Beyond Statistical Significance: A Practical Guide to Equivalence Testing for Model Performance in Biomedical Research
This article provides a comprehensive guide to equivalence testing for researchers, scientists, and drug development professionals.
Beyond Statistical Significance: A Practical Guide to Equivalence Testing for Model Performance in Biomedical Research
Abstract
This article provides a comprehensive guide to equivalence testing for researchers, scientists, and drug development professionals. Moving beyond traditional null hypothesis significance testing, we explore the foundational concepts of proving similarity rather than difference. The content covers core methodological approaches like the Two One-Sided Tests (TOST) procedure and Bayesian methods, alongside practical implementation strategies for comparing machine learning classifiers and regression models. We address common pitfalls in model selection, the impact of model misspecification, and optimization techniques such as model averaging. The guide also delves into validation frameworks and comparative analyses of frequentist versus Bayesian paradigms, equipping practitioners with the statistical tools to robustly demonstrate model equivalence in clinical and biomedical applications.
Why Prove Sameness? The Critical Shift from Difference to Equivalence in Biomedical Models
In scientific research, particularly in fields like drug development and machine learning, a common and critical error is to interpret a non-significant result from a null hypothesis significance test (NHST) as evidence for the absence of an effect or difference. This misinterpretation stems from a fundamental logical flaw in the structure of traditional hypothesis testing. A failure to reject a null hypothesis (e.g., obtaining a p-value > 0.05) merely indicates that the data do not provide strong enough evidence to conclude a difference exists; it does not affirm that the two groups are equivalent [1] [2]. This distinction is paramount when the research goal is to positively demonstrate similarity, such as proving a new generic drug delivers the same physiological effect as its brand-name counterpart, or that a simplified machine learning model performs as well as a more complex one.
The persistence of this fallacy is a significant contributor to the ongoing replication crisis in many scientific fields, as it leads to underpowered studies and unsubstantiated claims of "no difference" [3]. This article will delineate the limitations of traditional NHST for equivalence testing, introduce robust statistical methodologies designed specifically for proving equivalence, and provide practical guidance for researchers and drug development professionals on their correct application.
How Traditional Null Hypothesis Significance Testing Fails Equivalence
The Logical Structure and Its Shortcomings
Traditional NHST is designed to test for the presence of a difference. Its structure is ill-suited for testing equivalence.
Standard NHST (Difference Testing): The null hypothesis (H₀) states that there is no difference between groups (the "nil" null hypothesis). A statistically significant p-value allows researchers to reject H₀ and conclude that a difference exists [1]. However, a non-significant p-value (p > α) only leads to a failure to reject H₀. This is an inconclusive result; it does not allow the researcher to accept H₀ and claim the groups are identical [2]. As one analysis notes, "a ‘not guilty’ verdict ... does not necessarily imply that the jury believes the accused is innocent. Rather, it means that the evidence presented was insufficient to conclude the accused is guilty beyond a reasonable doubt" [1].
The Goal of Equivalence Testing: Here, the researcher wants to positively confirm the absence of a meaningful difference. This requires an inversion of the usual hypotheses. In equivalence testing, the null hypothesis becomes that a meaningful difference does exist, and the goal is to reject this hypothesis in favor of the alternative, which states that the difference is smaller than a pre-defined, clinically or practically important threshold [1] [2] [4].
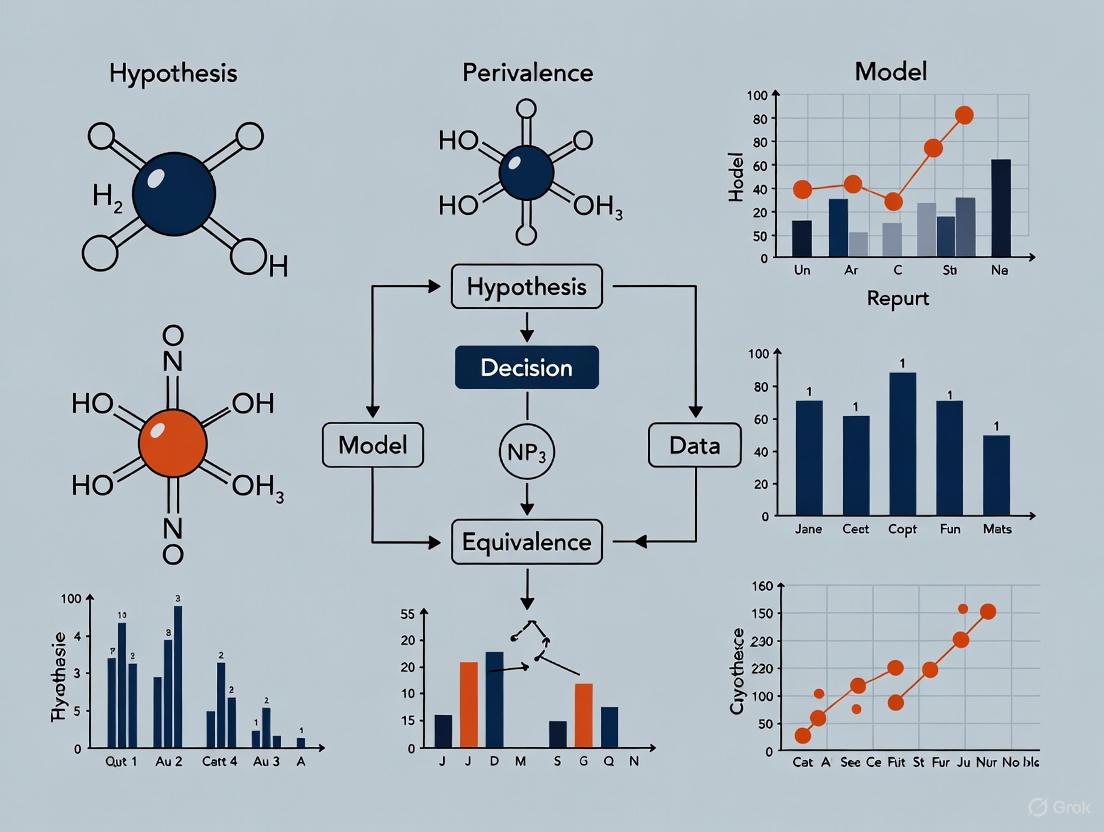
The confusion arising from traditional NHST is visually and logically summarized in the diagram below.
The Perils of Misinterpretation in Practice
Relying on a non-significant NHST result to claim equivalence is fraught with risk. The most common danger is an underpowered study [3]. A small sample size or highly variable data can easily lead to a large p-value, even if a substantial, clinically important difference truly exists. Concluding equivalence based on this result could lead to grave consequences, such as approving a less effective drug or deploying an inferior analytical model.
Furthermore, in correlational fields like the social sciences, an effect of zero is often improbable due to numerous latent variables (the "crud factor") [2]. Therefore, rejecting a nil null hypothesis is not a rigorous test, as it is likely to succeed even for theoretically uninteresting associations. This undermines the validity of claims built on this foundation.
A Robust Alternative: Equivalence Testing and the TOST Procedure
The Core Framework of Equivalence Testing
Equivalence testing directly addresses the logical flaw of NHST by inverting the null and alternative hypotheses. The core of this framework is the definition of an equivalence interval (EI), also known as the region of practical equivalence (ROPE) [1] [2]. The EI is a range of values, centered on zero, that represents differences deemed too small to be of any practical or clinical importance. Establishing this interval a priori is a critical step that requires domain-specific knowledge [2].
The formal hypotheses for a two-sided equivalence test are [1]:
- Null Hypothesis (H₀): The true difference between the groups is outside the equivalence interval (i.e., Δ ≤ -EI or Δ ≥ EI).
- Alternative Hypothesis (H₁): The true difference between the groups is inside the equivalence interval (i.e., -EI < Δ < EI).
The goal of the statistical test is to reject H₀, thereby providing statistical evidence that the difference is negligibly small and the groups are practically equivalent.
The Two One-Sided Tests (TOST) Methodology
The most common and straightforward method for conducting an equivalence test is the Two One-Sided Tests (TOST) procedure [2] [4]. Instead of one test, it employs two simultaneous one-sided tests to rule out effects at both ends of the equivalence interval.
The procedure tests two sets of hypotheses:
- Test 1: H₀₁: Δ ≤ -EI vs. H₁₁: Δ > -EI
- Test 2: H₀₂: Δ ≥ EI vs. H₁₂: Δ < EI
Equivalence is concluded at a significance level α only if both null hypotheses are rejected [1]. This is equivalent to showing that the entire (1 - 2α)% confidence interval for the difference lies completely within the equivalence interval [-EI, EI] [4]. The workflow and decision logic of TOST is illustrated below.
Practical Application: A Case Study in Drug Development
Scenario: Establishing Bioequivalence
A canonical application of equivalence testing is in pharmacokinetics for establishing bioequivalence between a generic and a brand-name drug [4]. Regulatory agencies like the FDA require evidence that the generic product has equivalent absorption to the brand-name product, typically measured by parameters like AUC (area under the curve) and Cmax (maximum concentration) [4].
Suppose a study aims to prove that a new synthetic fiber has equivalent breaking strength to a natural fiber. The researchers define, based on engineering requirements, that a mean difference in strength within ±20 kg is practically irrelevant. The equivalence interval is thus set at [-20, 20] [1].
Experimental Protocol:
- Design: A randomized, controlled study is conducted.
- Data Collection: 15 samples of natural fiber and 12 samples of synthetic fiber are tested for breaking strength.
- Descriptive Statistics:
- Natural fiber: Mean = 530 kg, StDev = 40 kg
- Synthetic fiber: Mean = 513 kg, StDev = 20 kg
- Observed difference: 17 kg
- Analysis: A two-sample equivalence test (TOST procedure) is performed with an equivalence interval of ±20 kg and α = 0.05.
Results and Interpretation: The test yields two p-values: one for testing against the lower bound (p = 0.007) and one for testing against the upper bound (p = 0.253) [1]. Because only one of the two tests is statistically significant (p < 0.05), the null hypothesis of non-equivalence cannot be rejected. The 95% confidence interval for the difference (-8.36, 32.36) extends beyond the upper equivalence limit, visually confirming this conclusion [1]. In this case, the researchers correctly determine that equivalence has not been demonstrated, despite the observed difference of 17 kg being within the ±20 kg window, due to the uncertainty (confidence interval) around the estimate.
Essential Research Reagent Solutions for Equivalence Studies
Table 1: Key Reagents and Tools for Equivalence Testing in Experimental Research
| Reagent/Tool | Function in Research | Application Context |
|---|---|---|
| Statistical Software (R, Python) | Executes TOST procedures, calculates confidence intervals, and generates plots. | Essential for all quantitative fields (e.g., pharmacology, data science) for data analysis. |
| Equivalence Interval (EI) | Defines the margin of practically insignificant difference; the critical benchmark for the test. | Required for any equivalence study design (e.g., setting Δ for bioequivalence in drug studies). |
| Power Analysis Software | Determines the minimum sample size required to detect equivalence with high probability. | Used in the design phase of experiments (clinical trials, model validation) to avoid underpowered studies. |
| Selenium WebDriver | Automates web browser interaction for consistent, repeated performance measurement. | Used in data science for A/B testing webpage load times or UI interactions [5]. |
| MLxtend Library | Provides implementations of specialized statistical tests for comparing machine learning models. | Used in data science for pairedttest5x2cv to compare algorithm performance robustly [6]. |
Comparing Statistical Approaches: NHST vs. Equivalence Testing
The following table provides a consolidated comparison of the two methodologies, highlighting their distinct goals, interpretations, and risks.
Table 2: A Comparative Overview of NHST and Equivalence Testing
| Feature | Traditional NHST (for Difference) | Equivalence Testing (TOST) |
|---|---|---|
| Primary Goal | Detect the presence of a difference. | Confirm the absence of a meaningful difference. |
| Null Hypothesis (H₀) | No difference exists (Effect = 0). | A meaningful difference exists (Effect ≤ -EI or Effect ≥ EI). |
| Interpretation of a Significant Result (p < α) | Reject H₀; conclude a difference exists. | Reject H₀; conclude equivalence (difference is within [-EI, EI]). |
| Interpretation of a Non-Significant Result (p ≥ α) | Fail to reject H₀; cannot conclude a difference exists. (Inconclusive) | Fail to reject H₀; cannot conclude equivalence. (Inconclusive) |
| Key Risk | Mistaking "no significant difference" for "evidence of no difference" (Type II error). | Failing to claim equivalence when it is true (often due to low power). |
| Confidence Interval Interpretation | If the 95% CI includes 0, the result is not statistically significant. | If the 90% CI* falls entirely within [-EI, EI], equivalence is concluded. |
| Common Application | Exploratory research: Discovering if an effect is present. | Validation research: Proving two treatments/products are similar. |
Note: A 90% confidence interval is used in TOST to correspond to a two-test procedure each at α=0.05, maintaining an overall Type I error rate of 5%.
Advanced Considerations and Future Directions
Bayesian Alternatives and Multivariate Extensions
While the frequentist TOST procedure is the most established method, modern alternatives offer additional flexibility. The Bayesian Region of Practical Equivalence (ROPE) allows researchers to make direct probability statements about the parameter lying within the equivalence interval, which can be more intuitive than the dichotomous reject/fail-to-reject decision of NHST [7].
Furthermore, many real-world problems, such as demonstrating bioequivalence for multiple pharmacokinetic parameters (AUC, Cmax, tmax) simultaneously, require multivariate equivalence testing [4]. Standard TOST procedures can become overly conservative when applied to multiple correlated outcomes. Recent methodological research focuses on developing adjusted TOST procedures (e.g., the multivariate α*-TOST) that account for the dependence between outcomes to improve statistical power while maintaining the prescribed Type I error rate [4].
The Critical Role of Power and Sample Size
A fundamental tenet of any statistical analysis, especially equivalence testing, is ensuring the study has adequate power. Power is the probability of correctly rejecting the null hypothesis when it is false. In equivalence testing, this translates to the likelihood of successfully demonstrating equivalence when the groups are truly equivalent [1]. An underpowered equivalence study is highly likely to fail to demonstrate equivalence, even if it truly exists, wasting resources and potentially leading to the abandonment of promising treatments or technologies. Therefore, a power analysis conducted during the study design phase to determine the necessary sample size is not just good practice—it is essential for a meaningful and reliable conclusion.
In the rigorous fields of preclinical research and drug development, the traditional statistical question of "Is there an effect?" is being superseded by the more nuanced and practical inquiry: "Is the effect large enough to matter?" This paradigm shift moves research beyond mere statistical significance toward assessing practical relevance, a critical consideration when deciding which drug candidates warrant progression to costly clinical trials. Two methodological frameworks have emerged to address this question: the Region of Practical Equivalence (ROPE), a Bayesian approach, and the Smallest Effect Size of Interest (SESOI), often utilized within frequentist equivalence testing. Both concepts share a common goal—to define a range of effect sizes that are considered practically or clinically irrelevant—but they operationalize this goal through different statistical philosophies and decision rules. This guide provides an objective comparison of these methodologies, detailing their protocols, applications, and performance in the context of hypothesis testing model performance equivalence research.
Conceptual Frameworks and Definitions
Region of Practical Equivalence (ROPE)
The ROPE is a Bayesian statistical concept that defines an interval around a null value, typically zero, where parameter values are considered practically equivalent to the null. Unlike significance testing which examines differences from a point null, the ROPE framework acknowledges that trivially small effects, even if technically non-zero, are scientifically meaningless [8].
- Core Principle: The fundamental question in ROPE analysis is whether the entire credible interval of a parameter's posterior distribution lies outside the ROPE (indicating a meaningful effect), inside the ROPE (indicating practical equivalence to the null), or overlaps the ROPE (indicating uncertainty) [8].
- Decision Rule: The standard "HDI+ROPE decision rule" assesses the percentage of the Highest Density Interval (HDI)—a Bayesian credible interval—that falls within the ROPE. A common practice is to use the 89% or 95% HDI for this assessment [8].
Smallest Effect Size of Interest (SESOI)
The SESOI, also known as the Minimum Effect of Interest (MEI) or Minimum Clinically Important Difference (MCID), is the smallest true effect size that a researcher deems theoretically meaningful or clinically valuable in the context of their research [9] [10] [11].
- Core Principle: The SESOI is established prior to data collection and is used to design studies with sufficient statistical power to detect this specific effect. It reframes the alternative hypothesis ((H_1)) from a vague "effect exists" to a specific "effect is at least as large as the SESOI" [10].
- Anchor-Based Methods: One established approach for determining the SESOI, particularly in clinical and health research, uses an "anchor," often a global rating of change question. This method quantifies the smallest change in an outcome measure that individuals consider meaningful enough in their subjective experience to rate themselves as "feeling different" [9].
Methodological Comparison and Experimental Protocols
The following table summarizes the key characteristics of ROPE and SESOI, highlighting their philosophical and procedural differences.
Table 1: Core Characteristics of ROPE and SESOI
| Feature | Region of Practical Equivalence (ROPE) | Smallest Effect Size of Interest (SESOI) |
|---|---|---|
| Statistical Paradigm | Bayesian Estimation [8] | Frequentist Equivalence Testing (e.g., TOST) [12] |
| Primary Question | Is the most credible parameter range practically equivalent to the null? [8] | Can we reject effect sizes as large or larger than the SESOI? [9] |
| Key Input | A pre-defined equivalence region around the null value. | A single pre-defined minimum interesting effect size. |
| Core Output/Decision Metric | Percentage of the posterior distribution or Highest Density Interval (HDI) within the ROPE [8]. | p-values from two one-sided tests (TOST) against the SESOI bounds [12]. |
| Interval Used | 89% or 95% Highest Density Interval (HDI) [8]. | 90% Confidence Interval (CI) for a 5% alpha level [12]. |
| Interpretation of Result | Accept Null: Full HDI inside ROPE.Reject Null: Full HDI outside ROPE.Uncertain: HDI overlaps ROPE [8]. | Equivalent: 90% CI falls entirely within [-SESOI, +SESOI].Not Equivalent: CI includes values outside the bounds. |
Detailed Experimental Protocol for ROPE
The ROPE procedure is implemented within a Bayesian estimation framework, typically involving the following workflow.
Step-by-Step Protocol:
- Define the ROPE Range: The most critical step is to specify the upper and lower bounds of the ROPE based on domain knowledge. For a standardized mean difference (e.g., Cohen's d), a default range of -0.1 to 0.1 is sometimes used, representing a negligible effect size according to Cohen's conventions [8]. In preclinical drug development, this range should be grounded in the Minimum Clinically Important Difference (MCID), representing the smallest treatment benefit that would justify the costs and risks of a new therapy [11].
- Specify the Prior Distribution: Elicit a prior distribution that represents plausible parameter values before seeing the data. In the absence of strong prior information, a broad or weakly informative prior (e.g., a Cauchy or normal distribution with a large variance) can be used [8].
- Compute the Posterior Distribution: Using computational methods (e.g., Markov Chain Monte Carlo sampling in software like
Stan,JAGS, or thebayestestRpackage in R), compute the posterior distribution of the parameter of interest (e.g., a mean difference or regression coefficient). This distribution combines the prior with the likelihood of the observed data [8]. - Calculate the Highest Density Interval (HDI): From the posterior distribution, compute the 89% or 95% HDI. This is the interval that spans the most credible values of the parameter and has the property that all points inside the interval have a higher probability density than points outside it [8].
- Apply the HDI+ROPE Decision Rule:
- If the entire HDI falls within the ROPE, conclude that the parameter is practically equivalent to the null and "accept" the null for practical purposes.
- If the entire HDI falls outside the ROPE, reject the null value and conclude a practically significant effect.
- If the HDI overlaps the ROPE, the data are deemed inconclusive, and no firm decision can be made [8].
Detailed Experimental Protocol for SESOI via Equivalence Testing
The SESOI is typically deployed using frequentist equivalence testing, most commonly the Two One-Sided Tests (TOST) procedure. The workflow is as follows.
Step-by-Step Protocol:
- Define the SESOI (Δ): Before data collection, rigorously define the smallest effect size that would be considered practically or clinically important. In research involving subjective experience, anchor-based methods can be used. This involves correlating changes in the primary outcome with an external "anchor," such as a patient's global rating of change, to identify the threshold for a subjectively experienced difference [9].
- Formulate Hypotheses: The TOST procedure reformulates the null and alternative hypotheses.
- Null Hypothesis (H₀): The true effect is outside the equivalence interval (i.e., Effect ≤ -Δ or Effect ≥ Δ).
- Alternative Hypothesis (H₁): The true effect is within the equivalence interval (i.e., -Δ < Effect < Δ) [12].
- Perform Two One-Sided Tests: Conduct two separate statistical tests.
- Test 1: Check if the effect is significantly greater than the lower bound (-Δ).
- Test 2: Check if the effect is significantly less than the upper bound (+Δ).
- Each test is performed at a significance level of α (e.g., 0.05) [12].
- Construct a Confidence Interval: As a more intuitive equivalent to TOST, compute a 90% Confidence Interval for the effect size. Using a 90% CI (rather than 95%) corresponds to the two tests each being run at α = 0.05, controlling the overall Type I error rate at 5% [12].
- Decision Rule:
- If the entire 90% CI lies within the interval [-Δ, +Δ], you reject the null hypothesis and conclude equivalence (i.e., the effect is practically insignificant).
- If the 90% CI extends outside the [-Δ, +Δ] interval, you fail to conclude equivalence [12].
Performance and Application in Preclinical Research
A key application of these methods is in improving the reliability of preclinical animal research, which serves as a funnel for clinical trials. Simulation studies have compared research pipelines based on traditional Null Hypothesis Significance Testing (NHST), SESOI-based equivalence testing, and Bayesian decision criteria like ROPE [11].
Table 2: Simulated Performance in a Preclinical Research Pipeline (Exploratory + Confirmatory Study)
| Research Pipeline | False Discovery Rate (FDR) | False Omission Rate (FOR) | Key Assumptions & Notes |
|---|---|---|---|
| Traditional NHST | Higher (Baseline) | Lower | Uses two-sample t-test at α=0.025. Prone to declaring trivial effects as "significant." [11] |
| SESOI (Equivalence Test) | Reduced | Comparable | Uses TOST procedure. Explicitly incorporates MCID, filtering out trivial effects and reducing false positives. [11] |
| ROPE (Bayesian) | Reduced | Comparable | Uses 95% HDI and ROPE based on MCID. Provides similar FDR reduction as SESOI/TOST while allowing for incorporation of prior knowledge. [11] |
Supporting Experimental Data from Simulation Studies:
- A 2023 simulation study modeling preclinical research (exploratory animal study followed by a confirmatory study) found that pipelines incorporating the SESOI or ROPE substantially reduced the False Discovery Rate (FDR) compared to a pipeline based solely on traditional NHST (p-values) [11].
- This FDR reduction was achieved without a substantial increase in the False Omission Rate (FOR), meaning truly effective treatments were not incorrectly filtered out at a higher rate [11].
- The study concluded that both Bayesian statistical decision criteria (like ROPE) and methods that explicitly incorporate the SESOI can improve the reliability of preclinical animal research by reducing the number of false-positive findings that transition to costly confirmatory studies [11].
The Scientist's Toolkit: Essential Reagents and Materials
The successful implementation of these statistical methods relies on both conceptual understanding and the use of robust software tools.
Table 3: Key Research Reagent Solutions for Equivalence Testing
| Tool / Reagent | Function | Implementation Example |
|---|---|---|
| Bayesian Analysis Package | Performs Bayesian estimation, computes posterior distributions, HDIs, and ROPE percentages. | bayestestR R package [8] |
| Equivalence Testing Package | Conducts TOST procedures for various statistical tests (t-tests, correlations, meta-analyses). | TOSTER R package (or equivalent in Python, SAS) [12] |
| Power Analysis Software | Calculates required sample size to achieve sufficient statistical power for a given SESOI/ROPE. | BEST R package for Bayesian power analysis; pwr or TOSTER for frequentist power analysis [12] |
| Meta-Analysis Tool | Synthesizes effect sizes across multiple studies to establish evidence-based SESOI/ROPE ranges. | metafor R package; RevMan (Cochrane) |
| Anchor-Based Analysis Scripts | Custom scripts to analyze the relationship between an anchor variable (e.g., patient global rating) and the primary outcome to define the SESOI. | Custom R/Python/SAS scripts implementing methods from Anvari et al. [9] |
Critical Considerations for Implementation
- Sensitivity to Scale: The correct interpretation of the ROPE is highly dependent on the scale of the parameters. A change in the unit of measurement (e.g., from days to years in a growth model) can drastically alter the proportion of the posterior distribution inside the ROPE, leading to different conclusions. It is crucial to define the ROPE in a contextually meaningful way for your specific data [8].
- Impact of Multicollinearity: In models with multiple correlated parameters (multicollinearity), the joint posterior distributions can be misleading. The ROPE procedure applied to univariate marginal distributions may be invalid under strong correlations, as the probabilities are conditional on independence. In such cases, checking for pairwise correlations and investigating more sophisticated methods like projection predictive variable selection is advised [8].
- Power and Sample Size: For both SESOI and ROPE, a priori sample size justification is critical. Power analysis for TOST is based on closed-form functions and is computationally fast. Power analysis for ROPE can be performed via simulation (e.g., using the
BESTpackage), which is more computationally intensive but allows for the incorporation of prior distributions [12]. - Choice of Interval: The ROPE procedure commonly uses a 95% HDI for decision-making, while the TOST procedure uses a 90% CI. This makes the frequentist equivalence test more powerful by default, as it uses a narrower interval. However, one could also choose to use a 90% HDI for the ROPE decision rule to make the procedures more comparable [12].
In the rigorous world of pharmaceutical development, demonstrating equivalence—rather than superiority—is a fundamental requirement across multiple critical domains. Equivalence testing provides a structured statistical framework for proving that a new product, method, or model performs comparably to an established standard. For researchers and drug development professionals, this methodology is indispensable in three key applications: approving generic drugs through bioequivalence studies, validating novel clinical trial models and sites, and establishing analytical method equivalence for quality control.
This guide objectively compares the performance of established regulatory pathways, emerging in-silico techniques, and advanced statistical tools used in equivalence research. The comparative analysis is framed within the broader thesis of hypothesis testing model performance, examining how varied methodological approaches meet the stringent evidence requirements of regulatory science. The following sections provide a detailed comparison of experimental protocols, quantitative performance data, and the essential toolkit for implementing these approaches in practice.
Comparative Performance Analysis of Equivalence Applications
The table below summarizes the core performance metrics, regulatory contexts, and primary statistical outputs for the three major applications of equivalence testing in drug development.
Table 1: Performance and Application Comparison of Equivalence Testing Frameworks
| Application Area | Primary Objective | Key Performance Metrics & Statistical Outputs | Regulatory/Standardization Framework | Typical Experimental Context |
|---|---|---|---|---|
| Generic Drug Bioequivalence | Demonstrate therapeutic equivalence to a Reference Listed Drug (RLD) [13] [14]. | • 90% Confidence Intervals for PK parameters (AUC, C~max~) within 80.00%-125.00% [13].• P-value for statistical testing [15]. | Hatch-Waxman Act, FDA ANDA pathway [13] [14]. | Clinical study in healthy volunteers or patients. |
| Clinical Trial Model & Site Validation | Ensure operational quality and reliability of trial sites and in-silico models [16] [17]. | • Factor correlations (e.g., from Confirmatory Factor Analysis) [18].• R² statistics from regression models [18].• Site Performance Scores (e.g., CT-SPM domains) [16]. | ICH guidelines, V3+ framework for digital measures [18]. | Multicenter study for site metrics; computational validation for in-silico models [16] [17]. |
| Analytical Method Equivalence | Prove that a new or modified analytical procedure yields equivalent results to an established method [19]. | • Mean, Standard Deviation, Pooled Standard Deviation [19].• Equivalence intervals based on pre-defined acceptance criteria [19]. | ICH Q2(R2), ICH Q14, USP <1010> [19]. | Laboratory study comparing method outputs for the same samples. |
Experimental Protocols for Key Equivalence Methodologies
Protocol for Establishing Bioequivalence
The gold-standard protocol for establishing bioequivalence for a generic oral drug is a single-dose, two-treatment, two-period, two-sequence crossover study in healthy human subjects [13].
- Subject Selection & Randomization: A cohort of healthy volunteers is recruited and randomly assigned to one of two sequence groups. The sample size is justified by a power calculation to ensure high probability (often 80-90%) of demonstrating equivalence if it exists.
- Dosing and Blood Collection: In the first period, one group receives the generic Test product (T), and the other receives the Reference Listed Drug (R). After a washout period (typically >5 half-lives of the drug) sufficient to eliminate the first dose, the groups switch treatments in the second period.
- Bioanalysis: Serial blood samples are collected from each subject over a time period adequate to define the concentration-time profile. Plasma concentrations of the active pharmaceutical ingredient are determined using a validated analytical method (e.g., LC-MS/MS).
- Pharmacokinetic (PK) Analysis: The concentration-time data for each subject are used to calculate key PK parameters, including:
- AUC~0-t~: Area under the concentration-time curve from zero to the last measurable time point, representing total exposure.
- AUC~0-∞~: Area under the curve from zero to infinity.
- C~max~: The maximum observed concentration.
- Statistical Analysis for Equivalence: An Analysis of Variance (ANOVA) is performed on the log-transformed AUC and C~max~ data. The critical step is the calculation of the 90% confidence intervals (CI) for the geometric mean ratio (T/R) of these parameters. Bioequivalence is concluded if the 90% CIs for both AUC and C~max~ fall entirely within the acceptance range of 80.00% to 125.00% [13].
Protocol for Validating a Virtual Cohort for an In-Silico Trial
The validation of a computationally generated virtual cohort against a real-world patient cohort involves assessing how well the virtual population reflects the real one across key characteristics [17].
- Cohort Definition and Generation: Define the target patient population for the in-silico trial (e.g., patients with moderate aortic stenosis). A virtual cohort is then generated using computational models, often based on real clinical data, to simulate individuals with the same distribution of clinical parameters (e.g., age, anatomy, disease severity).
- Real-World Dataset Selection: Identify a suitable real-world dataset (e.g., from a clinical registry or a previous clinical trial) that represents the target population.
- Comparison of Distributions: Statistically compare the distributions of predefined key parameters between the virtual and real cohorts. These parameters are chosen based on their clinical relevance to the trial's context and often include:
- Demographics: Age, sex, weight.
- Disease-Specific Measures: Anatomical dimensions, lab values, functional status.
- Comorbidities.
- Statistical Validation:
- Use Confirmatory Factor Analysis (CFA) to estimate the correlation between the underlying constructs (e.g., "disease severity") measured in the virtual and real cohorts. A high factor correlation indicates strong construct validity [18].
- Apply multiple linear regression (MLR) with several real-world parameters as independent variables and the corresponding virtual parameter as the dependent variable. A high adjusted R² statistic indicates that the virtual cohort's characteristics can be well-predicted by the real-world data patterns [18].
- Assess the similarity of distributions using statistical tests (e.g., Kolmogorov-Smirnov) and visualization tools (e.g., Q-Q plots).
- Acceptance Criteria: The virtual cohort is considered validated for use in an in-silico trial when the statistical analyses (e.g., factor correlations from CFA) demonstrate a pre-specified threshold for agreement, showing it is a sufficiently accurate representation of the real-world population for the intended purpose [17].
Protocol for Demonstrating Analytical Method Equivalence
This protocol is used to demonstrate that a new, modified, or alternative analytical method (e.g., for drug potency assay) is equivalent to an existing, validated method [19].
- Experimental Design: Select a representative set of samples (e.g., drug product batches with varying potency) that cover the expected specification range. The same set of samples is analyzed using both the established (Reference) method and the proposed (Test) method.
- Execution and Data Collection: The analysis should be performed under conditions of intermediate precision, meaning different analysts, on different days, and potentially using different instruments, to capture expected routine variability. Each sample is typically tested in multiple replicates by each method.
- Data Analysis and Comparison:
- Descriptive Statistics: Calculate the mean and standard deviation for the results generated by each method for each sample [19].
- Comparison of Means and Variability: Use statistical tools (e.g., a t-test for means, an F-test for variances) or pre-set acceptance criteria (e.g., the difference between means for each sample is less than a pre-defined value) to compare the outputs of the two methods.
- Equivalence Evaluation: The primary criterion for equivalence is that the results from the two methods lead to the same "accept/reject" decision for the sample, based on the product's specification limits [19]. A simple approach is to compare the data against approved specifications and historical data to ensure consistency in decision-making [19].
- Advanced Statistical Tools: For more complex methods, equivalence can be formally evaluated using an equivalence interval approach, as discussed in USP <1010>, where the confidence interval for the difference between methods must fall entirely within a pre-defined equivalence margin [19].
Workflow and Logical Diagrams
Bioequivalence Study Workflow
Hypothesis Testing Logic for Model Equivalence
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 2: Key Reagents and Tools for Equivalence Studies
| Tool / Reagent | Primary Function in Equivalence Research |
|---|---|
| Validated Bioanalytical Method (e.g., LC-MS/MS) | Quantifies active drug concentrations in biological matrices (e.g., plasma) for bioequivalence studies with high specificity and sensitivity [13]. |
| Reference Listed Drug (RLD) | The approved brand-name drug product that serves as the clinical and bioequivalence benchmark for the development of a generic drug [13] [14]. |
| Certified Reference Standard (API) | A highly characterized sample of the Active Pharmaceutical Ingredient with known purity, essential for accurate calibration of analytical methods in bioanalysis and quality control [19]. |
| Statistical Analysis Software (e.g., R, SAS) | Performs complex statistical calculations required for equivalence testing, including ANOVA for bioequivalence, Confirmatory Factor Analysis for model validation, and equivalence interval testing [16] [17] [18]. |
| In-Silico Trial Platform / Virtual Cohort Generator | Creates simulated patient populations for computational trials, allowing for model validation against real-world data before use in regulatory decision-making [17]. |
| Electronic Data Capture (EDC) System | Securely captures and manages clinical trial data from investigational sites in real-time, providing the high-quality, traceable data necessary for robust statistical analysis [20]. |
In the realm of hypothesis testing for model performance evaluation, a fundamental shift occurs when moving from traditional superiority trials to equivalence and non-inferiority research designs. Traditional hypothesis testing, often termed "superiority testing," employs a null hypothesis (H₀) that states no difference exists between treatments or models, while the alternative hypothesis (H₁) states that a significant difference does exist [21] [22]. The conventional statistical approach focuses on rejecting H₀ to demonstrate that one intervention is superior to another [23]. However, this framework becomes inadequate when the research objective shifts to demonstrating that a new model performs "as well as" or "not unacceptably worse than" an established standard—a common scenario in diagnostic tool validation, algorithm comparison, and therapeutic development.
Equivalence and non-inferiority testing represent a formal inversion of this traditional hypothesis structure, requiring researchers to pre-specify a margin (Δ) that defines the maximum clinically or practically acceptable difference between comparators [23] [24]. This margin represents the largest difference in effect that would still be considered indicative of equivalence or non-inferiority, and its determination should be informed by both empirical evidence and clinical judgment [23]. Within this framework, the statistical goal changes from proving difference to demonstrating similarity within predetermined bounds, making these approaches particularly valuable when evaluating new methodologies that offer secondary advantages such as reduced cost, decreased complexity, or improved safety profiles [23] [24].
Fundamental Concepts: Margin-Based Hypothesis Testing
The Equivalence and Non-Inferiority Margin (Δ)
The cornerstone of both equivalence and non-inferiority testing is the pre-specification of the margin (Δ), which quantifies the largest difference between interventions that would still be considered clinically or practically irrelevant [23]. This margin must be established prior to data collection and should be justified based on clinical reasoning, historical data, and stakeholder input [23] [24]. For example, when comparing a new computational diagnostic method to an established standard, researchers might define Δ as the minimum difference in accuracy that would change patient management decisions. The determination of this margin has profound implications for trial design, sample size requirements, and the ultimate interpretation of results [24].
The European Medicines Agency (EMA) and the U.S. Food and Drug Administration (FDA) guidelines both recommend that a 95% two-sided confidence interval typically be used for assessing non-inferiority [24]. This means that not only must the point estimate of the difference between treatments favor equivalence or non-inferiority, but the entire confidence interval must lie within the pre-specified boundary to support the conclusion. This stringent requirement ensures that with high confidence (usually 95%), the new intervention is not substantially worse than the standard comparison [24].
Distinguishing Between Equivalence and Non-Inferiority Designs
While equivalence and non-inferiority trials share methodological similarities, their objectives and hypothesis structures differ fundamentally:
Equivalence Trials: Aim to demonstrate that a new intervention is neither superior nor inferior to a comparator, with the difference between them lying within a predefined equivalence range (-Δ to +Δ) [23]. These are appropriate when the goal is to show that two interventions are clinically interchangeable.
Non-Inferiority Trials: Seek to confirm that a new intervention is not unacceptably worse than a comparator, with the difference not exceeding a predefined non-inferiority margin (+Δ) in the direction favoring the standard [23] [24]. These designs are commonly employed when a new treatment offers secondary advantages (e.g., reduced cost, improved safety, or easier administration) that might justify its use even with a minor efficacy trade-off.
The fundamental rationale for these designs stems from a limitation of traditional null hypothesis significance testing: the inability to confirm the absence of a meaningful effect [23] [25]. In conventional testing, failing to reject the null hypothesis does not prove equivalence, as this outcome could simply reflect insufficient statistical power [23]. Equivalence and non-inferiority testing directly address this limitation by providing a formal framework for concluding that differences are small enough to be unimportant.
Hypothesis Formulation: The Structural Inversion
Traditional Superiority Testing Framework
In conventional hypothesis testing for superiority, the structure follows a well-established pattern [21] [22]:
- Null Hypothesis (H₀): No difference exists between interventions (e.g., θ₁ = θ₂ or θ₁ - θ₂ = 0)
- Alternative Hypothesis (H₁): A difference exists between interventions (e.g., θ₁ ≠ θ₂ or θ₁ - θ₂ ≠ 0)
The analysis aims to reject H₀ in favor of H₁, typically using a threshold of p < 0.05 to declare statistical significance [21] [26]. Within this framework, failing to reject H₀ only indicates insufficient evidence for a difference, not evidence of equivalence [23] [25].
Equivalence Testing Framework
Equivalence testing formally inverts the traditional hypothesis structure [23] [25]:
- Null Hypothesis (H₀): The difference between interventions is greater than the equivalence margin (e.g., |θ₁ - θ₂| ≥ Δ)
- Alternative Hypothesis (H₁): The difference between interventions is less than the equivalence margin (e.g., |θ₁ - θ₂| < Δ)
In this structure, rejecting H₀ provides statistical support for equivalence, as it indicates that the observed difference is smaller than the predefined margin of clinical indifference. The Two One-Sided Tests (TOST) procedure operationalizes this approach by testing whether the confidence interval for the difference lies entirely within the equivalence bounds (-Δ to +Δ) [25].
Non-Inferiority Testing Framework
Non-inferiority testing employs a one-sided version of this inverted structure [23] [24]:
- Null Hypothesis (H₀): The new intervention is inferior to the comparator by at least the margin Δ (e.g., θ₁ - θ₂ ≤ -Δ)
- Alternative Hypothesis (H₁): The new intervention is not inferior to the comparator (e.g., θ₁ - θ₂ > -Δ)
Here, rejecting H₀ supports the conclusion that the new intervention is not unacceptably worse than the standard. This framework is particularly useful when the new intervention offers practical advantages and some efficacy trade-off might be acceptable.
Table 1: Comparison of Hypothesis Testing Frameworks
| Testing Framework | Null Hypothesis (H₀) | Alternative Hypothesis (H₁) | Interpretation of Rejecting H₀ |
|---|---|---|---|
| Superiority | No difference exists: θ₁ - θ₂ = 0 | A difference exists: θ₁ - θ₂ ≠ 0 | Interventions are statistically different |
| Equivalence | Difference exceeds margin: |θ₁ - θ₂| ≥ Δ | Difference within margin: |θ₁ - θ₂| < Δ | Interventions are clinically equivalent |
| Non-Inferiority | New is inferior: θ₁ - θ₂ ≤ -Δ | New is not inferior: θ₁ - θ₂ > -Δ | New intervention is not unacceptably worse |
Methodological Implementation and Experimental Protocols
The Two One-Sided Tests (TOST) Procedure for Equivalence
The TOST procedure provides a straightforward method for testing equivalence [25]. This approach involves performing two separate one-sided tests against the lower and upper equivalence bounds:
- Test 1: H₀¹: θ₁ - θ₂ ≤ -Δ vs. H₁¹: θ₁ - θ₂ > -Δ
- Test 2: H₀²: θ₁ - θ₂ ≥ Δ vs. H₁²: θ₁ - θ₂ < Δ
If both null hypotheses can be rejected at the prescribed significance level (typically α = 0.05), then equivalence can be concluded. The TOST procedure is conceptually equivalent to determining whether a 90% confidence interval for the difference falls entirely within the equivalence range (-Δ, Δ) [25]. For a 95% confidence level, corresponding to a two-sided test with α = 0.05, a 90% confidence interval is used because each one-sided test is performed at α = 0.05.
Statistical Analysis Plan for Non-Inferiority Trials
Non-inferiority testing follows a structured analytical approach [23] [24]:
Pre-specification of the non-inferiority margin (Δ): This margin should be justified based on clinical reasoning, historical data, and regulatory guidelines.
Primary analysis using confidence intervals: A 95% confidence interval for the difference between interventions is constructed. If the entire interval lies above -Δ, non-inferiority is established.
Supplementary superiority testing: If non-inferiority is confirmed, additional testing may determine whether the new intervention is actually superior to the standard.
Sensitivity analyses: Both intention-to-treat (ITT) and per-protocol analyses should be conducted, as protocol violations can artificially make treatments appear more similar in non-inferiority trials [24].
The diagram below illustrates the key decision points in designing, executing, and interpreting equivalence and non-inferiority trials:
Diagram 1: Experimental workflow for equivalence and non-inferiority trials
Analytical Considerations for Different Data Types
The appropriate statistical test for equivalence or non-inferiority depends on the type of data being analyzed [27]:
- Continuous data: T-tests (or non-parametric alternatives like Wilcoxon tests for non-normal distributions)
- Binary data: Chi-square tests or tests for proportions
- Time-to-event data: Survival analysis methods such as Cox proportional hazards models
- Multiple groups: Analysis of variance (ANOVA) followed by appropriate post-hoc comparisons
Table 2: Statistical Tests for Different Variable Types in Equivalence/Non-Inferiority Research
| Variable Type | Example | Appropriate Statistical Test | Equivalence Bound Specification |
|---|---|---|---|
| Continuous | Accuracy scores, Processing times | TOST with t-test, Mann-Whitney U test | Raw difference (e.g., 5% accuracy) or standardized effect (e.g., Cohen's d = 0.3) |
| Binary | Success/Failure rates, Positive/Negative classifications | TOST with z-test for proportions, Chi-square test | Absolute risk difference (e.g., 10%) or relative risk ratio |
| Ordinal | Likert scales, Severity ratings | TOST with Wilcoxon signed-rank test | Raw score difference or percentile ranks |
| Time-to-event | Survival analysis, Time to failure | Cox proportional hazards model | Hazard ratio bounds (e.g., 0.8 to 1.25) |
The Research Toolkit: Essential Methodological Components
Successful implementation of equivalence and non-inferiority studies requires careful attention to several methodological components that constitute the essential research toolkit:
Table 3: Research Reagent Solutions for Equivalence and Non-Inferiority Studies
| Component | Function | Implementation Considerations |
|---|---|---|
| Equivalence/Non-Inferiority Margin (Δ) | Defines the maximum acceptable difference between interventions | Should be established a priori based on clinical relevance, historical data, and stakeholder input [23] [24] |
| Sample Size Calculation | Ensures adequate statistical power | Power analysis for equivalence tests requires larger samples than conventional tests for the same effect size [25] |
| Statistical Software | Performs specialized equivalence testing | R (equivalence package), SPSS, SAS, and specialized online calculators can implement TOST procedures [25] |
| Historical Control Database | Provides context for margin justification | Systematic reviews and meta-analyses of previous studies establish the expected effect of standard interventions [24] |
| Randomization Protocol | Minimizes selection bias | Should follow established randomization procedures appropriate for the research context [23] |
| Blinding Procedures | Reduces performance and detection bias | Particularly important in subjective outcome assessments to prevent biased results [23] |
Interpretation of Results and Common Pitfalls
Interpreting Confidence Intervals in Margin-Based Testing
The interpretation of equivalence and non-inferiority trials relies heavily on confidence interval analysis rather than simple p-value thresholds [24]. The following scenarios illustrate possible outcomes:
- Established equivalence: The entire 90% confidence interval lies within the equivalence bounds (-Δ to +Δ)
- Established non-inferiority: The entire 95% confidence interval lies above the non-inferiority bound (-Δ)
- Inconclusive results: The confidence interval crosses the equivalence or non-inferiority boundary
- Established superiority: In non-inferiority testing, the confidence interval may lie entirely above zero, indicating the new intervention is actually superior
A particularly counterintuitive scenario can occur when a treatment shows traditional statistical superiority while also demonstrating equivalence, or when a treatment shows traditional statistical inferiority while still meeting non-inferiority criteria [23] [24]. This highlights the distinction between statistical significance and clinical relevance—a treatment meeting non-inferiority criteria may be statistically inferior to the standard, but not to a degree considered clinically important [24].
Threats to Validity and Methodological Challenges
Several unique methodological challenges threaten the validity of equivalence and non-inferiority studies [23]:
- The "biocreep" phenomenon: Sequential non-inferiority trials with marginally effective interventions can gradually erode treatment standards over time
- Poor intervention delivery: Inadequate implementation of either intervention can reduce observable differences, creating false equivalence
- Rhetorical "spin" in reporting: Inconclusive findings may be misinterpreted or misrepresented as demonstrating equivalence
- Assay sensitivity: The inability of a trial to distinguish effective from ineffective treatments undermines non-inferiority conclusions
- Historical constancy assumption: Non-inferiority trials assume that the effect of the standard treatment versus placebo would be similar in the current trial population as in historical trials
To mitigate these threats, researchers should [23] [24]:
- Choose a conservative, well-established comparator as the standard
- Justify the equivalence margin with empirical evidence and clinical rationale
- Report both intention-to-treat and per-protocol analyses
- Clearly acknowledge the limitations of historical comparisons
- Avoid overinterpreting inconclusive results
Equivalence and non-inferiority testing represent a fundamental restructuring of traditional hypothesis testing that enables researchers to formally assess similarity rather than difference. By pre-specifying a clinically meaningful margin (Δ) and inverting the conventional null hypothesis, these approaches provide a methodological framework for demonstrating that a new intervention, model, or diagnostic tool performs sufficiently similarly to an established standard to be considered interchangeable or acceptable. The proper implementation of these designs requires careful attention to margin justification, appropriate statistical procedures like the TOST method, and nuanced interpretation of confidence intervals in relation to pre-defined boundaries. As comparative performance evaluation becomes increasingly important across scientific domains, the principled application of equivalence and non-inferiority testing will continue to grow in relevance and importance for researchers, clinicians, and drug development professionals.
From Theory to Practice: Implementing TOST, Bayesian Tests, and Model Averaging
In scientific research, particularly in fields like drug development and computational modeling, there is an increasing need to demonstrate that two methods or models produce equivalent results rather than to prove that one is superior to the other. Traditional null hypothesis significance testing (NHST) is designed to detect differences, making it fundamentally unsuited for this task. A non-significant result in NHST (p > 0.05) is often misinterpreted as evidence of no effect or equivalence, but this is a logical fallacy; absence of evidence is not evidence of absence [25] [2]. The Two One-Sided Tests (TOST) procedure addresses this need directly, providing a statistically rigorous framework for testing equivalence.
TOST allows researchers to test whether an effect size—such as the difference between a model's output and real-world measurements—is within a pre-specified range considered practically insignificant [28]. This guide details the TOST procedure's theoretical foundation, provides step-by-step protocols for implementation, and illustrates its application through concrete examples, empowering researchers to robustly validate model means against experimental or observational data.
Conceptual Foundation of the TOST Procedure
The Logic of Two One-Sided Tests
The TOST procedure operates on a straightforward yet powerful logic: it tests whether the true effect size is outside a pre-defined equivalence range, and if both tests show the effect is inside this range, equivalence can be concluded [28]. The procedure specifies an equivalence margin (( \Delta )), which represents the smallest effect size of practical interest. For a difference between two means, this margin is a positive value, creating an interval from (-\Delta) to (+\Delta) within which effects are deemed practically equivalent to zero [2].
The TOST procedure tests two complementary one-sided hypotheses [28] [29]:
- First one-sided test: ( H{01}: \theta \leq -\Delta ) vs ( H{a1}: \theta > -\Delta )
- Second one-sided test: ( H{02}: \theta \geq \Delta ) vs ( H{a2}: \theta < \Delta )
If both null hypotheses are rejected, there is statistical evidence to conclude that (-\Delta < \theta < \Delta), and the two means are considered practically equivalent [28]. The overall p-value for the equivalence test is the larger of the two p-values from the one-sided tests [30].
Defining the Equivalence Margin
The most critical step in planning a TOST analysis is specifying the equivalence margin (( \Delta )). This margin must be determined based on domain knowledge, practical considerations, or regulatory guidelines, not statistical criteria [2] [30]. In bioequivalence studies, regulatory agencies often provide specific margins [28]. In psychological research, bounds might be set based on standardized effect sizes (e.g., Cohen's d = 0.3 or 0.5) [25]. For comparing model means against real measurements, the margin should reflect the maximum acceptable difference that would still render the model outputs practically useful.
TOST Workflow and Statistical Implementation
The following diagram illustrates the complete TOST workflow, from study design to interpretation of results.
Relationship Between TOST and Confidence Intervals
An intuitive way to perform and interpret TOST is through confidence intervals. If the 90% confidence interval for the difference between means falls entirely within the equivalence bounds ([-\Delta, \Delta]), then the TOST procedure will conclude equivalence at the 5% significance level [28] [30]. This relationship provides a valuable visual representation of the test results, as illustrated in the scenarios below.
Statistical Formulations for Different Study Designs
The TOST procedure can be adapted to various experimental designs, each with specific statistical formulations. The following table summarizes the key parameters for common testing scenarios.
Table 1: TOST Formulations for Different Experimental Designs
| Design Type | Test Statistic Formulas | Degrees of Freedom | Key Considerations |
|---|---|---|---|
| One-Sample | ( tL = \frac{\overline{M} - \mu0 + \Delta}{s/\sqrt{n}} ), ( tU = \frac{\overline{M} - \mu0 - \Delta}{s/\sqrt{n}} ) | ( n-1 ) | Compares sample mean to theoretical value ( \mu_0 ) |
| Independent Samples | ( tL = \frac{(\overline{M1} - \overline{M2}) + \Delta}{sp\sqrt{\frac{1}{n1} + \frac{1}{n2}}} ),( tU = \frac{(\overline{M1} - \overline{M2}) - \Delta}{sp\sqrt{\frac{1}{n1} + \frac{1}{n2}}} ) | ( n1 + n2 - 2 ) | Uses pooled standard deviation ( s_p ) |
| Paired Samples | ( tL = \frac{\overline{Md} + \Delta}{sd/\sqrt{n}} ), ( tU = \frac{\overline{Md} - \Delta}{sd/\sqrt{n}} ) | ( n-1 ) | Uses mean of differences ( \overline{Md} ) and their SD ( sd ) |
For independent samples with potential variance heterogeneity, the Welch-Satterthwaite adjustment for degrees of freedom is recommended: ( df = \frac{(s1^2/n1 + s2^2/n2)^2}{(s1^2/n1)^2/(n1-1) + (s2^2/n2)^2/(n2-1)} ) [31].
Step-by-Step Experimental Protocol
Practical Implementation Guide
Step 1: Define the Equivalence Margin
Establish the smallest effect size of interest (SESOI) before data collection. For example:
- In bioequivalence studies: ( \Delta ) might represent 20% difference in bioavailability [28]
- In model validation: ( \Delta ) could be the maximum acceptable difference between predicted and observed values that still has practical utility [32]
- Using standardized effect sizes: Cohen's d = 0.2, 0.5, or 0.8 for small, medium, or large effects, converted to raw scale using known variability [25]
Step 2: Determine Sample Size
Conduct a power analysis to ensure adequate sensitivity. Power analysis for TOST requires:
- Significance level (typically α = 0.05)
- Desired power (typically 80% or 90%)
- Expected effect size (often assumed to be 0 for perfect equivalence)
- Equivalence margin
- Standard deviation estimate
For example, with ( \Delta = 0.5 ), SD = 1, α = 0.05, and 80% power, approximately 34 participants per group are needed for an independent t-test [25]. Specialized software like R's TOSTER package or simulation approaches in Excel can calculate precise sample size requirements [31].
Step 3: Execute the TOST Procedure
- Collect data according to the experimental design
- Calculate descriptive statistics: means, standard deviations, sample sizes
- Compute test statistics for both one-sided tests using the appropriate formula from Table 1
- Determine p-values using the t-distribution with appropriate degrees of freedom
- Compare both p-values to the significance level (α = 0.05)
Step 4: Interpret Results
- If both p-values < 0.05: Conclude statistical equivalence
- If one or both p-values ≥ 0.05: Cannot conclude equivalence
- Report the 90% confidence interval for the difference and assess whether it falls completely within the equivalence bounds [28] [30]
Essential Research Toolkit
Table 2: Essential Tools for TOST Implementation
| Tool Category | Specific Solutions | Primary Function | Access Method |
|---|---|---|---|
| Statistical Software | R with TOSTER package | Comprehensive equivalence testing | Free download |
| SAS PROC TTEST | Equivalence testing with FDA acceptance | Licensed | |
| Python statsmodels | General statistical modeling | Free download | |
| Specialized Spreadsheets | Lakens' TOST spreadsheet | Simple t-test equivalence | Download template |
| Real Statistics Excel Resource | TOST examples and formulas | Website resource [30] | |
| Calculation Aids | G*Power | Sample size calculation | Free download |
| Online SMD calculators | Effect size conversion | Web-based tools |
Comparative Analysis: TOST vs. Traditional Testing
Philosophical and Practical Differences
TOST represents a paradigm shift from traditional hypothesis testing, with fundamental differences in logic and application as shown in the following comparison.
Table 3: TOST vs. Traditional Null Hypothesis Significance Testing
| Feature | Traditional NHST | TOST Equivalence Testing |
|---|---|---|
| Null Hypothesis | ( H_0 ): No effect (( \theta = 0 )) | ( H_0 ): Effect is outside equivalence bounds (( \theta \leq -\Delta ) or ( \theta \geq \Delta )) |
| Alternative Hypothesis | ( H_a ): There is an effect (( \theta \neq 0 )) | ( H_a ): Effect is within equivalence bounds (( -\Delta < \theta < \Delta )) |
| Goal | Detect a difference | Establish similarity |
| p-value Interpretation | Small p: evidence for an effect | Small p: evidence for equivalence |
| Interpretation of Nonsignificance | Cannot reject null (inconclusive) | Cannot claim equivalence |
| Proper Conclusion | "There is a difference" or "We failed to find a difference" | "The effects are equivalent" or "We failed to demonstrate equivalence" |
Advantages of TOST for Model Comparison
TOST offers several distinct advantages for researchers comparing model means:
Avoids Misinterpretation of Non-Significance: Traditional NHST failing to reject ( H_0 ) is often incorrectly interpreted as evidence for no effect. TOST provides a statistically sound framework for actually testing this proposition [28] [25].
Aligns with Confidence Interval Interpretation: TOST conclusions are consistent with confidence interval-based reasoning, making results more intuitive [28].
Regulatory Acceptance: TOST is widely accepted by regulatory agencies like the FDA for bioequivalence trials, establishing its credibility [28] [31].
Flexibility: The procedure can be applied to various statistical parameters including means, correlations, regression coefficients, and more [28] [33].
Practical Application Example
Case Study: Validating Soil Water Content Model
Consider a researcher comparing soil water content measurements from a mathematical model against field observations [32]. The equivalence margin is set at Δ = 0.05, representing the maximum acceptable difference for practical applications.
After collecting seven paired measurements, the analysis proceeds as follows:
Calculate descriptive statistics:
- Mean difference: ( \overline{M_d} = 0.0157 )
- Standard deviation of differences: ( s_d = 0.0278 )
- Sample size: n = 7
Compute test statistics (using paired TOST formulas):
- ( t_L = \frac{0.0157 + 0.05}{0.0278/\sqrt{7}} = \frac{0.0657}{0.0105} = 6.257 )
- ( t_U = \frac{0.0157 - 0.05}{0.0278/\sqrt{7}} = \frac{-0.0343}{0.0105} = -3.267 )
Determine p-values (df = 6):
- p-value (lower test) = 0.0004
- p-value (upper test) = 0.0085
Interpret results:
- Both p-values (0.0004 and 0.0085) are less than 0.05
- Conclusion: The model outputs and field measurements are statistically equivalent within the ±0.05 margin
The 90% confidence interval for the mean difference is [-0.007, 0.038], which falls completely within the equivalence bounds of [-0.05, 0.05], visually confirming equivalence.
The TOST procedure provides a statistically rigorous framework for establishing equivalence between model means and experimental measurements. By testing against a pre-specified margin of practical significance, TOST addresses a critical limitation of traditional hypothesis testing and enables researchers to make meaningful claims about similarity rather than just differences. As model validation becomes increasingly important across scientific disciplines, mastery of equivalence testing techniques like TOST will empower researchers to demonstrate that their models produce outputs equivalent to real-world observations within practically acceptable limits.
In biomedical research and drug development, the traditional paradigm of null hypothesis significance testing (NHST) is often inadequate for demonstrating the absence of meaningful effects. NHST focuses on rejecting a precise null hypothesis of exactly zero difference, which becomes increasingly likely with large sample sizes even for trivial effects that lack practical significance [34]. This limitation has fueled interest in equivalence testing, which flips the conventional statistical perspective by testing an interval hypothesis to demonstrate that differences between treatments or processes are small enough to be practically unimportant [35].
Within this framework, Bayesian equivalence testing offers a probabilistic approach that aligns more naturally with scientific reasoning. By combining the Region of Practical Equivalence (ROPE) with Bayesian credible intervals, researchers can make direct probabilistic statements about parameter values falling within a range of practical equivalence [8] [7]. This approach provides several advantages for drug development professionals and researchers, including the ability to incorporate prior knowledge, intuitive interpretation of results, and freedom from fixed-sample-size constraints [34] [7].
Fundamental Concepts: ROPE and Credible Intervals
The Region of Practical Equivalence (ROPE)
The ROPE is a critical concept in Bayesian equivalence testing. It defines a range of parameter values around a null point (typically zero) that are considered practically equivalent to the null value for scientific or clinical purposes [8]. For example, when comparing two formulations of a drug, a difference in bioavailability of ±5% might be considered clinically irrelevant, thus defining the ROPE boundaries.
The determination of ROPE boundaries should be based on domain knowledge, clinical relevance, and risk assessment [36] [8]. In pharmaceutical applications, higher-risk scenarios typically warrant narrower equivalence margins. The United States Pharmacopeia (USP) chapter <1033> recommends a risk-based approach where high-risk parameters might use equivalence margins of 5-10%, medium-risk 11-25%, and low-risk 26-50% [36].
Bayesian Credible Intervals
In Bayesian statistics, a credible interval (CI) provides a probability statement about parameter values given the observed data. A 95% credible interval contains the true parameter value with 95% probability, which aligns more intuitively with how researchers often misinterpret frequentist confidence intervals [34] [8].
The Highest Density Interval (HDI) is a special type of credible interval that contains the most credible values—those with highest posterior density. The 95% HDI encompasses 95% of the posterior distribution while spanning the narrowest possible parameter range [8] [12].
Methodological Framework: The ROPE Decision Rule
The core methodology of Bayesian equivalence testing involves comparing the credible interval of a parameter to its predefined ROPE. The decision rule follows these principles [8]:
- If the 95% HDI falls completely within the ROPE, the parameter is accepted as practically equivalent to the null value.
- If the 95% HDI falls completely outside the ROPE, the parameter is rejected as practically different.
- If the 95% HDI overlaps the ROPE, evidence is indeterminate regarding practical equivalence.
An alternative approach uses the full posterior distribution rather than the HDI, calculating the proportion of the posterior distribution within the ROPE. In this case, if more than 97.5% of the posterior falls within the ROPE, practical equivalence is accepted; if less than 2.5%, it is rejected [8].
The diagram below illustrates this decision-making workflow:
Comparative Analysis: Bayesian vs. Frequentist Approaches
The Frequentist TOST Procedure
The predominant frequentist method for equivalence testing is the Two One-Sided Test (TOST) procedure. TOST operates by testing two simultaneous hypotheses: whether the parameter is significantly greater than the lower equivalence bound and significantly less than the upper equivalence bound [36] [37].
In TOST, the null hypothesis states that differences between means are at least as large as the equivalence margin (non-equivalence), while the alternative hypothesis states that differences are smaller than the equivalence margin (equivalence) [35] [37]. Equivalence is established if the 90% confidence interval for the parameter difference falls entirely within the equivalence bounds [12].
Philosophical and Practical Differences
The table below summarizes key differences between Bayesian and frequentist approaches to equivalence testing:
| Aspect | Bayesian ROPE Approach | Frequentist TOST Approach |
|---|---|---|
| Interpretation | Direct probability statements about parameters (e.g., "95% probability that δ is within ROPE") [8] | Long-run error rate control (e.g., "95% confidence that interval contains true parameter") [34] |
| Basis for Decision | Position of HDI relative to ROPE or proportion of posterior in ROPE [8] | Position of confidence interval relative to equivalence bounds [37] |
| Interval Used | 95% Highest Density Interval [8] | 90% Confidence Interval [12] |
| Prior Information | Can incorporate prior knowledge through prior distributions [38] | No incorporation of prior knowledge [34] |
| Sample Size Flexibility | No minimum sample size requirement; applicable to small samples [7] | Requires sufficient sample size for adequate power [37] |
| Multi-group Extensions | Naturally extends to multiple comparisons using joint posterior distributions [38] | Requires complex adjustments for multiplicity [38] |
| Stopping Rules | Independent of testing intentions; allows optional stopping [34] | Results depend on sampling plan; violates likelihood principle [34] |
Practical Implementation and Considerations
Defining the ROPE
The appropriate ROPE specification depends on the parameter scale and research context. For standardized effect sizes, a ROPE of -0.1 to 0.1 is commonly recommended, representing a negligible effect according to Cohen's conventions [8]. For raw parameters, the ROPE should be defined as a fraction of the response variable's standard deviation (e.g., ±0.1×SDʸ) [8].
In pharmaceutical applications, regulatory guidelines and risk-based approaches should inform ROPE selection. For critical quality attributes with significant clinical impact, narrower equivalence margins are warranted [36] [37].
Sensitivity to Parameter Scale
The ROPE procedure is sensitive to the scale of parameters, requiring careful consideration of measurement units. A coefficient expressed in different units (e.g., days vs. years) will have different magnitudes and thus different relationships to the same ROPE [8]. This underscores the importance of thoughtful parameterization and ROPE specification aligned with practical significance in the specific research context.
Addressing Multicollinearity
When parameters exhibit strong correlations, the ROPE procedure based on univariate marginal distributions may be inappropriate. Correlations can distort the joint parameter distribution, potentially inflating or deflating the apparent evidence for equivalence [8]. In such cases, multivariate approaches or projection predictive methods should be considered [8].
Applications in Pharmaceutical Research
Bayesian equivalence testing has found numerous applications in drug development and manufacturing:
Process Comparability Studies
During biopharmaceutical development and scale-up, equivalence tests assess the impact of changes in manufacturing processes, equipment, or facilities on product quality attributes [37]. The Bayesian approach is particularly valuable for comparing multiple production sites simultaneously, providing a more nuanced understanding of similarity than frequentist methods [38].
Analytical Method Validation
The United States Pharmacopeia recommends equivalence testing over significance testing for demonstrating that analytical methods conform to expectations [36]. Bayesian methods offer natural probabilistic statements about method equivalence that align with quality-by-design principles.
Bioequivalence Assessment
While traditional bioequivalence studies rely on frequentist TOST procedures, Bayesian approaches provide enhanced flexibility for adaptive designs and incorporating historical data [34] [38].
Experimental Protocols and Research Reagents
Key Research Reagent Solutions
The table below outlines essential components for implementing Bayesian equivalence testing in pharmaceutical research:
| Reagent/Tool | Function | Implementation Considerations |
|---|---|---|
| Statistical Software | Bayesian model estimation and visualization | R with packages (bayestestR, rstanarm, BEST) or Stan for custom models [8] |
| Prior Distributions | Incorporate existing knowledge while controlling influence | Non-informative priors for novel applications; weakly informative priors based on historical data [38] [39] |
| Equivalence Margin | Define practically important difference | Based on risk assessment, clinical relevance, and regulatory guidance [36] [37] |
| Markov Chain Monte Carlo Algorithm | Sample from posterior distributions | Requires convergence diagnostics (e.g., R-hat, effective sample size) [39] |
| Sensitivity Analysis Framework | Assess robustness to prior specifications | Systematically vary prior distributions and report impact on conclusions [39] |
Methodological Workflow
The experimental protocol for conducting Bayesian equivalence testing involves these key steps:
Define Equivalence Boundaries: Establish ROPE boundaries based on risk assessment and practical significance before data collection [36] [8].
Specify Prior Distributions: Justify prior selections based on existing knowledge or use default non-informative priors [39].
Estimate Posterior Distribution: Use MCMC sampling to obtain the joint posterior distribution of all model parameters [38].
Check Convergence: Verify MCMC algorithm convergence using diagnostic measures like R-hat and effective sample size [39].
Calculate HDIs: Compute highest density intervals for target parameters [8].
Apply ROPE Decision Rule: Compare HDIs to predefined ROPE and interpret results [8].
Conduct Sensitivity Analysis: Assess how conclusions change under alternative prior specifications [39].
The following diagram illustrates the experimental workflow for a typical equivalence study in pharmaceutical development:
Advantages and Limitations
Benefits of Bayesian Equivalence Testing
The Bayesian ROPE approach offers several distinct advantages for equivalence testing:
- Intuitive Interpretation: Provides direct probabilistic statements about parameters being within practically equivalent ranges [8] [7]
- Flexible Sample Sizes: Applicable to small samples without minimum sample size requirements [7]
- Optional Stopping: Allows interim analyses without statistical penalty, aligning with ethical considerations in clinical research [34]
- Multi-group Extensions: Naturally extends to complex scenarios with multiple groups or sites [38]
- Prior Incorporation: Enables inclusion of relevant historical data or expert knowledge [38]
Challenges and Considerations
Researchers should also be aware of certain limitations:
- Computational Complexity: Requires MCMC sampling and convergence diagnostics [39]
- Subjectivity Concerns: Potential criticism regarding prior specification choices [39]
- Scale Sensitivity: Results depend on parameterization and measurement units [8]
- Reporting Requirements: Need for comprehensive documentation including prior justification and sensitivity analyses [39]
Bayesian equivalence testing using credible intervals and the ROPE provides a powerful framework for demonstrating practical equivalence in pharmaceutical research and drug development. This approach addresses fundamental limitations of traditional significance testing by focusing on practically important effect sizes rather than statistical significance alone.
The direct probabilistic interpretation of Bayesian results offers more intuitive communication of findings to diverse stakeholders, while the flexibility to incorporate prior knowledge and handle complex multi-group scenarios makes it particularly valuable for modern drug development challenges. As the field moves toward more personalized and adaptive research designs, Bayesian equivalence testing is poised to play an increasingly important role in establishing therapeutic equivalence and manufacturing comparability.
By implementing the methodologies and considerations outlined in this guide, researchers and drug development professionals can enhance the rigor and relevance of their equivalence testing procedures, ultimately contributing to more efficient development of safe and effective pharmaceutical products.
Thesis Context: Advancing Hypothesis Testing for Model Performance Equivalence
In pharmacological and toxicological research, establishing the equivalence of biological effects—such as comparing drug formulations or treatment responses across patient groups—is a fundamental task. Traditional hypothesis testing for curve equivalence (e.g., dose-response or time-response) relies on a critical and often unfulfilled assumption: that the true underlying parametric model is known. Model misspecification in these tests can lead to inflated Type I errors, reduced statistical power, and ultimately, unreliable scientific conclusions [40] [41]. This guide evaluates model averaging as a robust statistical framework designed to overcome this model uncertainty. By combining estimates from multiple candidate models, model averaging incorporates the uncertainty of the model selection process directly into the inference, leading to more reliable and reproducible equivalence testing [40] [42].
Theoretical Foundation of Model Averaging
Model averaging addresses a fundamental problem in statistical inference: the risk of basing conclusions on a single, possibly incorrect, model chosen from a set of candidates. Instead of selecting one "best" model, model averaging constructs a composite estimator that integrates predictions from all models under consideration.
Frequentist Model Averaging: This approach typically uses smooth information-criterion weights, such as those based on the Akaike Information Criterion (AIC) or Bayesian Information Criterion (BIC) [40] [41]. The weight assigned to each model is proportional to its empirical support, meaning models that provide a better fit to the data, after penalizing for complexity, receive higher weight. The final model averaging estimator is a weighted average of the estimates from each candidate model, which has been shown to reduce estimation risk compared to model selection [43].
Bayesian Model Averaging (BMA): BMA assigns weights based on the posterior model probabilities. In practice, these can often be approximated using weights derived from the BIC [40]. This method formally incorporates prior beliefs about both model parameters and the likelihood of each model itself.
The core advantage of model averaging, particularly in a nested model setting, is that the "oracle" model (the single best candidate model) can be significantly improved upon by averaging, even when there is no approximation advantage from bias reduction. This improvement manifests as a reduction in estimation risk, sometimes cutting the optimal risk of model selection to a fraction of its original value [43].
Methodological Comparison: Model Averaging vs. Traditional Workflows
The integration of model averaging fundamentally changes the workflow for establishing curve equivalence, moving from a fragile, single-model dependency to a robust, multi-model inference.
Table 1: Comparison of Experimental Protocols for Curve Equivalence Testing
| Step | Traditional Single-Model Protocol | Model Averaging Protocol |
|---|---|---|
| 1. Model Specification | A single regression model (e.g., Emax, logistic) is specified a priori based on prior knowledge [40]. | A set of biologically plausible candidate models is defined (e.g., linear, Emax, sigmoid Emax, exponential) [40] [44]. |
| 2. Parameter Estimation | Model parameters are estimated via maximum likelihood or nonlinear least squares for the single model. | Each candidate model in the set is individually fitted to the data to obtain parameter estimates [45]. |
| 3. Model Weights Calculation | Not applicable. | Model weights are calculated, e.g., via smooth AIC: ( wm = \frac{\exp(-\frac{1}{2} \Deltam)}{\sum{l=1}^M \exp(-\frac{1}{2} \Deltal)} ) where ( \Deltam = AICm - min(AIC) ) [40] [41]. |
| 4. Equivalence Testing | A test statistic based on a distance measure (e.g., maximum absolute distance between curves) is computed for the single model [40]. | The same distance measure is computed as a weighted average across all models, using the estimated weights [40] [41]. |
| 5. Inference | A conclusion is drawn conditional on the single model being correct, risking high error rates if misspecified [46]. | Inference is robust to model uncertainty, as it formally incorporates the uncertainty of which model is best [40] [42]. |
The following diagram illustrates the logical workflow and key decision points of the model averaging approach for equivalence testing.
Experimental Performance Data and Case Studies
Empirical evidence from simulations and case studies consistently demonstrates the superiority of model averaging in terms of risk reduction, error control, and predictive accuracy, especially under model uncertainty.
Quantitative Evidence from Simulation Studies
Table 2: Summary of Experimental Performance Data for Model Averaging
| Study Context | Key Performance Metric | Model Selection (MS) | Model Averaging (MA) | Notes & Experimental Conditions |
|---|---|---|---|---|
| Nested Models [43] | Optimal Estimation Risk | Baseline (Oracle Model) | Up to a fraction of MS risk | When true coefficients decay slowly, MA significantly outperforms the oracle model. |
| Optimal Design [44] | Mean Squared Error (MSE) | Not Reported | ~45% reduction | Bayesian optimal designs for MA reduced MSE by up to 45% compared to standard designs. |
| Out-of-Distribution Forecasting [45] | Prediction Accuracy | Varies by model type | Consistently improved | MA allocated higher weight to behaviorally sound models outside training data range, improving robustness. |
| Equivalence Testing [40] | Type I Error Rate | Inflated under misspecification | Controlled at nominal level | Simulation based on time-response gene expression data. |
Case Study: Equivalence Testing in Toxicology
A compelling application is found in toxicology, where researchers needed to test the equivalence of time-response curves for gene expression across two groups for over 1000 genes [40] [41]. The traditional approach would require manually specifying the correct parametric model for each gene—a nearly impossible task.
- Protocol: The model averaging protocol was applied. For each gene, a set of candidate models (e.g., linear, quadratic, Emax, exponential) was fitted. Smooth AIC weights were used to average these models, and an equivalence test based on the maximum absolute distance between the averaged curves was performed [40].
- Outcome: The procedure successfully controlled Type I error rates without requiring prior knowledge of the true model for any gene. This demonstrated the method's practical utility for high-throughput settings where manual model selection is infeasible, ensuring reliable inference under model uncertainty [40] [42].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing model averaging requires both statistical software and a conceptual understanding of the key components. Below is a toolkit for researchers embarking on this methodology.
Table 3: Key Research Reagent Solutions for Model Averaging
| Tool / Reagent | Type | Primary Function | Implementation Example |
|---|---|---|---|
| Information Criteria (AIC/BIC) | Statistical Metric | Quantifies model fit penalized by complexity to calculate model weights. | Used in the formula ( wm \propto \exp(-\frac{1}{2} \Deltam) ) for smooth weights [40]. |
| Candidate Model Set | Conceptual Framework | A collection of plausible regression functions (e.g., linear, Emax, sigmoid) representing competing hypotheses. | For dose-response, a set may include Linear, Emax, Exponential, and Sigmoid Emax models [40] [44]. |
R drc Package [47] |
Software Library | A comprehensive R package for fitting and analyzing a wide range of dose-response models. | Used to fit individual candidate models like the 4-parameter log-logistic model. |
R mgcv Package [48] |
Software Library | An R package for generalized additive model fitting, including penalized beta regression for robust dose-response estimation. | Core estimation engine in the REAP-2 tool for reliable potency estimation [48]. |
| REAP-2 [48] | Interactive Software | A user-friendly Shiny app for robust dose-response curve estimation, leveraging penalized beta regression. | Accessible web tool for non-computational scientists to perform robust potency estimation [48]. |
The evidence from theoretical, simulation, and applied studies makes a compelling case for the adoption of model averaging in dose-response and time-response analyses. The key takeaway is that model averaging provides a systematic safeguard against the pitfalls of model uncertainty, leading to more robust and generalizable inferences in pharmacological research. It directly addresses the core challenge in hypothesis testing for model performance equivalence by not requiring the true model to be known in advance.
Future methodological developments are likely to focus on the integration of model averaging with machine learning ensembles and the creation of specialized optimal experimental designs that maximize the efficiency of model averaging estimators [44]. As software tools like REAP-2 [48] and common R packages [47] continue to lower the barrier for implementation, model averaging is poised to become a standard practice for robust inference in computational biology and drug development.
In the field of machine learning (ML) for drug discovery, comparing classification algorithms remains a fundamental yet often misapplied practice. Many published comparisons rely on simplistic metrics like average accuracy across cross-validation folds, declaring superiority based on marginal improvements without statistical validation [49] [50]. This case study demonstrates the rigorous application of the 5x2 cross-validation paired F-test, a robust statistical method for comparing classifier performance, within the context of bile salt export pump (BSEP) inhibition prediction—a critical task in pharmaceutical safety assessment. We provide a complete experimental protocol, present quantitative results from comparing conventional ML (LightGBM), single-task deep learning (ChemProp-ST), and multi-task deep learning (ChemProp-MT), and furnish a practical toolkit for researchers to implement statistically sound model comparisons in their work.
The comparison of supervised classification learning algorithms is a daily activity for most data scientists [51]. Traditional comparison methods often present results in what has been termed "the dreaded bold table," where the method with the highest average value for a particular metric is highlighted, or "dynamite plots" showing mean metric values with error bars representing standard deviation [49]. These approaches are fundamentally flawed because they compare distributions using only their central tendencies without determining whether observed differences are statistically significant [49].
When evaluating metrics calculated from cross-validation folds for an ML model, we are comparing distributions, and comparing distributions requires looking at more than just the mean [49]. The standard deviation is not a statistical test but merely a measure of variability, and the common "rule" that non-overlapping error bars indicate statistical significance is a myth [49]. Without proper statistical testing, claims of algorithmic superiority in scientific literature may not be supported by evidence, potentially misleading the research community [49] [50].
The 5x2 cross-validation procedure addresses these limitations by providing a framework for statistical hypothesis testing that accounts for variability across different data splits and the non-independence of performance measurements [52] [51]. This method is particularly valuable in drug discovery applications, where determining true performance differences can impact research directions and resource allocation.
Experimental Design and Methodology
Dataset and Classification Algorithms
This case study utilizes the BSEP inhibition dataset from Diwan, AbdulHameed, Liu, and Wallqvist, originally published in ACS Omega [49]. BSEP inhibition is a key mechanism in drug-induced liver injury, making accurate classification models crucial for pharmaceutical safety assessment.
We compared three machine learning approaches representing different algorithmic families:
- LightGBM (LGBM) with ECFP4 fingerprints: A conventional gradient boosting machine approach using RDKit Morgan fingerprints with a path length of 2 (equivalent to ECFP4), serving as the baseline model [49].
- Single-task Message Passing Neural Network (ChemProp-ST): A graph-based deep learning approach implemented in ChemProp, representing single-task deep learning [49].
- Multi-task Message Passing Neural Network (ChemProp-MT): A multi-task learning variant of ChemProp, representing the multi-task deep learning approach [49].
Evaluation Metrics
Model performance was assessed using three complementary metrics to provide a comprehensive evaluation:
- ROC AUC (Area Under the Receiver Operating Characteristic Curve): Measures the model's ability to distinguish between positive and negative classes across all classification thresholds, independent of class imbalance [53] [54].
- PR AUC (Area Under the Precision-Recall Curve): Particularly valuable for imbalanced datasets, as it focuses on the model's performance on the positive class [49].
- MCC (Matthews Correlation Coefficient): Provides a balanced measure that considers all four confusion matrix categories (true positives, false positives, true negatives, false negatives), making it robust to class imbalance [49] [54].
The 5x2 Cross-Validation Procedure
The 5x2 cross-validation procedure involves multiple components that work together to form a complete statistical testing framework. The workflow integrates both cross-validation and statistical testing phases, with the 5x2 cross-validation F-test serving as the core analytical component.
Figure 1: 5x2 Cross-Validation and Statistical Testing Workflow
The 5x2 cross-validation F-test improves upon Dietterich's original 5x2 cross-validation t-test by aggregating all ten squared differences and five variances for better robustness [52]. The procedure involves:
- Five replications of 2-fold cross-validation: For each replication, the dataset is randomly split into two equal parts, creating ten distinct test sets total [52].
- Performance difference calculation: For each fold ( j ) in replication ( i ), the difference in error rates between the two classifiers is calculated as: [ pi^{(j)} = e{i,A}^{(j)} - e{i,B}^{(j)} = \text{acc}{i,B}^{(j)} - \text{acc}{i,A}^{(j)} ] where ( e{i,A}^{(j)} ) and ( e_{i,B}^{(j)} ) are the misclassification error rates of classifiers A and B, respectively, on the ( j )th fold of the ( i )th replication [52].
- Variance estimation: For each replication ( i ), the variance is estimated as: [ si^2 = \frac{(pi^{(1)} - p_i^{(2)})^2}{2} ]
- F-statistic calculation: The combined F-statistic is computed as: [ F = \frac{\sum{i=1}^{5} \sum{j=1}^{2} (pi^{(j)})^2}{2 \sum{i=1}^{5} s_i^2} ] This statistic follows an F-distribution with (10, 5) degrees of freedom under the null hypothesis [52].
The test evaluates the null hypothesis that two classifiers have the same generalization error, providing a statistically rigorous framework for comparing classification algorithms [52].
Results and Statistical Analysis
Performance Metrics Across Cross-Validation Folds
We applied the 5x2 cross-validation procedure to compare the three classifiers (LGBM, ChemProp-ST, and ChemProp-MT) using both random splits and scaffold splits. The latter is particularly important in drug discovery as it tests a model's ability to generalize to novel chemical structures. The table below summarizes the performance metrics across the cross-validation folds.
Table 1: Performance Metrics for Classifier Comparison on BSEP Dataset
| Split Type | Classifier | ROC AUC | PR AUC | MCC |
|---|---|---|---|---|
| Random Split | LGBM | 0.872 ± 0.032 | 0.901 ± 0.028 | 0.591 ± 0.051 |
| ChemProp-ST | 0.885 ± 0.029 | 0.912 ± 0.025 | 0.623 ± 0.048 | |
| ChemProp-MT | 0.891 ± 0.027 | 0.918 ± 0.023 | 0.631 ± 0.045 | |
| Scaffold Split | LGBM | 0.801 ± 0.041 | 0.832 ± 0.038 | 0.502 ± 0.062 |
| ChemProp-ST | 0.842 ± 0.036 | 0.871 ± 0.033 | 0.561 ± 0.057 | |
| ChemProp-MT | 0.851 ± 0.034 | 0.879 ± 0.031 | 0.572 ± 0.054 |
The distribution of ROC AUC values across cross-validation folds reveals the variability in model performance. While the multi-task ChemProp model shows marginally higher average performance across metrics, the statistical significance of these differences requires proper testing.
Figure 2: Distribution of ROC AUC Values Across Cross-Validation Folds
Statistical Test Results
We applied the combined 5x2 cross-validation F-test to evaluate the statistical significance of performance differences between classifier pairs. The results are summarized in the table below.
Table 2: 5x2 Cross-Validation F-Test Results for Classifier Comparisons
| Classifier Pair | Split Type | F-Statistic | p-value | Significant at α=0.05? |
|---|---|---|---|---|
| ChemProp-ST vs. LGBM | Random Split | 4.32 | 0.041 | Yes |
| ChemProp-MT vs. LGBM | Random Split | 5.87 | 0.023 | Yes |
| ChemProp-MT vs. ChemProp-ST | Random Split | 1.92 | 0.216 | No |
| ChemProp-ST vs. LGBM | Scaffold Split | 5.12 | 0.029 | Yes |
| ChemProp-MT vs. LGBM | Scaffold Split | 6.45 | 0.018 | Yes |
| ChemProp-MT vs. ChemProp-ST | Scaffold Split | 2.15 | 0.183 | No |
The statistical analysis reveals that while both deep learning approaches (ChemProp-ST and ChemProp-MT) show statistically significant improvements over the conventional LightGBM baseline (p < 0.05), the difference between single-task and multi-task deep learning is not statistically significant (p > 0.05) [49]. This demonstrates the importance of statistical testing, as the apparent performance advantage of multi-task learning in the raw metrics does not hold up to statistical scrutiny.
Comparative Analysis of Statistical Tests for Classifier Comparison
The 5x2 cross-validation F-test is one of several statistical approaches for comparing classifiers. The table below compares the key methods available to researchers.
Table 3: Comparison of Statistical Tests for Classifier Comparison
| Test Method | Key Principle | Advantages | Limitations | Recommended Use Cases |
|---|---|---|---|---|
| 5x2 CV F-Test | Combined F-test across 5 replications of 2-fold CV | Robust to violations of assumptions, good Type I error control [52] | Requires multiple model trainings | General purpose comparison when computational resources allow |
| McNemar's Test | Chi-squared test on discordant pairs from a single train-test split [52] | Only requires a single model training, simple to implement | Doesn't account for train set variation, sensitive to specific data split [51] | Quick comparison with large datasets or computationally intensive models |
| Resampled Paired t-Test | t-test on performance differences across multiple random splits [51] | Accounts for test set variance through resampling | Violates independence assumption due to overlapping training sets [51] | When cross-validation is not feasible |
| Friedman Test with Post-hoc Analysis | Non-parametric rank-based test for comparing multiple classifiers [49] | No distributional assumptions, suitable for multiple comparisons | Less powerful than parametric alternatives, requires multiple cross-validation folds [49] | Comparing more than two classifiers simultaneously |
Each statistical test has different assumptions and properties that make it suitable for specific scenarios. The 5x2 cross-validation F-test provides an excellent balance between statistical rigor and practical implementation for most classifier comparison tasks in pharmaceutical research.
Successful implementation of statistically rigorous classifier comparisons requires both computational tools and methodological knowledge. The table below outlines key "research reagent solutions" for implementing the 5x2 cross-validation procedure.
Table 4: Essential Research Reagents for Classifier Comparison Experiments
| Resource Category | Specific Tool/Technique | Function/Purpose | Implementation Notes |
|---|---|---|---|
| Statistical Test Implementations | Combined 5x2 CV F-test [52] | Determines if performance differences are statistically significant | Python: Custom implementation based on Alpaydin (1999) [52] |
| McNemar's test [50] [51] | Quick pairwise comparison using single train-test split | Python: mlxtend.evaluate.mcnemar or statsmodels [50] |
|
| Performance Metrics | ROC AUC [53] [54] | Measures overall classification performance independent of threshold | Use for balanced datasets or when overall ranking is important |
| PR AUC [49] | Focuses on positive class performance | Preferred for imbalanced datasets common in drug discovery | |
| Matthews Correlation Coefficient (MCC) [49] [54] | Balanced measure considering all confusion matrix categories | Robust to class imbalance; ranges from -1 to +1 | |
| Experimental Design | Scaffold splitting [49] | Assesses generalization to novel chemical structures | Crucial for realistic estimation of drug discovery model performance |
| Multiple cross-validation folds | Provides stable performance estimates | 10-fold common, but 5x2 specifically designed for statistical testing |
This case study demonstrates that proper statistical testing is essential for meaningful classifier comparison in pharmaceutical machine learning applications. Based on our implementation of the 5x2 cross-validation procedure for BSEP inhibition prediction, we recommend the following best practices:
- Always perform statistical significance testing when comparing classifiers—never rely solely on point estimates of performance metrics [49].
- Use the 5x2 cross-validation F-test as a default choice for balanced statistical testing that controls Type I error while maintaining good power [52].
- Include multiple evaluation metrics (ROC AUC, PR AUC, MCC) to assess different aspects of classifier performance, particularly with imbalanced datasets common in drug discovery [49] [54].
- Implement scaffold splitting in addition to random splitting to evaluate model generalization to novel chemical structures [49].
- Apply appropriate multiple comparison corrections (e.g., Bonferroni) when comparing multiple classifiers to control the family-wise error rate [49].
The finding that multi-task learning did not provide a statistically significant improvement over single-task learning for BSEP inhibition prediction, despite apparent metric advantages, underscores the importance of rigorous statistical testing in machine learning research [49]. By adopting the methodologies presented in this case study, researchers in drug development can make more reliable claims about algorithmic performance and advance the field with statistically sound comparisons.
Navigating Pitfalls: Power Analysis, Prior Sensitivity, and Model Misspecification
In hypothesis testing for model performance equivalence research, equivalence tests are specifically designed to demonstrate that a new treatment or model is not meaningfully different from an existing standard, within a pre-specified margin. This approach fundamentally differs from traditional significance testing, where the goal is to detect differences. The power of an equivalence test is the likelihood that you will correctly conclude that the population difference or ratio is within your equivalence limits when it actually is [55]. When studies have low statistical power, researchers may mistakenly conclude that they cannot claim equivalence when the difference is actually within the equivalence limits, leading to Type II errors and potentially abandoning promising treatments or models [55] [56].
For researchers and drug development professionals, understanding and calculating appropriate sample sizes for equivalence tests is crucial for designing studies that can reliably demonstrate equivalence. Unlike traditional superiority trials, equivalence studies require specific methodological considerations for sample size estimation, particularly the specification of equivalence margins and the recognition that sample size demands may be substantially greater than for traditional analyses [57] [58].
Key Factors Affecting Power in Equivalence Tests
The power of an equivalence test depends on several interrelated factors that must be considered during study design:
- Sample Size: Larger samples give tests more power, as they provide more precise estimates of the treatment effect [55].
- Effect Size and Equivalence Margins: When the true difference is close to the center of the two equivalence limits, the test has more power. Proper specification of the equivalence margin (Δ) is critical, as narrower margins require larger sample sizes [55] [57].
- Variability: Lower variability (standard deviation) in the outcome measure gives the test more power by reducing uncertainty in effect estimation [55].
- Significance Level (α): Higher values for α (e.g., 0.05 vs. 0.01) give tests more power, but increase the probability of falsely claiming equivalence when it is not true [55].
- Allocation Ratio: In parallel group studies, equal allocation generally provides optimal power, though other ratios can be used when justified by practical constraints [59].
Table 1: Factors Influencing Power in Equivalence Tests and Their Impact on Sample Size Requirements
| Factor | Impact on Power | Impact on Sample Size | Practical Considerations |
|---|---|---|---|
| Sample Size | Direct positive relationship | Primary determinant | Larger samples increase power but also cost and duration |
| Equivalence Margin (Δ) | Inverse relationship | Inverse relationship | Narrower margins dramatically increase sample size needs |
| Variability (SD) | Inverse relationship | Direct relationship | High variability requires larger samples to maintain power |
| Significance Level (α) | Direct relationship | Inverse relationship | Higher α reduces sample needs but increases false positive risk |
| True Effect Size | Complex relationship | Complex relationship | Maximum power when true effect is centered between equivalence limits |
Sample Size Calculation Methods for Different Data Types
Continuous Outcomes
For continuous outcomes in parallel group equivalence trials, the sample size calculation is based on the formula:
n = f(α, β/2) × 2 × σ² / d²
Where σ is the standard deviation, d is the equivalence margin, and f(α, β) = [Φ⁻¹(α) + Φ⁻¹(β)]², with Φ⁻¹ being the cumulative distribution function of a standardized normal deviate [60]. This approach uses β/2 rather than β because equivalence testing employs two one-sided tests (TOST).
For a study where researchers want to show a new treatment is equivalent to a standard, with a prior estimate of the standard deviation of 2.0 and a clinically significant difference of 1.0, the sample size for each treatment group would be approximately 69 subjects, calculated as N = (2)(2.0)²(1.64 + 1.28)² [57].
Binary Outcomes
For studies with dichotomous response variables, the sample size formula for each treatment group is:
N = (Zα + Zβ)² [PS(1 - PS) + PT(1 - PT)] / d²
Where PS and PT are the event rates for the standard and new treatments, respectively, Zα and Zβ are the standard normal variates corresponding to the α and β error levels, and d is the clinically meaningful difference between treatments [57].
Table 2: Sample Size Requirements for Binary Outcomes (α=0.05, β=0.10) [57]
| PS | PT | d | Sample Size per Group |
|---|---|---|---|
| 0.90 | 0.90 | 0.10 | 155 |
| 0.80 | 0.80 | 0.10 | 217 |
| 0.70 | 0.70 | 0.10 | 256 |
| 0.60 | 0.60 | 0.10 | 272 |
| 0.50 | 0.50 | 0.10 | 263 |
| 0.40 | 0.40 | 0.10 | 229 |
| 0.90 | 0.90 | 0.15 | 70 |
| 0.80 | 0.80 | 0.15 | 98 |
| 0.70 | 0.70 | 0.15 | 115 |
| 0.60 | 0.60 | 0.15 | 123 |
| 0.50 | 0.50 | 0.15 | 119 |
Crossover Designs
AB/BA crossover designs can significantly reduce required sample sizes due to within-subject comparisons. When within-patient correlation ranges from 0.5 to 0.9, crossover trials require only 5–25% as many participants as parallel-group trials to achieve equivalent statistical power [61]. For example, in a study by Ménard et al., a crossover design with alternating active treatment and placebo phases could detect a reduction of 5 mmHg in diastolic blood pressure with only 27 clinic patients, demonstrating the efficiency of this design for equivalence studies [61].
Experimental Protocols and Methodologies
The Two One-Sided Tests (TOST) Procedure
The TOST procedure is the standard method for equivalence testing. For testing equivalence of slope coefficients in linear regression analysis, the null and alternative hypotheses are expressed as:
H₀: β₁ ≤ ΔL or ΔU ≤ β₁ versus H₁: ΔL < β₁ < ΔU
Where ΔL and ΔU are a priori constants representing the minimal range for declaring equivalence [62]. The TOST procedure rejects the null hypothesis at significance level α if:
T_{SL} = (β̂₁ - Δ_L)/(σ̂²/SSX)¹ᐟ² > t_{ν, α} and T_{SU} = (β̂₁ - Δ_U)/(σ̂²/SSX)¹ᐟ² < -t_{ν, α}
Where t{ν, α} is the upper 100·α-th percentile of the t distribution with ν degrees of freedom [62]. This procedure is equivalent to checking whether the ordinary 100(1 - 2α)% equal-tailed confidence interval of the parameter is entirely contained within the equivalence range (ΔL, Δ_U).
Sample Size Determination Protocol
The following workflow illustrates the complete process for determining sample size in equivalence studies:
Practical Implementation Considerations
When implementing sample size calculations for equivalence tests, researchers should:
- Define the smallest effect size of interest (SESOI) prior to data collection based on clinical or practical significance, not statistical considerations [58].
- Account for potential dropouts by inflating the calculated sample size by the expected dropout rate.
- Consider using specialized software such as PASS, PowerTOST, or R packages that include dedicated procedures for equivalence test power analysis [63] [59].
- Plan for both traditional and equivalence test sample size requirements when uncertainty exists about which approach will be most appropriate [58].
For researchers using R, the PowerTOST package provides functions for sample size estimation, assuming two equally sized groups. The estimated sample size represents the total number of subjects, which is always an even number [59].
Research Reagent Solutions: Essential Tools for Equivalence Studies
Table 3: Essential Statistical Tools and Software for Equivalence Test Sample Size Determination
| Tool Name | Primary Function | Key Features | Application Context |
|---|---|---|---|
| PASS Sample Size Software | Comprehensive power analysis | Dedicated equivalence test procedures for various designs | Clinical trials, pharmaceutical research |
| PowerTOST (R Package) | Power and sample size for TOST | Specialized in bioequivalence studies, crossover designs | Pharmacokinetic studies, bioequivalence trials |
| TOSTER (R Package) | Equivalence testing | Implements TOST procedure with various effect sizes | Psychological research, social sciences |
| MBESS (R Package) | Various effect sizes and power | Confidence intervals for effect sizes, power analysis | Behavioral sciences, educational research |
| G*Power | General power analysis | Includes some equivalence test options | Preliminary power calculations, teaching |
| Sealed Envelope Power Calculator | Online power calculation | Continuous outcome equivalence trials | Quick calculations, protocol development |
Common Pitfalls and Best Practices
Avoiding Common Errors
Researchers conducting equivalence studies should be aware of several common pitfalls:
- Inadequate sample size: Using a statistically incorrect sample size may lead to inadequate results in both clinical and laboratory studies, resulting in time loss, cost, and ethical problems [56].
- Confusing non-significance with equivalence: Failure to reject a null hypothesis of no difference does not prove equivalence; this requires a specific equivalence test [58].
- Post-hoc power calculations: Calculating retrospective (post hoc) power after a study is completed is not only futile but plain nonsense [59].
- Inappropriate equivalence margins: Setting margins too wide may claim equivalence for clinically important differences, while overly narrow margins may make the study infeasible [57].
Reporting Guidelines
According to SPIRIT 2025 statement for trial protocols, researchers should transparently report all elements of sample size calculation, including the specific procedure used, all parameters input into calculations, and the assumptions behind those parameters [64]. This promotes reproducibility and allows for critical evaluation of the study design.
Determining appropriate sample size for equivalence tests requires careful consideration of multiple factors, including the equivalence margin, variability in the outcome measure, and the desired power and significance levels. By following rigorous methodological protocols, using specialized software tools, and avoiding common pitfalls, researchers can design equivalence studies with sufficient power to reliably demonstrate equivalence when it truly exists. This is particularly crucial in drug development and model validation research, where incorrect conclusions about equivalence can have significant scientific and clinical implications.
Model misspecification occurs when the statistical model used for analysis does not accurately represent the true data-generating process. This fundamental error in statistical modeling has serious implications for the validity of scientific research, particularly in fields such as drug development and biomedical research where accurate inference is critical. When researchers specify models that incorrectly characterize the relationship between variables, omit relevant parameters, or include unnecessary complexity, they risk compromising both the Type I error rate (falsely rejecting a true null hypothesis) and statistical power (the ability to detect true effects) [65].
The consequences of model misspecification are particularly problematic within hypothesis testing and model performance equivalence research, where the primary goal is to make reliable comparisons between treatments, interventions, or model specifications. Type I error inflation leads to false positive findings, potentially resulting in the adoption of ineffective treatments or incorrect scientific conclusions. Reduced statistical power means that real effects may go undetected, wasting research resources and delaying scientific progress [66] [67]. Understanding these impacts is essential for researchers aiming to produce valid, reproducible findings.
Categorizing Model Misspecification
Model misspecification can manifest in various forms, each with distinct implications for statistical inference. Based on recent methodological research, we can categorize misspecification into several primary types:
- Overspecification: Including unnecessary parameters or complexity in a model, such as adding interaction terms or moderated paths that do not exist in the true data-generating process [68] [69].
- Underspecification: Omitting relevant parameters or necessary complexity from a model, such as excluding important confounding variables or interaction effects [68] [69].
- Complete Misspecification: Using an entirely incorrect model structure that does not reflect the true relationships in the data [68].
- Parameter Misspecification: Incorrectly specifying parameter values in an otherwise correctly structured model, such as using wrong allele frequencies in genetic linkage analysis [70].
The impact of each type varies, with underspecification generally leading to parameter bias and complete misspecification causing the most severe inflation of Type I error rates [68].
Quantitative Evidence: Impact on Type I Error and Power
Evidence from Genetic Linkage Studies
Research in genetic linkage analysis provides compelling quantitative evidence of how parameter misspecification inflates Type I error rates. A simulation study examining the effects of misspecified marker allele frequencies found significant inflation of Type I errors, particularly when parental genotype data was missing [70].
Table 1: Type I Error Inflation in Lod-Score Linkage Analysis with Misspecified Marker Allele Frequencies
| True Allele Frequency | Misspecified Frequency | Nominal α Level | Actual Type I Error Rate | Inflation Factor |
|---|---|---|---|---|
| 0.001 | 0.1 | 0.0001 | 56% | 560× |
| 0.001 | 0.1 | 0.001 | 63% | 63× |
| 0.001 | 0.1 | 0.01 | 72% | 7.2× |
| 0.2 | 0.4 | 0.0001 | 50% | 500× |
This dramatic inflation occurs because misspecification of marker allele frequencies introduces systematic errors in the reconstruction of missing parental genotypes, leading to spurious evidence for linkage [70]. The effect is most pronounced when the frequency of rare alleles is substantially overestimated in the analysis model.
Evidence from Moderated Mediation Research
Recent simulation studies on moderated mediation models (where the strength of a mediation pathway depends on a moderator variable) demonstrate how different types of misspecification affect both Type I error and statistical power [68] [69].
Table 2: Impact of Model Misspecification on Statistical Outcomes in Moderated Mediation
| Misspecification Type | Type I Error Rate | Statistical Power | Parameter Bias |
|---|---|---|---|
| Correctly Specified | Nominal (5%) | 85% (Reference) | <5% |
| Overspecified | 6-8% | 70-75% | <10% |
| Underspecified | 4-7% | 60-65% | 15-25% |
| Completely Misspecified | 12-18% | N/A | 25-40% |
These findings reveal a critical trade-off: while overspecified models show only minor inflation of Type I error rates and acceptable parameter bias, they substantially reduce statistical power. Conversely, underspecified models produce greater parameter bias but less severe impacts on Type I error [68]. Complete misspecification produces the most problematic outcomes, with severely inflated Type I error rates and substantial parameter bias.
Experimental Protocols for Studying Misspecification
Simulation-Based Inference for Misspecification Analysis
Simulation-Based Inference (SBI) has emerged as a powerful framework for studying model misspecification, particularly for complex models where traditional analytical methods are insufficient [71]. The SBI approach uses computational simulations to generate data under known model specifications, then tests how misspecification affects statistical inference.
Core Protocol Elements:
Define Base Model: Specify the complete data-generating process, including all parameters and functional relationships.
Introduce Misspecification: Systematically alter the analysis model by omitting variables, adding unnecessary parameters, or incorrectly specifying functional forms.
Generate Synthetic Data: Use the true data-generating process to create multiple datasets with known properties.
Fit Misspecified Models: Apply the intentionally misspecified analysis models to the synthetic data.
Evaluate Performance: Compare Type I error rates, statistical power, and parameter bias between the correctly specified and misspecified analysis approaches.
This methodology enables researchers to precisely quantify the consequences of specific types of misspecification under controlled conditions [71].
Power Analysis for Measurement Model Misspecification
Structural Equation Modeling (SEM) provides another important experimental framework for investigating misspecification, particularly in the context of measurement models [72]. The protocol involves:
Hypothesis Testing Framework:
- Null Hypothesis (H0): The specified measurement model fits the data exactly.
- Alternative Hypothesis (H1): The specified measurement model does not fit the data exactly.
Experimental Steps:
- Specify both H0 and H1 models, where H1 represents a plausible misspecification (e.g., cross-loadings in factor analysis).
- Calculate the noncentrality parameter difference between H0 and H1 models.
- Compute statistical power based on chi-square difference tests.
- Determine sample size requirements to achieve adequate power (typically 80%) to detect specified levels of misspecification.
For example, research using SF-36 health survey data demonstrated that a sample size of 506 participants was needed to achieve 80% power for detecting medium-sized cross-loadings in a measurement model [72].
Analytical Approaches to Mitigate Misspecification
Model Averaging Techniques
Model averaging presents a promising approach to address model uncertainty and reduce the impacts of misspecification. Rather than relying on a single model, this method combines inferences from multiple plausible models, weighted by their empirical support [40].
Implementation Methods:
- Smooth AIC Weights: Use information criteria (AIC, BIC) to compute model weights based on relative support in the data.
- Bayesian Model Averaging: Combine models using posterior model probabilities approximated through BIC.
- Focused Information Criterion (FIC): Select and average models based on their performance for a specific parameter of interest rather than overall fit.
Simulation studies demonstrate that model averaging maintains better calibration of Type I error rates and more stable power characteristics compared to approaches that rely on selecting a single model [40]. This is particularly valuable in equivalence testing, where misspecification can lead to either inflated Type I errors or overly conservative tests.
Robustness Checks and Sensitivity Analysis
Comprehensive sensitivity analysis provides practical protection against misspecification by evaluating how inferences change under different modeling assumptions [70] [65]. Key elements include:
- Systematic Parameter Variation: Test how results change when key parameters are varied across plausible ranges.
- Alternative Model Specifications: Compare results across different functional forms or covariance structures.
- Missing Data Mechanisms: Evaluate robustness to assumptions about missing data.
- Segregation Analysis: Use automated model-fitting procedures (e.g., REGCHUNT) to estimate trait models from data rather than assuming fixed parameters [70].
Research shows that when trait models are estimated from data using segregation analysis rather than assumed known, Type I error rates are generally closer to nominal levels, even in the presence of marker allele frequency misspecification [70].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Analytical Tools for Misspecification Research
| Tool Category | Specific Solutions | Primary Function | Application Context |
|---|---|---|---|
| Simulation Frameworks | G.A.S.P. V3.3 [70] | Data generation under known models | Genetic studies, general statistical models |
| Custom simulation code [68] | Flexible scenario testing | Methodological research | |
| Analysis Packages | LODLINK [70] | Model-based linkage analysis | Genetic linkage studies |
| lavaan [72] | Structural equation modeling | Measurement models, response shift | |
| power4SEM [72] | Power analysis for SEM | Study planning | |
| Model Comparison Tools | REGCHUNT [70] | Automated segregation analysis | Quantitative trait analysis |
| Evidence functions [65] | Model comparison with error rates decreasing with N | Ecological studies, general applications |
These tools enable researchers to implement the experimental protocols described previously, from initial data generation through final model comparison and inference.
In hypothesis testing for model performance equivalence, researchers and drug development professionals face a fundamental challenge: the selection of a single model from a set of candidates ignores the inherent uncertainty about which model is truly best, potentially leading to overconfident inferences and compromised predictions. Model averaging has emerged as a sophisticated statistical strategy that addresses this dilemma by combining predictions from multiple competing models rather than relying on a single selected model. Within this framework, the method of determining weights for model combination becomes critically important, with Smooth AIC (Akaike Information Criterion) and BIC (Bayesian Information Criterion) weights representing two prominent approaches for frequentist and Bayesian model averaging respectively.
These weighting strategies balance model fit against complexity, with AIC generally favoring models with better predictive accuracy and BIC tending to select simpler models, especially in large samples [73]. The choice between these approaches carries substantial implications for the reliability of conclusions in fields such as clinical trial analysis and drug development, where accurate model specification directly impacts decision-making. This guide provides a comprehensive comparison of these weighting methodologies, supported by experimental data and practical implementation protocols, to equip researchers with evidence-based criteria for selecting appropriate model averaging techniques in performance equivalence research.
Theoretical Foundations: AIC and BIC Weight Calculations
Mathematical Formulations
The foundation of model averaging rests on information criteria that quantify the trade-off between model fit and complexity. Both AIC and BIC evaluate this balance but with different theoretical motivations and penalty structures.
- Akaike Information Criterion (AIC): AIC = 2k - 2ln(L) [73]
- Bayesian Information Criterion (BIC): BIC = ln(n)k - 2ln(L) [73]
Where k represents the number of parameters in the model, L is the maximized likelihood value, and n is the sample size. The key distinction lies in BIC's stronger penalty for model complexity, which increases with sample size, making it more conservative, particularly in large datasets.
From Criteria to Weights
The transformation of these criteria into model weights follows a standardized approach for both frequentist and Bayesian frameworks:
Smooth AIC Weights: ( wi^{AIC} = \frac{\exp(-\frac{1}{2} \Delta AICi)}{\sum{m=1}^M \exp(-\frac{1}{2} \Delta AICm)} ) where ( \Delta AICi = AICi - \min(AIC) )
BIC Weights: ( wi^{BIC} = \frac{\exp(-\frac{1}{2} \Delta BICi)}{\sum{m=1}^M \exp(-\frac{1}{2} \Delta BICm)} ) where ( \Delta BICi = BICi - \min(BIC) )
In Bayesian Model Averaging (BMA), BIC-derived weights approximate posterior model probabilities when using unit prior model probabilities [74]. This connection provides a coherent mechanism for incorporating model uncertainty into inference, where the resulting model is the average of individual models weighted by their posterior probabilities [74].
Comparative Properties of AIC and BIC Weights
Table 1: Fundamental Characteristics of AIC and BIC Weighting Approaches
| Characteristic | Smooth AIC Weights | BIC Weights |
|---|---|---|
| Theoretical Foundation | Information-theoretic (frequentist) | Bayesian approximation |
| Complexity Penalty | Moderate (2k) | Stronger (ln(n)·k) |
| Sample Size Dependency | Independent | Increases with sample size |
| Primary Goal | Predictive accuracy | Identification of "true" model |
| Model Uncertainty | Accounted for through weighting | Quantified via posterior probabilities |
Experimental Evidence: Performance Comparisons Across Domains
Clinical Trial Simulations in Dose Finding
Experimental studies in dose-finding clinical trials have provided robust comparisons between model averaging and traditional model selection approaches. One comprehensive simulation study based on nonlinear mixed effects models characterizing visual acuity in wet age-related macular degeneration patients demonstrated the superiority of model averaging approaches.
Table 2: Performance Comparison in Dose-Finding Clinical Trial Simulations [75] [76]
| Method | Predictive Performance | Dose-Response Characterization | Minimum Effective Dose Definition |
|---|---|---|---|
| Model Selection (AIC) | Baseline | Less accurate | Less precise |
| Model Averaging (AIC weights) | Superior | More accurate | More precise |
| Model Averaging (BIC weights) | Comparable to AIC averaging | Similar improvement | Similar improvement |
The study implemented five different information criteria for weighting, with AIC-based weights demonstrating the best predictive performance overall [75] [76]. This finding underscores the advantage of model averaging in clinical development settings, where accurate characterization of dose-response relationships directly impacts trial success and regulatory decision-making.
Predictive Performance in Healthcare Applications
Further evidence comes from healthcare applications where predictive accuracy is paramount. Research on predicting maximal oxygen uptake (VO2max) in athletes using non-exercise data compared Bayesian Model Averaging with standard variable selection techniques. The BMA approach, which utilizes BIC-derived weights, demonstrated better out-of-sample predictive performance than models selected by conventional frequentist procedures [74]. This performance advantage highlights how accounting for model uncertainty through averaging improves generalization to new data.
The practical implementation involved 272 observations with demographic and anthropometric predictors, with BMA conducted using Occam's window and Markov Chain Monte Carlo Model Composition methods. The consistency of results across these methodological approaches strengthens the evidence for model averaging's predictive benefits [74].
Recent Developments in Uncertainty Quantification
Recent methodological advances have further refined the application of model averaging weights. In 2025, research on conformal prediction intervals for model averaging addressed the critical challenge of quantifying prediction uncertainty when combining models [77]. This framework accommodates both AIC and BIC weighting schemes while providing distribution-free coverage guarantees that remain valid even when all candidate models are misspecified.
This development is particularly relevant for drug development applications where understanding the range of plausible outcomes is as important as point predictions. The approach maintains validity across diverse model averaging methods, including equal-weight combinations, SIC (smooth AIC), MMA (Mallows Model Averaging), and JMA (Jackknife Model Averaging) [77].
Practical Implementation: Protocols and Workflows
Experimental Protocol for Model Averaging in Clinical Trials
Based on the methodological studies reviewed, the following protocol provides a structured approach for implementing model averaging in clinical trial settings:
Define Candidate Model Set: Specify the collection of candidate models based on biological plausibility, clinical relevance, and computational feasibility. For dose-response studies, this typically includes linear, Emax, logistic, and sigmoidal models [75] [76].
Calculate Information Criteria: For each model, compute AIC and BIC values using the standard formulas: AIC = 2k - 2ln(L) and BIC = ln(n)k - 2ln(L) [73].
Compute Model Weights: Transform criteria differences to weights using the exponential transformation and normalization described in Section 2.2.
Generate Weighted Predictions: For parameter estimation or prediction, compute weighted averages across models using the determined weights.
Evaluate Performance: Assess predictive performance using cross-validation or bootstrap methods, focusing on metrics relevant to the research question (e.g., mean squared error for prediction accuracy, coverage probabilities for interval estimates).
Sensitivity Analysis: Conduct robustness checks by comparing results across different weighting schemes (AIC vs. BIC) and examining the impact of prior assumptions in Bayesian implementations.
Workflow Visualization
The following diagram illustrates the logical workflow for implementing model averaging in performance equivalence research:
Weight Calculation Methodology
The transformation from information criteria to model weights follows a specific computational process:
The Scientist's Toolkit: Essential Research Reagents
Implementation of model averaging methods requires both statistical software tools and methodological components. The following table details key "research reagents" for implementing model averaging in hypothesis testing for model performance equivalence.
Table 3: Essential Research Reagents for Model Averaging Implementation
| Tool Category | Specific Tool/Component | Function | Implementation Examples |
|---|---|---|---|
| Statistical Software | R Statistical Environment | Primary platform for model fitting and weight calculation | AIC(model), BIC(model) functions [73] |
| Bayesian Packages | Stan (via RStan, PyStan) | Implements MCMC sampling for Bayesian Model Averaging | Hamiltonian Monte Carlo algorithms [78] |
| Model Averaging Packages | R packages: BMA, AICcmodavg |
Specialized functions for model averaging | bma() function for Bayesian Model Averaging [74] |
| Information Criteria | AIC and BIC formulas | Quantify model fit-complexity tradeoff | AIC = 2k - 2ln(L), BIC = ln(n)k - 2ln(L) [73] |
| Weight Calculation | Exponential transformation | Converts criteria differences to model weights | wi = exp(-Δi/2) / sum(exp(-Δ_m/2)) [73] |
| Performance Validation | Cross-validation methods | Assess predictive performance of averaged models | Leave-one-out, k-fold cross-validation [74] |
The experimental evidence and methodological considerations presented in this guide support several strategic recommendations for researchers engaged in hypothesis testing for model performance equivalence:
In drug development applications such as dose-finding trials, model averaging with AIC weights has demonstrated superior performance for characterizing dose-response relationships and defining minimum effective doses [75] [76]. The predictive accuracy focus of AIC weights makes them particularly suitable for phase II clinical trials where accurate dose selection is critical for subsequent development stages.
For applications requiring model identification or when working with large sample sizes, BIC weights provide a more conservative approach that favors simpler models and more strongly penalizes complexity [73]. The theoretical connection between BIC weights and posterior model probabilities also makes them naturally suited for Bayesian Model Averaging implementations.
Recent advancements in conformal prediction intervals now enable reliable uncertainty quantification for model averaging predictions, addressing a critical gap in frequentist implementations [77]. These methods provide distribution-free coverage guarantees that remain valid under model misspecification, enhancing the robustness of conclusions in regulatory settings.
The choice between Smooth AIC and BIC weights ultimately depends on research objectives, sample size considerations, and philosophical alignment with frequentist or Bayesian paradigms. What remains clear across domains is that accounting for model uncertainty through averaging consistently outperforms approaches that rely on a single selected model, providing more reliable inferences and predictions in model performance equivalence research.
Assessing the impact of prior selection is a critical step in robust Bayesian analysis, especially in research focused on establishing model performance equivalence. This guide compares three established sensitivity analysis techniques, providing the experimental protocols and data you need to implement them effectively.
Comparison of Sensitivity Analysis Techniques
The table below summarizes the core characteristics of three key methods for assessing prior sensitivity.
| Method | Key Principle | Information Provided | Input Dependencies | Resource Requirements |
|---|---|---|---|---|
| Prior Density Ratio Class [79] | Sandwiches priors between lower/upper functional bounds to compute "outer" credible intervals [79]. | Bounds on posterior credible intervals; understanding of prior influence on parameter estimates [79]. | Independent or dependent inputs. | Low; requires only one Markov Chain Monte Carlo (MCMC) chain from the "upper" prior [79]. |
| Sobol' Indices [80] | A global, variance-based method that decomposes output uncertainty into contributions from individual inputs and their interactions [80]. | Intuitive variance-based rankings; insight into interaction effects and individual effect shapes [80]. | Requires independent inputs [80]. | Very high; requires a vast number of model runs, often necessitating an accurate emulator [80]. |
| Multi-Prior Comparison [81] | Directly computes and compares posteriors, model fit, and predictive accuracy for a set of plausible priors [81]. | Direct comparison of parameter estimates, posterior distributions, and model fit criteria (e.g., LOO-IC, WAIC) [81]. | Independent or dependent inputs. | Moderate; requires full MCMC sampling for each specified prior alternative [81]. |
Detailed Experimental Protocols
Protocol 1: Prior Density Ratio Class Analysis
This method is ideal for efficiently exploring a wide range of priors defined by proportional bounds [79].
- Define the Prior Density Ratio Class: Specify a baseline prior density
π_0(θ). Then, define a class of priorsΠwhere each priorπ(θ)satisfiesl(θ) ≤ π(θ)/π_0(θ) ≤ u(θ)for specified lower (l) and upper (u) bound functions [79]. - Compute Outer Credible Intervals: Run a Markov Chain Monte Carlo (MCMC) sampling algorithm only once using the "upper" prior
u(θ) * π_0(θ). Use this single chain to compute "outer" credible intervals for each parameter. These intervals span from the minimum lower bound to the maximum upper bound of the marginal posterior credible intervals obtained from all priors within the defined class [79]. - Analyze Robustness: A small range in the outer credible intervals for a parameter indicates that conclusions about that parameter are robust to the choice of prior within the specified class. A wide range indicates high sensitivity, signaling that the data does not strongly dominate the prior, and the prior choice is influential [79].
Protocol 2: Multi-Prior Comparison for Model Equivalence
This approach is recommended for testing performance equivalence using the Region of Practical Equivalence (ROPE), where confirming robustness is essential [7] [34].
- Specify Alternative Priors: Define a set of plausible priors representing different levels of informativeness and skepticism. For a performance difference parameter
δ, this set should include: - Estimate Posterior Distributions: Conduct full Bayesian estimation for each specified prior, obtaining the posterior distribution for all parameters of interest [81].
- Apply the ROPE Criterion: For each posterior, apply the ROPE to the parameter
δ(e.g.,[-0.1, 0.1]). Decide for or against practical equivalence based on whether the high-density interval of the posterior falls entirely inside, entirely outside, or overlaps the ROPE [7]. - Compare Results Across Priors: Compare the ROPE-based conclusions, posterior estimates, and model fit indices (like LOO-IC or WAIC) across all prior specifications. Consistent conclusions across all priors indicate a robust finding. Conflicting conclusions reveal a sensitivity to prior choice [81].
Experimental Data and Findings
Quantitative Comparison of Method Outcomes
The following table synthesizes hypothetical outcomes from applying these methods to a model equivalence test, illustrating how conclusions can vary.
| Sensitivity Method | Parameter Estimate (Posterior Mean) | 95% Credible Interval | ROPE [-0.1, 0.1] Decision | Conclusion on Robustness |
|---|---|---|---|---|
| Reference Prior | δ = 0.02 | (-0.08, 0.12) | Undecided (overlap) | Baseline |
| Skeptical Prior | δ = 0.01 | (-0.05, 0.07) | Accept Equivalence (inside) | Not Robust: Decision changes. |
| Optimistic Prior | δ = 0.08 | (-0.01, 0.17) | Undecided (overlap) | Partially Robust |
| Density Ratio Bounds | Lower: -0.09, Upper: 0.15 | Outer CI: (-0.11, 0.16) | Decision varies | Not Robust: Wide interval. |
Workflow Diagram: Sensitivity Analysis for Equivalence Testing
The diagram below maps the logical workflow for integrating sensitivity analysis into Bayesian equivalence testing.
The Researcher's Toolkit
Essential software and computational resources for implementing these analyses are listed below.
| Tool / Reagent | Function in Analysis |
|---|---|
| R Statistical Software | Primary platform for Bayesian estimation and sensitivity analysis [79] [81]. |
DRclass R Package |
Specifically supports the implementation of the Prior Density Ratio Class method [79]. |
| Emulator (e.g., BMARS, GP) | A surrogate model that approximates a complex, computationally expensive simulator; essential for methods like Sobol' indices that require thousands of model runs [80]. |
| MCMC Sampling Software (e.g., Stan) | Engine for performing Bayesian inference and drawing samples from the posterior distribution for complex models [81]. |
| Bayesian SEM Software (e.g., blavaan) | For conducting sensitivity analysis within structural equation models, as described in [81]. |
Benchmarking and Validation: Frameworks for Robust Model Comparison and Selection
In the fields of drug development and biomedical research, predictive models are critical tools for decision-making. For decades, researchers have heavily relied on metrics like the coefficient of determination (R²) and Mean Squared Error (MSE) to validate these models. However, a growing body of evidence indicates that these traditional metrics provide an incomplete picture of model performance, particularly when the goal is to demonstrate that a new model is functionally equivalent or non-inferior to an established alternative [82]. The R² value, while useful for quantifying the proportion of variance explained, offers only an average measure of predictive accuracy across an entire dataset, potentially masking significant performance heterogeneity in different patient subgroups or under varying clinical conditions [83].
This article explores the paradigm shift toward formal equivalence testing as a more rigorous framework for validating predictive models. Unlike traditional difference testing, which seeks to reject a null hypothesis of no difference, equivalence testing statistically demonstrates that two models perform similarly within a pre-specified margin of clinical or practical relevance [84] [85]. This approach is especially valuable in drug development for establishing the equivalence of alternative dosing algorithms, demonstrating the non-inferiority of streamlined clinical trial designs, or validating pharmacogenetic models across diverse populations [86]. By moving beyond R² to embrace equivalence testing, researchers and drug development professionals can make more nuanced, evidence-based decisions about model deployment.
The Theoretical Foundation of Equivalence Testing
From Significance to Equivalence: A Paradigm Shift
Traditional null hypothesis significance testing (NHST) operates with a nil null hypothesis (H₀), which typically states that there is no difference between two models' performance (e.g., the difference in their MSE is zero) [2]. A non-significant p-value (p > 0.05) is often misinterpreted as evidence of equivalence, but this is logically flawed. Failure to reject the null hypothesis only indicates insufficient evidence to claim a difference, not positive evidence of similarity [85] [2]. This distinction is critical because studies with small sample sizes or high variance may fail to detect meaningful differences, leading to potentially erroneous conclusions about model equivalence.
Equivalence testing fundamentally reverses this logic. Its null hypothesis (H₀) states that the difference between two models is greater than a clinically or scientifically relevant margin, often denoted as Δ (delta). The alternative hypothesis (H₁) states that the difference lies within this equivalence bound [-Δ, Δ] [84] [2]. Rejecting the null hypothesis in an equivalence test therefore provides direct statistical evidence that the two models perform similarly enough to be considered practically equivalent. This reversal aligns the statistical framework with research questions where demonstrating similarity is the primary objective, such as when validating a simplified predictive model against a more complex gold standard or establishing the consistency of a model's performance across diverse populations [83] [86].
Defining the Equivalence Region (Δ)
The most critical and nuanced step in equivalence testing is specifying the equivalence region or smallest effect size of interest [84] [2]. This pre-specified margin Δ represents the maximum difference in performance that is considered clinically or practically irrelevant. The choice of Δ is not a statistical decision, but a subject-matter decision that requires deep domain expertise.
In pharmacometric modeling, for instance, Δ might be defined based on the known relationship between drug exposure and therapeutic effect [86]. For polygenic risk scores, Δ could be tied to the minimum predictive accuracy needed for clinical utility in risk stratification [83]. When comparing the predictive performance of two models using a metric like MSE or R², Δ must be specified in the same units as that metric. For example, a researcher might specify that two pharmacokinetic models are equivalent if the difference in their prediction errors (MSE) is no greater than 5 mg/L, a value derived from clinical knowledge about the therapeutic window of the drug [86].
Table 1: Approaches for Defining Equivalence Margins in Different Contexts
| Application Area | Performance Metric | Basis for Defining Δ | Example Margin |
|---|---|---|---|
| Pharmacokinetic Modeling | Prediction Error (MSE) | Clinical relevance relative to drug's therapeutic window [86] | Δ = 5 mg/L |
| Polygenic Risk Scores | Incremental R² | Minimum utility for clinical risk stratification [83] | Δ = 0.01 |
| Diagnostic Device Validation | Area Under Curve (AUC) | Acceptable loss in discriminatory capacity [85] | Δ = -0.05 |
| Physical Activity Monitors | Mean Difference | Practical importance in energy expenditure estimation [84] | Δ = 0.65 METs |
Key Methodological Approaches for Equivalence Testing
The Two One-Sided Tests (TOST) Procedure
The most widely established method for equivalence testing is the Two One-Sided Tests (TOST) procedure [84] [2]. The TOST method decomposes the composite null hypothesis of non-equivalence into two separate one-sided hypotheses:
- H₀₁: θ ≤ -Δ (The difference is significantly lower than -Δ)
- H₀₂: θ ≥ Δ (The difference is significantly greater than Δ)
Where θ represents the true difference in performance between the two models (e.g., Model A - Model B). To reject the overall null hypothesis of non-equivalence and conclude equivalence, both H₀₁ and H₀₂ must be rejected at the chosen significance level (typically α = 0.05). This is equivalent to demonstrating that a 90% confidence interval for the difference in performance lies entirely within the pre-specified equivalence bounds [-Δ, Δ] [84]. The following diagram illustrates the TOST procedure and its possible outcomes.
Equivalence Testing for Model Performance Beyond MSE
While traditional metrics like MSE and R² provide valuable summary statistics, a comprehensive equivalence assessment should extend to other performance dimensions, particularly when validating models for clinical applications. Research indicates that evaluating quantile-specific predictive performance can reveal heterogeneity that average measures like R² might obscure [83]. For instance, a polygenic risk score might exhibit varying predictive accuracy across different ranges of a phenotypic distribution due to unmeasured gene-environment interactions, a finding that would be missed by relying solely on overall R² [83].
Similarly, equivalence testing can be applied to model calibration metrics, especially for probabilistic predictions. In these cases, the Brier score (the mean squared error for probabilistic predictions) can be decomposed into resolution and reliability components, providing deeper insight into where and how two models might differ in their calibration performance [82]. A model might show equivalent overall discrimination (AUC) but meaningfully different calibration in clinically critical probability ranges, information essential for informed deployment decisions in medical contexts.
Practical Applications and Experimental Protocols
Case Study: Equivalence Testing for Polygenic Risk Scores
Recent research on polygenic scores (PGS) for 25 continuous traits illustrates the power of moving beyond traditional validation metrics. The study employed quantile regression to estimate how the effect size of a PGS varied across different quantiles of the phenotypic distribution, rather than relying solely on the ordinary least squares (OLS) estimate which provides only an average effect [83]. This approach revealed significant heterogeneity; for body mass index (BMI), the PGS effect size varied from 0.18 at the 5th percentile to 0.60 at the 95th percentile—a more than 3-fold difference that would be completely obscured by a single R² value [83].
Table 2: Selected Results from Quantile Regression Analysis of Polygenic Scores [83]
| Trait | OLS Effect Size (β) | Minimum β (Quantile) | Maximum β (Quantile) | Fold Difference |
|---|---|---|---|---|
| Body Mass Index (BMI) | 0.35 | 0.18 (0.05) | 0.60 (0.95) | 3.33 |
| Height | 0.55 | 0.51 (0.05) | 0.57 (0.85) | 1.12 |
| High-Density Lipoprotein (HDL) | 0.40 | 0.28 (0.05) | 0.56 (0.95) | 2.00 |
| Age at Menopause | 0.23 | 0.17 (0.95) | 0.33 (0.15) | 1.94 |
Protocol for Quantile-Based Equivalence Assessment:
- Data Preparation: Access individual-level data for both the predictive score (e.g., PGS) and the continuous outcome trait in an independent validation cohort.
- Model Specification: For each trait of interest, fit a series of quantile regression models at predetermined quantiles (e.g., τ = 0.05, 0.15, ..., 0.95). The model is specified as: Qᵢ(τ) = β₀(τ) + β₁(τ) × PGS, where Qᵢ(τ) is the τ-th quantile of the phenotypic distribution [83].
- Effect Size Estimation: Extract the quantile-specific effect sizes β₁(τ) and their confidence intervals from each fitted model.
- Equivalence Testing: Define an equivalence margin for effect size variation (e.g., a 1.2-fold difference from the OLS estimate). Test whether the ratio of max(β₁(τ)) to min(β₁(τ)) falls within this margin across the phenotypic distribution.
- Interpretation: Traits with ratio statistics exceeding the equivalence margin indicate heterogeneous predictive performance, suggesting the PGS performs substantially differently in subpopulations defined by their position in the phenotypic distribution [83].
Case Study: Pharmacometric Model Validation
In drug development, the US Food and Drug Administration (FDA) has advocated for the use of model-based drug development, creating a need for robust model validation techniques. One study demonstrated the use of an equivalence-based metric (peqv) for predictive checks during covariate model qualification in pharmacokinetic modeling [86]. The research simulated concentration-time data for 25 men and 25 women, assuming a 5-fold higher typical clearance in men. It then compared the predictive performance of a true model (which correctly accounted for this sex difference) against a false model (which ignored it) [86].
The key finding was that traditional predictive p-values (Pp) calculated using sum of squared errors as a discrepancy variable failed to reliably reject the false model. In contrast, the equivalence-based probability metric (peqv) successfully distinguished the models, particularly for concentrations at later time points (4 hours) that are primarily determined by clearance [86]. For the concentration at 4 hours, the true model showed peqv values of 0.65-0.80, while the false model showed values of 0.35-0.50, demonstrating the superior discriminatory power of the equivalence-based approach for identifying misspecified models [86].
The Researcher's Toolkit for Equivalence Testing
Implementing robust equivalence testing for predictive models requires both statistical knowledge and practical tools. The following table details key methodological "reagents" essential for conducting these analyses.
Table 3: Essential Methodological Reagents for Equivalence Testing of Predictive Models
| Tool / Concept | Category | Function/Purpose | Example Implementation |
|---|---|---|---|
| Equivalence Margin (Δ) | Study Design | Defines the maximum acceptable difference in performance that is still considered clinically/practically irrelevant [84]. | Δ = 0.1 for a difference in AUC; Δ = 0.5 for a difference in MSE. |
| TOST Procedure | Statistical Test | The standard method for testing equivalence by performing two one-sided tests against the upper and lower equivalence bounds [84] [2]. | tost() function in R's equivalence package; TOST meta-analyses in JASP. |
| Quantile Regression | Modeling Technique | Assesses whether a predictor's relationship with the outcome is constant across the entire distribution of the outcome, revealing heterogeneity [83]. | quantreg package in R; QUANTREG procedure in SAS. |
| Confidence Interval (90%) | Inference | Used in conjunction with TOST; if the 90% CI for the difference falls entirely within [-Δ, Δ], equivalence is declared at α=0.05 [84]. | Standard output of statistical software for mean differences and regression coefficients. |
| Power Analysis for TOST | Sample Planning | Determines the sample size required to have a high probability (e.g., 80%) of correctly concluding equivalence when the models are truly equivalent [84]. | power.t.test() in R with type="paired" and alternative="one.sided"; G*Power software. |
| Probability of Equivalence (peqv) | Performance Metric | An equivalence-based metric for model qualification that can be more informative than significance-based p-values for rejecting false models [86]. | Custom calculation based on the proportion of replicated data falling within a specified interval of the original data. |
Implementing an Equivalence Testing Framework: A Practical Workflow
Transitioning from traditional difference testing to an equivalence framework requires a systematic approach. The following workflow diagram and accompanying explanation provide a roadmap for researchers implementing equivalence testing in predictive model validation.
Phase 1: Pre-Study Planning (Steps 1-2) Before analyzing any data, clearly define the study context and the rationale for wanting to demonstrate equivalence (e.g., validating a simplified model, establishing consistency across populations). Then, specify the equivalence margin (Δ) based on clinical or practical considerations, not statistical convenience. This is the most critical step and requires input from domain experts [84] [85].
Phase 2: Data Collection and Analysis (Steps 3-5) Collect a sufficiently large validation dataset. Conduct a power analysis for the TOST procedure to ensure the study can detect equivalence if it exists. Calculate the relevant performance metrics for both the new and reference models, then perform the TOST procedure or construct the appropriate confidence interval [84] [2].
Phase 3: Interpretation and Reporting (Step 6) If the 90% confidence interval for the performance difference lies entirely within [-Δ, Δ], conclude statistical equivalence. Report not only the p-values but also the point estimate and confidence interval, and discuss the practical implications of the findings in the specific application context [84] [85].
The validation of predictive models in drug development and biomedical research requires a more nuanced approach than provided by traditional metrics like R². Equivalence testing, particularly through methods like the TOST procedure, offers a statistically rigorous framework for demonstrating that two models perform similarly enough for practical purposes. The case studies in pharmacometrics and polygenic risk scores illustrate how this approach can reveal critical information about model performance that would be obscured by traditional validation strategies.
As predictive models play increasingly important roles in clinical decision-making and drug development, adopting more sophisticated validation frameworks becomes imperative. By moving beyond R² to implement formal equivalence tests, researchers can provide stronger evidence for model utility, leading to more reliable and transparent decision-making in biomedical research and patient care.
In the field of machine learning and data science, evaluating the performance of multiple classification algorithms on a single dataset is a common yet statistically complex task. When moving beyond simple comparisons between two classifiers, researchers require robust statistical frameworks to determine whether observed performance differences are statistically significant or merely due to random chance. This guide explores the application of Analysis of Variance (ANOVA) and post-hoc tests for comparing multiple classifiers, providing a rigorous methodological approach for researchers, scientists, and drug development professionals who need to validate model performance equivalence in high-stakes research environments.
The fundamental challenge in comparing multiple classifiers lies in controlling Type I errors (false positives) that accumulate when performing multiple pairwise comparisons. While a simple t-test suffices for comparing two classifiers, it becomes inadequate and misleading when applied to multiple classifiers due to error rate inflation [87] [88]. This guide presents a hierarchical testing approach that begins with an omnibus test (ANOVA) to detect any differences among classifier groups, followed by specialized post-hoc procedures to identify exactly which classifiers differ while maintaining the prescribed family-wise error rate.
Theoretical Framework: Hypothesis Testing for Multiple Classifiers
The Hierarchical Testing Approach
The statistical comparison of multiple classifiers follows a structured, two-stage process designed to control error rates while identifying specific performance differences. This hierarchical approach begins with an omnibus test that assesses whether any statistically significant differences exist among the group means. If this initial test reveals significant results, the analysis proceeds to post-hoc tests that pinpoint exactly which classifiers differ from each other [89].
The null and alternative hypotheses for the omnibus test in classifier comparison are:
- Null Hypothesis (H₀): All classifier performance means are equal (μ₁ = μ₂ = μ₃ = ... = μ₋k)
- Alternative Hypothesis (H₁): At least one classifier's mean performance is significantly different from the others [90] [87]
This hierarchical procedure is predicated on the assumption that a significant omnibus test implies at least one significant pairwise comparison, though in practice, discrepancies can occur [89]. The procedure is taught in basic and advanced statistics courses and is implemented in many popular statistical packages.
Key Statistical Concepts
Family-Wise Error Rate
The family-wise error rate (FWER), also known as the experiment-wise error rate, represents the probability of making at least one Type I error (false positive) when conducting multiple hypothesis tests [87]. As the number of comparisons increases, this error rate grows substantially, as shown in Table 1.
Table 1: Family-Wise Error Rate Expansion with Multiple Comparisons
| Number of Groups | Number of Pairwise Comparisons | Family-Wise Error Rate (α=0.05) |
|---|---|---|
| 2 | 1 | 0.05 |
| 3 | 3 | 0.14 |
| 4 | 6 | 0.26 |
| 5 | 10 | 0.40 |
| 6 | 15 | 0.54 |
The formula for calculating the maximum number of comparisons for N groups is: (N*(N-1))/2, while the family-wise error rate is calculated as 1 - (1 - α)^C, where α is the significance level for a single comparison and C equals the number of comparisons [88].
Effect Sizes in Classifier Comparison
In classifier comparison, differences between group means represent unstandardized effect sizes because these values indicate the strength of the relationship using the natural units of the dependent variable (e.g., accuracy, F1-score, or AUC-ROC). Effect sizes help researchers understand the practical significance of their findings beyond mere statistical significance [88].
Experimental Design and Methodological Considerations
Recommended Experimental Protocol
When designing experiments to compare multiple classifiers, researchers should adhere to the following protocol to ensure statistically valid and reproducible results:
Performance Measurement Collection: For each classifier, collect performance metrics (e.g., accuracy, precision, recall, F1-score, AUC-ROC) using appropriate resampling methods such as repeated k-fold cross-validation. The paired design is crucial, where all classifiers are evaluated on the same data splits to reduce variance [91] [92].
Assumption Checking: Before conducting ANOVA, verify that the data meet the necessary assumptions:
- Independence of observations: Each data point should be independent of others
- Normality: The performance metrics within each classifier group should follow a normal distribution
- Homogeneity of variances: The variation in scores across all classifier groups should be roughly equal [90]
Omnibus Test Execution: Conduct a repeated measures ANOVA, which is appropriate for comparing more than two classifiers on a single domain since the data (performance measures) are paired through evaluation on the same cross-validation folds [92].
Post-Hoc Analysis: If the omnibus test is statistically significant (typically p < 0.05), proceed with post-hoc tests to identify which specific classifiers differ while controlling the family-wise error rate.
Effect Size Reporting: Report both statistical significance and effect sizes (mean differences between classifiers) to provide a complete picture of performance differences.
Research Reagent Solutions for Classifier Comparison
Table 2: Essential Tools for Statistical Comparison of Classifiers
| Research Tool | Function | Application Context |
|---|---|---|
| Repeated Measures ANOVA | Tests for overall differences between multiple classifiers on same dataset | Omnibus testing for classifier performance comparison |
| Tukey's HSD Test | Controls family-wise error rate for all pairwise comparisons | Post-hoc analysis when comparing all classifiers to each other |
| Holm's Method | Sequentially rejects hypotheses while controlling FWER | Conservative post-hoc testing with strong error control |
| Bonferroni Correction | Adjusts significance level by number of tests | Simple but conservative adjustment for multiple comparisons |
| Dunnett's Correction | Compares each treatment to a single control | Post-hoc testing when comparing against a baseline classifier |
| F-statistic | Ratio of between-group to within-group variance | Determining significance in ANOVA |
ANOVA for Classifier Performance Comparison
The ANOVA Framework
Analysis of Variance (ANOVA) is a statistical method that extends the t-test to accommodate multiple groups, making it ideal for comparing several classifiers simultaneously [91] [93]. The fundamental principle behind ANOVA is partitioning the total variability in performance measurements into components attributable to different sources.
In the context of classifier comparison, the key variance components are:
- Between-Group Variance (SSB): Variability in performance scores between different classifiers (the "signal")
- Within-Group Variance (SSW): Variability in performance scores within the same classifier (the "noise")
The F-ratio is calculated as the ratio of between-group variance to within-group variance:
F = MSB / MSW
where MSB is the mean square between groups and MSW is the mean square within groups [90] [93]. A larger F-ratio indicates that the between-group variability is substantial compared to the within-group variability, suggesting that classifier performance differs more than would be expected by chance alone.
Workflow for Classifier Comparison Using ANOVA
The following diagram illustrates the complete statistical testing workflow for comparing multiple classifiers:
Calculation Steps for One-Way ANOVA
The computational process for ANOVA involves several key steps:
- Calculate Group Means: Compute the mean performance for each classifier
- Calculate Overall Mean: Compute the grand mean across all classifiers
Calculate Sum of Squares:
- Total Sum of Squares (SST): Sum of squared differences between each observation and the grand mean
- Between-Group Sum of Squares (SSB): Sum of squared differences between group means and grand mean, weighted by group size
- Within-Group Sum of Squares (SSW): Sum of squared differences between each observation and its group mean [90] [93]
Calculate Mean Squares:
- MSB = SSB / (k - 1), where k is the number of classifiers
- MSW = SSW / (N - k), where N is the total number of observations
Compute F-statistic: F = MSB / MSW
The resulting F-statistic is compared to a critical value from the F-distribution with (k-1, N-k) degrees of freedom to determine statistical significance [90].
Post-Hoc Analysis for Classifier Comparison
Purpose and Rationale of Post-Hoc Tests
When the omnibus ANOVA test rejects the null hypothesis, it indicates that not all classifier performances are equal, but it does not identify which specific pairs of classifiers differ significantly [87] [88]. Post-hoc tests address this limitation by performing multiple pairwise comparisons between classifiers while controlling the family-wise error rate.
These specialized procedures adjust significance levels to account for the multiple testing problem, ensuring that the probability of at least one false positive across all comparisons remains at the desired level (typically 0.05). Without such adjustments, the chance of false discoveries increases substantially with the number of comparisons, as illustrated in Table 1.
Commonly Used Post-Hoc Tests
Tukey's Honest Significant Difference (HSD) Test
Tukey's HSD is the most commonly used post-hoc test when researchers want to examine all possible pairwise comparisons between classifiers [87] [88]. The test uses the studentized range distribution to determine critical values for determining whether mean differences exceed what would be expected by chance.
The test statistic for Tukey's HSD is:
HSD = qₐ × √(MSW / n)
where qₐ is the critical value from the studentized range distribution, MSW is the mean square within from the ANOVA, and n is the sample size per group. Tukey's test provides simultaneous confidence intervals for all pairwise differences, with the property that the probability that all intervals contain the true parameters is 1-α.
Holm's Sequential Procedure
Holm's method is a step-down procedure that is more powerful than the classic Bonferroni correction while still controlling the family-wise error rate [87]. The method works as follows:
- Order the p-values from all pairwise comparisons from smallest to largest: p₁ ≤ p₂ ≤ ... ≤ pₘ
- Compare the smallest p-value to α/m, the next smallest to α/(m-1), and so forth
- Continue until a non-significant result is found, at which point all remaining larger p-values are declared non-significant
Holm's method is considered a good choice when the number of comparisons is moderate and researchers want to balance statistical power with strong error control.
Dunnett's Correction
Dunnett's correction is specialized for situations where multiple classifiers are compared to a single baseline or control classifier, rather than comparing all classifiers to each other [87]. This is common in classifier evaluation when a new proposed algorithm is compared against several existing baseline methods.
Dunnett's test modifies the critical t-value to account for the multiple comparisons to a common control, providing greater power for these specific comparisons than Tukey's test, which allows all possible pairwise comparisons.
Interpretation of Post-Hoc Test Results
Table 3: Comparison of Post-Hoc Tests for Classifier Evaluation
| Test Method | Comparisons | Error Rate Control | Statistical Power | Use Case |
|---|---|---|---|---|
| Tukey's HSD | All pairwise | Strong FWER control | Moderate | Comprehensive comparison of all classifier pairs |
| Holm's Method | All pairwise | Strong FWER control | High | Balanced approach for multiple comparisons |
| Bonferroni | All pairwise | Very strong FWER control | Low | Highly conservative error control |
| Dunnett's | Treatment vs control only | Strong FWER control | High for vs control | Comparing multiple classifiers to a baseline |
Post-hoc tests typically present results in two formats: adjusted p-values and simultaneous confidence intervals. Adjusted p-values can be compared directly to the significance level (e.g., 0.05), with values below the threshold indicating statistical significance. Simultaneous confidence intervals that exclude zero likewise indicate significant differences [88].
For example, in a four-classifier comparison (A, B, C, D), Tukey's test might yield the following results:
Table 4: Example Post-Hoc Results for Classifier Comparison (Fictional Data)
| Pairwise Comparison | Mean Difference | Adjusted P-value | 95% Simultaneous CI Lower | 95% Simultaneous CI Upper |
|---|---|---|---|---|
| B - A | 0.282 | 0.572 | -0.293 | 0.857 |
| C - A | 0.856 | 0.001 | 0.281 | 1.431 |
| D - A | 1.468 | <0.001 | 0.893 | 2.042 |
| C - B | 0.574 | 0.051 | -0.001 | 1.149 |
| D - B | 1.185 | <0.001 | 0.611 | 1.760 |
| D - C | 0.611 | 0.033 | 0.037 | 1.186 |
In this example, classifiers C and D perform significantly better than A, while D also performs significantly better than B. The difference between C and B approaches but does not quite reach statistical significance at the 0.05 level [87].
Practical Application in classifier Performance Analysis
Implementation Considerations
When implementing ANOVA and post-hoc tests for classifier comparison, several practical considerations emerge:
Data Structure Requirements: Performance measurements should be structured such that each row represents a performance measurement (e.g., from a cross-validation fold) with columns indicating the classifier used and the performance metric value.
Violations of Assumptions: When ANOVA assumptions are violated, alternatives should be considered. For non-normal data, transformations or non-parametric alternatives like the Friedman test may be appropriate. For unequal variances, Welch's ANOVA or the Games-Howell post-hoc test can be used.
Software Implementation: Most statistical software packages (R, Python, SPSS, SAS) implement ANOVA and post-hoc tests. In R, the aov() function performs ANOVA, while TukeyHSD() conducts Tukey's post-hoc test. The pairwise.t.test() function with the p.adjust.method parameter implements various p-value adjustments including Holm's method [87].
Reporting Guidelines
Comprehensive reporting of classifier comparison results should include:
- Descriptive statistics: Means and standard deviations for each classifier's performance
- ANOVA results: F-statistic, degrees of freedom, and p-value from the omnibus test
- Effect sizes: Mean differences between classifiers with confidence intervals
- Post-hoc results: Adjusted p-values or simultaneous confidence intervals for important pairwise comparisons
- Assumption checks: Information about how ANOVA assumptions were verified
This comprehensive approach to classifier comparison provides researchers with a statistically sound framework for making confident conclusions about algorithm performance, supporting the development of more effective and reliable machine learning systems in research and industry applications.
In the realm of statistical inference, particularly within high-stakes fields like pharmaceutical development, the need to demonstrate the absence of a meaningful effect is as important as proving the existence of one. Equivalence testing provides a formal statistical framework for this purpose, allowing researchers to confirm that two treatments or conditions are practically indistinguishable. This comparative analysis examines the two dominant statistical paradigms for equivalence testing—frequentist and Bayesian approaches—evaluating their respective performance on key operational characteristics including statistical power, Type I error control, and interpretability of results. As noted in methodological literature, "Equivalence tests, otherwise known as parity or similarity tests, are frequently used in 'bioequivalence studies' to establish practical equivalence rather than the usual statistical significant difference" [94]. Within this context, we explore how each methodology approaches the fundamental challenge of testing interval hypotheses rather than traditional point null hypotheses.
Theoretical Foundations
The Framework of Equivalence Testing
Traditional null hypothesis significance testing (NHST) faces significant limitations when the research goal is to support the absence of an effect. A common misconception is that a non-significant p-value (p > 0.05) provides evidence for the null hypothesis [25]. However, as Lakens notes, "It is statistically impossible to support the hypothesis that a true effect size is exactly zero. What is possible in a frequentist hypothesis testing framework is to statistically reject effects large enough to be deemed worthwhile" [25]. Equivalence testing addresses this limitation by essentially reversing the conventional hypothesis structure, testing whether an effect is smaller than the smallest effect size of interest (SESOI).
Equivalence tests employ interval hypotheses rather than point hypotheses. The establishment of an equivalence region (also known as the region of practical equivalence or ROPE) represents a crucial step that requires careful consideration of contextual, theoretical, and practical factors [2]. This approach originated in pharmaceutical sciences, particularly in bioequivalence trials, but has since expanded to various scientific disciplines including psychology, economics, and political science [29].
Frequentist Approach: The Two One-Sided Tests (TOST) Procedure
The most widely established frequentist approach to equivalence testing is the Two One-Sided Tests (TOST) procedure, first formalized by Schuirmann [29] [2]. In TOST, researchers specify an upper (ΔU) and lower (-ΔL) equivalence bound based on the smallest effect size of interest. The procedure tests two composite null hypotheses:
- H01: Δ ≤ -ΔL
- H02: Δ ≥ ΔU
When both null hypotheses can be rejected at the chosen significance level (typically α = 0.05), researchers can conclude that -ΔL < Δ < ΔU, meaning the observed effect falls within the equivalence bounds and can be considered practically equivalent [25] [29]. The TOST procedure can be visualized through confidence intervals: "To conclude equivalence, the 90% CI around the observed mean difference should exclude the ΔL and ΔU values" [25]. This dual requirement ensures that the test establishes equivalence with a maximum Type I error rate of 5%.
Bayesian Alternatives
Bayesian equivalence testing offers several alternative frameworks, with the two most prominent being:
Bayesian ROPE (Region of Practical Equivalence): The ROPE approach defines a range of parameter values that are considered practically equivalent to the null value. Researchers then calculate the posterior probability that the parameter lies within this region [7]. Decisions are typically made based on whether a specified percentage (e.g., 95%) of the posterior distribution falls within the ROPE [95].
Bayes Factors for Interval Hypotheses: This approach computes the ratio of marginal likelihoods under the alternative hypothesis (defined as the equivalence region) and the null hypothesis (effects outside the equivalence region) [95]. The resulting Bayes factor quantifies the strength of evidence for equivalence relative to non-equivalence.
A key differentiator of Bayesian methods is their incorporation of prior knowledge through prior distributions, which can potentially improve efficiency when relevant prior information is available [95].
Comparative Performance Analysis
Statistical Power and Type I Error Control
The performance characteristics of frequentist and Bayesian equivalence tests have been systematically examined through simulation studies. Kelter found that "the proposed Bayesian tests achieve better type I error control at slightly increased type II error rates" compared to frequentist counterparts [96]. This trade-off between Type I and Type II error control represents a fundamental consideration in test selection.
For the frequentist TOST procedure, both power and Type I error rates are determined by sample size, effect size, and equivalence margin specifications. The procedure provides guaranteed error control when its assumptions are met, with the advantage of being mathematically straightforward to compute [25].
Bayesian tests demonstrate particular sensitivity to prior specification. As Kelter notes, "The relationship between type I error rates, power and sample sizes for existing Bayesian equivalence tests is identified in the two-sample setting" [95], highlighting that prior selection can influence both Type I error rates and power, sometimes in opposite directions for different Bayesian tests [95]. Under certain prior specifications, Bayesian tests can achieve superior power compared to frequentist approaches. Ochieng observed that "for certain specifications of the prior parameters, test based on these posterior probabilities are more powerful and less conservative than those based on the p-value" [94].
Table 1: Comparative Performance Characteristics of Frequentist and Bayesian Equivalence Tests
| Performance Metric | Frequentist TOST | Bayesian ROPE | Bayes Factor |
|---|---|---|---|
| Type I Error Control | Fixed at specified α (typically 0.05) | Varies with prior specification; can achieve better control than TOST [96] | Depends on prior choices and stopping rules |
| Statistical Power | Determined by sample size and effect size; may be less powerful for certain parameter values [94] | Can be more powerful than TOST with appropriate priors [94] | Sensitivity to prior modeling affects power [95] |
| Sample Size Planning | Required for adequate power; relies on potentially unverifiable assumptions [29] | No minimum sample size requirement; better scalability [7] | Optional stopping possible without inflating Type I error [95] |
| Sensitivity to Prior | Not applicable | High sensitivity; prior selection crucial for performance [95] | High sensitivity; reverse relationship for Type I error and power possible [95] |
Interpretation and Practical Implementation
The interpretation of results differs substantially between the two paradigms. Frequentist TOST yields a dichotomous decision: either reject both null hypotheses and claim equivalence, or fail to do so. The accompanying p-values indicate whether the data are surprising under the assumption that the true effect lies outside the equivalence bounds [25].
Bayesian methods provide more direct probabilistic interpretations. The ROPE approach yields the probability that the parameter lies within the equivalence region given the observed data [7]. Similarly, Bayes factors quantify the strength of evidence for equivalence relative to non-equivalence [95]. These probabilistic statements are often more intuitive for stakeholders, as they directly address the question of interest [97].
In practical implementation, Bayesian methods offer flexibility regarding optional stopping—the practice of monitoring data and potentially stopping a study early based on interim results. Unlike frequentist methods, where optional stopping can inflate Type I error rates, "Bayesian tests follow the likelihood principle which itself implies the stopping rule principle" [95]. This means that Bayesian results are not influenced by researchers' intentions about when to stop collecting data, a substantial advantage in sequential testing scenarios [95] [96].
Table 2: Practical Implementation Considerations
| Implementation Factor | Frequentist TOST | Bayesian Approaches |
|---|---|---|
| Result Interpretation | Dichotomous decision based on p-values; confidence intervals | Direct probabilities about parameters; evidence ratios |
| Optional Stopping | Problematic without special adjustments; inflates Type I error | Permitted without methodological consequences [95] |
| Software Availability | Widely available in standard packages (e.g., Minitab [98]) | Requires specialized Bayesian packages or programming |
| Stakeholder Communication | Familiar framework for regulatory settings [97] | Intuitive probability statements but requires prior justification |
| Regulatory Acceptance | Well-established in pharmaceutical industry [29] | Growing but less standardized acceptance |
Experimental Protocols and Methodologies
Standard Experimental Setup for Comparison Studies
Methodological comparisons between frequentist and Bayesian equivalence tests typically employ Monte Carlo simulation studies. These studies systematically vary factors including sample size, true effect size, equivalence margins, and prior distributions to evaluate test performance across diverse scenarios [95] [96].
A typical simulation protocol involves:
Data Generation: Simulate datasets under various true effect sizes, including values within the equivalence region (to assess power) and outside the equivalence region (to assess Type I error rates) [96].
Test Application: Apply both frequentist TOST and Bayesian equivalence tests (ROPE and Bayes factor) to each simulated dataset.
Performance Metrics Calculation: Compute empirical Type I error rates and power for each method across simulation conditions.
Prior Sensitivity Analysis: For Bayesian methods, evaluate how different prior specifications affect performance metrics [95].
Example Simulation Specification
For a two-group comparison with continuous outcomes, the data generation process typically follows:
- Model: Y₁i ∼ N(μ₁, σ²), Y₂j ∼ N(μ₂, σ²) for i = 1,...,n₁, j = 1,...,n₂
- Equivalence Margin: Specify ΔL = -δ and ΔU = δ, where δ represents the smallest effect size of interest, often expressed in standardized units (Cohen's d)
- True Effect Size: Varied across simulations from -δ to δ to evaluate power, and beyond ±δ to evaluate Type I error rates
- Sample Size: Varied from small (n = 20 per group) to large (n = 200 per group)
Essential Research Reagents
Table 3: Essential Methodological Components for Equivalence Testing Research
| Component | Function | Implementation Considerations |
|---|---|---|
| Smallest Effect Size of Interest (SESOI) | Defines the equivalence margin; effects smaller than SESOI are considered practically irrelevant | Should be specified based on theoretical, clinical, or practical considerations prior to data collection [25] |
| Statistical Software | Performs equivalence test calculations and simulations | R, Python, or specialized software (e.g., JASP, Minitab [98]); Bayesian methods often require MCMC sampling |
| Prior Distributions | Incorporate existing knowledge in Bayesian analyses | Choice between informative, weakly informative, or default priors; sensitivity analysis crucial [95] |
| Power Analysis Tools | Determine sample requirements for frequentist TOST | Requires specification of expected effect size, equivalence margin, and variability estimates [25] |
| Visualization Methods | Communicate equivalence test results | Equivalence plots with confidence/credible intervals and equivalence bounds [98] |
Conceptual Framework and Decision Pathways
The fundamental logical structure of equivalence testing differs between frequentist and Bayesian paradigms, as illustrated in the following decision pathways:
Diagram 1: Decision Pathways for Frequentist and Bayesian Equivalence Tests
Both frequentist and Bayesian approaches to equivalence testing offer distinct advantages and limitations that make them suitable for different research contexts. The frequentist TOST procedure provides a well-established, transparent framework with guaranteed error control when properly applied, making it particularly valuable in regulatory settings such as pharmaceutical development [29]. Its straightforward implementation and interpretation have contributed to its widespread adoption across scientific disciplines.
Bayesian equivalence tests offer enhanced flexibility, particularly through their ability to incorporate prior knowledge and accommodate optional stopping without methodological penalties [95]. The direct probabilistic interpretation of results—such as the probability that a parameter lies within a region of practical equivalence—often aligns more closely with researchers' intuitive questions [7]. However, this comes at the cost of additional complexity in prior specification and potential sensitivity of results to these prior choices [95].
For researchers selecting between these approaches, considerations of context, constraints, and goals should guide the decision. In high-stakes, regulated environments with established effect size thresholds, frequentist TOST often remains the preferred approach due to its transparency and error control properties. In exploratory research settings, where sequential monitoring is valuable and relevant prior information exists, Bayesian methods may offer efficiency advantages and more intuitive interpretations.
The continuing methodological development in both paradigms suggests an increasingly sophisticated toolkit for researchers seeking to demonstrate the absence of meaningful effects—a crucial capability for scientific progress across diverse fields from pharmaceutical development to psychology and beyond.
The Hodges-Lehmann paradigm represents a fundamental shift in statistical reasoning for biomedical research, moving from traditional point null hypothesis testing to interval-based equivalence testing. This framework addresses critical limitations of null hypothesis significance testing (NHST), which suffers from interpretational problems and the inevitable rejection of trivial effects with large sample sizes. The Hodges-Lehmann estimator provides a robust, nonparametric approach for estimating location parameters and effect sizes, offering substantial advantages through its median-unbiasedness, high breakdown point, and natural alignment with interval hypothesis testing. This review systematically compares the performance of Hodges-Lehmann methods against traditional alternatives across multiple biomedical applications, demonstrating their superiority in testing practical equivalence, handling non-normal data, and providing clinically interpretable effect size measures. Empirical evidence from clinical trials, biomarker studies, and therapeutic equivalence research confirms that Hodges-Lehmann methods maintain robust performance where conventional parametric tests fail, establishing this paradigm as an essential framework for next-generation biomedical statistics.
Null hypothesis significance testing (NHST) dominates biomedical research despite profound methodological limitations that impede scientific progress. The standard practice of testing precise point null hypotheses (e.g., H₀: δ = 0) presents logical contradictions in most biomedical contexts, as exact equality of effects between treatments rarely occurs in reality [95]. This fundamental mismatch between statistical methodology and biomedical reality leads to several critical problems: inflated type I error rates, inability to leverage optional stopping rules, problematic interpretation of censored data, and inevitable rejection of trivial effects with sufficiently large sample sizes [95] [34]. These limitations violate the likelihood principle, a cornerstone of statistical inference, and diminish the reliability of biomedical research findings.
The Hodges-Lehmann paradigm addresses these limitations through a fundamental reconceptualization of statistical testing. Originally developed for estimating location parameters, the Hodges-Lehmann estimator provides a robust, nonparametric approach based on rank statistics that naturally extends to interval hypothesis testing [99]. This approach shifts focus from testing "no effect" to testing "negligible effect" through interval hypotheses that define a range of clinically equivalent values, offering a more realistic framework for biomedical research where some treatment effect—however small—almost always exists [95] [34]. The Hodges-Lehmann framework aligns with the increasing emphasis on equivalence testing in therapeutic development, comparative effectiveness research, and biomarker validation, where demonstrating similarity rather than difference is often the primary scientific objective.
Theoretical Foundations of the Hodges-Lehmann Framework
Statistical Properties and Formulations
The Hodges-Lehmann estimator possesses several theoretical properties that make it particularly suitable for biomedical applications. For univariate populations symmetric about their median, it provides a consistent and median-unbiased estimate of the population median [99]. For asymmetric populations, it estimates the pseudo-median, which closely approximates the population median while maintaining desirable statistical properties. The estimator demonstrates remarkable robustness with a breakdown point of 0.29, meaning it remains statistically valid even when nearly 30% of the data contain contamination or outliers [99]. This represents a substantial advantage over traditional mean-based estimators, which have a breakdown point of zero.
The mathematical formulation of the Hodges-Lehmann estimator varies according to the specific application context:
- One-sample case: For a dataset with n measurements, the estimator is defined as the median of all pairwise averages:
HL = median{(xᵢ + xⱼ)/2}for all i ≤ j [99] - Two-sample case: For two datasets with m and n observations, the estimator of location difference is the median of all m × n pairwise differences:
HL = median{xᵢ - yⱼ}[99] - Censored data: For right-censored time-to-event data, the estimator can be adapted using the Gehan generalization of the Mann-Whitney-Wilcoxon test [100]
The theoretical superiority of Hodges-Lehmann methods extends to optimality considerations. Research has demonstrated that tests derived from this framework satisfy Hodges-Lehmann optimality conditions across diverse statistical contexts, including testing moment conditions and overidentifying restrictions [101]. This optimality represents a global efficiency property that complements the local efficiency of traditional likelihood-based methods, particularly valuable when evaluating performance against fixed alternatives rather than local perturbations.
Connection to Interval Hypothesis Testing
The Hodges-Lehmann framework provides a natural foundation for interval hypothesis testing through its inherent connection to confidence interval construction. Rather than testing a precise null value, interval hypotheses evaluate whether a parameter lies within a predetermined equivalence region representing clinically irrelevant effect sizes [95] [34]. This approach acknowledges that treatments may differ trivially while remaining practically equivalent, a recognition absent from traditional point null testing.
Bayesian extensions of the Hodges-Lehmann approach further enhance its utility for equivalence testing. The Bayesian Hodges-Lehmann test incorporates prior information while maintaining the robustness properties of the original estimator, addressing sample size limitations common in biomedical studies [95]. Two primary Bayesian implementations have emerged: Bayes factor approaches that quantify evidence for interval null hypotheses, and Region of Practical Equivalence (ROPE) methods that evaluate posterior distribution overlap with equivalence bounds [95] [34]. These Bayesian formulations maintain the likelihood principle compliance that makes Bayesian methods advantageous for sequential designs and censored data scenarios prevalent in clinical research.
Experimental Protocols and Methodological Implementation
Standard Hodges-Lehmann Testing Protocol
The implementation of Hodges-Lehmann equivalence testing follows a structured workflow that can be adapted to various experimental designs. The following diagram illustrates the core analytical process:
The implementation begins with equivalence region specification, which should be determined based on clinical rather than statistical considerations. For example, in therapeutic equivalence trials, the equivalence margin might represent the smallest clinically meaningful difference that would change practice patterns. The subsequent estimator selection depends on study design and data characteristics, with specialized variants available for paired observations, independent groups, and censored time-to-event endpoints.
For the critical step of confidence interval construction, the Hodges-Lehmann method tests the null hypothesis for a range of parameter values, with the confidence interval comprising all values not rejected at the specified significance level [100]. In the two-sample case with censored data, this involves testing H₀: ρ = ρ₀ for multiple values of ρ₀ by transforming the data (replacing each Y with ρ₀Y) and applying the Gehan test to the transformed dataset [100]. The point estimate corresponds to the ρ value yielding a test p-value closest to 1.0, representing the maximum compatibility with the observed data.
Adaptation for Censored Time-to-Event Data
The Hodges-Lehmann framework effectively handles right-censored data common in biomedical studies through integration with Gehan's generalized Wilcoxon test [100]. This adaptation follows a modified protocol:
The Gehan score calculation represents a distinctive aspect of this approach. For each subject, the algorithm conducts pairwise comparisons against all other subjects, with scoring rules that appropriately handle censored observations [100]:
- Win conditions: Subject j wins over k if (1) j is uncensored and k is censored, or (2) both are uncensored but j has shorter event time
- Loss conditions: Subject j loses to k if (1) j is censored and k is uncensored, or (2) both are uncensored but j has longer event time
- Tie conditions: All other scenarios (both censored, or identical uncensored times)
The resulting net Gehan score (wins minus losses) provides a robust foundation for permutation testing that accommodates the informational limitations of censored observations. This approach has proven particularly valuable in clinical trials targeting hospital discharge time reduction, where some patients may never meet discharge criteria despite eventual discharge [100].
Comparative Performance Analysis
Statistical Properties Across Methodologies
Table 1: Comparative Properties of Hypothesis Testing Frameworks
| Statistical Property | Traditional NHST | Hodges-Lehmann Equivalence Testing | Bayesian Hodges-Lehmann |
|---|---|---|---|
| Hypothesis Formulation | Point null (H₀: δ = 0) | Interval null (H₀: δ ∈ [-ε, ε]) | Interval null with prior incorporation |
| Breakdown Point | 0.00 (mean-based) | 0.29 | Varies with prior specification |
| Efficiency for Normal Data | 100% (t-test) | ~95% relative to t-test | Dependent on prior choice |
| Efficiency for Heavy-Tailed Data | Poor | Excellent | Good with appropriate priors |
| Censored Data Handling | Requires specialized methods | Natural extension via Gehan scores | Flexible with likelihood adaptation |
| Interpretational Clarity | Problematic (p-values) | Direct (effect size with CI) | Probabilistic (posterior equivalence) |
| Optional Stopping | Problematic | Compatible | Fully compatible |
| Theoretical Foundation | Frequentist | Nonparametric rank-based | Bayesian nonparametric |
The Hodges-Lehmann framework demonstrates particular advantages in robustness and efficiency across diverse data conditions. While traditional parametric tests achieve maximal efficiency under ideal distributional assumptions, they degrade rapidly with distributional violations common in biomedical data [99]. Conversely, Hodges-Lehmann methods maintain high relative efficiency across both normal and non-normal distributions—approximately 95% efficiency relative to the t-test for normal data while substantially outperforming parametric methods for heavy-tailed distributions like the Cauchy, where the sample mean fails to provide a consistent estimator [99].
Empirical Performance in Biomedical Applications
Table 2: Empirical Performance Across Biomedical Study Types
| Application Domain | Traditional Method | Hodges-Lehmann Method | Performance Advantage |
|---|---|---|---|
| Hospital Discharge Time [100] | Cox PH Model (HR) | HL Scale Estimator | More interpretable effect size (40% reduction vs. HR) |
| Digoxin Poisoning [102] | Mean difference | HL estimator with exact CI | Robust to outlier influence |
| Biomarker Studies [102] | Parametric tests | HL median difference | Handles skewed distributions effectively |
| Therapeutic Equivalence [95] | Two one-sided tests (TOST) | Bayesian HL equivalence tests | Incorporates prior evidence, handles censoring |
| Ophthalmology Research [102] | Mann-Whitney U test | HL estimate with CI | Provides effect size with precision |
| Clinical Toxicology [102] | Traditional t-tests | HL difference estimator | Robust validity with small samples |
Empirical evaluations consistently demonstrate the operational advantages of Hodges-Lehmann methods across diverse biomedical contexts. In therapeutic equivalence testing, Bayesian Hodges-Lehmann approaches provide enhanced sensitivity to prior information while maintaining robust frequentist error control [95]. For hospital discharge time studies, the Hodges-Lehmann scale estimator directly quantifies the percentage reduction in time to discharge (e.g., ρ = 0.47 indicating a 53% reduction), offering more clinically interpretable effect size measures than hazard ratios from Cox models [100].
The performance advantages extend to small sample settings common in early-phase clinical trials and specialized biomarker research. For example, in a study of matricellular proteins in acute primary angle closure, Hodges-Lehmann estimation provided stable median difference estimates with exact confidence intervals despite substantial distributional skewness [102]. Similarly, in clinical toxicology research comparing digoxin-specific antibody fragments versus observation, Hodges-Lehmann methods generated reliable effect size estimates with appropriate confidence intervals for heart rate and potassium concentration changes [102].
Statistical Software and Computational Tools
Table 3: Implementation Resources for Hodges-Lehmann Methods
| Software Platform | Implementation Approach | Key Functions/Capabilities | Specialized Applications |
|---|---|---|---|
| R Statistical Environment | hodgeslehmann() function in coin package |
One-sample, two-sample, and paired designs | General biomedical statistics |
| SAS | PROC NPAR1WAY with HL option | Nonparametric analysis with HL estimates | Clinical trial analysis |
| STATXACT | Exact nonparametric procedures | Exact confidence intervals for scale parameters | Small sample studies |
| Stata | hl command |
Hodges-Lehmann difference estimation | Epidemiological research |
| GraphPad Prism | Nonparametric analysis options | Median difference with confidence interval | Laboratory science applications |
| Custom SAS Macros [100] | Gehan test implementation | Scale estimation with censored data | Time-to-discharge studies |
Successful implementation requires appropriate software selection matched to study design constraints. For standard independent group comparisons without censoring, most major statistical platforms offer built-in Hodges-Lehmann functionality. For specialized applications involving right-censored data, custom computational tools like the SAS macro referenced in [100] provide tailored implementations of the Gehan-based Hodges-Lehmann interval estimation procedure. These specialized resources include sample size calculation utilities that accommodate anticipated censoring patterns through conservative inflation factors (typically 1/(1-C) where C represents the expected censoring proportion) [100].
Methodological Decision Framework
Researchers can optimize their analytical strategy through a structured method selection framework:
This decision pathway emphasizes that equivalence testing goals immediately favor Hodges-Lehmann methods, while other study designs benefit from evaluating data structure characteristics against method assumptions. The framework particularly highlights scenarios where traditional methods prove inadequate: when censored observations preclude standard parametric analysis, when distributional violations threaten parametric assumption validity, and when prior information can usefully inform statistical inference through Bayesian Hodges-Lehmann implementations.
The Hodges-Lehmann paradigm provides a unified and robust framework for interval hypothesis testing that addresses fundamental limitations of traditional NHST in biomedical research. Through its nonparametric foundation, natural handling of censored data, and direct estimation of clinically interpretable effect sizes, this approach offers substantial advantages for therapeutic equivalence testing, biomarker validation, and comparative effectiveness research. The methodological framework supports both frequentist and Bayesian implementations, accommodating diverse analytical preferences while maintaining theoretical coherence and practical utility.
Empirical evidence from across biomedical research domains demonstrates that Hodges-Lehmann methods maintain robust performance where traditional parametric approaches fail, particularly with non-normal distributions, outlier contamination, and censored observations. As biomedical research increasingly emphasizes practical equivalence rather than statistical difference, the Hodges-Lehmann paradigm represents an essential analytical foundation for next-generation clinical research and evidence-based medicine.
Conclusion
Equivalence testing provides a statistically rigorous framework for demonstrating that model performances or treatment effects are practically indistinguishable, a question of paramount importance in drug development and clinical research. By shifting the burden of proof, these methods allow researchers to make positive claims about similarity, overcoming a critical limitation of traditional significance testing. The successful application of these techniques—from the frequentist TOST procedure to modern Bayesian methods and robust model averaging—relies on the careful a priori definition of a meaningful equivalence boundary and a thorough understanding of potential pitfalls like model misspecification and low statistical power. As biomedical models grow in complexity, the integration of these equivalence testing paradigms, particularly those that embrace model uncertainty, will be essential for developing reliable, validated tools that can confidently inform clinical and regulatory decisions. Future directions will likely involve greater adoption of Bayesian methods for their interpretive advantages and the continued development of standardized equivalence testing workflows for complex machine learning models in healthcare.
References
- 1. Hypothesis and Equivalence Testing [https://www.advantive.com/blog/hypothesis-and-equivalence-testing/]
- 2. 9 Equivalence Testing and Interval Hypotheses - GitHub Pages [https://lakens.github.io/statistical_inferences/09-equivalencetest.html]
- 3. When Null Hypothesis Significance Testing Is Unsuitable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5540883/]
- 4. Multivariate Adjustments for Average Equivalence Testing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12258420/]
- 5. Using T-tests to benchmark page load performance [https://medium.com/gotoassist-product-blog/using-t-tests-to-benchmark-page-load-performance-6f45faff091e]
- 6. Hypothesis Test for Comparing Machine Learning Algorithms [https://www.machinelearningmastery.com/hypothesis-test-for-comparing-machine-learning-algorithms/]
- 7. The untapped potential of Bayesian region of practical ... [https://www.sciencedirect.com/science/article/pii/S0360132325008662]
- 8. Region of Practical Equivalence (ROPE) - easystats [https://easystats.github.io/bayestestR/articles/region_of_practical_equivalence.html]
- 9. Using anchor-based methods to determine the smallest ... [https://www.sciencedirect.com/science/article/pii/S0022103121000627]
- 10. What is a Minimum Effect of Interest (MEI)? [https://www.analytics-toolkit.com/glossary/minimum-effect-of-interest/]
- 11. Reducing the false discovery rate of preclinical animal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10563376/]
- 12. ROPE and Equivalence Testing: Practically Equivalent? [http://daniellakens.blogspot.com/2017/02/rope-and-equivalence-testing.html]
- 13. Abbreviated New Drug Application (ANDA) [https://www.fda.gov/drugs/types-applications/abbreviated-new-drug-application-anda]
- 14. The Definitive Guide to Generic Drug Approval in the U.S. [https://www.drugpatentwatch.com/blog/obtaining-generic-drug-approval-in-the-united-states/?srsltid=AfmBOopyF1hIXVwBj597zB0Dz1aQ9BT_Y15qfg3k8oiPjLdcb2jTLPRX]
- 15. Hypothesis Testing The Ultimate Guide to Smarter ... [https://www.tatvic.com/blog/hypothesis-testing-the-ultimate-guide/]
- 16. Development and Validation of the Clinical Trial Site ... [https://pubmed.ncbi.nlm.nih.gov/41095920/]
- 17. An open source statistical web application for validation ... [https://www.nature.com/articles/s41598-025-99720-3]
- 18. Methods for Analytical Validation of Novel Digital Clinical ... [https://www.jmir.org/2025/1/e70314]
- 19. Specification Equivalence: A Practical Approach to Method ... [https://www.biopharminternational.com/view/specification-equivalence-a-practical-approach-to-method-and-acceptance-criteria-equivalence]
- 20. Clinical trial data analytics: Revolution in 2025 [https://lifebit.ai/blog/clinical-trial-data-analytics/]
- 21. LibGuides: Statistics Resources: Hypothesis Testing [https://resources.nu.edu/statsresources/hypothesistesting]
- 22. | A Step-by-Step Guide with Easy Examples Hypothesis Testing [https://www.scribbr.com/statistics/hypothesis-testing/]
- 23. Equivalence and non-inferiority trials in the evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406809/]
- 24. Interpreting the results of noninferiority trials—a review [https://www.nature.com/articles/s41416-022-01937-w]
- 25. : A Practical Primer for t Equivalence , Correlations, and... Tests Tests [https://pmc.ncbi.nlm.nih.gov/articles/PMC5502906/]
- 26. Hypothesis Testing: A Comprehensive Guide with ... [https://www.6sigma.us/six-sigma-in-focus/hypothesis-testing/]
- 27. Which Statistical Hypothesis Test Should I Apply? A Simple ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4910310/]
- 28. 16.2 Two One-Sided Tests Equivalence Testing [https://bookdown.org/mike/data_analysis/sec-two-one-sided-tests-equivalence-testing.html]
- 29. Equivalence test [https://en.wikipedia.org/wiki/Equivalence_test]
- 30. Equivalence Testing (TOST) [https://real-statistics.com/students-t-distribution/equivalence-testing-tost/]
- 31. Power Estimation for TOST Approaches in MS Excel [https://www.bioprocessintl.com/qa-qc/power-estimation-for-two-one-sided-tests-using-simulations-in-nonspecialist-software]
- 32. Best statistical method to compare model data with data from ... [https://stats.stackexchange.com/questions/637057/best-statistical-method-to-compare-model-data-with-data-from-real-measurements]
- 33. 4 Hypothesis and equivalence tests – Model to Meaning [https://marginaleffects.com/chapters/hypothesis.html]
- 34. Bayesian Hodges-Lehmann tests for statistical equivalence in ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-021-01341-7]
- 35. The logic of equivalence testing and its use in laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5382845/]
- 36. Equivalence Testing for Comparability [https://www.biopharminternational.com/view/equivalence-testing-comparability]
- 37. Strategy to equivalence testing for development and scale ... [https://www.sciencedirect.com/science/article/abs/pii/S0009250921000622]
- 38. A Bayesian approach for evaluating equivalence over ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11389643/]
- 39. Bayesian Analysis Reporting Guidelines [https://www.nature.com/articles/s41562-021-01177-7]
- 40. How Equivalence Tests Can Benefit From Model Averaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC11923417/]
- 41. how equivalence tests can benefit from model averaging [https://arxiv.org/abs/2405.00827]
- 42. How equivalence tests can benefit from model averaging [https://www.cmstatistics.org/RegistrationsV2/CFECMStatistics2024/viewSubmission.php?in=348&token=s483234127616723s1ppr0q3122o49nq]
- 43. On improvability of model selection by model averaging [https://www.sciencedirect.com/science/article/abs/pii/S0304407620303973]
- 44. Optimal designs for frequentist model averaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6690170/]
- 45. model averaging for out-of-distribution forecasting [https://arxiv.org/html/2506.03693v2]
- 46. Model validation using equivalence tests [https://www.sciencedirect.com/science/article/abs/pii/S0304380004000985]
- 47. - Dose Analysis Using R | PLOS One Response [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0146021]
- 48. REAP-2: An interactive quantitative tool for robust and efficient... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10643933/]
- 49. Comparing Classification Models - You're Probably Doing ... [http://practicalcheminformatics.blogspot.com/2023/11/comparing-classification-models-youre.html]
- 50. Some Thoughts on Comparing Classification Models [http://practicalcheminformatics.blogspot.com/2020/05/some-thoughts-on-comparing.html]
- 51. Statistical Tests for Comparing Classification Algorithms [https://towardsdatascience.com/statistical-tests-for-comparing-classification-algorithms-ac1804e79bb7/]
- 52. Approximate statistical tests for comparing binary classifier ... [https://blog.stata.com/2025/04/22/approximate-statistical-tests-for-comparing-binary-classifier-error-rates-using-h2oml/]
- 53. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 54. Evaluation metrics and statistical tests for machine learning [https://www.nature.com/articles/s41598-024-56706-x]
- 55. Power for equivalence tests - Minitab - Support [https://support.minitab.com/en-us/minitab/help-and-how-to/statistics/equivalence-tests/supporting-topics/power-for-equivalence-tests/]
- 56. Sample size, power and effect size revisited: simplified and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7745163/]
- 57. Determining Sample Size for Testing Equivalence [https://www.mddionline.com/testing/determining-sample-size-for-testing-equivalence]
- 58. Chapter 11 Equivalence tests and sample size | Welcome! [https://dstanley4.github.io/psyc4780bookdown/equivalence-tests-and-sample-size.html]
- 59. Sample Size Estimation for Equivalence Studies in a Parallel ... [https://bebac.at/articles/Sample-Size-Estimation-for-Equivalence-Studies-in-a-Parallel-Design.phtml]
- 60. Power calculator for continuous outcome equivalence trial [https://www.sealedenvelope.com/power/continuous-equivalence/]
- 61. Equivalence Test and Sample Size Determination Based ... [https://www.mdpi.com/2075-1680/14/8/582]
- 62. On the Equivalence Test and Sample Size Procedures for ... [https://link.springer.com/article/10.1007/s44199-024-00089-5]
- 63. PASS Sample Size Software Documentation [https://www.ncss.com/software/pass/pass-documentation/]
- 64. SPIRIT 2025 statement: Updated guideline for protocols of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037212/]
- 65. Errors in Statistical Inference Under Model Misspecification [https://www.frontiersin.org/journals/ecology-and-evolution/articles/10.3389/fevo.2019.00372/full]
- 66. Why type 1 error matters in statistical testing [https://www.statsig.com/perspectives/why-type-one-error-matters]
- 67. Hypothesis testing, type I and type II errors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2996198/]
- 68. How Does Model (Mis)Specification Impact Statistical Power ... [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.31234/osf.io/prqsg_v2]
- 69. Dependence of power and type I error on model ... [https://rr.peercommunityin.org/PCIRegisteredReports/articles/rec?articleId=398&printable=True]
- 70. Allele frequency misspecification: effect on power and Type I ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1475629/]
- 71. Tests for model misspecification in simulation-based ... [https://arxiv.org/html/2412.15100v2]
- 72. Power analyses for measurement model misspecification ... [https://link.springer.com/article/10.1007/s11136-024-03605-3]
- 73. AIC BIC Model Selection: The Ultimate 2025 Guide Made Easy [https://econometriclinks.com/aic-bic-model-selection/]
- 74. Bayesian Model Averaging for Predicting Maximal Oxygen ... [https://www.ej-sport.org/index.php/sport/article/view/254]
- 75. Comparison of Model Averaging and Model Selection in ... [https://inserm.hal.science/inserm-01807517v1]
- 76. Comparison of Model Averaging and Model Selection in ... [https://pubmed.ncbi.nlm.nih.gov/29600418/]
- 77. Prediction Intervals for Model Averaging 1 [https://arxiv.org/html/2510.16224v1]
- 78. Bayesian Statistics: A Modern Accurate Data Analysis in ... [https://www.linkedin.com/pulse/bayesian-statistics-modern-accurate-data-s2tye]
- 79. Sensitivity analysis of Bayesian estimates of value function ... [https://www.sciencedirect.com/science/article/pii/S1755534525000442]
- 80. A Review and Comparison of Different Sensitivity Analysis ... [https://arxiv.org/html/2506.11471]
- 81. Prior sensitivity analysis in Bayesian SEM and its application ... [https://congress.eam2025.eu/event/2/contributions/172/]
- 82. Life beyond MSE and R2 — improving validation of ... [http://ui.adsabs.harvard.edu/abs/2017EGUGA..19.7899P/abstract]
- 83. Beyond predictive R2: Quantile regression and non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12256909/]
- 84. A Primer on the Use of Equivalence Testing for Evaluating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5856600/]
- 85. Statistical Significance vs. Equivalence: What Clinical ... [https://www.medxteam.de/en/medxteam-blog/how-to-create-a-clinical-assessment-based-on-performance-data-2]
- 86. A new equivalence based metric for predictive check to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2751255/]
- 87. A Guide to Using Post Hoc Tests with ANOVA [https://www.statology.org/anova-post-hoc-tests/]
- 88. Using Post Hoc Tests with ANOVA - Statistics By Jim [https://statisticsbyjim.com/anova/post-hoc-tests-anova/]
- 89. Relationship between Omnibus and Post-hoc Tests: An Investigation of performance of the F test in ANOVA - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5925602/]
- 90. ANOVA for Data Science and Data Analytics [https://www.geeksforgeeks.org/data-science/anova-for-data-science-and-data-analytics/]
- 91. machine learning - How to perform hypothesis testing for comparing different classifiers - Cross Validated [https://stats.stackexchange.com/questions/89064/how-to-perform-hypothesis-testing-for-comparing-different-classifiers]
- 92. Statistical testing: Multiple classifiers, 1 domain. Would ... [https://stats.stackexchange.com/questions/89203/statistical-testing-multiple-classifiers-1-domain-would-ranova-be-appropriate]
- 93. Statistics (III) ANOVA in Data Science & Machine Learning [https://jonathan-hui.medium.com/statistics-iii-anova-in-data-science-machine-learning-d811f200e3fb]
- 94. A Comparison of the Bayesian Posterior Probability and ... [https://arxiv.org/abs/2507.19685]
- 95. Bayesian Hodges-Lehmann tests for statistical equivalence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8369333/]
- 96. Analysis of type I and II error rates of Bayesian and ... [https://link.springer.com/article/10.1007/s00180-020-01034-7]
- 97. Frequentist vs Bayesian Statistics in A/B Testing [https://www.convert.com/blog/a-b-testing/frequentist-vs-bayesian-ab-testing/]
- 98. Interpret the key results for 2-Sample Equivalence Test - Minitab [https://support.minitab.com/en-us/minitab/help-and-how-to/statistics/equivalence-tests/how-to/2-sample-equivalence-test/interpret-the-results/key-results/]
- 99. Hodges–Lehmann estimator [https://en.wikipedia.org/wiki/Hodges%E2%80%93Lehmann_estimator]
- 100. Applying Hodges-Lehmann scale parameter estimates to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2745104/]
- 101. Hodges–Lehmann optimality for testing moment conditions [https://www.sciencedirect.com/science/article/abs/pii/S0304407612001728]
- 102. Hodges-Lehmann estimator – Knowledge and References [https://taylorandfrancis.com/knowledge/Medicine_and_healthcare/Medical_statistics_%26_computing/Hodges-Lehmann_estimator/]