actual - prediction) [39]. Different metrics aggregate and interpret these residuals in various ways, each with specific sensitivities and use cases.
Key Metric Definitions and Interpretations
Mean Absolute Error (MAE): The average of the absolute differences between predicted and actual values [39]. MAE is linear and provides an easy-to-interpret measure of average error magnitude in the original units of the target variable. It is robust to outliers [39].
MAE = (1/n) * Σ|actual - prediction|Mean Squared Error (MSE): The average of the squared differences between predicted and actual values [39]. By squaring the errors, MSE heavily penalizes larger errors. This property is useful for optimization (as it's differentiable) but makes it sensitive to outliers [39].
MSE = (1/n) * Σ(actual - prediction)²Root Mean Squared Error (RMSE): The square root of the MSE [39]. This brings the error back to the original units of the target variable, improving interpretability. It retains the squaring property of MSE, meaning it also penalizes large errors more than small ones [39].
RMSE = √MSER-squared (R²) or Coefficient of Determination: A scale-independent metric that represents the proportion of the variance in the dependent variable that is predictable from the independent variables [39]. It is a relative measure, often used to compare models on the same dataset. An R² of 1.0 indicates perfect prediction, while 0 indicates the model performs no better than predicting the mean [39].
Mean Absolute Percentage Error (MAPE): The average of the absolute percentage differences between predicted and actual values [39]. It provides an intuitive, percentage-based measure of error, making it easy to communicate to business stakeholders. However, it is asymmetric and can be problematic when actual values are zero or very close to zero [39].
MAPE = (1/n) * Σ|(actual - prediction)/actual|
Strategic Metric Selection for Regression
The choice of a regression metric should be guided by the importance of large errors, the presence of outliers, and the need for interpretability [4] [39].
Table 3: A Guide to Selecting Regression Metrics
| Research Context & Goal | Recommended Metric(s) | Rationale |
|---|---|---|
| General Purpose, Interpretability, Robustness to Outliers | Mean Absolute Error (MAE) [39] | Easy to understand; not overly penalized by occasional large errors. |
| Large Errors are Critical, Model Optimization | (Root) Mean Squared Error (MSE/RMSE) [39] | Heavily penalizes large errors, which is often desirable. RMSE is in the original units. |
| Comparing Model Performance, Explaining Variance | R-squared (R²) [39] | Provides a standardized, unitless measure of how well the model fits compared to a baseline mean model. |
| Communicating Results to Non-Technical Stakeholders | Mean Absolute Percentage Error (MAPE) [39] | Expresses error as a percentage, which is often intuitively understood. |
| Comparing Models Across Different Datasets/Scales | R-squared (R²), MAPE [39] | These normalized or scale-independent metrics allow for fair comparison. |
Experimental Protocols for Metric Evaluation
Protocol for Comparing Binary Classifiers
This protocol outlines a standard methodology for evaluating and selecting between multiple binary classification models, emphasizing robust metric calculation.
- Data Splitting and Preprocessing: Split the dataset into training (e.g., 70%), validation (e.g., 15%), and test (e.g., 15%) sets. The validation set is used for hyperparameter tuning and threshold selection, while the test set is held back for the final, unbiased evaluation. Address class imbalance at this stage if necessary, using techniques like SMOTE on the training set only.
- Model Training and Prediction: Train each candidate model (e.g., Logistic Regression, Random Forest, Gradient Boosting) on the training set. Use the trained models to generate prediction scores (probabilities) for the validation set.
- Threshold Selection and Metric Calculation on Validation Set:
- For metrics that require a threshold (Accuracy, Precision, Recall, F1), generate a table or plot showing the metric values across a range of thresholds (e.g., from 0.1 to 0.9).
- Select the optimal threshold based on the research goal (e.g., maximize F1, achieve 95% recall).
- Apply the chosen threshold to convert prediction scores into class labels.
- Calculate the confusion matrix and all relevant metrics (Accuracy, Precision, Recall, F1) [38] [10].
- Threshold-Independent Metric Calculation on Validation Set: Calculate threshold-independent metrics like ROC AUC and PR AUC directly from the prediction scores [38].
- Final Evaluation on Test Set: Apply the model and the threshold selected in Step 3 to the held-out test set. Report all final metrics calculated exclusively on the test set. This provides an unbiased estimate of model performance on unseen data.
- Statistical Significance Testing: Perform statistical tests (e.g., McNemar's test for paired classification results) to determine if the performance differences between the top-performing models are statistically significant.
Protocol for Evaluating Regression Models
This protocol provides a framework for assessing the performance of regression models, focusing on error distribution and model comparison.
- Data Splitting: Split the dataset into training and test sets, ensuring the test set remains untouched during model development. Use k-fold cross-validation on the training set for robust hyperparameter tuning.
- Model Training and Prediction: Train regression models (e.g., Linear Regression, Decision Tree Regressor, etc.) on the training set. Generate predictions for the test set.
- Residual Analysis:
- Calculate the residuals (actual - prediction) for each observation in the test set [39].
- Plot a histogram and a Q-Q plot of the residuals to check for normality. Many model assumptions rely on residuals being approximately normally distributed.
- Plot residuals against predicted values. A healthy model will show residuals randomly scattered around zero with constant variance (homoscedasticity). Any pattern (e.g., a funnel shape) indicates a model flaw (heteroscedasticity).
- Calculation of Multiple Error Metrics: Calculate a suite of error metrics on the test set predictions, including MAE, MSE, RMSE, and MAPE [39]. Reporting multiple metrics provides a holistic view of model performance.
- Calculation of Goodness-of-Fit Metric: Calculate R-squared on the test set to understand the proportion of variance explained [39].
- Benchmarking: Compare the model's performance (e.g., using MAE or RMSE) against a simple baseline model, such as predicting the mean or median of the training target variable. This contextualizes the model's practical utility.
This section details key software tools and libraries that facilitate the implementation of the evaluation metrics and protocols discussed in this guide.
Table 4: Key Research Reagent Solutions for Metric Implementation
| Tool / Library | Primary Function | Key Features for Metric Evaluation |
|---|---|---|
| scikit-learn (Python) | General-purpose ML library | Provides comprehensive suite of functions: accuracy_score, precision_score, recall_score, f1_score, roc_auc_score, mean_absolute_error, mean_squared_error, r2_score. Essential for standard model evaluation [35] [38]. |
| Evidently AI (Python) | AI Observability and Evaluation | Specializes in model evaluation and monitoring. Offers interactive visualizations for metrics, data drift, and model performance reports, going beyond static calculations [15]. |
| Neptune.ai | ML Experiment Tracking | Logs, visualizes, and compares ML model metadata (parameters, metrics, curves) across multiple runs. Crucial for managing complex experiments and metric comparisons [38]. |
| LightGBM / XGBoost | Gradient Boosting Frameworks | High-performance algorithms for both classification and regression that provide native support for custom evaluation metrics and are widely used in competitive and industrial settings [38]. |
| TensorFlow / PyTorch | Deep Learning Frameworks | Offer low-level control for building custom model architectures (including neural networks for regression and classification) and implementing tailored loss functions that align with evaluation metrics [35]. |
Clinical prediction models are increasingly fundamental to precision medicine, providing data-driven estimates for individual patient diagnosis and prognosis. These models fall broadly into two categories: diagnostic models, which estimate the probability of a specific condition being present, and prognostic models, which estimate the probability of developing a specific health outcome over a defined time period [40]. In oncology and other medical fields, these models enable superior risk stratification compared to simpler classification systems by incorporating multiple predictors simultaneously to generate more precise, individualized risk estimates [40]. The advent of machine learning (ML) and artificial intelligence (AI) has significantly expanded the methodological toolkit available for model development, offering enhanced capabilities to handle complex, non-linear relationships in multimodal data [40] [41].
However, the development and implementation of robust, clinically useful models present substantial methodological challenges. Many published models suffer from poor design, methodological flaws, incomplete reporting, and high risk of bias, limiting their clinical implementation and potential impact on patient care [40] [42]. This technical guide provides a comprehensive framework for the development, evaluation, and implementation of diagnostic and prognostic models within the context of predictive model performance metrics research, with specific considerations for researchers, scientists, and drug development professionals engaged in advancing precision medicine.
Foundational Concepts and Definitions
Diagnostic vs. Prognostic Prediction Models
Diagnostic Prediction Models: Estimate the probability of a specific disease or condition at the time of assessment. These models typically use cross-sectional data and are intended to support clinical decision-making regarding the presence or absence of a pathological state [40]. Example applications include models that distinguish malignant from benign lesions or predict the probability of bacterial infection.
Prognostic Prediction Models: Estimate the probability of developing a specific health outcome over a future time period. These models require longitudinal data and are used to forecast disease progression, treatment response, or survival outcomes [40]. Examples include models predicting overall survival in cancer patients or risk of disease recurrence following treatment.
Dynamic Prediction Models (DPMs)
Traditional prognostic models often rely on static baseline characteristics, which may become less accurate over time as patient conditions evolve. Dynamic Prediction Models address this limitation by incorporating time-varying predictors and repeated measurements to update risk estimates throughout a patient's clinical course [43]. These models are particularly valuable in chronic conditions and oncology, where disease trajectories and treatment responses can change substantially over time.
Table 1: Categories of Dynamic Prediction Models and Their Applications
| Model Category | Prevalence | Key Characteristics | Typical Application Scenarios |
|---|---|---|---|
| Two-stage Models | 32.2% | Separates longitudinal modeling from survival analysis | Initial studies with limited repeated measures |
| Joint Models | 28.2% | Simultaneously models longitudinal and survival data | Complex trajectory analysis with informative dropout |
| Time-dependent Covariate Models | 12.6% | Incorporates time-varying predictors in Cox models | Settings with regularly measured time-varying biomarkers |
| Multi-state Models | 10.3% | Models transitions between clinical states | Disease progression with defined intermediate events |
| Landmark Cox Models | 8.6% | Uses fixed time points for prediction | Dynamic prediction at specific clinical decision points |
| Artificial Intelligence Models | 4.6% | Handles high-dimensional, complex data patterns | Imaging data, multimodal data integration |
Methodological Framework for Model Development
Pre-Development Considerations
Before initiating model development, researchers must address several critical preliminary questions:
Systematic Review of Existing Models: The proliferation of prediction models for similar purposes (e.g., over 900 models for breast cancer decision-support) necessitates comprehensive literature review to avoid redundant efforts [40]. Researchers should systematically identify, critically appraise, and consider validating or updating existing models before developing new ones.
Clinical Purpose and Stakeholder Engagement: Meaningful engagement with end-users (clinicians, patients, healthcare administrators) from the outset ensures model relevance and usability [40]. This collaborative approach helps define the clinical decision the model will support, appropriate target populations, and implementation requirements.
Protocol Development and Registration: Creating a detailed study protocol and registering it on platforms like ClinicalTrials.gov enhances transparency, reduces selective reporting bias, and ensures methodological consistency throughout the research process [40].
Data Requirements and Preparation
Sample Size Considerations: Adequate sample size is critical for developing stable models with minimal overfitting. Sample size calculations should be performed during the planning phase, considering the number of candidate predictors and expected outcome prevalence [40].
Data Quality and Representativeness: Data used for model development should be representative of the target population and clinical setting where the model will be implemented. Prospective data collection is ideal, though well-curated retrospective data may be suitable with appropriate safeguards against bias [40].
Handling Missing Data: Complete-case analysis is generally inappropriate and may introduce significant bias. Multiple imputation or other appropriate missing data methods should be employed to preserve sample size and representativeness [40].
Model Development Techniques
Traditional Regression Approaches: Conventional methods like logistic regression (for binary outcomes) and Cox proportional hazards models (for time-to-event outcomes) remain robust choices for many prediction modeling applications, particularly with limited sample sizes [40].
Machine Learning Algorithms: ML techniques (random forests, gradient boosting, neural networks, etc.) offer advantages for capturing complex non-linear relationships and interactions without pre-specified functional forms [41]. These methods are particularly valuable with high-dimensional data but require careful attention to overfitting.
Feature Selection: Dimensionality reduction and feature selection techniques (e.g., LASSO regression, Boruta algorithm) are essential when working with large predictor sets to improve model interpretability and generalizability [41].
Diagram Title: Prediction Model Development Workflow
Performance Metrics and Validation Strategies
Core Performance Metrics
Comprehensive model evaluation requires assessment across multiple metric domains:
Table 2: Key Performance Metrics for Prediction Models
| Metric Category | Specific Metrics | Interpretation | Optimal Values |
|---|---|---|---|
| Discrimination | Area Under ROC Curve (AUC) | Ability to distinguish between cases and non-cases | 0.7-0.8: Acceptable0.8-0.9: Excellent>0.9: Outstanding |
| C-statistic | Similar to AUC, for time-to-event models | Same as AUC | |
| Calibration | Calibration Slope | Agreement between predicted and observed risks | Slope = 1 indicates perfect calibration |
| Calibration-in-the-large | Overall difference between mean predicted and observed risk | Intercept = 0 indicates perfect calibration | |
| Brier Score | Overall accuracy of probability predictions | 0 = Perfect accuracy0.25 = No discrimination | |
| Clinical Utility | Net Benefit | Clinical value considering tradeoffs at specific thresholds | Higher values indicate greater clinical utility |
| Decision Curve Analysis | Net benefit across range of threshold probabilities | Above "treat all" and "treat none" strategies |
Validation Approaches
Internal Validation: Assesses model reproducibility and overfitting using the development dataset through techniques like bootstrapping or cross-validation [40]. This represents the minimum validation standard for any prediction model.
External Validation: Evaluates model performance in new patient populations from different locations or time periods, providing critical evidence of generalizability and transportability [40] [44]. External validation should ideally precede clinical implementation.
Impact Studies: Assess whether model use actually improves patient outcomes, clinician decision-making, or healthcare efficiency [44]. These studies represent the highest level of evidence for model clinical value.
Advanced Applications: Dynamic Prediction in Oncology
Dynamic prediction models represent a significant advancement in prognostic modeling, particularly valuable in oncology where disease trajectories and treatment responses evolve over time. A recent cross-sectional analysis of 174 dynamic prediction models across 19 cancer types revealed a rising trend in DPM usage (trend test, p < 0.001), with breast, prostate, and lung cancers being the most frequently studied [43].
Dynamic Predictors in Oncology
The most commonly used dynamic predictors in oncology include:
- Intermediate clinical events (24.1%): Local-regional recurrence and distant metastasis
- Tumor size-based metrics (17.2%): Serial imaging measurements
- Prostate-specific antigen (10.3%): For prostate cancer monitoring
- Scores from assessment scales (8.6%): Patient-reported outcomes and performance status
- Circulating free DNA (7.5%): Emerging liquid biopsy biomarkers [43]
Methodological Approaches for Dynamic Modeling
Joint Models: Simultaneously model longitudinal biomarkers and time-to-event outcomes, accounting for measurement error and informative dropout [43]. These represented 28.2% of identified DPMs and are increasingly favored for their statistical rigor.
Landmarking: Focuses prediction at specific clinically relevant time points ("landmarks") using available longitudinal data up to that timepoint [43]. This approach balances complexity with clinical practicality.
Multi-state Models: Model transitions between multiple health states (e.g., remission, recurrence, death), providing a comprehensive framework for complex disease pathways [43].
Implementation Considerations and Barriers
Technical Implementation
Successful implementation requires integration into clinical workflows with minimal disruption:
Integration Modalities: Implemented models most commonly use hospital information systems (63%), web applications (32%), or patient decision aids (5%) [45]. The choice depends on local infrastructure, user preferences, and workflow considerations.
Interoperability: Models must interface effectively with existing electronic health record systems, with attention to data standardization, interoperability, and real-time data access [46] [47].
Post-Deployment Monitoring and Updating
Model performance monitoring after implementation is essential but frequently overlooked. Only 13% of implemented models have documented updates following deployment [45]. Model performance can degrade over time due to changes in patient populations, treatment practices, or disease patterns—a phenomenon known as "model drift."
Regular calibration assessment and scheduled model refitting should be incorporated into implementation plans to maintain prediction accuracy throughout the model lifecycle.
Case Study: AI-Based Prediction Model for Colorectal Cancer Surgery
A recent implementation study demonstrates a comprehensive approach to model development, validation, and clinical integration [47]. Researchers developed an AI-based prediction model for 1-year mortality risk following colorectal cancer surgery using registry data from 18,403 patients.
Model Development and Validation
The model achieved an AUROC of 0.82 (95% CI: 0.81-0.84) in the development set, 0.77 (95% CI: 0.74-0.80) in internal validation, and 0.79 (95% CI: 0.71-0.87) in external validation [47]. The slight performance decrease in validation sets illustrates the expected attenuation when moving from development to independent populations.
Clinical Implementation and Impact
The model was implemented as a decision support tool that stratified patients into four risk groups (A: ≤1%, B: >1-5%, C: >5-15%, D: >15% 1-year mortality risk) with corresponding perioperative care pathways [47]. In a non-randomized before/after study, the comprehensive complication index >20 incidence was 19.1% in the personalized treatment group versus 28.0% in standard care (adjusted OR 0.63, 95% CI: 0.42-0.92) [47].
Research Reagent Solutions
Table 3: Essential Research Components for Prediction Model Development
| Component Category | Specific Tools/Resources | Function | Examples |
|---|---|---|---|
| Data Sources | Electronic Health Records | Provides real-world clinical data for model development | TCGA, GEO databases [41] |
| Clinical Trial Databases | Source of rigorously collected interventional data | National clinical trial registries | |
| Disease Registries | Population-level data with outcome information | National cancer registries [47] | |
| Analytical Tools | Statistical Software | Implementation of modeling algorithms | R, Python with scikit-learn |
| Machine Learning Frameworks | Development of complex AI models | TensorFlow, PyTorch | |
| Validation Frameworks | PROBAST | Risk of bias assessment tool for prediction models | Prediction Model Risk of Bias Assessment Tool [42] |
| TRIPOD+AI | Reporting guideline for prediction model studies | Transparent Reporting guidelines [40] |
Diagram Title: Model Validation to Impact Pathway
The development and implementation of robust diagnostic and prognostic models requires meticulous attention to methodological rigor throughout the model lifecycle—from initial conceptualization through post-deployment monitoring. While technical advancements in machine learning and dynamic modeling offer exciting opportunities for enhanced prediction accuracy, these must be balanced with thoughtful consideration of clinical utility, implementation feasibility, and ongoing performance monitoring.
The validation culture in prediction modeling deserves greater emphasis, with researchers encouraged to prioritize validation studies of existing models over development of new models when evidence is insufficient [44]. Future directions should focus on dynamic model updating, integration of novel data sources, and demonstrated improvement in patient outcomes through rigorous impact studies.
For drug development professionals and clinical researchers, strategic investment in robust prediction models offers the potential to optimize trial design, enhance patient selection, and ultimately accelerate the development of safer, more effective therapies through improved risk stratification and treatment personalization.
In predictive modeling, particularly within clinical and drug development research, selecting appropriate metrics to evaluate model performance is a critical step that directly impacts the interpretation and utility of a model. While numerous metrics exist, the Brier Score and R-squared are two fundamental measures that provide distinct yet complementary insights. The Brier Score assesses the accuracy of probabilistic predictions for binary outcomes, incorporating both discrimination and calibration, and is a strictly proper scoring rule [48] [49]. In contrast, R-squared, also known as the coefficient of determination, is a cornerstone metric for linear regression models, quantifying the proportion of variance in a continuous dependent variable explained by the model [50] [51]. This guide provides an in-depth technical examination of these two metrics, framed within a broader thesis on predictive model performance metrics research. It is designed to equip researchers, scientists, and drug development professionals with the knowledge to accurately implement, interpret, and contextualize these measures, thereby fostering robust model evaluation practices essential for reliable research outcomes.
Brier Score: A Measure for Probabilistic Predictions
Definition and Mathematical Formulation
The Brier Score (BS) is an evaluation metric for the accuracy of probabilistic predictions for binary outcomes. It was introduced by Brier in 1950 for the verification of weather forecasts and has since been widely adopted in healthcare, machine learning, and other fields [48] [49]. The BS is defined as the mean squared difference between the predicted probability and the actual observed outcome. For a set of n predictions, it is calculated as:
$$ BS = \frac{1}{n} \sum{i=1}^{n} (pi - y_i)^2 $$
Here, $pi$ represents the predicted probability of the event occurring for the *i*-th case, and $yi$ is the actual outcome, coded as 1 if the event occurred and 0 if it did not [48] [52]. The score is equivalent to the mean squared error (MSE) applied to probabilistic predictions [48].
The BS is a strictly proper scoring rule, meaning it is minimized if and only if the predicted probabilities are the true underlying risks [48] [49]. This property is crucial as it encourages honest and accurate predictions.
Interpretation and Key Properties
The value of the Brier score always lies between 0.0 and 1.0 [52]. A model with perfect predictive skill, where all predicted probabilities exactly match the observed outcomes, achieves a BS of 0.0. Conversely, the worst possible score is 1.0 [53] [52].
Table 1: Interpretation of Brier Score Values
| Brier Score Value | Interpretation |
|---|---|
| 0.0 | Perfect prediction skill. All predicted probabilities match observed outcomes exactly. |
| Close to 0.0 | High accuracy in probabilistic predictions. |
| Close to 1.0 | Low accuracy in probabilistic predictions. |
| 1.0 | Worst possible prediction skill. |
The BS provides an overall measure of accuracy that incorporates both discrimination (the ability to separate cases from non-cases) and calibration (the agreement between predicted probabilities and observed frequencies) [54] [49]. This holistic view is one of its key strengths.
Experimental Protocol and Calculation
The following protocol outlines the steps for calculating and interpreting the Brier score in a typical model validation setting, such as evaluating a clinical prediction model.
Protocol 1: Calculating and Interpreting the Brier Score
- Data Preparation: Partition your dataset into training and test sets. A common split is 80% for training and 20% for testing [52].
- Model Training: Train your binary prediction model (e.g., Logistic Regression, Random Forest) on the training set.
- Probability Prediction: Use the trained model to generate predicted probabilities for the positive class ($p_i$) for each observation in the test set.
- Score Calculation: Compute the Brier Score by comparing the predicted probabilities ($pi$) to the actual binary outcomes ($yi$) using the formula above. This can be done manually or using library functions such as
brier_score_lossfromsklearn.metricsin Python [52]. - Benchmarking: Compare the calculated BS against a naive baseline. A common baseline is the Brier score of a model that always predicts the event's prevalence, $\bar{y}$. The score for this baseline model is $\bar{y} \cdot (1 - \bar{y})$ [48]. A useful model should have a BS lower than this value.
- Contextual Interpretation: Interpret the BS value within the context of your research domain and the prevalence of the outcome. There is no universal "good" threshold, as it depends on the inherent noise in the problem [48].
Advanced Applications: Weighted Brier Score and Clinical Utility
A key advancement in the use of the Brier score is the development of the weighted Brier score to incorporate clinical utility [54]. The classic BS treats all prediction errors equally, which may not align with clinical consequences where false positives and false negatives have different costs.
The weighted Brier score aligns with a decision-theoretic framework by assigning different weights to misclassifications based on an optimal risk cutoff, c, which reflects the cost trade-offs of a specific clinical application [54]. This establishes a theoretical link to net benefit measures and the H measure, providing a more nuanced evaluation of a model's practical impact [54].
Common Misconceptions and Limitations
Despite its utility, the Brier score is often misinterpreted. Key misconceptions are summarized below [48].
Table 2: Common Misconceptions about the Brier Score
| Misconception | Reality |
|---|---|
| A BS of 0 indicates a perfect model. | A BS of 0 requires extreme (0% or 100%) predictions that exactly match outcomes, which is unrealistic and may indicate errors. |
| A lower BS always means a better model. | Comparing BS across datasets with different outcome prevalences or distributions can be misleading. Comparisons are only valid within the same population and context. |
| A low BS indicates good calibration. | Calibration and BS measure different aspects. A model can have a low BS yet still be poorly calibrated. |
| A BS near the baseline ($\bar{y} - \bar{y}^2$) means the model is useless. | Even perfect predictions can yield a BS near this value if the true risks are close to the mean incidence. |
A significant limitation of the classic Brier score is its dependence on event prevalence. This can lead to counter-intuitive model rankings in scenarios where clinical consequences are discordant with prevalence, making it potentially unsuitable as a sole metric for clinical value [49]. Decision-analytic measures like net benefit are often more appropriate for evaluating clinical utility in such cases [49].
Diagram 1: A workflow for comprehensive model evaluation using the Brier Score and related metrics.
R-squared: The Coefficient of Determination
Definition and Mathematical Formulation
R-squared ($R^2$), or the coefficient of determination, is a statistical measure that evaluates the goodness of fit for linear regression models. It indicates the percentage of the variance in the dependent variable that is explained collectively by the independent variables in the model [50] [51].
R-squared is calculated by comparing the sum of squares of errors (SSE) from the model to the total sum of squares (SST) of the dependent variable:
$$ R^2 = 1 - \frac{SSE}{SST} $$
Where:
- SSE (Sum of Squared Errors) is the sum of the squared differences between the actual ($yi$) and predicted ($\hat{y}i$) values: $\sum (yi - \hat{y}i)^2$. It represents the variability not explained by the model.
- SST (Total Sum of Squares) is the sum of the squared differences between the actual values and the overall mean ($\bar{y}$): $\sum (y_i - \bar{y})^2$. It represents the total variability in the dependent variable [51] [55].
Interpretation and Key Properties
R-squared values range from 0 to 1, or 0% to 100% [50] [51].
Table 3: Interpretation of R-squared Values
| R-squared Value | Interpretation |
|---|---|
| 0% | The model explains none of the variability in the response data. The model's predictions are no better than using the mean of the dependent variable. |
| 0% to 100% | The percentage of the response variable variation that is explained by the linear model. |
| 100% | The model explains all the variability in the response data. All data points fall exactly on the fitted regression line. |
A higher R-squared value generally indicates that more of the variance is explained, suggesting a better fit [51]. However, a high $R^2$ does not automatically mean the model is good for prediction, nor does it imply a causal relationship between the variables [50] [55].
Experimental Protocol and Calculation
The following protocol details the steps for calculating and validating R-squared in a regression analysis.
Protocol 2: Calculating and Validating R-squared in Regression Analysis
- Model Fitting: Fit your linear regression model to the training data.
- Prediction and Error Calculation:
- Generate predictions ($\hat{y}_i$) for your observations.
- Calculate the residuals ($yi - \hat{y}i$) and compute the Sum of Squared Errors (SSE).
- Total Variation Calculation: Calculate the overall mean of the dependent variable ($\bar{y}$) and compute the Total Sum of Squares (SST).
- R-squared Calculation: Compute $R^2$ using the formula $R^2 = 1 - (SSE/SST)$. In practice, this can be done using software like Python's
scikit-learnand itsr2_scorefunction [51]. - Residual Analysis: Before relying on the $R^2$ value, analyze the residual plots (residuals vs. fitted values). Look for any non-random patterns that indicate a biased model (e.g., heteroscedasticity, non-linearity). A good model should have residuals that are randomly scattered around zero [50].
- Contextual Evaluation: Interpret the $R^2$ value in the context of your field of study. For example, in social or behavioral sciences, an $R^2$ of 0.2 might be considered reasonable, whereas in physical processes, values above 0.8 are often expected [50].
Limitations and Adjusted R-squared
R-squared has several critical limitations that researchers must recognize:
- No Indication of Bias: A high $R^2$ does not guarantee the model is unbiased. The residual plots are essential for diagnosing bias [50].
- Non-Linearity: $R^2$ is designed for linear relationships and may not detect non-linear patterns [51].
- Overfitting: $R^2$ can be artificially inflated by adding more predictors to the model, even if they are irrelevant. This can lead to models that fit the sample data well but fail to generalize [50] [51].
To address the overfitting issue, the adjusted R-squared is used. It penalizes the addition of non-informative predictors, providing a more reliable measure for models with multiple independent variables [51].
$$ \text{Adjusted } R^2 = 1 - \left[ \frac{(1 - R^2)(n-1)}{n - k - 1} \right] $$
Where n is the number of observations and k is the number of independent variables. The adjusted $R^2$ will always be less than or equal to the standard $R^2$, and it can help in selecting a more parsimonious model [51].
Table 4: Key Computational Tools for Metric Evaluation
| Tool / Reagent | Function / Application | Example Use Case |
|---|---|---|
sklearn.metrics.brier_score_loss |
Calculates the Brier score for probabilistic predictions. | Evaluating a logistic regression model's probability outputs in a clinical trial risk assessment. |
sklearn.metrics.r2_score |
Calculates the R-squared value for a regression model. | Assessing the goodness-of-fit of a linear model predicting drug concentration from dosage. |
| Calibration Curve (Reliability Diagram) | Visual tool to assess the calibration of a probabilistic model. | Plotting predicted probabilities against observed frequencies to diagnose miscalibration in a medical diagnosis model [53]. |
| Residual Plots | Diagnostic plots to check for non-linearity, heteroscedasticity, and bias in a regression model. | Identifying a non-random pattern in residuals that suggests an important variable is missing from the model [50]. |
| Net Benefit / Decision Curve Analysis | A decision-analytic measure to evaluate the clinical utility of a prediction model across different probability thresholds. | Comparing models to determine which provides the highest net benefit for guiding treatment decisions, factoring in the harm of false positives and false negatives [54] [49]. |
Within the rigorous framework of predictive model performance research, both the Brier score and R-squared serve as foundational, yet distinct, metrics. The Brier score stands as a robust, strictly proper scoring rule for probabilistic classifications, offering an integrated assessment of calibration and discrimination, with emerging weighted versions enhancing its relevance for clinical decision-making. R-squared remains a cornerstone for linear regression, providing an intuitive percentage-based measure of explained variance. Crucially, neither metric is a panacea. A comprehensive evaluation strategy must move beyond a single number, incorporating residual analyses, calibration plots, domain-specific context, and, where appropriate, decision-analytic measures like net benefit. This multi-faceted approach is essential for researchers and drug development professionals to accurately validate models, ensuring they are not only statistically sound but also clinically meaningful and reliable for informing critical decisions.
In the rigorous evaluation of predictive models, particularly within high-stakes fields like drug development, model calibration stands as a critical performance metric. Calibration is a measure of the statistical reliability of a model's probabilistic outputs. A model is considered perfectly calibrated if its predicted probabilities align precisely with the observed empirical frequencies [56]. For instance, among all patients for whom a model predicts a 70% risk of an adverse event, approximately 70% should actually experience that event if the model is well-calibrated [56]. This characteristic is distinct from, and complementary to, a model's discriminative ability (its power to separate classes). A model can have high discrimination yet poor calibration, for example, by consistently over-estimating risk for all patients. For clinical researchers and drug development professionals, relying on a poorly calibrated model for decision-making can lead to inaccurate risk-benefit assessments and suboptimal resource allocation [57].
The evaluation of predictive models rests on two foundational pillars: discrimination and calibration. Discrimination, often measured by metrics like the Area Under the Receiver Operating Characteristic Curve (AUROC) or the C-index for survival data, assesses how well a model ranks patients by risk [58] [57]. Calibration, on the other hand, assesses the veracity of the absolute probability values themselves [58]. This is paramount in clinical settings, where decisions are often based on estimated risk thresholds. The importance of calibration is underscored by its status as the "Achilles heel of predictive analytics," a field where its significance is paramount but often overlooked [58]. This guide provides an in-depth examination of the methodologies for quantitatively evaluating model calibration, framed within the critical context of validating models for use in drug development and clinical research.
Core Concepts and Definitions of Calibration
The term "calibration" encompasses several related but distinct statistical definitions. Understanding these nuances is essential for selecting the appropriate evaluation metric.
Confidence Calibration: This is the most common notion in machine learning. A model is considered confidence-calibrated if for all confidence levels (c), the probability that the model's predicted class is correct, given that its maximum confidence is (c), equals (c) [56]. Formally: [ \mathbb{P}(Y = \text{arg max}(\hat{p}(X)) \; | \; \max(\hat{p}(X))=c ) = c \quad \forall c \in [0, 1] ] In essence, this ensures that when a model makes a prediction with 70% confidence, it is correct 70% of the time across all such instances.
Multi-class Calibration: A stricter definition that considers the entire predicted probability vector. A model is multi-class calibrated if for any prediction vector (q), the true distribution of classes among instances where the model predicts (q) matches (q) itself [56]. This is a much stronger condition than confidence calibration, as it requires alignment for every class probability, not just the maximum.
Class-wise Calibration: This is a weaker, class-specific form of calibration. A model is class-wise calibrated if for each class (k) and any predicted probability (qk) for that class, the true probability of class (k) matches (qk) [56]. Formally: [ \mathbb{P}(Y = k \; | \; \hat{p}k(X)=qk) = q_k ]
Human-Uncertainty Calibration: Emerging in fields with inherent label ambiguity, this definition calibrates a model's predictions against the distribution of human annotator labels rather than a single "ground truth" [56]. It requires the model's predicted probability vector for a specific sample to match the empirical distribution of labels provided by human annotators for that same sample.
Table 1: Summary of Key Calibration Definitions
| Calibration Type | Scope | Formal Requirement | Key Strength |
|---|---|---|---|
| Confidence Calibration | Maximum probability | (\mathbb{P}(Y = \hat{y} | \max(\hat{p})=c) = c) | Intuitive; relates model confidence to accuracy. |
| Multi-class Calibration | Full probability vector | (\mathbb{P}(Y = k | \hat{p}=q) = q_k \quad \forall k) | Most comprehensive reliability assessment. |
| Class-wise Calibration | Per-class probability | (\mathbb{P}(Y = k | \hat{p}k=qk) = q_k) | Useful when specific class probabilities are critical. |
| Human-Uncertainty Calibration | Single-instance vector | (\mathbb{P}{vote}(Y = k | X=x) = \hat{p}k(x)) | Handles ambiguous labels and aligns with human judgment. |
Quantitative Metrics for Evaluating Calibration
Moving beyond definitions, several quantitative metrics have been developed to measure the degree of miscalibration. The choice of metric often involves a trade-off between interpretability, statistical power, and robustness.
The Expected Calibration Error (ECE)
The Expected Calibration Error (ECE) is a widely used binning-based metric for confidence calibration [56]. It operates by grouping predictions into (M) equal-width bins (e.g., [0, 0.1), [0.1, 0.2), ...) based on their maximum confidence. The ECE is then calculated as a weighted average of the absolute difference between the average accuracy and average confidence within each bin: [ \text{ECE} = \sum{m=1}^{M} \frac{|Bm|}{n} |\text{acc}(Bm) - \text{conf}(Bm)| ] where (Bm) is the set of samples in bin (m), (\text{acc}(Bm)) is the empirical accuracy of the bin, and (\text{conf}(B_m)) is the average predicted confidence in the bin [56]. A perfectly calibrated model has an ECE of 0.
Despite its popularity, the ECE has known drawbacks [56]:
- Sensitivity to Binning: The value of ECE can vary significantly with the number of bins chosen.
- Pathologies: A model can achieve a low ECE without having high accuracy, as the metric is focused on reliability of probabilities, not correctness of classifications.
- Focus on Top-Label: It only considers the maximum predicted probability, ignoring the rest of the probability vector.
Advanced Calibration Metrics for Survival Analysis
In time-to-event data, such as that common in clinical trials, calibration assessment is more complex due to right-censoring. The following table compares two modern methods for this setting.
Table 2: Comparison of D-Calibration and A-Calibration for Survival Models
| Feature | D-Calibration | A-Calibration |
|---|---|---|
| Core Principle | Pearson’s goodness-of-fit test on Probability Integral Transform (PIT) residuals [58]. | Akritas’s goodness-of-fit test, designed for censored data [58]. |
| Handling of Censoring | Uses imputation under the null hypothesis, which can be conservative [58]. | Directly handles censoring without imputation, using a specified estimator for the censoring distribution [58]. |
| Statistical Power | Less powerful, particularly under moderate to high censoring rates [58]. | Similar or superior power in all cases, and more robust to different censoring mechanisms [58]. |
| Key Strength | Simple, intuitive test producing a single p-value [58]. | More powerful and less sensitive to censoring, making it preferable for many real-world applications [58]. |
| Primary Limitation | Loss of power due to the imputation process, which can make the test fail to reject poor models [58]. | No significant disadvantages identified relative to D-calibration [58]. |
Experimental Protocols and Evaluation Workflows
Implementing a robust calibration assessment requires a structured experimental protocol. The following diagrams and workflows outline standardized procedures for general classification and survival analysis settings.
General Workflow for Calibration Assessment
The following diagram illustrates the end-to-end process for evaluating a classification model's calibration, from data preparation to metric calculation and visualization.
The foundational step in this workflow is the creation of a calibration plot. This visual tool is generated by first grouping a model's predicted probabilities for a test set with known outcomes into bins (commonly 10 bins: [0-10%], [10-20%], etc.) [57]. For each bin, the mean predicted probability is plotted on the x-axis against the observed empirical frequency (the fraction of positive outcomes) on the y-axis [57]. A perfectly calibrated model will produce a plot where all points fall along the 45-degree diagonal line. Deviations from this line indicate miscalibration: points above the line suggest underconfidence (the model predicted a lower probability than observed), while points below suggest overconfidence.
Specialized Protocol for Survival Model Calibration
Evaluating calibration in survival models requires specific methodologies to handle censored observations. The A-calibration and D-calibration methods provide a structured hypothesis-testing framework.
The core of this protocol is the Probability Integral Transform (PIT). For a survival time (Ti) with a predicted survival function (S(\cdot|Zi)), the PIT residual is calculated as (Ui = S(Ti | Zi)) [58]. If the model is perfectly calibrated and the survival function is continuous, these (Ui) values follow a standard uniform distribution, (U(0,1)), in the absence of censoring [58]. The key innovation of A-calibration is its use of Akritas's goodness-of-fit test, which is specifically designed for randomly right-censored data. This test evaluates whether the transformed and censored residuals adhere to the uniform distribution without relying on the imputation strategies that weaken D-calibration, leading to a more powerful test [58].
The Scientist's Toolkit: Essential Reagents for Calibration Experiments
To implement the evaluation protocols described, researchers require a set of conceptual and software-based tools.
Table 3: Essential Research Reagents for Calibration Analysis
| Reagent / Tool | Type | Primary Function |
|---|---|---|
| Calibration Plot | Diagnostic Visual | Provides an intuitive, visual assessment of model calibration across the probability spectrum [57]. |
| Expected Calibration Error (ECE) | Numerical Metric | Summarizes the average miscalibration of a model using a binning approach, providing a single number for comparison [56]. |
| A-Calibration Test | Statistical Test | A powerful hypothesis test for assessing the calibration of survival models in the presence of random right-censoring [58]. |
| Probability Integral Transform (PIT) | Mathematical Transform | Converts observed survival times under a model's predicted distribution into a sample that should be uniform if the model is correct, forming the basis for tests like A- and D-calibration [58]. |
| Inverse Probability of Censoring Weighting (IPCW) | Statistical Method | A technique used to correct for selection bias introduced by censoring, ensuring consistent estimation of performance metrics [58]. |
Application in Drug Development and Clinical Trials
The rigorous evaluation of calibration is not merely an academic exercise; it is a fundamental component of building trustworthy predictive tools for drug development. Well-calibrated models are being explored for several critical applications.
A prominent use case is the creation of virtual comparators or control arms. In one example, researchers used pre-treatment and post-treatment image datasets to train a model. The pre-treatment data was then used to simulate the infarct size if a patient had received only medical therapy instead of the experimental thrombectomy device [59]. This generated a simulated outcome for the control therapy, which was compared against the observed outcome from the trial, providing a powerful within-subject comparison where a randomized controlled trial was not feasible [59]. The integrity of the training data and transparency of the method are absolutely crucial for the credibility of such approaches [59].
Furthermore, predictive analytics are being investigated to augment or potentially replace aspects of animal testing. Computational models might offer a more accurate representation of human biological activity compared to animal models, which can be poor predictors of human response [59]. The validation of these models, including rigorous calibration checks, is essential before they can be trusted for regulatory decisions. Predictive models are also being applied to optimize clinical trial design, for example, by using historical data to inform sample size calculations or by borrowing historical controls to reduce the number of patients required in the control arm of a trial [59].
As the field advances, regulators like the FDA are grappling with a "wild west of algorithms," highlighting the urgent need for robust validation frameworks and external scrutiny to ensure the safe and effective deployment of these powerful tools [59]. A comprehensive calibration assessment is a non-negotiable part of this validation process.
In the field of predictive modeling, particularly in medical statistics and biomarker research, the Area Under the Receiver Operating Characteristic Curve (AUC) has long been the standard metric for evaluating model performance. However, AUC has recognized limitations: it may show only small increases even when a new biomarker provides clinically meaningful information, and it does not directly illustrate how patient classification changes across decision-relevant risk thresholds [60]. To address these limitations, researchers developed more nuanced metrics that better capture the clinical utility of new predictors. The Net Reclassification Improvement (NRI) and Integrated Discrimination Improvement (IDI) were introduced to quantify how well a new model reclassifies subjects—either appropriately or inappropriately—compared to an existing model [61]. These metrics have gained significant traction in biomedical research, with thousands of applications in the literature since their introduction, though their implementation and interpretation require careful consideration [62] [63].
Theoretical Foundations of NRI and IDI
Net Reclassification Improvement (NRI)
The Net Reclassification Improvement (NRI) is a measure that quantifies the improvement in risk prediction achieved by adding a new biomarker to an existing model. Its core concept revolves around assessing how well a new model correctly reclassifies subjects into clinically meaningful risk categories [61]. The NRI is particularly valuable when risk strata have been pre-defined and inform clinical decisions regarding treatment or further testing [63].
The calculation of category-based NRI involves classifying subjects into predetermined risk categories and then examining movement between these categories after incorporating the new biomarker:
- For cases (subjects who experience the event), reclassification to a higher risk category represents appropriate reclassification, while movement to a lower risk category represents inappropriate reclassification.
- For non-cases (subjects who do not experience the event), reclassification to a lower risk category represents appropriate reclassification, while movement to a higher risk category represents inappropriate reclassification [61] [60].
The mathematical formulation of NRI is:
NRI = [P(up|case) - P(down|case)] + [P(down|non-case) - P(up|non-case)]
Where:
- P(up|case) = Proportion of cases moving to higher risk category
- P(down|case) = Proportion of cases moving to lower risk category
- P(down|non-case) = Proportion of non-cases moving to lower risk category
- P(up|non-case) = Proportion of non-cases moving to higher risk category [60]
To address limitations associated with categorical thresholds, a continuous NRI was developed as a category-less version that is more objective and less affected by event rates [61].
Integrated Discrimination Improvement (IDI)
The Integrated Discrimination Improvement (IDI) provides a complementary approach to evaluating predictive performance that does not require predefined risk categories. The IDI measures the average improvement in predicted probabilities across all possible thresholds [60] [63].
The IDI is calculated as:
IDI = (ΔP̄cases - ΔP̄non-cases)
Where:
- ΔP̄_cases = Average improvement in predicted probabilities for cases
- ΔP̄_non-cases = Average change in predicted probabilities for non-cases [60]
In practical terms, the IDI represents the difference in discrimination slopes between the new and old models. It captures both the appropriate increase in predicted risks for cases and the appropriate decrease (or smaller increase) in predicted risks for non-cases when the new biomarker is added to the model [63].
Table 1: Key Characteristics of NRI and IDI
| Measure | What It Captures | Requires Cutoffs? | Clinical Interpretation |
|---|---|---|---|
| AUC | Overall discrimination | No | General model comparison |
| NRI | Movement across decision thresholds | Yes | Useful when treatment decisions hinge on specific risk levels |
| IDI | Average separation of predicted probabilities | No | Overall improvement regardless of cutoffs |
Calculation Methodologies and Workflows
Practical Computation of NRI
The calculation of NRI follows a systematic process that begins with creating a reclassification table. The following workflow illustrates the key steps in calculating both categorical and continuous NRI:
Step-by-Step Calculation Example:
Consider a study evaluating a new biomarker for deep vein thrombosis (DVT) with 416 confirmed cases and 1670 non-cases [60]:
For Cases (DVT = 1):
- Number moving up (appropriate): 123
- Number moving down (inappropriate): 26
- Proportion moving up: 123/416 = 0.296
- Proportion moving down: 26/416 = 0.063
- NRI for cases: 0.296 - 0.063 = 0.233
For Non-Cases (DVT = 0):
- Number moving down (appropriate): 227
- Number moving up (inappropriate): 116
- Proportion moving down: 227/1670 = 0.136
- Proportion moving up: 116/1670 = 0.069
- NRI for non-cases: 0.136 - 0.069 = 0.067
Overall NRI: 0.233 + 0.067 = 0.300
This indicates a net 30% improvement in correct reclassification with the new model [60].
IDI Calculation Methodology
The calculation of IDI follows a more direct approach without needing risk categories:
Step-by-Step Calculation Example:
Calculate the average predicted probability for cases:
- Base model: 0.13
- Extended model: 0.49
- Difference: 0.36
Calculate the average predicted probability for non-cases:
- Base model: 0.18
- Extended model: 0.28
- Difference: 0.10
Compute IDI: (0.49 - 0.13) - (0.28 - 0.18) = 0.36 - 0.10 = 0.26 [60]
This result indicates a 26% average improvement in discrimination between cases and non-cases with the extended model.
Experimental Applications and Case Studies
Biomarker Evaluation in Toxicology
The Critical Path Institute's Predictive Safety Testing Consortium (PSTC) has utilized NRI and IDI to evaluate novel biomarkers for drug-induced injuries. However, they noted concerns about statistical validity and subsequently recommended likelihood-based methods for significance testing [62].
Table 2: Application of NRI and IDI in Skeletal Muscle Injury Biomarker Research
| Marker | Fraction Improved Positive Findings | Fraction Improved Negative Findings | Total IDI | Likelihood Ratio Test P-value |
|---|---|---|---|---|
| CKM | 0.828 | 0.730 | 0.2063 | <1.0E-17 |
| FABP3 | 0.725 | 0.775 | 0.2217 | <1.0E-17 |
| MYL3 | 0.688 | 0.818 | 0.2701 | <1.0E-17 |
| sTnI | 0.706 | 0.787 | 0.2030 | <1.0E-17 |
Source: Adapted from PMC5837334 [62]
In this study of skeletal muscle injury biomarkers, all four novel markers (CKM, FABP3, MYL3, and sTnI) showed substantial improvements in reclassification and discrimination when added to standard biomarkers. The consistently highly significant likelihood ratio test p-values validated these improvements using a statistically sound method [62].
A similar approach was applied to evaluate kidney injury biomarkers:
Table 3: Application of NRI and IDI in Kidney Injury Biomarker Research
| Marker | Fraction Improved Positive Findings | Fraction Improved Negative Findings | Total IDI | Likelihood Ratio Test P-value |
|---|---|---|---|---|
| OPN | 0.659 | 0.756 | 0.158 | <1.0E-17 |
| NGAL | 0.735 | 0.646 | 0.066 | 7.8E-09 |
Source: Adapted from PMC5837334 [62]
Both osteopontin (OPN) and neutrophil gelatinase-associated lipocalin (NGAL) demonstrated significant improvement in detecting drug-induced kidney injury, with OPN showing particularly strong performance in IDI [62].
Critical Assessment and Methodological Controversies
Statistical Limitations and Concerns
Despite their popularity, both NRI and IDI face significant methodological criticisms:
Inflated False Positive Rates: Significance tests for NRI and IDI may have inflated false positive rates, making them unreliable for hypothesis testing [62]. Pepe et al. demonstrated that the NRI is likely to be positive even for uninformative markers, which is not the case for other metrics such as AUC, Brier score, or net benefit [61].
Redundancy with Association Measures: For biomarkers that have already been shown to be risk factors conditional on standard biomarkers, tests of predictive performance may be redundant. Demonstrating that a biomarker is a significant risk factor in a model that includes standard biomarkers may be sufficient to conclude that it improves prediction [62].
Dependence on Risk Categories: The categorical NRI is highly dependent on the choice and number of risk categories, which can lead to manipulation or misinterpretation [64] [63]. This has led to recommendations for using continuous NRI or ensuring that categories are clinically meaningful and pre-specified.
Interpretation Challenges: The NRI sums proportions from different groups (cases and non-cases), which has been criticized as "adding apples and oranges" [65]. This explains why NRI's theoretical range is -200% to +200% rather than -100% to +100%, making clinical interpretation challenging.
Current Recommendations for Best Practices
Based on identified limitations, current methodological recommendations include:
Use Likelihood-Based Methods for Significance Testing: When parametric models are used, likelihood ratio tests are recommended to assess whether a novel biomarker significantly improves prediction [62]. This approach maintains appropriate false positive rates while providing a valid test of improvement.
Pre-specify and Justify Risk Categories: For categorical NRI, risk thresholds should be clinically meaningful and defined a priori [64]. Categories should reflect actual decision thresholds used in clinical practice.
Report Components Separately: Always report the components of NRI (movement in cases and non-cases) separately to allow for appropriate interpretation [64] [63].
Address Calibration: NRI and IDI primarily measure discrimination. Assessment of calibration (how well predicted probabilities match observed probabilities) is also crucial for model evaluation [64].
Supplement with Decision-Analytic Measures: Promising NRI findings should be followed with decision-analytic or formal cost-effectiveness evaluations to assess clinical impact [64].
Implementation Tools and Research Reagents
Statistical Software and Packages
Several specialized statistical packages have been developed to calculate NRI and IDI:
Table 4: Statistical Software Packages for NRI and IDI Calculation
| Package Name | Platform | Key Functions | Data Types Supported |
|---|---|---|---|
| PredictABEL | R | Assessment of risk prediction models | Binary outcomes |
| survIDINRI | R | IDI and NRI for censored survival data | Time-to-event data |
| nricens | R | NRI for risk prediction models | Time-to-event and binary data |
| Integrated Discriminatory Improvement | MATLAB | IDI calculation | Binary outcomes |
Source: Adapted from Wikipedia and MATLAB File Exchange [61] [66]
Essential Methodological Components
The following components are essential for proper implementation of NRI and IDI analyses:
Reference Standard: A gold standard for determining true case status is fundamental for calculating both NRI and IDI [63].
Baseline Prediction Model: A well-established model using standard predictors serves as the reference for comparison.
Extended Prediction Model: The baseline model enhanced with the new biomarker(s) under investigation.
Clinically Meaningful Risk Categories: For categorical NRI, pre-specified risk strata that align with clinical decision thresholds.
Validation Data Set: Independent data for validating performance metrics to avoid overoptimism.
NRI and IDI provide valuable tools for evaluating the contribution of new biomarkers to predictive models, offering insights beyond traditional metrics like AUC. However, researchers must be aware of their methodological limitations, particularly regarding statistical testing and interpretation. Proper implementation requires careful study design, appropriate risk categorization, and the use of validated statistical approaches. When used judiciously and in conjunction with other performance measures, NRI and IDI can meaningfully contribute to assessing the clinical utility of novel biomarkers in medical research and drug development.
Diagnostics and Tuning: Overcoming Common Pitfalls and Biases
Identifying and Correcting Overfitting and Underfitting with Learning Curves
Within predictive model performance metrics research, the capacity to diagnose and remediate suboptimal learning is paramount for developing robust, generalizable models. This technical guide provides researchers and drug development professionals with an in-depth analysis of using learning curves—graphical representations of model performance over time or experience—to identify overfitting, underfitting, and optimal fit [67]. We present a structured diagnostic framework, detailed experimental protocols for generating learning curves, and a suite of corrective strategies. The guide further formalizes key diagnostic metrics into comparative tables, outlines essential research reagent solutions, and provides standardized workflows for implementation, enabling scientists to systematically enhance model reliability in critical applications.
In machine learning, a learning curve is a plot that shows the change in a model's learning performance over experience, typically measured by epochs or the amount of training data [67]. These curves are indispensable diagnostic tools for understanding a model's learning behavior and generalization capability. For researchers in fields like drug development, where predictive models inform critical decisions, ensuring a model is neither underfit nor overfit is a foundational aspect of model validation [68].
This guide frames the use of learning curves within a broader thesis on predictive model performance metrics, asserting that dynamic, trajectory-based diagnostics like learning curves are as crucial as static, single-point metrics (e.g., final accuracy or AUC-ROC). By monitoring the learning process itself, scientists can preemptively identify issues, optimize resources, and build more trustworthy predictive models.
Theoretical Foundations: Diagnosing Model Behavior with Learning Curves
Learning curves typically display two key lines: the training loss, which shows how well the model is fitting the training data, and the validation loss, which indicates how well the model generalizes to unseen data [67] [69]. The relationship between these two curves reveals the model's fundamental learning state.
The Triad of Model Fit
The table below summarizes the defining characteristics of the three primary model conditions.
Table 1: Diagnostic Signatures of Model Fit from Learning Curves
| Model Condition | Training Loss | Validation Loss | Gap Between Curves |
|---|---|---|---|
| Underfit | High; may be flat, noisy, or decreasing but halted prematurely [67] [70]. | High and similar to training loss [69]. | Small or non-existent [71] [69]. |
| Overfit | Low and continues to decrease [67] [72]. | Decreases to a point, then begins to increase [71] [67]. | Large and growing after the inflection point [71] [72]. |
| Good Fit | Decreases to a point of stability [67] [69]. | Decreases to a point of stability [67] [69]. | Small and stable [67] [72]. |
The following diagram illustrates the logical workflow for diagnosing model performance using the learning curve signatures detailed in Table 1.
Experimental Protocol: Generating and Interpreting Learning Curves
This section provides a detailed methodology for conducting learning curve analysis, using a structured approach applicable to diverse datasets.
Detailed Workflow for Learning Curve Analysis
The following Graphviz diagram maps the end-to-end experimental workflow, from data preparation to final diagnosis.
Protocol Steps and Specifications
- Data Preparation: Split the dataset into three parts: a training set (e.g., 70%), a validation set (e.g., 20%), and a held-out test set (e.g., 10%). The validation set must be representative of the problem domain to avoid unrepresentative dataset issues [67] [70]. Standardize or normalize features based on the training set to prevent data leakage.
- Model Selection and Initialization: Select a model with capacity suitable for the problem's complexity. For diagnostic purposes, one might deliberately choose a model that is too simple (e.g., Linear Regression for a complex problem) or too complex (e.g., a Deep Neural Network with many layers for a simple problem) to illustrate underfitting and overfitting, respectively [71] [72].
- Iterative Training: Train the model incrementally. This can be done in two primary ways, as outlined in the table below.
Table 2: Methods for Incremental Model Training in Learning Curve Analysis
| Method | X-Axis | Protocol | Use Case |
|---|---|---|---|
| Epoch-based | Number of training epochs/iterations. | Train the model for a fixed number of epochs. After each epoch, evaluate loss on both training and validation sets [71]. | Diagnosing overfitting due to excessive training. |
| Sample size-based | Number of training examples. | Incrementally increase the size of the training data, retraining the model from scratch each time. The validation set is typically held constant [72]. | Determining if collecting more data will improve performance. |
- Per-Iteration Evaluation: After each training step (epoch or with a new data subset), use a loss function (e.g., Mean Squared Error for regression, Cross-Entropy for classification) to calculate the error on both the training and validation sets. Record these values.
- Curve Generation: Plot the recorded loss values against the experience (epochs or sample size). Use the training loss and validation loss curves to diagnose the model's state based on the signatures in Table 1.
- Diagnosis and Correction: Use the diagnostic framework in Section 2.1 to identify the model's condition and apply the corrective strategies outlined in Section 4.
The Scientist's Toolkit: Corrective Strategies and Reagents
Upon diagnosing an issue, researchers must have a systematic approach to remediation. The following table functions as a "toolkit" of standard solutions.
Table 3: Research Reagent Solutions for Model Correction
| Reagent (Solution) | Function | Primary Use Case |
|---|---|---|
| Increase Model Capacity [70] | Adds complexity (e.g., more layers/nodes in a neural network, deeper trees) to allow the model to learn more intricate patterns. | Correcting Underfitting. |
| Reduce Regularization [70] | Removes or reduces constraints (e.g., lowering weight decay, removing dropout) that may be overly restricting the model's learning. | Correcting Underfitting. |
| Add Early Stopping [71] [70] | Halts training once validation performance stops improving, preventing the model from continuing to learn noise. | Correcting Overfitting. |
| Introduce Regularization (L1/L2, Dropout) [72] [70] | Applies constraints to make the model simpler, penalizing complexity to reduce memorization of training data noise. | Correcting Overfitting. |
| Gather More Training Data [72] [70] | Provides more examples for the model to learn the underlying data distribution rather than the noise in a small set. | Correcting Overfitting. |
| Data Augmentation [70] | Artificially increases the size and diversity of the training data by creating modified versions of existing data (e.g., image rotations). | Correcting Overfitting. |
| Hyperparameter Tuning (e.g., Learning Rate) [70] | Optimizes the training process itself; a learning rate that is too high can cause overfitting, while one too low can cause underfitting. | Correcting Both. |
Advanced Considerations in Learning Curve Analysis
Diagnosing Unrepresentative Datasets
Sometimes, the shape of a learning curve indicates a problem with the data split rather than the model itself [67] [70].
- Unrepresentative Training Set: This is indicated by a validation loss that is consistently and significantly lower than the training loss. It suggests the training data is harder to learn from or lacks the diversity present in the validation set [70].
- Unrepresentative Validation Set: This is indicated by a validation loss that is noisy, shows little improvement, or is paradoxically lower than the training loss. It suggests the validation set is too small or does not adequately represent the task [67] [70].
- Solution: The primary remedy for both issues is to ensure a random and stratified split of the data. Employing k-fold cross-validation is a robust method to mitigate these issues, as it allows all data to be used for both training and validation across different folds, providing a more reliable performance estimate [70].
Learning curves are a powerful, dynamic diagnostic tool that should be integral to the model development lifecycle, especially in high-stakes research environments like drug development. By moving beyond final performance metrics to analyze the learning trajectory, scientists can proactively diagnose and correct model pathologies like underfitting and overfitting. The frameworks, protocols, and toolkits presented in this guide provide a systematic approach to cultivating robust, generalizable, and high-performing predictive models, thereby strengthening the foundation of data-driven scientific research.
In predictive modeling, the class imbalance problem presents a significant challenge, particularly in high-stakes fields like healthcare and drug development. This challenge arises when one class significantly outnumbers others, causing models to exhibit bias toward the majority class and perform poorly on critical minority class predictions [73]. The "class imbalance problem" is frequently encountered in real-world applications such as fraud detection, disease diagnosis, and material discovery [73] [74].
The standard evaluation metrics and algorithms often fail with imbalanced data, as they prioritize overall accuracy over minority class detection. Resampling techniques have emerged as fundamental strategies to address this by rebalancing class distributions before model training. This technical guide examines oversampling, undersampling, and SMOTE variants within a comprehensive predictive model performance framework, providing researchers with evidence-based methodologies for handling imbalanced data scenarios.
Understanding Class Imbalance in Predictive Modeling
The Fundamental Challenge
Class imbalance occurs when datasets contain disproportionate class representations, causing standard classifiers to favor majority classes. This bias stems from algorithmic design principles that optimize for overall accuracy without considering distribution skew [75]. In practical terms, a model achieving 95% accuracy might fail completely on a minority class representing 5% of data, which is often the most critical to identify correctly.
The problem extends beyond simple ratio disparities to intrinsic data characteristics. Studies identify safe, borderline, and noisy regions within feature space, with the most significant classification challenges occurring in borderline and noisy areas where class overlap is prevalent [75]. These regions become particularly problematic when combined with imbalance, as minority class examples in overlapping regions may be treated as noise.
Performance Metrics for Imbalanced Data
Standard accuracy fails as a reliable metric for imbalanced problems. Research demonstrates that proper evaluation requires threshold-dependent and threshold-independent metrics [73] [75]. The selection of appropriate metrics must align with domain-specific costs of misclassification.
Table 1: Key Performance Metrics for Imbalanced Classification
| Metric | Formula | Interpretation | Use Case |
|---|---|---|---|
| F1-Score | ( F1 = 2 \times \frac{Precision \times Recall}{Precision + Recall} ) | Harmonic mean of precision and recall | When balance between false positives and false negatives is needed |
| Balanced Accuracy | ( \frac{1}{2} \left( \frac{TP}{TP+FN} + \frac{TN}{TN+FP} \right) ) | Average of recall for each class | General-purpose metric for imbalanced data |
| G-mean | ( \sqrt{Sensitivity \times Specificity} ) | Geometric mean of class accuracies | When both classes are important |
| Matthew's Correlation Coefficient (MCC) | ( \frac{TP \times TN - FP \times FN}{\sqrt{(TP+FP)(TP+FN)(TN+FP)(TN+FN)}} ) | Correlation between observed and predicted | Balanced measure for all class sizes |
| AUC-PR | Area under Precision-Recall curve | Performance focused on positive class | When positive class is of primary interest |
| AUC-ROC | Area under ROC curve | Overall discriminative ability | General model comparison |
For healthcare applications like disease detection, metrics focusing on minority class performance (AUC-PR, F1-Score) often provide more realistic assessments than traditional accuracy or AUC-ROC [76]. A 2023 systematic review highlighted the critical importance of metric selection in healthcare systems, where reliance on accuracy alone leads to clinically unreliable models [77].
Resampling Techniques: Methodologies and Experimental Protocols
Oversampling Techniques
Oversampling increases minority class representation through duplication or generation of new synthetic examples. The fundamental approach balances class distributions without removing majority class instances.
Random Oversampling duplicates existing minority class instances randomly. While simple to implement, it carries significant risk of overfitting, as models may memorize repeated examples rather than learning generalizable patterns [73]. This method performs best with strong regularization or when combined with ensemble methods.
SMOTE (Synthetic Minority Over-sampling Technique) generates synthetic minority class examples by interpolating between existing instances [78]. The algorithm selects a minority instance, identifies its k-nearest neighbors, and creates new points along the line segments connecting them. This approach expands the minority class region more effectively than duplication alone.
Experimental Protocol for Basic SMOTE Implementation:
- Input: Training set ( D{train} ) with minority class ( S{min} ) and majority class ( S_{maj} )
- Parameter Setting: Determine oversampling percentage ( N ) and number of nearest neighbors ( k )
- For each instance ( xi ) in ( S{min} ):
- Find k-nearest neighbors for ( xi ) from ( S{min} )
- While synthetic samples needed:
- Randomly select neighbor ( x_{zi} ) from k-nearest neighbors
- Generate synthetic sample: ( x{new} = xi + \lambda \times (x{zi} - xi) )
- where ( \lambda ) is random number between 0 and 1
- Output: Augmented training set with original plus synthetic minority samples
Advanced SMOTE Variants
Standard SMOTE has limitations, including potential generation of noisy samples in overlapping regions and inability to account for within-class variance [78]. These limitations have prompted development of numerous variants:
Borderline-SMOTE identifies minority instances near class boundaries and focuses synthetic generation in these regions [78] [79]. This approach strengthens decision boundaries where misclassification risk is highest.
Safe-Level-SMOTE assigns safety measures to minority instances based on neighbor class composition, generating samples in safest regions to avoid noise introduction [78].
ADASYN (Adaptive Synthetic Sampling) uses a density distribution to adaptively generate more samples for minority instances harder to learn [78]. This approach automatically determines the number of synthetic samples needed for each minority example.
Counterfactual SMOTE combines SMOTE with counterfactual generation framework to create informative samples near decision boundaries within safe regions [80]. A 2025 study demonstrated its superiority in healthcare applications where critical outcomes are inherently rare.
HSMOTE (Hybrid SMOTE) integrates density-aware synthesis with selective cleaning to preserve minority manifolds while pruning borderline and overlapping regions [81]. This approach is particularly designed for big data environments with severe class imbalance.
BSGAN represents a cutting-edge approach combining Borderline-SMOTE with Generative Adversarial Networks to generate diverse, Gaussian-distributed synthetic data [79]. This hybrid model achieved remarkable performance, including 100% accuracy on multiple benchmark datasets.
Undersampling Techniques
Undersampling balances datasets by reducing majority class instances. These methods improve class ratio while decreasing computational requirements, though they risk discarding potentially useful majority class information.
Random Undersampling randomly removes majority class instances until desired balance is achieved. While computationally efficient, it may eliminate important patterns and lead to underfitting [73].
Tomek Links identify and remove majority class instances forming "Tomek Links" - pairs of instances from different classes that are each other's nearest neighbors [75]. This cleaning approach specifically targets borderline and ambiguous regions.
Instance Hardness Threshold applies data complexity measures to identify and remove majority class instances that are easy to classify, preserving challenging cases near decision boundaries [73].
UBMD (Undersampling Based on Minority Class Density) is a novel approach incorporating minority class density distribution to guide majority class removal [82]. The method uses kernel density estimation to learn minority class distribution, then removes majority samples located in high-density minority regions while preserving information-rich instances through a fitness-based selection.
Experimental Protocol for UBMD Implementation:
- Input: Training set with feature matrix ( X ) and labels ( y )
- KDE Calculation: Estimate probability density function for minority class using Gaussian kernel
- Filtering: Remove majority class instances falling within high-density minority regions
- Fitness Computation: Calculate sampling fitness for remaining majority instances ( Fitness(xi) = \frac{1}{d(xi, C{min})} \times PDF{min}(x_i) )
- Roulette Selection: Select majority instances proportional to fitness scores
- Output: Balanced dataset with full minority class and selected majority instances
Table 2: Comparative Analysis of Undersampling Methods
| Method | Mechanism | Advantages | Limitations | Computational Complexity |
|---|---|---|---|---|
| Random Undersampling | Random removal of majority samples | Simple, fast, reduces dataset size | Loss of potentially useful information | O(1) |
| Tomek Links | Removes overlapping majority samples | Cleans class boundaries, improves precision | Cannot control final sample size | O(n²) for nearest neighbors |
| Cluster Centroids | Replaces majority with cluster centroids | Preserves overall data distribution | May oversimplify complex structures | O(nk) for k-means |
| Instance Hardness | Removes easy-to-classify majority | Preserves challenging cases | Requires model training first | O(n²) |
| UBMD | Density-based filtering and selection | Preserves information-rich samples, handles overlap | Complex implementation | O(n log n) |
Experimental Framework and Evaluation
Comprehensive Performance Comparison
Recent large-scale evaluations provide empirical evidence for method selection. A 2024 study tested 20 imbalanced algorithms across 58 real-life binary datasets with imbalance rates from 3 to 120, evaluating eight performance metrics [75]. Key findings revealed that no single strategy dominates across all metrics, with optimal approach depending heavily on evaluation criteria.
A 2025 benchmarking study specifically evaluated 31 SMOTE variants on text classification tasks using transformer-based embeddings [78]. The research employed TREC and Emotions datasets vectorized with MiniLMv2, with classification performed using six machine learning algorithms. Results demonstrated significant performance variations across techniques, with the best method depending on dataset characteristics and classifier type.
Table 3: Experimental Performance Comparison Across Domains
| Application Domain | Best Performing Methods | Key Findings | Reference |
|---|---|---|---|
| Healthcare (Glaucoma Prediction) | SMOTE-enhanced AI | AUC 0.83, sensitivity 0.81, specificity 0.77 | [76] |
| Text Classification | Borderline-SMOTE, SVM-SMOTE | Performance varies by dataset; transformer embeddings improve results | [78] |
| Big Data Analytics | HSMOTE with Ensemble Deep Dynamic Classifier | Superior precision, recall, and F-measure on high-dimensional data | [81] |
| Chemistry/Drug Discovery | RF-SMOTE, Balanced Random Forests | Effective for predicting HDAC8 inhibitors; addresses active/inactive compound imbalance | [74] |
| General Benchmarking (58 datasets) | Cost-sensitive learning, EasyEnsemble | Effectiveness metric-dependent; newer algorithms don't necessarily outperform established ones | [75] |
Integrated Decision Framework
Choosing appropriate resampling strategies requires systematic consideration of dataset characteristics, model requirements, and performance priorities. The following decision framework guides method selection:
Research Reagent Solutions: Technical Implementation
Successful implementation of resampling strategies requires specific technical components and methodologies. The following table details essential "research reagents" for experimental work with imbalanced data.
Table 4: Essential Research Reagents for Imbalanced Data Experiments
| Component | Function | Implementation Examples | Considerations |
|---|---|---|---|
| Imbalanced-Learn Library | Python-based resampling toolkit | SMOTE(), BorderlineSMOTE(), TomekLinks() |
Seamless integration with scikit-learn ecosystem |
| Performance Metrics | Model evaluation beyond accuracy | f1_score, balanced_accuracy, precision_recall_curve |
Critical for meaningful performance assessment |
| Strong Classifiers | Algorithms robust to imbalance | XGBoost, CatBoost, Balanced Random Forests | May reduce need for extensive resampling |
| Threshold Tuning Tools | Optimization of decision thresholds | scikit-learn's CalibratedClassifierCV |
Essential for threshold-dependent metrics |
| Data Visualization | Assessment of class distribution | PCA plots, t-SNE, class distribution charts | Identifies overlap and data complexity |
| Cross-Validation Strategies | Robust evaluation protocol | Stratified K-Fold, Repeated Stratified K-Fold | Preserves class distribution in splits |
Resampling strategies for imbalanced datasets represent a critical component of the predictive modeling pipeline, particularly in domains like drug development and healthcare where minority class detection carries significant implications. The empirical evidence demonstrates that method effectiveness depends fundamentally on dataset characteristics, model selection, and evaluation metrics.
Oversampling techniques, particularly SMOTE and its advanced variants, provide powerful mechanisms for addressing imbalance without discarding majority class information. Undersampling approaches offer computational efficiency benefits while requiring careful implementation to avoid information loss. The emerging consensus suggests that simple methods like random oversampling often perform comparably to more complex techniques, with advanced methods providing marginal gains in specific scenarios.
Future directions point toward hybrid approaches combining multiple strategies, adaptive techniques for streaming data, and deeper integration with strong classifiers. As predictive models continue to support critical decisions in scientific research and healthcare, rigorous implementation of appropriate resampling strategies remains essential for developing reliable, unbiased models that perform effectively across all classes.
In predictive model performance metrics research, particularly in scientific fields like drug development, the selection of optimal model hyperparameters is a critical determinant of success. Hyperparameters are configuration variables external to the model that are not learned from data but are set prior to the training process, governing the very learning process itself [83]. These parameters control aspects such as model complexity, learning speed, and capacity, directly influencing a model's ability to identify meaningful patterns in complex biological and chemical datasets common in pharmaceutical research.
The fundamental challenge in hyperparameter optimization stems from the unknown nature of the optimal configuration for any given dataset and model combination. Unlike model parameters, which are learned automatically from training data, hyperparameters must be specified by the researcher, creating a significant search problem in a high-dimensional space [84]. This process, known as hyperparameter tuning or hyperparameter optimization, systematically searches for the hyperparameter combination that minimizes a predefined loss function or maximizes a performance metric on validation data [85].
For researchers and scientists in drug development, where model performance can directly impact discovery timelines and therapeutic outcomes, implementing rigorous hyperparameter optimization methodologies is essential. This technical guide examines three principal hyperparameter tuning techniques—Grid Search, Random Search, and Bayesian Optimization—within the context of predictive model performance metrics research, providing detailed experimental protocols, comparative analyses, and implementation frameworks tailored to the needs of scientific professionals.
Theoretical Foundations of Hyperparameter Optimization
Defining the Hyperparameter Optimization Problem
Hyperparameter optimization can be formally expressed as an optimization problem where the goal is to find the hyperparameter vector (x^*) that minimizes an objective function (f(x)), which typically represents the loss or error of the model evaluated on a validation set [86]:
[ x^* = \arg\min_{x \in \mathcal{X}} f(x) ]
Here, (x) represents a vector of hyperparameters from the domain (\mathcal{X}), and (x^*) is the optimal hyperparameter configuration that yields the lowest validation error [86]. The domain (\mathcal{X}) constitutes the search space, which can include discrete, continuous, and categorical hyperparameters across multiple dimensions.
In practice, the objective function (f(x)) is computationally expensive to evaluate, as each function evaluation requires training a machine learning model on the training data and evaluating it on validation data [86]. This computational expense is particularly pronounced in drug development applications, where models may be complex and datasets large, making efficient optimization strategies essential.
Key Hyperparameters by Model Type
Different machine learning algorithms have distinct hyperparameters that significantly impact model performance. The table below summarizes critical hyperparameters for common model types used in predictive research:
Table 1: Key Hyperparameters by Model Type
| Model Type | Hyperparameters | Impact on Model Performance |
|---|---|---|
| Neural Networks | Learning rate, Number of hidden layers, Number of neurons per layer, Batch size, Epochs, Activation function, Momentum [83] | Controls convergence behavior, model capacity, and training stability. Learning rate particularly affects gradient descent optimization. |
| Support Vector Machines (SVM) | C (regularization parameter), Kernel, Gamma [83] [87] | Governs trade-off between margin maximization and classification error; kernel choice determines feature space transformation. |
| Random Forest/XGBoost | nestimators (number of trees), maxdepth, minsamplesleaf, minsamplessplit, max_features [88] [89] | Affects ensemble diversity, model complexity, and resistance to overfitting. |
The Bias-Variance Tradeoff in Hyperparameter Tuning
Hyperparameter tuning fundamentally addresses the bias-variance tradeoff in machine learning [83]. Models with inappropriate hyperparameter settings may suffer from high bias (underfitting), where the model fails to capture relevant patterns in the data, or high variance (overfitting), where the model fits the training data too closely, including noise, and fails to generalize to unseen data [83].
Proper hyperparameter tuning balances this tradeoff, resulting in models that maintain both accuracy on training data and generalization capability to new datasets [85]. In drug development applications, where dataset sizes may be limited due to the high costs of experimental data collection, this balance is particularly crucial to ensure models generalize to novel compounds or biological targets.
Grid Search Methodology
Theoretical Framework
Grid Search represents the most straightforward approach to hyperparameter optimization, employing an exhaustive brute-force strategy [89]. The method operates by defining a discrete grid of hyperparameter values, then systematically training and evaluating a model for every possible combination of values within this grid [90] [91]. Each point in the grid represents a unique model configuration, which is evaluated using cross-validation to obtain a robust performance estimate [85].
The key advantage of Grid Search is its comprehensive nature—by exploring all specified combinations, it guarantees finding the optimal hyperparameter configuration within the predefined grid [90]. This thoroughness makes Grid Search particularly valuable when researchers have strong prior knowledge about the approximate location of optimal hyperparameters within a bounded search space, or when the hyperparameter space is small enough to make exhaustive search computationally feasible.
Experimental Protocol
Implementing Grid Search involves the following methodological steps:
Define Hyperparameter Grid: Specify a dictionary where keys are hyperparameter names and values are lists of potential settings [87]. For example:
Initialize GridSearchCV Object: Configure the search with the model, parameter grid, cross-validation strategy, scoring metric, and computational resources [91] [87]:
Execute Search: Fit the GridSearchCV object to training data, which triggers the exhaustive search across all parameter combinations [87]:
Extract Optimal Parameters: After completion, access the best performing hyperparameter combination and its associated score [87]:
The following diagram illustrates the exhaustive, parallel evaluation process of Grid Search:
Diagram 1: Grid Search Exhaustive Evaluation Workflow
Performance Analysis
Grid Search's primary strength is its thoroughness within the defined search space, ensuring identification of the optimal combination from the specified candidates [90] [89]. However, this comprehensiveness comes with significant computational costs that grow exponentially with each additional hyperparameter—a phenomenon known as the "curse of dimensionality" [89].
For research applications, Grid Search is most appropriate when:
- The hyperparameter space is relatively small and well-understood
- Computational resources are abundant
- Researchers require the guarantee of having tested all specified combinations
- The relationship between hyperparameters and performance is complex and non-monotonic
In drug development contexts, Grid Search may be suitable for final model optimization after the approximate hyperparameter ranges have been established through faster methods, particularly for well-studied model architectures on datasets of manageable size.
Random Search Methodology
Theoretical Framework
Random Search addresses the computational inefficiency of Grid Search by replacing exhaustive enumeration with random sampling from specified hyperparameter distributions [88] [91]. Rather than evaluating every point in a predefined grid, Random Search selects a fixed number of random combinations from the search space, making it particularly advantageous in high-dimensional hyperparameter spaces [90].
The theoretical justification for Random Search stems from the observation that in many machine learning problems, only a few hyperparameters significantly impact model performance [91]. While Grid Search expends equal computational resources across all dimensions, Random Search naturally allocates more trials to important variables by random chance, often finding competitive solutions with far fewer iterations [90] [91].
Experimental Protocol
Implementing Random Search involves these key methodological steps:
Define Hyperparameter Distributions: Specify probability distributions for each hyperparameter rather than discrete lists [88] [89]:
Initialize RandomizedSearchCV Object: Configure with the number of iterations to sample [88]:
Execute Search and Extract Results: The fitting and result extraction process mirrors Grid Search [88]:
The random sampling approach of Random Search is visualized in the following diagram:
Diagram 2: Random Search Stochastic Sampling Workflow
Performance Analysis
Random Search typically achieves comparable or superior performance to Grid Search with significantly fewer iterations, as demonstrated in a study where Random Search found better hyperparameters in only 60 iterations than Grid Search did with 1,024 configurations [86]. This efficiency advantage grows as the dimensionality of the hyperparameter space increases [91].
The table below quantifies the comparative performance between Grid Search and Random Search based on empirical studies:
Table 2: Grid Search vs. Random Search Performance Comparison
| Metric | Grid Search | Random Search |
|---|---|---|
| Search Strategy | Exhaustive enumeration | Random sampling from distributions |
| Computational Efficiency | Exponential time complexity (O(n^d)) | Linear time complexity (O(n)) [90] |
| Optimality Guarantee | Finds best in grid | Probabilistic, improves with iterations |
| Parameter Interactions | Explores all interactions | Discovers important interactions by chance |
| Best Use Cases | Small spaces (<5 parameters), discrete parameters | Large spaces, continuous parameters, limited resources [90] |
For drug development researchers, Random Search offers a practical compromise between computational cost and performance, particularly during preliminary investigations or when working with complex models with numerous hyperparameters. The ability to specify continuous distributions for hyperparameters like learning rates or regularization strengths is especially valuable for fine-tuning model performance.
Bayesian Optimization Methodology
Theoretical Framework
Bayesian Optimization represents a paradigm shift in hyperparameter tuning by incorporating learning from past evaluations [86] [92]. Unlike Grid and Random Search, which treat each hyperparameter evaluation as independent, Bayesian methods construct a probabilistic model of the objective function, using this surrogate model to guide the search toward promising regions [86].
The Bayesian Optimization framework consists of two core components:
Surrogate Model: A probability model (p(y|x)) that approximates the expensive objective function, typically using Gaussian Processes, Random Forest Regressions, or Tree Parzen Estimators (TPE) [86] [92]. The surrogate is computationally inexpensive to evaluate and provides both predicted performance and uncertainty estimates.
Acquisition Function: A selection criterion that determines the next hyperparameters to evaluate by balancing exploration (sampling in uncertain regions) and exploitation (sampling where the surrogate predicts good performance) [86]. Common acquisition functions include Expected Improvement (EI), Probability of Improvement, and Upper Confidence Bound (UCB).
This approach enables Bayesian Optimization to make informed decisions about which hyperparameters to test next, typically requiring far fewer objective function evaluations than non-adaptive methods [86].
Experimental Protocol
Implementing Bayesian Optimization involves the following methodological framework:
Define Search Space: Specify bounded ranges for each hyperparameter, which can include continuous, integer, and categorical types [92]:
Initialize Bayesian Optimization Procedure: Configure with the surrogate model and acquisition function [92]:
Execute Optimization: The fitting process sequentially evaluates hyperparameters based on the surrogate model's recommendations [92]:
The sequential model-based optimization process of Bayesian methods is illustrated below:
Diagram 3: Bayesian Optimization Sequential Learning Workflow
Performance Analysis
Bayesian Optimization typically achieves superior efficiency compared to both Grid and Random Search, often finding better hyperparameters with fewer objective function evaluations [86]. In empirical studies, Bayesian methods using Tree Parzen Estimators have demonstrated significantly lower validation errors compared to Random Search for equivalent computation budgets, particularly in complex optimization landscapes [86].
The key advantage of Bayesian Optimization emerges from its ability to model complex relationships between hyperparameters and model performance, allowing it to avoid unpromising regions of the search space that non-adaptive methods would exhaustively explore [86]. This adaptive intelligence makes it particularly valuable for optimizing deep learning architectures and other computationally intensive models where each objective function evaluation requires substantial resources.
For drug development researchers working with large-scale biological data or complex neural architectures, Bayesian Optimization offers the most efficient approach to hyperparameter tuning, potentially reducing computation times from weeks to days while simultaneously improving model performance.
Comparative Analysis and Research Applications
Quantitative Performance Comparison
The three hyperparameter optimization techniques demonstrate distinct performance characteristics across key metrics relevant to predictive model research. The following table synthesizes empirical findings from comparative studies:
Table 3: Comprehensive Comparison of Hyperparameter Optimization Techniques
| Characteristic | Grid Search | Random Search | Bayesian Optimization |
|---|---|---|---|
| Search Strategy | Exhaustive grid | Random sampling | Sequential model-based optimization |
| Optimality | Best in grid | Probabilistic, improves with iterations | Often finds superior solutions with fewer evaluations [86] |
| Computational Efficiency | (O(n^d)), exponential growth | (O(n)), linear growth | (O(n)), with better constant factors [86] |
| Parallelization | Fully parallelizable | Fully parallelizable | Sequential (inherently iterative) |
| Theoretical Guarantees | Finds optimum in discrete grid | Converges to optimum with infinite samples | Faster convergence under smoothness assumptions |
| Best Application Context | Small, discrete search spaces (<5 parameters) | Medium to large search spaces, limited budget | Expensive objective functions, complex search spaces [86] |
| Ease of Implementation | Simple | Simple | Moderate complexity |
| Adaptation to Results | None | None | Learns from all previous evaluations [86] |
Experimental Validation in Research Contexts
In practical research scenarios, the choice of optimization technique significantly impacts both model performance and computational resource utilization. A comparative study on a Random Forest regressor applied to diabetes data demonstrated that Random Search achieved performance comparable to Grid Search while requiring only 15% of the computation time [90]. Similarly, Bayesian Optimization applied to an SVM classifier on breast cancer data improved test accuracy from 94.7% to 99.1% while efficiently navigating a four-dimensional hyperparameter space [92].
For drug development professionals, these efficiency gains translate to tangible benefits in research timelines and computational resource allocation. The ability to rapidly optimize model hyperparameters enables more thorough experimentation with alternative architectures and feature sets, potentially leading to more predictive models for tasks such as compound activity prediction, toxicity assessment, and patient stratification.
Successful implementation of hyperparameter optimization in research environments requires both conceptual understanding and practical tools. The following table outlines essential computational resources for implementing these techniques:
Table 4: Essential Research Reagent Solutions for Hyperparameter Optimization
| Tool/Library | Function | Implementation Example |
|---|---|---|
| Scikit-learn | Provides GridSearchCV and RandomizedSearchCV implementations [91] | from sklearn.model_selection import GridSearchCV |
| Scikit-optimize | Bayesian Optimization implementation with BayesSearchCV [92] | from skopt import BayesSearchCV |
| Optuna | Advanced Bayesian Optimization framework with pruning | import optuna |
| SciPy | Probability distributions for parameter sampling [89] | from scipy.stats import loguniform, randint |
| Cross-validation | Robust performance evaluation strategy [91] | RepeatedStratifiedKFold(n_splits=10, n_repeats=3) |
Hyperparameter optimization represents a critical component in the development of high-performance predictive models for scientific research and drug development. Grid Search provides a comprehensive but computationally expensive approach suitable for small parameter spaces. Random Search offers significantly improved efficiency for medium to large search spaces, making it ideal for preliminary investigations and resource-constrained environments. Bayesian Optimization delivers superior efficiency and performance for complex optimization landscapes by leveraging sequential model-based learning, particularly valuable for computationally intensive models like deep neural networks.
For researchers in drug development and pharmaceutical sciences, the selection of an appropriate hyperparameter optimization strategy should be guided by the specific research context, computational resources, and model characteristics. Random Search serves as an excellent default choice for most applications, while Bayesian Optimization provides advanced capabilities for the most challenging optimization scenarios. As predictive modeling continues to play an increasingly central role in drug discovery and development, rigorous implementation of these hyperparameter optimization techniques will be essential for maximizing model performance and accelerating research progress.
In predictive model performance metrics research, the adage "garbage in, garbage out" is a fundamental truth. Data preprocessing and feature engineering are not mere preliminary steps but constitute the foundational process that determines the ultimate success or failure of predictive models [93]. In high-stakes fields like drug development, where model interpretability and accuracy are paramount, the systematic preparation of data is especially critical [94]. Research indicates that data practitioners dedicate approximately 60-80% of their time to data preparation and preprocessing activities, underscoring their significance in the machine learning pipeline [93] [95]. This investment is justified by the substantial performance improvements that proper preprocessing confers upon predictive models, with some studies suggesting that preprocessing choices can exert a greater influence on final model accuracy than hyperparameter tuning itself [94].
This technical guide examines the critical role of data preprocessing within the context of predictive model performance metrics research, with particular attention to applications in pharmaceutical development and scientific research. We present a systematic framework for implementing preprocessing techniques that enhance model robustness, reproducibility, and predictive validity—attributes essential for research environments where models inform consequential decisions.
The Data Preprocessing Pipeline: A Systematic Framework
A structured approach to data preprocessing ensures consistency and reproducibility, which are essential requirements in scientific research. The preprocessing pipeline can be conceptualized as a sequential workflow with distinct but interconnected stages.
Stage 1: Data Cleaning and Integrity Assurance
Data cleaning addresses fundamental data quality issues that would otherwise compromise model validity. This stage establishes the basic integrity of the dataset before more advanced transformations are applied.
Handling Missing Data: The appropriate method for addressing missing values depends on the mechanism of missingness and the dataset's characteristics. Common approaches include deletion (listwise or pairwise) and imputation using statistical measures (mean, median, mode) or more sophisticated model-based techniques [96]. For biomedical datasets where missing values may contain biological significance, researchers should carefully consider whether imputation preserves or obscures meaningful patterns [94].
Detecting and Treating Outliers: Outliers can disproportionately influence model parameters, particularly in regression-based analyses. Detection methods include:
- Statistical methods: Z-scores, modified Z-scores, and Interquartile Range (IQR) rules
- Visualization techniques: Box plots, scatter plots, and distribution plots [96]
Outlier treatment strategies include removal, transformation, or winsorization, with the choice dependent on whether outliers represent genuine extreme values or measurement artifacts [96].
Eliminating Duplicate Records: Duplicate entries can artificially inflate the significance of certain patterns and introduce bias. Systematic identification and removal of duplicates ensures each observation receives appropriate weight in model training [93].
Stage 2: Data Transformation and Normalization
Transformation techniques standardize data representation to facilitate optimal model performance, particularly for algorithms that assume normalized feature distributions or are sensitive to variable scales.
Feature Scaling Techniques: Different scaling methods are appropriate for different data distributions and modeling scenarios:
| Scaling Method | Mathematical Formula | Use Case | Impact on Model Performance |
|---|---|---|---|
| Standard Scaler | (x - μ) / σ | Normally distributed data; algorithms assuming unit variance | Prevents features with larger variances from dominating objective function [93] [95] |
| Min-Max Scaler | (x - min) / (max - min) | Data with bounded ranges; neural networks requiring specific input ranges | Ensures all features contribute equally to distance calculations [93] [96] |
| Robust Scaler | (x - median) / IQR | Data containing outliers | Reduces outlier influence while maintaining majority distribution structure [93] |
| Max-Abs Scaler | x / max(|x|) | Data centered around zero | Preserves sparsity and sign of data while scaling [93] |
Encoding Categorical Variables: Non-numerical data must be converted to numerical representations compatible with mathematical models:
- One-Hot Encoding: Creates binary columns for each category; appropriate for nominal data without inherent ordering [96] [95]
- Ordinal Encoding: Assigns integer values to ordered categories; preserves meaningful ordinal relationships [96]
- Target Encoding: Replaces categories with the mean of the target variable; can improve signal capture but risks data leakage [96]
Stage 3: Feature Engineering and Selection
Feature engineering transcends mere data preparation by creating new input variables that enhance a model's ability to detect relevant patterns. This process often requires domain expertise to construct meaningful features that capture underlying biological mechanisms.
Feature Creation Techniques:
- Domain-Specific Feature Derivation: Creating clinically relevant variables (e.g., deriving Body Mass Index from height and weight measurements) [95]
- Temporal Feature Extraction: Decomposing timestamp information into biologically meaningful components (e.g., seasonal variations in disease progression) [95]
- Interaction Terms: Capturing synergistic effects between variables (e.g., drug-gene interactions) [94]
Feature Selection Methods: Dimensionality reduction techniques mitigate overfitting and improve model interpretability by identifying the most predictive feature subsets:
| Selection Method | Mechanism | Research Application |
|---|---|---|
| Filter Methods | Statistical measures (correlation, mutual information) | Preliminary feature screening in high-dimensional biological data |
| Wrapper Methods | Feature subset evaluation using model performance | Identifying minimal feature sets for diagnostic models |
| Embedded Methods | Regularization techniques (L1/Lasso) built into model training | Automated feature selection during model optimization [94] |
| Dimensionality Reduction | Projection methods (PCA, t-SNE) | Visualizing high-dimensional data; reducing multicollinearity [96] |
The following diagram illustrates the complete data preprocessing pipeline with its key decision points:
Experimental Protocols for Preprocessing Evaluation
Protocol 1: Assessing Imputation Method Impact on Model Performance
Objective: To evaluate the effect of different missing data imputation techniques on predictive model performance metrics.
Materials and Reagents:
| Research Reagent/Resource | Function/Application |
|---|---|
| Complete dataset (pre-imputation) | Baseline for introducing controlled missingness |
| Python scikit-learn environment | Implementation of imputation methods and models |
| Multiple imputation by chained equations (MICE) | Advanced imputation handling complex missingness patterns |
| k-Nearest Neighbors (KNN) imputer | Distance-based imputation preserving local structures |
| Mean/median/mode imputation | Simple baseline imputation methods |
| Regression-based imputation | Model-driven imputation leveraging feature relationships |
Methodology:
- Data Preparation: Begin with a complete dataset (D_complete) and introduce missing values completely at random (MCAR) at controlled rates (e.g., 5%, 15%, 30%)
- Imputation Application: Apply multiple imputation methods (MICE, KNN, mean/median, regression) to create completed datasets
- Model Training: Train identical predictive models (e.g., random forest, logistic regression) on each imputed dataset
- Performance Assessment: Evaluate models on a held-out test set using multiple metrics (AUC-ROC, precision, recall, F1-score)
- Statistical Analysis: Compare performance distributions across imputation methods using appropriate statistical tests (e.g., repeated measures ANOVA)
Expected Outcomes: The experiment quantifies the performance degradation associated with different imputation approaches and missingness rates, providing evidence-based guidance for selecting imputation methods specific to research datasets [94] [96].
Protocol 2: Evaluating Feature Scaling Techniques for Convergence Behavior
Objective: To measure the effect of feature scaling methods on optimization convergence and model performance across algorithm classes.
Materials and Reagents:
| Research Reagent/Resource | Function/Application |
|---|---|
| Unscaled dataset with mixed feature scales | Baseline for scaling comparisons |
| StandardScaler, MinMaxScaler, RobustScaler | Implementation of scaling techniques |
| Gradient-based optimization algorithms | Sensitivity analysis to feature scales |
| Convergence monitoring framework | Tracking iteration-to-optimization progress |
| Distance-based algorithms (SVM, KNN) | Assessing scaling impact on distance metrics |
Methodology:
- Baseline Establishment: Train models on unscaled data to establish performance baselines
- Scaling Application: Apply respective scaling techniques to create normalized datasets
- Convergence Monitoring: Track optimization progress (loss function values per iteration) for gradient-based algorithms
- Performance Benchmarking: Evaluate final model performance on standardized metrics
- Statistical Comparison: Compare convergence rates and stability across scaling methods
Expected Outcomes: This protocol quantifies improvements in training stability and convergence speed attributable to proper feature scaling, particularly for gradient-based optimization algorithms common in deep learning applications [93] [95].
Impact on Predictive Model Performance Metrics
The influence of preprocessing decisions manifests across key model evaluation metrics, with particularly pronounced effects in scientific domains:
Accuracy and ROC-AUC: Proper preprocessing directly enhances model discriminative ability. For instance, addressing outliers in biomarker measurements can improve AUC scores by preventing extreme values from disproportionately influencing decision boundaries [1].
Precision and Recall: The tradeoff between precision and recall is significantly affected by preprocessing choices. In drug discovery applications, where false positives in compound screening carry substantial costs, targeted preprocessing strategies can optimize precision without unduly compromising recall [94] [1].
F1-Score: As the harmonic mean of precision and recall, the F1-score provides a balanced assessment of preprocessing efficacy. Research demonstrates that comprehensive preprocessing pipelines can yield F1-score improvements of 15-25% in classification tasks involving biological data [1].
Model Robustness and Generalizability: Preprocessing techniques that address dataset shift and covariate drift enhance model performance on external validation sets—a critical consideration for clinical applications [94].
The relationship between preprocessing components and model evaluation metrics is summarized in the following diagram:
Best Practices for Research Applications
Preventing Data Leakage in Experimental Design
Data leakage represents a critical threat to model validity in research settings, where it can produce optimistically biased performance estimates [96]. Prevention strategies include:
- Temporal Segmentation: For time-series biological data, strictly partition data chronologically so models are trained on past data and tested on future data
- Preprocess Fitting: Calculate preprocessing parameters (e.g., scaling factors, imputation values) exclusively from training data, then apply these parameters to validation and test sets
- Pipeline Architecture: Implement preprocessing and modeling as integrated pipelines to ensure consistent application of transformations [94] [96]
Domain-Specific Considerations for Drug Development
Pharmaceutical research presents unique preprocessing challenges that require specialized approaches:
- Batch Effect Correction: Address technical variations in experimental batches through normalization techniques like Combat or empirical Bayes methods
- Handling Censored Data: Appropriately manage right-censored outcomes in time-to-event analyses common in clinical trial data
- Biomarker Standardization: Normalize biomarker measurements across different assay platforms and measurement units [94]
Reproducibility and Documentation Standards
Research implementations of preprocessing must prioritize reproducibility through:
- Version Control: Maintain versioned datasets documenting all preprocessing transformations
- Parameter Serialization: Save and document all preprocessing parameters for consistent application to new data
- Transparent Reporting: Comprehensive methodology sections detailing preprocessing decisions and their theoretical justifications [94]
Data preprocessing constitutes a methodological foundation rather than a mere technical preliminary in predictive model development for research applications. The systematic implementation of cleaning, transformation, and feature engineering techniques directly determines model performance, interpretability, and ultimately, the validity of scientific insights derived from predictive analytics. As predictive models assume increasingly prominent roles in drug development and scientific discovery, rigorous attention to preprocessing methodologies will remain essential for producing reliable, reproducible, and actionable research outcomes.
Future directions in preprocessing research include the development of domain-adaptive preprocessing techniques that automatically adjust to dataset characteristics, increased integration of causal reasoning into feature engineering, and enhanced methods for preprocessing multimodal data streams characteristic of contemporary scientific investigations. By advancing both the theory and practice of data preprocessing, the research community can unlock further improvements in predictive model performance while strengthening the evidentiary foundation of data-driven scientific discovery.
Leveraging Automated Machine Learning (AutoML) for Efficient Model Optimization
In the rapidly evolving field of data science, Automated Machine Learning (AutoML) has emerged as a transformative technology for optimizing predictive models. By automating the complex, time-consuming processes of algorithm selection, hyperparameter tuning, and feature engineering, AutoML significantly accelerates model development cycles while enhancing performance metrics critical for research applications [97]. For researchers and drug development professionals, this automation is particularly valuable as it enables greater focus on domain-specific problem formulation and interpretation of results rather than technical implementation details. The integration of AutoML into predictive modeling workflows represents a paradigm shift in how organizations approach machine learning, democratizing access to advanced analytical capabilities while ensuring robust, production-ready model performance [98].
This technical guide examines AutoML's role within the broader context of predictive model performance metrics research, with particular emphasis on applications relevant to scientific domains. We present a comprehensive analysis of current AutoML frameworks, performance benchmarking across diverse tasks, experimental protocols for implementation, and emerging trends that are shaping the future of automated model optimization. The content is structured to provide researchers with both theoretical foundations and practical methodologies for leveraging AutoML in their own predictive modeling initiatives, with special consideration for the rigorous evidential standards required in scientific research and drug development.
AutoML Frameworks and Performance Benchmarking
Comparative Analysis of AutoML Frameworks
AutoML frameworks automate the end-to-end machine learning pipeline, from data preprocessing to model deployment, systematically exploring combinations of preprocessing techniques, algorithms, and hyperparameters to discover optimal solutions that might be overlooked in manual processes [97]. The performance of these frameworks varies significantly based on their underlying optimization strategies and architectural approaches.
Table 1: Performance Benchmarking of AutoML Frameworks
| Framework | Optimization Strategy | Reported AUC | Accuracy | Sensitivity | Specificity | Key Advantages |
|---|---|---|---|---|---|---|
| TPOT | Evolutionary Algorithm | 92.1% [99] | 87.3% [99] | 85.8% [99] | 89.0% [99] | Discovers novel pipeline structures; Strong with complex interactions |
| Auto-Sklearn | Bayesian Optimization | - | - | - | - | Leverages meta-learning; Efficient search strategy |
| H2O AutoML | Stacked Ensembles | - | - | - | - | Scalable distributed computing; User-friendly interface |
| LLM-Driven Agent | Adaptive Optimization | Superior to traditional frameworks [100] | - | - | - | Natural language interface; Dynamic search space adjustment |
In a landmark study comparing AutoML frameworks for metabolomic and lipidomic profiling in medical research, TPOT significantly outperformed its counterparts, achieving an area under the curve (AUC) of 92.1%, accuracy of 87.3%, sensitivity of 85.8%, and specificity of 89.0% [99]. The study utilized a dataset comprising 888 metabolic features from 106 patients and 91 matched controls, with each framework allocated identical 600-second time constraints for pipeline search. TPOT's evolutionary algorithm approach enabled it to discover high-performing pipeline structures that may be overlooked by human experts or other automated approaches.
Performance Advantages Over Manual Approaches
Research consistently demonstrates that AutoML can match or exceed manually developed models while drastically reducing development time. A comparative study of predictive analysis found that AutoML, particularly when using logistic regression, outperformed manual methods in prediction accuracy [101]. The research highlighted AutoML's ability to automate tricky parts of the modeling process, including data cleaning, feature selection, and tuning model parameters, thereby saving significant time and effort compared to manual approaches that require more expertise to achieve similar results [101].
In evaluations of Large Language Model (LLM)-driven AutoML systems, 93.34% of users achieved superior performance compared to traditional implementation methods, with 46.67% showing higher accuracy (10%-25% improvement over baseline) and 46.67% demonstrating significantly higher accuracy (>25% improvement over baseline) [102]. Additionally, 60% of users reported substantially reduced development time, demonstrating the dual efficiency benefits of these approaches [102].
Core Optimization Techniques in AutoML
Algorithmic Optimization Strategies
AutoML employs several sophisticated techniques to enhance model performance while managing computational resources:
Hyperparameter Optimization: Advanced approaches using Bayesian optimization have largely replaced traditional grid and random search strategies, demonstrating superior performance in identifying optimal model configurations while minimizing computational overhead [100]. This approach uses previous evaluation results to guide the search for optimal values, making it more efficient than exhaustive methods [103].
Neural Architecture Search (NAS): This approach focuses on the algorithmic design of optimal neural network architectures for specific tasks through reinforcement learning, evolutionary strategies, and gradient-based optimization methods [100]. Recent innovations have significantly improved search efficiency, making automated architecture design feasible for complex deep learning models.
Ensemble Methods: Many high-performing AutoML systems utilize stacked ensembles that combine multiple models to improve accuracy and robustness [100] [98]. This capability allows organizations to achieve results that might be difficult for a single model to replicate, particularly in complex prediction tasks.
Model Compression and Acceleration
For deployment in production environments, particularly in resource-constrained settings, AutoML incorporates specialized optimization techniques:
Pruning: This technique removes unnecessary connections in neural networks, addressing the overparameterization common in many models [103]. Magnitude pruning removes weights with values close to zero, while structured pruning targets entire channels or layers for better hardware acceleration [103]. Research based on the lottery ticket hypothesis suggests that within large networks exist smaller "winning ticket" subnetworks that can achieve comparable performance with significantly fewer parameters [103].
Quantization: This method reduces the precision of numbers used in neural networks, typically converting 32-bit floating-point numbers to lower precision formats like 8-bit integers [103]. This can reduce model size by 75% or more, making models faster and more energy-efficient without significant accuracy loss [103]. Post-training quantization applies this technique after training is complete, while quantization-aware training incorporates precision limitations during the training process for better accuracy preservation [103].
Table 2: Model Optimization Techniques and Performance Impact
| Technique | Implementation Methods | Computational Efficiency | Model Size Reduction | Accuracy Preservation |
|---|---|---|---|---|
| Pruning | Magnitude-based, Structured, Iterative | High improvement | Moderate to high (up to 60% [104]) | High with careful implementation |
| Quantization | Post-training, Quantization-aware training, Dynamic | High improvement | High (75% or more [103]) | Moderate to high |
| Knowledge Distillation | Teacher-student networks, Response-based | Moderate improvement | High | Moderate |
| Neural Architecture Search | Reinforcement learning, Evolutionary, Gradient-based | Low to moderate | Variable | High |
Experimental Protocols and Methodologies
Standardized Experimental Framework
To ensure reproducible and valid results in AutoML experiments, researchers should implement the following standardized protocol:
Data Preprocessing and Cleaning: Prior to model training, data must undergo comprehensive cleaning. For omics data and other scientific datasets, features with missing rates exceeding 30% should be excluded, while less severe missingness can be addressed using sophisticated imputation approaches like Multiple Imputation with Chain Equations (MICE) based on the LightGBM model [99]. Feature scaling should then be applied using methods like StandardScaler to standardize all values to a distribution with a mean of zero and standard deviation of one, ensuring no feature disproportionately influences the model due to its original scale [99].
Training-Testing Partitioning: To ensure robust and generalizable performance estimates, datasets should be subjected to repeated random sub-sampling validation. Specifically, the split into 80% training and 20% testing sets should be repeated 100 times, with performance metrics reported as the mean and standard deviation across all iterations [99].
Framework Configuration: Each AutoML framework should be configured with identical time budgets for pipeline search to ensure fair comparisons. In the metabolomics study, each framework was allocated 600 seconds: TPOT was initialized with a populationsize of 100 and generation count of 10; Auto-Sklearn was used with timeleftforthistask = 600 seconds and perruntimelimit = 60 seconds; and H2O AutoML was executed with maxruntimesecs = 600 [99].
Performance Evaluation Metrics
For comprehensive assessment of AutoML-optimized models, researchers should employ multiple performance metrics:
Discriminatory Performance: Area under the curve (AUC) provides an aggregate measure of model performance across all classification thresholds, while accuracy, sensitivity, and specificity offer threshold-specific assessments of model capability [99].
Business Alignment Metrics: For real-world applications, metrics like customer satisfaction, click-through rates, and other domain-specific key performance indicators help determine whether models are delivering meaningful business results [105].
Computational Efficiency: Inference time, memory usage, and FLOPS (floating-point operations per second) provide insight into computational requirements, with lower values indicating more efficient models that consume less energy [103].
Advanced Integration: LLM-Enhanced AutoML Systems
Architectural Framework
The integration of Large Language Models (LLMs) with AutoML represents a significant advancement in automated model optimization. These systems leverage natural language understanding to create more flexible, intuitive AutoML frameworks that reduce reliance on predefined rules and abstract away complex technical requirements [100].
Performance Advantages
LLM-enhanced AutoML systems have demonstrated remarkable capabilities in empirical evaluations:
Accessibility and Success Rates: Research shows that LLM-based interfaces can dramatically improve ML implementation success rates, with 93.34% of users achieving superior performance in the LLM condition compared to traditional methods [102]. This approach effectively bridges the technical skills gap in organizations, cutting implementation time by 50% while improving accuracy across all expertise levels [102].
Error Reduction and Learning Acceleration: These systems have reduced error resolution time by 73% and significantly accelerated employee learning curves, making them particularly valuable in environments with limited machine learning expertise [102].
Adaptive Optimization: Unlike traditional AutoML approaches that rely on fixed optimization strategies and predefined parameter spaces, LLM-enhanced systems analyze specific task characteristics, suggest initial hyperparameter configurations based on similar historical problems, and dynamically adjust the search space based on intermediate training results [100].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential AutoML Frameworks and Their Research Applications
| Tool/Framework | Primary Function | Research Application Context | Implementation Considerations |
|---|---|---|---|
| TPOT | Automated pipeline optimization using genetic programming | Ideal for complex biomedical data with non-linear relationships; Proven in metabolomics research [99] | Requires substantial computational resources for large datasets |
| Auto-Sklearn | Model selection & hyperparameter tuning via Bayesian optimization | Suitable for structured tabular data common in clinical datasets | Limited to scikit-learn compatible algorithms |
| H2O AutoML | Automated stacking ensemble generation | Effective for large-scale genomic and molecular data analysis | Distributed computing capability enhances scalability |
| LLM-Driven AutoML Agent | Natural language-guided end-to-end ML pipeline | Democratizes ML access for domain experts without coding background [100] | Emerging technology with evolving best practices |
| XGBoost | Gradient boosting with built-in regularization | High-performance tabular data prediction; Often selected by AutoML systems [103] | Minimal hyperparameter tuning required compared to other algorithms |
| Optuna | Hyperparameter optimization framework | Flexible optimization for custom research models | Supports various samplers (TPE, CMA-ES) for different search spaces |
Future Directions and Research Implications
The future of AutoML for model optimization is rapidly evolving, with several key trends shaping its trajectory:
Edge Computing Integration: Gartner predicts that more than 55% of all data analysis by deep neural networks will occur at the point of capture in an edge system by 2025, indicating a significant shift toward distributed AutoML implementations [97]. This trend will enable real-time, edge-computing applications that reduce latency and support immediate decision-making capabilities in clinical and research settings.
Generative AI Convergence: The integration of generative AI and large language models into AutoML systems is enhancing model training processes and expanding the scope of automatable tasks [97]. This technological convergence is making AutoML tools more powerful and versatile, enabling users to tackle increasingly complex machine learning challenges with greater ease and effectiveness.
Explainable AI (XAI) Integration: As AutoML systems become more complex, the need for transparency and interpretability grows. Techniques like SHAP (SHapley Additive Explanations) are being integrated with AutoML to transform "black box" models into biologically meaningful analytical frameworks [99]. In one study, SHAP analysis of the optimal TPOT model identified key metabolites implicating dysregulated pathways in mitochondrial energy metabolism, chronic inflammation, and gut-brain axis communication [99].
For researchers focused on predictive model performance metrics, AutoML represents not just a convenience tool but a fundamental shift in methodological approach. By systematically exploring a wider solution space than practical through manual methods, AutoML can discover novel interactions and model configurations that might otherwise remain undiscovered, potentially leading to scientific insights in addition to optimized predictive performance.
Ensuring Reliability: Robust Validation Frameworks and Model Comparison
Within the critical field of predictive model development for drug discovery and development, accurately estimating future model performance is paramount. A model that performs well on its training data but fails to generalize to new, unseen data can lead to costly and potentially dangerous decisions in clinical trials and therapeutic targeting. This paper addresses two foundational components of robust model evaluation within a broader research thesis on predictive performance metrics. First, we explore k-fold cross-validation, a resampling technique that provides a more reliable estimate of model generalization error compared to a single train-test split [106] [107]. Second, we tackle the subsequent statistical challenge of comparing models validated through such resampling methods, introducing corrected resampled t-tests designed to account for the inherent dependencies in the performance estimates, thereby controlling Type I error rates [108] [109].
k-Fold Cross-Validation: A Robust Protocol for Performance Estimation
The Principle and Motivation
In predictive modeling, a standard practice is to split the available data into a training set, used to build the model, and a held-out test set, used to evaluate it. However, the performance calculated from a single, arbitrary split can be highly variable and optimistic, as the model may have been overfitted to that specific training sample or may have been tested on an unrepresentative subset of data [107]. This is particularly problematic in high-stakes fields like drug development, where data is often limited and expensive to acquire.
K-fold cross-validation (k-fold CV) is a resampling method designed to mitigate this issue. Its core purpose is model checking, not model building [110]. It provides a more robust estimate of how a given modeling procedure (e.g., a specific algorithm with fixed hyperparameters) will perform on unseen data by using the entire dataset for both training and testing in a structured way. The key advantage is that it results in "skill estimates that generally have a lower bias than other methods," such as a single train-test split [106].
Detailed Experimental Protocol
The standard k-fold CV procedure is as follows [106] [107] [111]:
- Shuffle and Partition: Randomly shuffle the dataset, D, and split it into k subsets (the "folds") of approximately equal size. Common choices for k are 5 or 10 [106] [111].
- Iterative Training and Validation: For each of the k folds:
- Designate the current fold as the validation set (or test set).
- Combine the remaining k-1 folds to form the training set.
- Train the predictive model on the training set. It is critical that any data preprocessing (e.g., scaling, feature selection) is learned from the training set and then applied to the validation set to avoid data leakage [106].
- Use the trained model to make predictions on the validation set and compute the desired performance metric (e.g., accuracy, AUC).
- Aggregation: Once all k folds have been used as the validation set, aggregate the k performance metric values. The final performance estimate is typically the mean of these k values.
The following workflow diagram illustrates this process:
The k-Fold CV Output and a Critical Distinction
Upon completing k-fold CV, the researcher obtains k trained models and k performance estimates. A common point of confusion is what to do with these k models. It is a best practice to discard these k models after evaluation, as they have served their purpose of providing a performance estimate for the modeling procedure [110].
The final predictive model that should be deployed or used for further analysis is trained on the entire available dataset [110]. The k-fold CV process is used to check if the model design is sound and to provide a credible estimate of its future performance; once this is confirmed, all data can be used to build the final, most robust model.
Table 1: Impact of the Choice of k on the Cross-Validation Estimate
| Value of k | Bias of Estimate | Variance of Estimate | Computational Cost | Typical Use Case |
|---|---|---|---|---|
| Low (e.g., 5) | Higher | Lower | Lower | Large datasets, rapid prototyping |
| Moderate (e.g., 10) | Moderate | Moderate | Moderate | Standard choice, good trade-off [106] [111] |
| High (e.g., n; LOOCV) | Lower [107] | Higher [107] | Higher | Very small datasets |
The Multiplicity Problem in Resampling and the Need for Correction
The Problem of Correlated Performance Estimates
While k-fold CV provides a better performance estimate, it introduces a statistical challenge when researchers need to compare two different modeling procedures (e.g., Model A vs. Model B). A naive approach is to conduct a paired t-test on the k performance scores from the k-folds of Model A against the k scores from Model B. However, this test relies on the assumption that the performance estimates are independent, which they are not in k-fold CV [108].
The training sets between any two folds overlap substantially, and the validation sets are mutually exclusive partitions of a fixed dataset. This creates a positive correlation between the performance scores across the folds. Ignoring this correlation inflates the variance of the difference between the two models' mean scores. This, in turn, makes the standard t-test anti-conservative, meaning it has an increased probability of detecting a statistically significant difference when none exists (i.e., increased Type I error rate) [109].
Resampling-Based Multiple Testing Correction
The problem of correlated tests is an instance of the broader multiple testing problem (or "multiplicity") in statistics [109]. When many statistical tests are performed simultaneously, the chance of finding at least one spuriously significant result increases. In the context of resampling, this occurs because each resampling iteration (e.g., each fold, each permutation) generates a new set of test statistics.
One powerful approach to address this is the resampling-based test [108] [109]. This method uses permutation or bootstrap procedures to simulate the null distribution of a test statistic while preserving the complex correlation structure of the data. For example, in a genome-wide association study (eQTL analysis), the resampling-based test involves randomly shuffling or bootstrapping the phenotype values and, for each resampled dataset, performing a whole-genome scan to find the maximum test statistic [108]. The corrected P-value is then the proportion of resampled datasets where this maximum test statistic exceeds the maximum test statistic from the original, non-shuffled data. This directly controls the Family-Wise Error Rate (FWER).
Corrected Resampled t-Test: A Solution for Model Comparison
The Theory and Protocol
The Corrected Resampled t-Test (also known as the Nadeau and Bengio correction) applies the principles of resampling-based correction to the specific problem of comparing two models via k-fold CV. It adjusts the standard paired t-test statistic to account for the dependency between the k performance scores.
Let ( \bar{X} ) be the mean difference in performance (e.g., Model A's accuracy minus Model B's accuracy) across the k folds. Let ( \sigma^2 ) be the sample variance of these k differences. The standard t-statistic is ( t = \frac{\bar{X}}{\sigma / \sqrt{k}} ). The corrected test uses ( t{corrected} = \frac{\bar{X}}{\sigma \cdot \sqrt{\frac{1}{k} + \frac{n2}{n1}}} ), where ( n1 ) is the number of samples in the training set and ( n_2 ) is the number in the validation set for a single fold.
The key modification is the denominator, which incorporates the overlap between training sets. The factor ( \frac{n2}{n1} ) estimates the correlation between the performance differences. The degrees of freedom for the test may also need adjustment. This correction results in a more conservative and valid test.
Experimental Protocol for Comparing Two Models
The following protocol details how to conduct a rigorous comparison of two predictive models using k-fold CV and a corrected resampled t-test.
- Define the Modeling Procedures: Clearly specify the two modeling procedures to be compared (e.g., Random Forest vs. Logistic Regression).
- Perform Stratified k-Fold CV: For a classification problem, perform stratified k-fold CV (e.g., k=10) for both models on the same dataset, using the same random splits. This ensures a paired comparison. For each fold, train both models and record their performance on the held-out fold. This results in two vectors of k performance scores: ( SA = [s{A1}, s{A2}, ..., s{Ak}] ) and ( SB = [s{B1}, s{B2}, ..., s{Bk}] ).
- Calculate the Difference in Performance: Compute the per-fold difference in scores: ( di = s{Ai} - s_{Bi} ).
- Compute the Corrected t-Statistic:
- Calculate the mean difference, ( \bar{d} ), and the standard deviation of the differences, ( sd ).
- Compute the corrected t-statistic: ( t = \frac{\bar{d}}{sd \cdot \sqrt{\frac{1}{k} + \frac{n2}{n1}}} )
- Here, ( n2 ) is the size of a single validation fold, and ( n1 ) is the size of the corresponding training set (( n_1 \approx (k-1)/k \cdot n ), where n is the total dataset size).
- Determine Significance: Compare the calculated t-statistic to the critical value from a t-distribution with k-1 degrees of freedom. Alternatively, use a permutation-based approach to generate the null distribution of the corrected t-statistic for more robust P-value calculation.
The logical relationship between the standard and corrected tests is shown below:
Table 2: Comparison of Standard and Corrected Resampled t-Tests
| Feature | Standard Paired t-Test | Corrected Resampled t-Test |
|---|---|---|
| Underlying Assumption | Independent samples | Accounts for correlated samples from overlapping training sets |
| Type I Error Rate | Inflated (Anti-conservative) | Controlled at the nominal level (e.g., α=0.05) |
| Statistical Validity | Invalid for k-fold CV outputs | Valid for k-fold CV and other resampling methods |
| Test Statistic | ( t = \frac{\bar{X}}{\sigma / \sqrt{k}} ) | ( t = \frac{\bar{X}}{\sigma \cdot \sqrt{\frac{1}{k} + \frac{n2}{n1}}} ) |
| Resulting Confidence | Overconfident, leading to spurious claims | More conservative, providing reliable inference |
The Scientist's Toolkit: Essential Research Reagents
The following table details key computational and statistical "reagents" required to implement the methodologies described in this guide.
Table 3: Essential Research Reagents for Robust Model Evaluation
| Reagent / Solution | Function / Purpose | Implementation Example |
|---|---|---|
| Stratified K-Fold Splitting | Ensures that each fold has the same proportion of class labels as the full dataset, preventing biased performance estimates in classification. | sklearn.model_selection.StratifiedKFold |
| Resampling Engine (Permutation/Bootstrap) | Generates resampled datasets under the null hypothesis to empirically construct reference distributions for multiple testing correction. | Custom scripting using numpy.random.permutation or np.random.choice with replacement. |
| Corrected Test Statistic Calculator | Computes the adjusted variance for the t-statistic to account for dependencies in k-fold CV results. | A custom function implementing ( \sqrt{\frac{1}{k} + \frac{n2}{n1}} ) as a variance correction factor. |
| Performance Metric Library | Provides standardized, reproducible calculation of model performance metrics (e.g., AUC, Accuracy, MSE) for fair comparison. | sklearn.metrics (e.g., accuracy_score, roc_auc_score, mean_squared_error) |
| Statistical Distribution Tables/Software | Provides critical values for determining the statistical significance of the corrected test statistic (e.g., t-distribution). | scipy.stats.t for PDF/CDF and critical values. |
For researchers and drug development professionals, relying on a single data split or uncorrected statistical tests for model evaluation is a precarious practice. This guide has detailed two pillars of robust predictive model assessment. K-fold cross-validation provides a more reliable and efficient estimate of model generalization error by maximizing data usage. Following this, the corrected resampled t-test provides a statistically sound framework for comparing models, ensuring that observed differences are not artifacts of correlated resampling outputs. Together, these methodologies form a critical part of a rigorous predictive analytics pipeline, leading to more dependable and reproducible models that can be trusted to inform critical decisions in pharmaceutical research and development.
External validation represents a critical, yet often underutilized, stage in the development of predictive models, particularly within clinical and healthcare domains. This whitepaper delineates the fundamental principles, methodologies, and performance metrics essential for conducting robust external validation. Framed within broader research on predictive model performance metrics, this guide synthesizes current evidence to advocate for rigorous validation practices. Evidence indicates that fewer than 4% of studies in high-impact medical informatics journals perform external validation on data from settings different from their training data, a practice misaligned with responsible research given the potential risks of unreliable models in healthcare [112]. Furthermore, in the specific domain of digital pathology for lung cancer, only approximately 10% of developed models undergo any form of external validation [113]. This guide provides researchers and drug development professionals with the necessary toolkit to bridge this gap, ensuring model generalizability, reliability, and clinical applicability.
The proliferation of artificial intelligence and machine learning models has transformed predictive analytics across numerous fields, including drug development and clinical diagnostics. However, a model's performance on its internal training and testing data often provides an optimistic estimate of its real-world utility. External validation is the process of evaluating a model's performance using data that is entirely separate from the data used for its training and development, typically sourced from different locations, populations, or time periods [113] [112]. This process is the definitive benchmark for assessing a model's generalizability and robustness.
The necessity for external validation is underscored by the pervasive challenge of model overfitting and the inherent limitations of internal validation techniques. Without independent validation, models may fail when confronted with the natural variations found in real-world clinical practice, such as differences in patient demographics, laboratory protocols, imaging equipment, and operational workflows [113]. In healthcare, the consequences of such failures can be severe, impacting patient diagnosis, treatment decisions, and outcomes. External validation provides the empirical evidence needed to trust a model's predictions across diverse, real-world settings, moving it from a theoretical construct to a reliable tool [112].
Methodological Protocols for External Validation
A structured approach to external validation is paramount for generating credible and interpretable results. The following protocols outline the key methodological stages.
Sourcing Independent Validation Datasets
The foundation of any external validation is a high-quality, independent dataset. This dataset must be sourced from a distinct population, institution, or time period compared to the development data.
- Public Datasets: Utilizing publicly available repositories, such as The Cancer Genome Atlas (TCGA) or CPTAC, offers a practical option for initial external validation [113].
- Multi-Center Collaborations: Ideally, validation data should be prospectively collected from multiple, geographically distinct clinical centers. This approach best captures the spectrum of real-world variability.
- Key Considerations: The validation cohort should be of sufficient size, particularly concerning the number of positive events for rare outcomes. Recent research indicates that the stability of metrics like AUC is driven more by the absolute number of events than the event rate itself; for instance, near-zero bias can be achieved with around 1000 events [114]. Furthermore, datasets should be representative of the target population to avoid selection bias and ensure the findings are generalizable [115].
Experimental Workflow for Validation
The following diagram illustrates the end-to-end workflow for a rigorous external validation study, from dataset procurement to final performance reporting.
Key Performance Metrics and Their Calculation
A comprehensive external validation report must include multiple performance metrics to evaluate different aspects of model performance. The selection of metrics should be guided by the clinical context and the consequences of different types of prediction errors.
Table 1: Key Performance Metrics for Classification Models in External Validation
| Metric | Formula | Clinical Interpretation | Consideration in External Validation |
|---|---|---|---|
| Area Under the ROC Curve (AUC) | Integral of Sensitivity (TPR) vs. 1-Specificity (FPR) plot | Probability that a random positive case is ranked higher than a random negative case. | Can be overly optimistic with imbalanced datasets [57]. Stability depends on the number of events, not just the event rate [114]. |
| Sensitivity (Recall) | ( \text{TP} / (\text{TP} + \text{FN}) ) | Proportion of true positive cases correctly identified. | Crucial when the cost of missing a disease (FN) is high. Performance is driven by the number of events [114]. |
| Specificity | ( \text{TN} / (\text{TN} + \text{FP}) ) | Proportion of true negative cases correctly identified. | Vital when the cost of a false alarm (FP) is high. Performance is driven by the number of non-events [114]. |
| Precision (PPV) | ( \text{TP} / (\text{TP} + \text{FP}) ) | Proportion of positive predictions that are correct. | Highly sensitive to disease prevalence in the external dataset. |
| F1-Score | ( 2 \times \frac{\text{Precision} \times \text{Recall}}{\text{Precision} + \text{Recall}} ) | Harmonic mean of precision and recall. | Preferred over accuracy for imbalanced datasets as it balances FP and FN concerns [57] [116]. |
| Accuracy | ( (\text{TP} + \text{TN}) / \text{Total} ) | Overall proportion of correct predictions. | Can be highly misleading for imbalanced datasets and is not recommended as a sole metric [57] [116]. |
For regression models, different metrics are required. The Root Mean Squared Error (RMSE) measures the average magnitude of prediction error and is useful for penalizing large errors, while the Mean Absolute Error (MAE) provides a more robust measure against outliers [4]. The R-squared (R²) value indicates the proportion of variance explained by the model, though it can be deceptive when applied to non-linear models [4].
Beyond Discrimination: Assessing Calibration and Clinical Utility
A model can have excellent discrimination (high AUC) but still be poorly calibrated, meaning its predicted probabilities do not align with the true observed probabilities. Calibration is assessed by plotting predicted probabilities against observed event rates; a well-calibrated model will closely follow the 45-degree line [57]. This is especially important for risk prediction models that inform clinical decisions.
Furthermore, high discrimination and calibration do not guarantee that a model is clinically useful. Decision curve analysis is a method that evaluates the clinical value of a model by calculating its net benefit across a range of probability thresholds, factoring in the relative harm of false positives and false negatives [57]. This analysis helps determine if using the model for clinical decisions would lead to better outcomes than alternative strategies.
A Research Toolkit for External Validation
Successful execution of an external validation study requires both methodological rigor and the right set of analytical tools. The following table details essential "research reagents" for this process.
Table 2: Research Reagent Solutions for External Validation
| Tool/Resource | Function | Example in Practice |
|---|---|---|
| Independent Cohort | Serves as the ground truth for evaluating model generalizability. | A dataset of lung cancer histopathology images from three external hospitals, distinct from the development center [113]. |
| Public Data Repositories | Provide accessible, pre-collected datasets for initial external validation. | The Cancer Genome Atlas (TCGA); Clinical Proteomic Tumor Analysis Consortium (CPTAC) [113]. |
| Statistical Software (R, Python) | Platforms for calculating performance metrics and generating validation plots. | Using scikit-learn in Python to compute AUC, F1-score, and generate ROC curves. |
| Confusion Matrix | A foundational table that breaks down predictions vs. actual outcomes. | Used to derive core metrics like sensitivity, specificity, and precision [1] [57] [116]. |
| Calibration Plot | Visualizes the agreement between predicted probabilities and observed outcomes. | Binning predictions and plotting the mean predicted value vs. the mean observed frequency to assess reliability [57]. |
| Decision Curve Analysis | Quantifies the net clinical benefit of using the model for decision-making. | Comparing the net benefit of a model for initiating a biopsy against the "treat all" and "treat none" strategies [57]. |
External validation is not an optional add-on but an indispensable component of the predictive model lifecycle, especially in high-stakes fields like drug development and clinical diagnostics. It is the only process that can provide credible evidence of a model's robustness, generalizability, and readiness for deployment in the real world. As the field advances, the adoption of rigorous external validation practices, complemented by comprehensive performance assessment beyond a single metric like AUC, will be crucial. This entails a commitment to transparency, the use of diverse and representative datasets, and a focus on both statistical performance and tangible clinical value. By adhering to the protocols and utilizing the toolkit outlined in this guide, researchers can ensure their models are not only statistically sound but also reliable and effective tools for improving human health.
Predictive modeling is a cornerstone of data science, with model selection critically impacting the accuracy, efficiency, and interpretability of results. This paper presents a comparative analysis of three foundational model families within the context of predictive model performance metrics research: the simplicity of Linear Regression, the robust performance of Tree-Based Ensembles (including Random Forest and XGBoost), and the complex pattern recognition capabilities of Neural Networks. While linear regression remains a staple for interpretable, linear problems, tree-based models often dominate structured data challenges, and neural networks excel in capturing intricate, non-linear relationships. A recent large-scale benchmark study of 111 datasets found that deep learning models frequently do not outperform traditional methods like Gradient Boosting Machines on tabular data, highlighting the importance of context-specific model selection [117]. This analysis provides researchers and drug development professionals with a structured framework for evaluating these models based on quantitative performance metrics, computational characteristics, and suitability for specific data modalities.
Core Concepts and Model Architectures
Linear Regression
Linear regression is a foundational statistical method that models the linear relationship between a dependent variable and one or more independent variables. It operates under the assumption of a linear data relationship, making it highly interpretable but limited in capturing complex patterns. The model is represented by the equation ( y = β₀ + β₁x₁ + β₂x₂ + ... + βₙxₙ + ε ), where ( y ) is the target variable, ( x₁, x₂, ..., xₙ ) are input features, ( β₀, β₁, ..., βₙ ) are coefficients, and ( ε ) is the error term [118]. The algorithm works by finding the best-fit line that minimizes the sum of squared differences between predicted and actual values, typically using Ordinary Least Squares (OLS) or gradient descent [118]. Its simplicity makes it computationally efficient and easily explainable, though it struggles with non-linear relationships and high-dimensional data where interactions are complex.
Tree-Based Ensembles
Tree-based ensembles combine multiple decision trees to create more robust and accurate models than individual trees. The Random Forest algorithm operates by creating many decision trees, each using a random subset of the data and features, with final predictions determined through averaging (regression) or majority voting (classification) [119]. This approach reduces overfitting and improves generalization. XGBoost (Extreme Gradient Boosting) is an advanced implementation of gradient boosting that builds trees sequentially, with each new tree correcting errors of the previous ones [120]. Key parameters include the learning rate (eta), maximum tree depth (max_depth), and regularization terms (lambda, alpha) to control model complexity and prevent overfitting [120]. These models handle missing data effectively, provide feature importance rankings, and perform well with large, complex datasets without requiring extensive data preprocessing [119].
Neural Networks
Neural networks are biologically-inspired computing systems consisting of interconnected nodes (neurons) organized in layers: an input layer, one or more hidden layers, and an output layer [118]. Each connection has weights that are adjusted during training through backpropagation and optimization algorithms like stochastic gradient descent or Adam [118]. Unlike linear models, neural networks can learn complex non-linear relationships through activation functions (e.g., ReLU, sigmoid) that introduce non-linearity between layers. This capability makes them particularly powerful for modeling intricate patterns in high-dimensional data, though they require significant computational resources and large datasets to perform effectively [118]. Their "black box" nature can make interpretation challenging, though techniques like attention mechanisms and SHAP values are addressing this limitation.
Experimental Design and Evaluation Methodology
Benchmarking Framework
To ensure a rigorous comparison of model families, we implemented a standardized benchmarking framework based on established experimental protocols from recent literature [117]. All models were evaluated on both regression and classification tasks using 111 diverse tabular datasets varying in scale, dimensionality, and presence of categorical variables. This approach allowed for comprehensive assessment across different data conditions and problem types. The datasets were partitioned using stratified random sampling with an 80/20 train-test split while maintaining original class distributions for classification tasks [121]. To mitigate random variation, all experiments employed a fixed random seed (42) and were repeated with multiple initialization states where applicable. The benchmarking protocol specifically aimed to characterize conditions where deep learning models excel compared to traditional methods, addressing a key gap in existing literature [117].
Performance Metrics
Evaluating model performance requires different metrics for regression and classification tasks. For regression problems, the following key metrics are essential:
- Mean Absolute Error (MAE): Calculated as ( \frac{1}{n} \sum ^{n} _{i=1} |x _{i} - y _{i}| ), MAE represents the average absolute difference between predicted and actual values [122]. It is robust to outliers and provides an intuitive, linear penalty for errors.
- Mean Squared Error (MSE): Computed as ( \frac{1}{n} \sum ^{n} {i=1} (x{i} - y_{i})^2 ), MSE penalizes larger errors more heavily due to the squaring of each term [122]. This differentiability makes it suitable for optimization algorithms.
- Root Mean Squared Error (RMSE): Derived as ( \sqrt{\frac{1}{n}\sum ^{n} {i=1}(x{i} - y_{i})^2 } ), RMSE is on the same scale as the target variable, making it more interpretable than MSE [122].
- R-squared (R²): Representing the proportion of variance in the dependent variable explained by the model, R² is calculated as ( 1 - \frac{SSR}{SST} ), where SSR is the sum of squared residuals and SST is the total sum of squares [122].
For classification tasks, metrics such as accuracy, precision, recall, F1-score, and confusion matrices provide comprehensive assessment of model performance across different classes [121].
Experimental Workflow
The experimental workflow for model comparison follows a systematic process from data preparation to performance evaluation, ensuring reproducible and valid results. The following diagram illustrates this standardized methodology:
Figure 1: Experimental workflow for comparative model analysis
Quantitative Performance Analysis
Regression Performance Comparison
The following table summarizes the typical performance characteristics of each model family on regression tasks, based on aggregated results from multiple benchmark studies:
Table 1: Regression Model Performance Comparison
| Model Family | MAE | MSE | RMSE | R² | Training Time | Inference Speed |
|---|---|---|---|---|---|---|
| Linear Regression | Medium | Medium | Medium | 0.55-0.75 | Fast | Very Fast |
| Random Forest | Low | Low | Low | 0.75-0.95 | Medium | Medium |
| XGBoost | Very Low | Very Low | Very Low | 0.80-0.98 | Medium | Fast |
| Neural Networks | Variable | Variable | Variable | 0.60-0.90 | Slow | Variable |
Performance metrics are expressed relative to each other (Low/Medium/High/Variable) as absolute values are dataset-dependent. R² ranges represent typical performance on structured data benchmarks [117]. Neural networks show variable performance depending on architecture complexity, training duration, and data characteristics [117].
In a specific implementation using the California Housing Prices dataset, a Random Forest regressor achieved the following performance: Mean Absolute Error (MAE): 0.5332, Mean Squared Error (MSE): 0.5559, R-squared (R²): 0.5758, and Root Mean Squared Error (RMSE): 0.7456 [122]. These results demonstrate the practical application of these metrics in evaluating model performance on real-world datasets.
Classification Performance Comparison
For classification tasks, model performance varies significantly based on data complexity and class balance:
Table 2: Classification Model Performance Comparison
| Model Family | Accuracy | Precision | Recall | F1-Score | Handling Class Imbalance |
|---|---|---|---|---|---|
| Linear Models | Low-Medium | Medium | Medium | Medium | Poor |
| Random Forest | High | High | High | High | Good (with stratification) |
| XGBoost | Very High | Very High | Very High | Very High | Excellent (scaleposweight) |
| Neural Networks | Medium-Very High | Medium-Very High | Medium-Very High | Medium-Very High | Good (with weighting) |
In a classification benchmark using a forest cover type dataset with over half a million observations and 54 features, Random Forest achieved 94% accuracy [121]. However, the confusion matrix revealed specific challenges, with approximately 25% of Aspen instances misclassified as Lodgepole Pine, highlighting the importance of examining metrics beyond aggregate accuracy, particularly with imbalanced classes [121].
Implementation Protocols
Model Training Procedures
Linear Regression Implementation
Linear regression implementation follows a straightforward protocol using scikit-learn. After importing necessary libraries (pandas, numpy, sklearn.linear_model), the data is split into features (X) and target variable (y) [122]. The dataset is partitioned into training and testing sets (typically 80/20 split) using train_test_split with a fixed random state for reproducibility [122]. The model is instantiated as LinearRegression() and trained using the fit() method with training data [122]. Predictions are generated on the test set using predict(), and evaluation metrics (MAE, MSE, R²) are calculated by comparing predictions to actual values [122].
Random Forest Implementation
For Random Forest classification, the implementation protocol begins with importing RandomForestClassifier from sklearn.ensemble [119]. After data preparation and feature engineering, the data is split with stratification to maintain class distribution (stratify=y) [121]. The model is instantiated with key parameters including n_estimators=100 (number of trees) and random_state=42 for reproducibility [119]. For regression tasks, RandomForestRegressor is used instead, with similar parameter configuration [119]. After training the model with fit(), predictions are generated and evaluated using accuracy scores, confusion matrices, and classification reports for comprehensive assessment [121].
XGBoost Implementation
XGBoost implementation requires careful parameter configuration across three categories: general parameters (booster: gbtree, gblinear, or dart), tree booster parameters (eta/learning_rate, max_depth, gamma, subsample, colsample_bytree), and task parameters (objective: reg:squarederror for regression or binary:logistic for classification) [120]. The model is trained using xgb.train() with specified parameters and the number of boosting rounds, optionally with custom objective functions and evaluation metrics [123]. Early stopping is implemented using validation sets to prevent overfitting. For scikit-learn compatibility, XGBRegressor and XGBClassifier wrappers provide familiar interfaces.
Neural Network Implementation
Neural network implementation begins with data preprocessing, including normalization or standardization of input features [118]. The model architecture is defined with input layer dimensions matching the feature space, hidden layers with activation functions (typically ReLU), and output layer with activation appropriate to the task (linear for regression, softmax for multi-class classification) [118]. The model is compiled with loss function (MSE for regression, cross-entropy for classification) and optimizer (Adam, SGD). Training proceeds with fit() using training data, with validation split to monitor performance, and optional callbacks for early stopping and learning rate adjustment [118].
Hyperparameter Optimization
Each model family requires specific hyperparameter tuning strategies to achieve optimal performance:
Table 3: Hyperparameter Optimization Guidelines
| Model Family | Key Hyperparameters | Optimization Strategy | Typical Values |
|---|---|---|---|
| Linear Regression | Regularization (L1/L2), Fit Intercept | Grid Search | alpha: [0.001, 0.01, 0.1, 1, 10] |
| Random Forest | nestimators, maxdepth, minsamplessplit, minsamplesleaf | Random Search | nestimators: [100, 200, 500], maxdepth: [10, 20, None] |
| XGBoost | learningrate, maxdepth, subsample, colsamplebytree, nestimators | Bayesian Optimization | learningrate: [0.01, 0.1], maxdepth: [3, 6, 9] |
| Neural Networks | Layers, Units, Learning Rate, Batch Size, Activation Functions | Random Search/Tree-structured Parzen Estimator | Layers: [1-5], Units: [32-512], Learning Rate: [1e-4, 1e-2] |
For tree-based models, parameters like max_depth control model complexity, while subsample and colsample_bytree introduce randomness for better generalization [120]. Neural networks require careful tuning of architecture (layers, units) and optimization parameters (learning rate, batch size) [118]. Cross-validation is essential for reliable hyperparameter evaluation, with separate validation sets used for early stopping in iterative models like XGBoost and neural networks.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Computational Tools for Predictive Modeling Research
| Tool/Reagent | Function | Application Context |
|---|---|---|
| Scikit-learn | Provides implementations of Linear Regression and Random Forest models | Model training, evaluation, and preprocessing for traditional ML |
| XGBoost Library | Optimized distributed gradient boosting library | High-performance tree boosting with GPU support |
| TensorFlow/PyTorch | Deep learning frameworks for neural network implementation | Flexible neural network design and training |
| SHAP/LIME | Model interpretation and explainability tools | Feature importance analysis and prediction explanation |
| Hyperopt/Optuna | Hyperparameter optimization frameworks | Automated search for optimal model parameters |
This comparative analysis demonstrates that each model family possesses distinct strengths and limitations, making them suitable for different research scenarios in drug development and scientific inquiry. Linear regression offers interpretability and efficiency for linearly separable problems with clear feature relationships. Tree-based ensembles, particularly XGBoost and Random Forest, provide robust performance on structured data, with strong predictive accuracy and resistance to overfitting. Neural networks excel at capturing complex, non-linear relationships in high-dimensional data, though they require substantial computational resources and careful regularization. The comprehensive benchmark of 111 datasets reveals that deep learning models do not consistently outperform traditional methods on tabular data, with tree-based ensembles often achieving superior results [117]. This underscores the importance of context-driven model selection based on dataset characteristics, computational constraints, and interpretability requirements. Future research directions include automated model selection systems, hybrid approaches that combine model families, and enhanced interpretation methods for complex neural architectures.
In the field of predictive modeling, the comparison of classifier performance extends far beyond simply selecting the model with the highest reported accuracy. Rigorous statistical evaluation is paramount, particularly in high-stakes fields like drug development, where decisions based on model performance can have significant practical consequences. This guide addresses two fundamental challenges in this process: managing the statistical variance inherent in performance estimates and controlling the false positive rate when multiple comparisons are made. The reproducibility of machine learning research, especially in biomedicine, is often jeopardized by the oversight of these issues [124]. Properly addressing variance and multiple comparisons provides researchers with a robust statistical framework for drawing meaningful and reliable conclusions about classifier performance, thereby strengthening the foundation of predictive model performance metrics research.
The Challenge of Variance in Performance Estimation
The performance metrics of any classifier, such as accuracy or the Area Under the Curve (AUC), are subject to statistical variability due to the finite nature of available data. This variance stems from the random sampling of data into training and test sets and can be exacerbated by the specific resampling procedures used for evaluation, such as cross-validation. The high variance of an performance estimate leads to unreliable model comparisons and reduces the statistical power to detect true improvements in model performance. Studies have shown that the setup of cross-validation alone—such as the choice of the number of folds (K) and the number of repetitions (M)—can significantly impact the perceived statistical significance of performance differences, creating a potential for p-hacking and inconsistent conclusions [124].
Variance of the Multi-class AUC (MAUC)
The Area Under the Receiver Operating Characteristic (ROC) curve is a standard metric for quantifying binary classifiers. For multi-class problems, a popular generalization is the multi-class AUC (MAUC), which averages the pairwise binary AUCs between all classes [125]. For a C-class classifier, the MAUC is defined as:
MAUC Definition
| Component | Formula | Description | ||||
|---|---|---|---|---|---|---|
| Pairwise AUC | (\theta{ij} = \text{Pr}{Xi | i > X_i | j} + \frac{1}{2}\text{Pr}{X_i | i = X_i | j}) | Probability that a class (i) sample is ranked higher than a class (j) sample by the (i)-th classifier output, with ties broken evenly. |
| Overall MAUC | (\theta = \frac{1}{C(C-1)} \sum{i \neq j} \theta{ij}) | Average of all pairwise AUCs. |
The estimated MAUC from finite samples is subject to statistical variability. Due to the complex correlation patterns between the pairwise AUCs, estimating the variance of MAUC is non-trivial. While resampling techniques like bootstrapping can be used, they are computationally expensive and themselves subject to statistical variability [125].
Analytical Variance Estimation for MAUC
A non-parametric approach for estimating the covariance of correlated MAUCs has been developed as a generalization of DeLong's method for binary AUC. This method provides a closed-form, computationally efficient way to estimate the covariance matrix of the vector of pairwise AUCs within a single MAUC, as well as the covariance between MAUCs from multiple competing classifiers evaluated on the same dataset [125]. The key steps of this methodological framework are outlined below.
Experimental Protocol: MAUC Variance Estimation
- Objective: To estimate the variance of a single MAUC and the covariance of MAUCs from multiple classifiers without relying on resampling.
- Input: Classifier rating values (e.g., decision values or class membership probabilities) for all samples in the test set.
- Methodology:
- Compute Pairwise AUCs: Calculate the unbiased estimates of all (\theta_{ij}) components of the MAUC using the classifier's outputs.
- Derive Covariance Matrix: Apply the generalized DeLong's method to compute the covariance matrix (\Sigma) of the vector of pairwise AUCs. The derivation involves U-statistics and results in a compact, matrix factorization form.
- Propagate to MAUC Variance: The variance of the overall MAUC is derived from the covariance matrix of its components. For two correlated MAUCs, the covariance is estimated using the same underlying framework.
- Output: Variance estimate for a single MAUC, or a covariance matrix for multiple MAUCs, which can be used for hypothesis testing.
- Application: This method allows for the efficient computation of confidence intervals and the performance of statistically sound comparisons between multiple multi-class classifiers on the same dataset [125].
The Multiple Comparisons Problem
Understanding the Inflation of False Positives
When multiple statistical tests are performed simultaneously, the chance of obtaining at least one false positive (Type I error) increases dramatically. This is known as the multiple comparisons problem. In the context of classifier comparison, this occurs when a researcher compares multiple models across multiple datasets or using multiple performance metrics without adjusting the significance level.
The family-wise error rate (FWER) is the probability of making at least one Type I error among all hypotheses tested. If (m) independent comparisons are performed, each at a significance level (\alpha = 0.05), the FWER increases to (\bar{\alpha} = 1 - (1 - 0.05)^m). For (m = 10) tests, this probability is approximately 0.40, a stark increase from the nominal 0.05 [126] [127]. Failing to account for this inflation can lead to erroneously declaring an inferior classifier as superior, thus wasting resources and undermining scientific credibility.
Common Adjustment Methods
Several statistical techniques have been developed to control error rates in multiple testing scenarios. The choice of method often involves a trade-off between statistical power (the ability to detect true effects) and the strictness of false positive control [128].
Methods for Multiple Comparison Correction
| Method | Controlled Error Rate | Principle | Advantages & Disadvantages |
|---|---|---|---|
| Bonferroni | Family-Wise Error Rate (FWER) | Divides the significance level (\alpha) by the number of tests (m). Adjusted p-value: (p'i = \min(pi \times m, 1)). | Advantage: Simple to implement. Disadvantage: Very conservative, leads to low statistical power [127]. |
| Holm | Family-Wise Error Rate (FWER) | Step-down method: Orders p-values and compares (p_{(i)}) to (\alpha/(m - i + 1)). | Less conservative than Bonferroni while still controlling FWER [127]. |
| Hochberg | Family-Wise Error Rate (FWER) | Step-up method: Orders p-values and compares (p_{(i)}) to (\alpha/(m - i + 1)). | More powerful than Holm, but requires assumption of independent tests [127]. |
| Benjamini-Hochberg | False Discovery Rate (FDR) | Controls the expected proportion of false discoveries among all significant tests. | Advantage: More power than FWER methods. Disadvantage: Allows some false positives; suitable for exploratory analysis [126] [127]. |
The following diagram illustrates the decision-making process for selecting an appropriate correction method based on the research context and goals.
Experimental Protocol for Comparing Multiple Classifiers
A rigorous protocol for comparing multiple classifiers on a single dataset, which properly accounts for multiple testing, is described below. This protocol uses a combination of cross-validation and statistical testing to ensure robust conclusions [124].
Experimental Protocol: Multiple Classifier Comparison with Corrected Paired Tests
- Objective: To determine if there are statistically significant performance differences among multiple classifiers on a single dataset, while controlling the overall Type I error rate.
- Input: A single dataset with a fixed training/test split or a cross-validation scheme.
- Methodology:
- Performance Estimation: For each classifier, estimate its performance (e.g., accuracy, AUC) using a repeated K-fold cross-validation procedure. This generates a vector of performance scores for each classifier.
- Paired Test Calculation: Perform paired statistical tests (e.g., a paired t-test or a non-parametric alternative like the Wilcoxon signed-rank test) for every pair of classifiers. This pairing is crucial because all classifiers are evaluated on the same resampled data folds, making their performance estimates correlated. This step produces a p-value for each pairwise comparison.
- P-value Adjustment: Apply a multiple comparison correction method (e.g., Holm or Bonferroni) to the entire set of pairwise p-values to control the FWER or FDR.
- Output: A set of adjusted p-values indicating which pairwise differences between classifiers are statistically significant after correction.
- Considerations: The power of this procedure is highly sensitive to the cross-validation setup (number of folds and repetitions). It is also recommended to use tests that account for the non-independence of cross-validation folds, such as the corrected resampled t-test [124].
The Scientist's Toolkit: Key Research Reagents
This table details essential "research reagents" – the key methodological components and statistical tools required for rigorous classifier comparison.
Research Reagent Solutions for Classifier Comparison
| Item | Function & Purpose | Example Instances |
|---|---|---|
| Performance Metric | Quantifies a classifier's predictive accuracy in a single number, enabling comparison. | AUC/MAUC [125], Accuracy, F1-Score [1]. |
| Resampling Procedure | Provides an estimate of a metric's variance and helps assess generalizability by repeatedly evaluating models on different data splits. | K-Fold Cross-Validation, Repeated Cross-Validation, Bootstrapping [124]. |
| Variance Estimator | Quantifies the uncertainty of a performance metric estimate without exhaustive resampling. | Generalized DeLong's method for (M)AUC variance [125]. |
| Paired Statistical Test | Determines if the performance difference between two classifiers (evaluated on the same data splits) is statistically significant. | Paired t-test, Wilcoxon Signed-Rank Test [124]. |
| Multiple Testing Correction | Adjusts significance levels to control the probability of false discoveries when many hypotheses are tested. | Bonferroni correction, Holm's method, Benjamini-Hochberg (FDR) [127]. |
| Optimization Algorithm | Algorithms used to train the classifiers themselves, where reduced variance can lead to more stable and better-performing models. | Variance-reduced optimizers like MARS [129], SVRG, STORM. |
Navigating the complexities of variance and multiple comparisons is not merely an academic exercise but a fundamental requirement for producing reliable and reproducible research in machine learning and predictive modeling. By adopting the frameworks outlined in this guide—utilizing analytical variance estimation for metrics like MAUC, implementing rigorous cross-validation protocols, and applying appropriate multiple testing corrections—researchers and drug development professionals can make confident, data-driven decisions about classifier performance. Integrating these practices into the standard model evaluation workflow is a critical step towards mitigating the reproducibility crisis and advancing the rigorous application of predictive models in scientific discovery.
While traditional metrics like the Area Under the Receiver Operating Characteristic Curve (AUROC) focus on the statistical performance of predictive models, they do not directly inform clinical decision-making by incorporating the consequences of decisions [57] [130]. Decision-analytic measures, particularly Net Benefit and Decision Curve Analysis (DCA), address this gap by weighing the relative harms of false positives and false positives to evaluate the clinical utility of a model or test [131] [57]. This technical guide details the theoretical foundation, methodological protocols, and practical application of DCA, framing it within a broader research thesis on predictive model performance metrics. Designed for researchers and drug development professionals, this whitepaper provides the tools to implement DCA and critically assess whether a model's statistical performance translates into clinical value.
The evaluation of prediction models has traditionally relied on measures of discrimination and calibration [130]. Discrimination, a model's ability to differentiate between patients with and without the outcome, is often quantified by the AUROC [57] [130]. Calibration measures the agreement between predicted probabilities and observed event rates [57] [130]. While essential, these metrics exist in a vacuum separate from clinical consequences. A model with high AUROC might lead to worse patient outcomes if it causes a large number of harmful false positives or misses critical true positives [57].
Decision Curve Analysis, introduced by Vickers and Elkin in 2006, bridges this gap by integrating a formal assessment of clinical trade-offs into model evaluation [131] [130]. The core outcome of DCA is Net Benefit, a single metric that balances the benefit of true positives against the harm of false positives, standardized for a range of clinically reasonable threshold probabilities [131] [132]. This allows researchers to determine if using a model to guide decisions—such as initiating a treatment, performing a biopsy, or ordering a new diagnostic test—is superior to default strategies of "treat all" or "treat none" [131].
Table 1: Comparison of Common Prediction Model Performance Metrics
| Metric | What It Measures | Clinical Context Considered? | Key Limitation |
|---|---|---|---|
| AUROC | Discriminatory power at all thresholds [57] | No | Can be high for models that are not clinically useful; overestimates performance in imbalanced datasets [57] |
| Calibration | Agreement between predicted and observed risk [57] [130] | No | A well-calibrated model can still lead to poor decisions if not considered with Net Benefit [130] |
| F1 Score | Harmonic mean of precision and recall [57] | No | Does not incorporate outcome prevalence or relative value of TP/FP [57] |
| Net Benefit | Clinical utility, weighing benefits vs. harms [131] [57] | Yes | Requires specifying a clinically relevant range of threshold probabilities [131] |
Theoretical Foundations of Net Benefit and Decision Curve Analysis
The Concept of Threshold Probability
Clinical decisions are rarely based on a simple "yes/no" output from a model. Instead, a predicted probability is compared to a threshold probability ((pt)) to determine a course of action [131]. This threshold represents the minimum probability of disease at which a clinician or patient would opt for an intervention (e.g., biopsy, drug therapy) [131]. The value of (pt) is not a statistical property but a reflection of patient preferences, representing the point at which the expected benefit of intervention equals the expected harm [131]. For a patient who is very worried about disease and less concerned about the downsides of intervention, (pt) will be low. Conversely, for a patient focused on avoiding unnecessary procedures, (pt) will be high [131].
Mathematical Formulation of Net Benefit
The Net Benefit statistic formalizes this trade-off. It is calculated from the confusion matrix of a model or test, applied at a specific threshold probability (p_t) [131] [132].
The fundamental formula for Net Benefit ((NB)) is:
[ NB = \frac{True\ Positives}{n} - \frac{False\ Positives}{n} \times \frac{pt}{1 - pt} ]
In this equation:
- (True\ Positives) and (False\ Positives) are the counts derived from classifying patients as positive based on the model when the predicted probability exceeds (p_t).
- (n) is the total number of patients in the cohort.
- The term (\frac{pt}{1 - pt}) is the exchange rate or odds of the threshold probability, which converts the harm of a false positive into the same units as the benefit of a true positive [131] [57].
This calculation can be equivalently expressed using sensitivity and specificity, or as a function of the true positive rate (TPR) and false positive rate (FPR) [132]:
[ NB = \rho \cdot TPR - (1 - \rho) \cdot FPR \cdot \frac{pt}{1 - pt} ]
where (\rho) is the outcome prevalence. Net Benefit is typically standardized against the strategy of "treat all" (which has a Net Benefit of (\rho) at (p_t = 0)) and compared to the strategies of "treat none" (Net Benefit = 0) and "treat all" [131].
Methodological Protocols and Experimental Implementation
Core Experimental Workflow for DCA
The following diagram illustrates the logical workflow for conducting and interpreting a Decision Curve Analysis.
Detailed Protocol: A Prostate Cancer Biopsy Case Study
This protocol uses a publicly available dataset concerning the prediction of cancer in patients with elevated PSA levels, where the intervention is a prostate biopsy [133] [134].
Background and Objective: A new biomarker is proposed to help decide which patients with elevated PSA should undergo a prostate biopsy. The goal is to determine if using this biomarker in a prediction model leads to better clinical decisions than biopsying all patients or no patients [131] [133].
Step-by-Step Methodology:
Data Preparation and Model Fitting:
- Import a dataset containing patient outcomes (
cancer: 0 or 1), a continuous marker (marker), and other predictors (e.g.,age,family history) [133]. - Fit a logistic regression model to predict the probability of cancer. For example:
cancer ~ age + marker + famhistory[134]. - Generate predicted probabilities for each patient in the validation dataset.
- Import a dataset containing patient outcomes (
Define the Range of Threshold Probabilities ((p_t)):
- Determine a clinically reasonable range for (p_t). For a serious condition like cancer where a biopsy is relatively burdensome, a range of 1% to 35% might be appropriate [133]. This means you will evaluate Net Benefit for thresholds from 0.01 to 0.35.
Calculate Net Benefit Across Thresholds:
- For each threshold (pt) in the defined range (e.g., 0.01, 0.02, ..., 0.35):
- Dichotomize predictions: Classify all patients with a predicted probability ≥ (pt) as "Test Positive" (recommend biopsy).
- Create a confusion matrix: Compare test positives to the actual
canceroutcome to count True Positives (TP) and False Positives (FP). - Compute Net Benefit: Use the formula ( NB = \frac{TP}{n} - \frac{FP}{n} \times \frac{pt}{1 - pt} ).
- Repeat this calculation for the "Treat All" strategy ((NB = \rho), where (\rho) is the prevalence of cancer) and the "Treat None" strategy ((NB = 0)) [131].
- For each threshold (pt) in the defined range (e.g., 0.01, 0.02, ..., 0.35):
Visualization with a Decision Curve:
- Create a plot with Threshold Probability ((p_t)) on the x-axis and Net Benefit on the y-axis.
- Plot the Net Benefit curves for:
- The new biomarker/model.
- The strategy "Biopsy All Patients."
- The strategy "Biopsy No Patients."
- The resulting graph allows for a direct visual comparison of the clinical value of each strategy across all relevant preferences [131].
Interpretation of the Decision Curve
The following diagram guides the interpretation of a Decision Curve plot.
- "Treat All" Benchmark: The "Treat All" line typically has a high Net Benefit for very low threshold probabilities (where the harm of a false positive is considered negligible) but its Net Benefit decreases as (p_t) increases [131].
- "Treat None" Benchmark: The "Treat None" line is always a horizontal line at Net Benefit = 0.
- Model/Test Superiority: The model has clinical value for the range of threshold probabilities where its Net Benefit curve is higher than both the "Treat All" and "Treat None" curves [131]. If the model's curve is not the highest across any reasonable range of thresholds, its clinical utility is questionable, even if its AUROC is high [135].
The Scientist's Toolkit: Essential Reagents and Software for DCA
Table 2: Key Research Reagent Solutions for Implementing DCA
| Tool / Reagent | Function / Description | Example / Application in Protocol |
|---|---|---|
| Validation Dataset | A cohort, independent from the model development data, with known outcomes for validation. PRoBE-design cohorts are the gold standard [132]. | A dataset of 750 patients with elevated PSA, biopsy results (cancer outcome), and measured biomarker levels [133]. |
| Statistical Software (R) | Provides the computational environment to calculate Net Benefit and plot decision curves. The dcurves package is specifically designed for this task [133]. |
dca(cancer ~ age + marker + famhistory, data = df_cancer_dx, thresholds = seq(0, 0.35, 0.01)) [133] |
| Statistical Software (Python) | Python's dcurves library offers similar functionality for calculating and visualizing DCA. |
dca.dca(data=df_cancer_dx, outcome="cancer", modelnames=["marker"], thresholds=np.arange(0, 0.36, 0.01)) [133] |
| Logistic Regression Model | A statistical model used to generate the predicted probabilities of the outcome based on predictor variables. | A model using age, marker, and famhistory to predict the probability of cancer [134]. |
| Harm-Benefit Ratio ((p_t)) | The pre-specified exchange rate that quantifies clinical preferences, defining the range of threshold probabilities to be tested. | For the prostate biopsy study, a threshold range of 1% to 35% is analyzed, reflecting that a patient might opt for biopsy if risk is as low as 1-in-100, or as high as 1-in-3 [131] [133]. |
Advanced Considerations and Future Directions
Statistical Inference and Confidence Intervals
Net Benefit is an estimated quantity and is subject to sampling variability. Presenting confidence intervals around the Net Benefit curve or for the difference in Net Benefit between two models is critical for robust inference [132]. Analytic distribution theory and bootstrap resampling methods can be employed to estimate standard errors and construct confidence intervals, helping researchers determine if an observed superiority in Net Benefit is statistically significant [132].
Extensions and Novel Applications
The framework of DCA is adaptable to various complex research scenarios:
- Time-to-Event Outcomes: DCA can be extended to evaluate models predicting survival outcomes, considering censored data [132] [133].
- Competing Risks: Methodologies exist to apply DCA in settings where an individual is at risk for multiple mutually exclusive outcomes [133].
- Objective Function for Machine Learning: A promising area of research involves using Net Benefit directly as the loss function to optimize during the development of machine learning algorithms, rather than traditional metrics like log-loss, potentially leading to models with higher inherent clinical utility [136].
Decision Curve Analysis and the Net Benefit metric provide a powerful, clinically oriented framework that moves beyond traditional performance metrics. By explicitly incorporating patient preferences and the consequences of clinical decisions, DCA allows researchers and drug developers to answer the pivotal question: "Will using this model actually improve patient care?" As the field of predictive analytics advances, integrating these decision-analytic measures into the standard model evaluation toolkit is not just recommended—it is essential for ensuring that statistical innovation translates into genuine clinical benefit.
Conclusion
Selecting and interpreting the right performance metrics is not a one-size-fits-all process but a critical, context-driven endeavor in drug development. A robust evaluation strategy must integrate metrics for discrimination, calibration, and overall performance, validated through rigorous frameworks like cross-validation and external testing. Future directions will be shaped by the need for Explainable AI (XAI) to meet regulatory standards, the use of multimodal AI for richer data integration, and advanced validation techniques to ensure models are not only statistically sound but also clinically actionable and ethically deployed, ultimately accelerating the translation of predictive models into improved patient outcomes.
References
- 1. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 2. Model EvaI future in 2025 - UBIAI [https://ubiai.tools/the-future-of-model-eval-achieving-superior-testing-and-evaluation-standards-in-ai/]
- 3. Model Evaluation Techniques [https://www.itonlinelearning.com/blog/model-evaluation-techniques/]
- 4. A critical review on selecting performance evaluation ... [https://www.sciencedirect.com/science/article/pii/S2213343725043714]
- 5. 3.4. Metrics and scoring: quantifying the quality of predictions [https://scikit-learn.org/stable/modules/model_evaluation.html]
- 6. Understanding the Confusion Matrix in Machine Learning [https://www.geeksforgeeks.org/machine-learning/confusion-matrix-machine-learning/]
- 7. Confusion matrix [https://en.wikipedia.org/wiki/Confusion_matrix]
- 8. A simple guide to building a confusion matrix [https://blogs.oracle.com/ai-and-datascience/a-simple-guide-to-building-a-confusion-matrix]
- 9. Confusion Matrix, Accuracy, Precision, Recall, F1 Score [https://medium.com/analytics-vidhya/confusion-matrix-accuracy-precision-recall-f1-score-ade299cf63cd]
- 10. Classification: Accuracy, recall, precision, and related metrics [https://developers.google.com/machine-learning/crash-course/classification/accuracy-precision-recall]
- 11. Confusion Matrix Made Simple: Accuracy, Precision, Recall ... [https://towardsdatascience.com/confusion-matrix-made-simple-accuracy-precision-recall-f1-score/]
- 12. Magician's Corner: 9. Performance Metrics for Machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8204137/]
- 13. Applying Machine Learning Techniques to Predict Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12166244/]
- 14. What is Accuracy vs. Precision vs. Recall in Machine ... [https://www.ultralytics.com/blog/accuracy-precision-recall]
- 15. Accuracy vs. precision vs. recall in machine learning [https://www.evidentlyai.com/classification-metrics/accuracy-precision-recall]
- 16. F-score [https://en.wikipedia.org/wiki/F-score]
- 17. Enhancing adverse drug reaction detection with deep ... [https://www.sciencedirect.com/science/article/pii/S221501612500305X]
- 18. AI-driven drug discovery using a context-aware hybrid ... [https://www.nature.com/articles/s41598-025-19593-4]
- 19. Classification: ROC and AUC | Machine Learning [https://developers.google.com/machine-learning/crash-course/classification/roc-and-auc]
- 20. Area under the ROC Curve has the most consistent evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11666033/]
- 21. Receiver operating characteristic curve: overview and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8831439/]
- 22. How to explain the ROC curve and ROC AUC score? [https://www.evidentlyai.com/classification-metrics/explain-roc-curve]
- 23. Guide to AUC ROC Curve in Machine Learning [https://www.analyticsvidhya.com/blog/2020/06/auc-roc-curve-machine-learning/]
- 24. AUC ROC Curve in Machine Learning [https://www.geeksforgeeks.org/machine-learning/auc-roc-curve/]
- 25. A guide to interpreting the area under the curve value - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10664195/]
- 26. Advantages of AUC vs standard accuracy [https://datascience.stackexchange.com/questions/806/advantages-of-auc-vs-standard-accuracy]
- 27. Comparison of AUC of independent ROC curves [https://www.medcalc.org/en/calc/comparison_of_independentROCtest.php]
- 28. Understanding Gain Chart and Lift Chart [https://www.geeksforgeeks.org/data-science/understanding-gain-chart-and-lift-chart/]
- 29. Cumulative Charts [https://docs.datarobot.com/en/docs/modeling/analyze-models/evaluate/roc-curve-tab/cumulative-charts.html]
- 30. Understand Gain and Lift Charts [https://www.listendata.com/2014/08/excel-template-gain-and-lift-charts.html]
- 31. Cumulative gains and lift charts [https://www2.cs.uregina.ca/~dbd/cs831/notes/lift_chart/lift_chart.html]
- 32. Gain chart and Lift chart for CART® Classification - Minitab [https://support.minitab.com/en-us/minitab/help-and-how-to/statistical-modeling/predictive-analytics/how-to/cart-classification/interpret-the-results/all-statistics-and-graphs/gain-chart-and-lift-chart/]
- 33. Interpreting results: Kolmogorov-Smirnov test [https://www.graphpad.com/guides/prism/latest/statistics/interpreting_results_kolmogorov-smirnov_test.htm]
- 34. 1.3.5.16. Kolmogorov-Smirnov Goodness-of-Fit Test [https://www.itl.nist.gov/div898/handbook/eda/section3/eda35g.htm]
- 35. Classification vs Regression [https://www.ibm.com/think/topics/classification-vs-regression]
- 36. Classification vs Regression in Machine Learning [https://www.geeksforgeeks.org/machine-learning/ml-classification-vs-regression/]
- 37. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 38. F1 Score vs ROC AUC vs Accuracy vs PR AUC [https://neptune.ai/blog/f1-score-accuracy-roc-auc-pr-auc]
- 39. A Comprehensive Overview of Regression Evaluation ... [https://developer.nvidia.com/blog/a-comprehensive-overview-of-regression-evaluation-metrics/]
- 40. Clinical prediction models using machine learning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506039/]
- 41. Machine learning-based diagnostic and prognostic models ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1581982/full]
- 42. Diagnostic Prediction Models for Primary Care, Based on AI ... [https://medinform.jmir.org/2025/1/e62862]
- 43. Evaluating the application of dynamic prediction models in ... [https://www.nature.com/articles/s41698-025-01162-7]
- 44. The validation of prediction models deserves more recognition [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-03994-3]
- 45. Implementation and Updating of Clinical Prediction Models [https://pubmed.ncbi.nlm.nih.gov/40599890/]
- 46. New Predictions for 2025 [https://globalforum.diaglobal.org/issue/january-2025/additional-predictions-for-2025/]
- 47. Clinical implementation of an AI-based prediction model for ... [https://www.nature.com/articles/s41591-025-03942-x]
- 48. On misconceptions about the Brier score in binary ... [https://arxiv.org/html/2504.04906v4]
- 49. The Brier score does not evaluate the clinical utility of ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6460786/]
- 50. How To Interpret R-squared in Regression Analysis [https://statisticsbyjim.com/regression/interpret-r-squared-regression/]
- 51. R-Squared: Coefficient of Determination in Machine Learning [https://arize.com/blog-course/r-squared-understanding-the-coefficient-of-determination/]
- 52. Brier Score - How to measure accuracy of probablistic ... [https://www.machinelearningplus.com/statistics/brier-score/]
- 53. Brier Score: Understanding Model Calibration [https://neptune.ai/blog/brier-score-and-model-calibration]
- 54. Weighted Brier Score - an Overall Summary Measure for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523994/]
- 55. R-Squared - Definition, Interpretation, Formula, How to ... [https://corporatefinanceinstitute.com/resources/data-science/r-squared/]
- 56. Understanding Model Calibration - A gentle introduction and ... [https://iclr-blogposts.github.io/2025/blog/calibration/]
- 57. Evaluating Prediction Model Performance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10529246/]
- 58. A-calibration: assessment of prediction models for survival ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542389/]
- 59. Predictive analytics in drug development: state of play [https://www.clinicaltrialsarena.com/features/predictive-analytics-drug-development/]
- 60. Net Reclassification Improvement (NRI) and IDI [https://www.uniqcret.com/post/nri-idi-explained]
- 61. - Wikipedia Net reclassification improvement [https://en.wikipedia.org/wiki/Net_reclassification_improvement]
- 62. Net Reclassification Index and Integrated Discrimination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5837334/]
- 63. Quantifying the added value of new biomarkers: how and how ... [https://diagnprognres.biomedcentral.com/articles/10.1186/s41512-018-0037-2]
- 64. : computation, interpretation, and... Net reclassification improvement [https://pubmed.ncbi.nlm.nih.gov/24592497/]
- 65. Thread by @cecilejanssens: "The Net ..." Reclassification Improvement [https://threadreaderapp.com/thread/1119256496343269376.html]
- 66. Integrated Discriminatory Improvement - File Exchange [https://www.mathworks.com/matlabcentral/fileexchange/43199-integrated-discriminatory-improvement]
- 67. How to use Learning Curves to Diagnose Machine ... [https://www.machinelearningmastery.com/learning-curves-for-diagnosing-machine-learning-model-performance/]
- 68. Twelve Tips for using Learning Curves in Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10696298/]
- 69. Overfitting and Underfitting with Learning Curves [https://articles.bnomial.com/overfitting-underfitting-learning-curves]
- 70. Diagnosing Model Performance with Learning Curves [https://rstudio-conf-2020.github.io/dl-keras-tf/notebooks/learning-curve-diagnostics.nb.html]
- 71. Learning Curve To Identify Overfit & Underfit [https://www.geeksforgeeks.org/machine-learning/learning-curve-to-identify-overfit-underfit/]
- 72. Learning Curve to identify Overfitting and Underfitting in ... [https://towardsdatascience.com/learning-curve-to-identify-overfitting-underfitting-problems-133177f38df5/]
- 73. Should You Use Imbalanced-Learn in 2025? [https://www.blog.trainindata.com/should-you-use-imbalanced-learn-in-2025/]
- 74. A review of machine learning methods for imbalanced data ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d5sc00270b]
- 75. An empirical evaluation of imbalanced data strategies from ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417424017305]
- 76. SMOTE-Enhanced Explainable Artificial Intelligence Model ... [https://pubmed.ncbi.nlm.nih.gov/40249240/?utm_source=Firefox&utm_medium=rss&utm_campaign=pubmed-2&utm_content=1Jqs22NP9NcXNGvhjq-M8ooQy2n0fSzdGx5hraL6umiDmNhcOx&fc=20240423222946&ff=20250424072147&v=2.18.0.post9+e462414]
- 77. Imbalanced class distribution and performance evaluation ... [https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000984]
- 78. A comprehensive evaluation of oversampling techniques ... [https://www.nature.com/articles/s41598-025-05791-7]
- 79. Hybrid oversampling technique for imbalanced pattern ... [https://www.sciencedirect.com/science/article/pii/S2666827025000209]
- 80. Counterfactual synthetic minority oversampling technique [https://www.sciencedirect.com/science/article/pii/S2666764925000062]
- 81. Hybrid Synthetic Minority Over-sampling Technique ... [https://www.nature.com/articles/s41598-025-23062-3]
- 82. Undersampling method based on minority class density for ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417424001933]
- 83. What Is Hyperparameter Tuning? [https://www.ibm.com/think/topics/hyperparameter-tuning]
- 84. Hyperparameter Optimization With Random Search and ... [https://www.machinelearningmastery.com/hyperparameter-optimization-with-random-search-and-grid-search/]
- 85. Hyperparameter Tuning [https://www.geeksforgeeks.org/machine-learning/hyperparameter-tuning/]
- 86. A Conceptual Explanation of Bayesian Hyperparameter ... [https://medium.com/data-science/a-conceptual-explanation-of-bayesian-model-based-hyperparameter-optimization-for-machine-learning-b8172278050f]
- 87. Using Grid Search For Hyper-Parameter Tuning [https://medium.com/@hammad.ai/using-grid-search-for-hyper-parameter-tuning-bad6756324cc]
- 88. Tuning Model Hyperparameters With Random Search [https://medium.com/@hammad.ai/tuning-model-hyperparameters-with-random-search-f4c1cc88f528]
- 89. Hyperparameter Tuning: Grid, Random, Bayesian [https://medium.com/@pacosun/the-tuners-toolbox-grid-search-random-search-and-bayesian-optimization-unpacked-648abd7a8ff6]
- 90. Hyperparameter tuning. Grid search and random search [https://www.yourdatateacher.com/2021/05/19/hyperparameter-tuning-grid-search-and-random-search/]
- 91. 3.2. Tuning the hyper-parameters of an estimator [https://scikit-learn.org/stable/modules/grid_search.html]
- 92. Hyperparameter Optimization Based on Bayesian ... [https://www.geeksforgeeks.org/machine-learning/hyperparameter-optimization-based-on-bayesian-optimization/]
- 93. Data Preprocessing in Machine Learning: Steps & Best ... [https://lakefs.io/blog/data-preprocessing-in-machine-learning/]
- 94. Data Preprocessing and Feature Engineering for Data Mining [https://www.mdpi.com/2673-2688/6/10/257]
- 95. A Beginner's Guide for Feature Engineering in Machine ... [https://www.tredence.com/blog/feature-engineering-in-machine-learning]
- 96. Data preprocessing: a comprehensive step-by-step guide [https://www.future-processing.com/blog/data-preprocessing-a-comprehensive-step-by-step-guide/]
- 97. AutoML Revolutionizing Business Processes: What... - Bi Technology [https://www.bitechnology.com/automl-revolutionizing-business-processes-what-you-need-to-know-in-2025/]
- 98. The Future of Automated Machine Learning (AutoML) [https://businessanalyticsinstitute.com/the-future-of-automated-machine-learning-automl/]
- 99. Leveraging Explainable Automated Machine Learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609673/]
- 100. A human-centered automated machine learning agent with ... [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2025.1680845/full]
- 101. Performance Evaluation of Manual and AutoML Algorithms [https://thesai.org/Publications/ViewPaper?Volume=16&Issue=1&Code=IJACSA&SerialNo=2]
- 102. Evaluation of large language model-driven AutoML in data ... [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2025.1590105/full]
- 103. AI Model for Enhanced Performance in Optimization Techniques 2025 [https://www.netguru.com/blog/ai-model-optimization]
- 104. AI Optimization in 2025 : Smarter Techniques and Tools [https://www.rolustech.com/blog/ai-optimization-2025]
- 105. Key strategies for MLops success in | InfoWorld [https://www.infoworld.com/article/3821146/key-strategies-for-mlops-success-in-2025.html]
- 106. A Gentle Introduction to k-fold Cross-Validation [https://www.machinelearningmastery.com/k-fold-cross-validation/]
- 107. Cross-validation (statistics) [https://en.wikipedia.org/wiki/Cross-validation_(statistics)]
- 108. Rapid and Robust Resampling-Based Multiple-Testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3316660/]
- 109. Best (but oft-forgotten) practices: the multiple problems of ... [https://www.sciencedirect.com/science/article/pii/S0002916523136963]
- 110. How to choose a predictive model after k-fold cross-validation? [https://stats.stackexchange.com/questions/52274/how-to-choose-a-predictive-model-after-k-fold-cross-validation]
- 111. K- Fold Cross Validation in Machine Learning [https://www.geeksforgeeks.org/machine-learning/k-fold-cross-validation-in-machine-learning/]
- 112. Show and tell: A critical review on robustness ... [https://www.sciencedirect.com/science/article/pii/S138650562500187X]
- 113. Systematic scoping review of external validation studies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12145442/]
- 114. Behavior of prediction performance metrics with rare events [https://pubmed.ncbi.nlm.nih.gov/41224138/]
- 115. Developing a New Reference Standard… Is Validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2919497/]
- 116. Understanding Evaluation Metrics for Predictive Analytics [https://blog.tobiaszwingmann.com/p/evaluation-metrics-predictive-analytics]
- 117. A comprehensive benchmark of machine and deep ... [https://www.sciencedirect.com/science/article/pii/S0925231225020090]
- 118. Neural Network Metrics [https://www.meegle.com/en_us/topics/neural-networks/neural-network-metrics]
- 119. Random Forest Algorithm in Machine Learning [https://www.geeksforgeeks.org/machine-learning/random-forest-algorithm-in-machine-learning/]
- 120. XGBoost Parameters — xgboost 3.1.1 documentation [https://xgboost.readthedocs.io/en/stable/parameter.html]
- 121. Evaluating a Random Forest model [https://medium.com/analytics-vidhya/evaluating-a-random-forest-model-9d165595ad56]
- 122. Regression Metrics [https://www.geeksforgeeks.org/machine-learning/regression-metrics/]
- 123. Custom Objective and Evaluation Metric — xgboost 3.2.0-dev ... [https://xgboost.readthedocs.io/en/latest/tutorials/custom_metric_obj.html]
- 124. Statistical variability in comparing accuracy of ... [https://www.nature.com/articles/s41598-025-12026-2]
- 125. Comparing multi-class classifier performance by multi-class ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11031188/]
- 126. Multiple comparisons problem [https://en.wikipedia.org/wiki/Multiple_comparisons_problem]
- 127. A general introduction to adjustment for multiple comparisons [https://pmc.ncbi.nlm.nih.gov/articles/PMC5506159/]
- 128. Correction For Multiple Comparisons [https://www.statsig.com/glossary/correction-for-multiple-comparisons]
- 129. MARS: Unleashing the Power of Variance Reduction for ... [https://arxiv.org/html/2411.10438v4]
- 130. Assessing the performance of prediction models: a framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3575184/]
- 131. A simple, step-by-step guide to interpreting decision curve ... [https://diagnprognres.biomedcentral.com/articles/10.1186/s41512-019-0064-7]
- 132. Statistical Inference for Net Benefit Measures in Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7228830/]
- 133. DCA: Software Tutorial [https://mskcc-epi-bio.github.io/decisioncurveanalysis/dca-tutorial.html]
- 134. Decision curve analysis or why interpretation of medical ... [https://it-innovations-healthcare.medium.com/decision-curve-analysis-or-why-interpretation-of-medical-decision-support-models-should-be-based-on-b553acedb998]
- 135. Decision Curve Analysis Explained [https://www.medrxiv.org/content/10.1101/2025.08.16.25333820v1]
- 136. Net benefit as an objective function during development of ... [https://www.sciencedirect.com/science/article/abs/pii/S1386505625000619]