Hypothesis Testing for Model Validation: A Comprehensive Guide for Biomedical Research
This article provides a comprehensive framework for using statistical hypothesis testing to validate predictive models in biomedical research and drug development.
Hypothesis Testing for Model Validation: A Comprehensive Guide for Biomedical Research
Abstract
This article provides a comprehensive framework for using statistical hypothesis testing to validate predictive models in biomedical research and drug development. It covers foundational statistical principles, practical methodologies for comparing machine learning algorithms, strategies for troubleshooting common pitfalls like p-hacking and underpowered studies, and advanced techniques for robust model comparison and Bayesian validation. Designed for researchers and scientists, the guide synthesizes classical and modern approaches to ensure model reliability, reproducibility, and translational impact in clinical settings.
Core Principles of Hypothesis Testing and Statistical Foundations for Model Validation
Defining the Null and Alternative Hypothesis in a Validation Context
In model validation and scientific research, hypothesis testing provides a formal framework for investigating ideas using statistics [1]. It is a critical process for making inferences about a population based on sample data, allowing researchers to test specific predictions that arise from theories [1]. The core of this framework rests on two competing, mutually exclusive statements: the null hypothesis (H₀) and the alternative hypothesis (Hₐ or H₁) [2] [3]. In a validation context, these hypotheses offer competing answers to a research question, enabling scientists to weigh evidence for and against a particular effect using statistical tests [2].
The null hypothesis typically represents a position of "no effect," "no difference," or the status quo that the validation study aims to challenge [4] [3]. For drug development professionals, this often translates to assuming a new treatment has no significant effect compared to a control or standard therapy. The alternative hypothesis, conversely, states the research prediction of an effect or relationship that the researcher expects or hopes to validate [2] [4]. Properly defining these hypotheses before data collection and interpretation is crucial, as it provides direction for the research and a framework for reporting inferences [5].
Fundamental Definitions and Conceptual Framework
Null Hypothesis (H₀)
The null hypothesis (H₀) is the default position that there is no effect, no difference, or no relationship between variables in the population [2] [4]. It is a claim about the population parameter that the validation study aims to disprove or challenge [4]. In statistical terms, the null hypothesis always includes an equality symbol (usually =, but sometimes ≥ or ≤) [2].
In the context of model validation and drug development, the null hypothesis often represents the proposition that any observed differences in data are due to chance rather than a genuine effect of the treatment or model being validated [6]. For example, in clinical trial validation, the null hypothesis might state that a new drug has the same efficacy as a placebo or standard treatment.
Alternative Hypothesis (Hₐ or H₁)
The alternative hypothesis (Hₐ or H₁) is the complement to the null hypothesis and represents the research hypothesis—what the statistician is trying to prove with data [2] [3]. It claims that there is a genuine effect, difference, or relationship in the population [2]. In mathematical terms, alternative hypotheses always include an inequality symbol (usually ≠, but sometimes < or >) [2].
In validation research, the alternative hypothesis typically reflects the expected outcome of the study—that the new model, drug, or treatment demonstrates a statistically significant effect worthy of validation. The alternative hypothesis is sometimes called the research hypothesis or experimental hypothesis [6].
Table 1: Core Characteristics of Null and Alternative Hypotheses
| Characteristic | Null Hypothesis (H₀) | Alternative Hypothesis (Hₐ) |
|---|---|---|
| Definition | A claim of no effect in the population [2] | A claim of an effect in the population [2] |
| Role in Research | Represents the status quo or default position [3] | Represents the research prediction [2] |
| Mathematical Symbols | Equality symbol (=, ≥, or ≤) [2] | Inequality symbol (≠, <, or >) [2] |
| Verbal Cues | "No effect," "no difference," "no relationship" [2] | "An effect," "a difference," "a relationship" [2] |
| Mutually Exclusive | Yes, only one can be true at a time [2] | Yes, only one can be true at a time [2] |
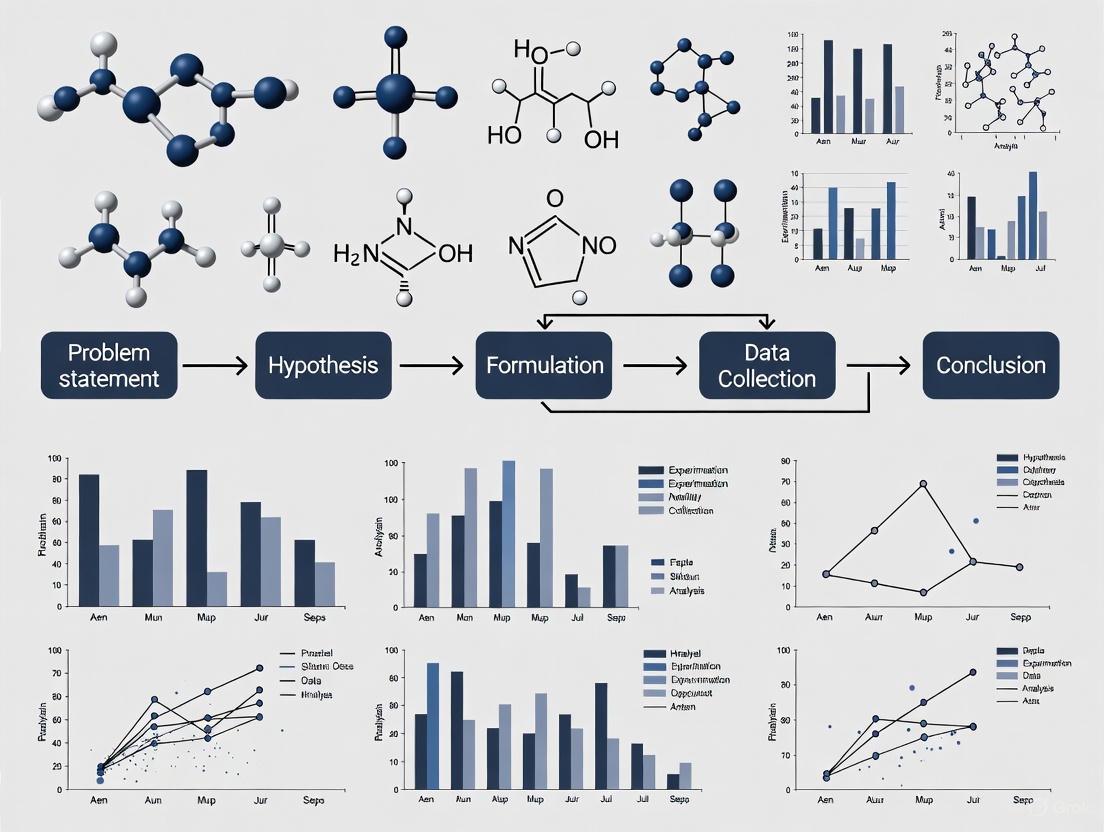
Figure 1: Hypothesis Testing Workflow in Validation Research
Formulating Hypotheses for Validation Studies
General Template Sentences
To formulate hypotheses for validation studies, researchers can use general template sentences that specify the dependent and independent variables [2]. The research question typically follows the format: "Does the independent variable affect the dependent variable?"
- Null hypothesis (H₀): "Independent variable does not affect dependent variable." [2]
- Alternative hypothesis (Hₐ): "Independent variable affects dependent variable." [2]
These general templates can be adapted to various validation contexts in drug development and model testing. The key is ensuring that both hypotheses are mutually exclusive and exhaustive, covering all possible outcomes of the study [4].
Test-Specific Formulations
Once the statistical test is chosen, hypotheses can be written in a more precise, mathematical way specific to the test [2]. The table below provides template sentences for common statistical tests used in validation research.
Table 2: Test-Specific Hypothesis Formulations for Validation Studies
| Statistical Test | Null Hypothesis (H₀) | Alternative Hypothesis (Hₐ) |
|---|---|---|
| Two-sample t-test | The mean dependent variable does not differ between group 1 (µ₁) and group 2 (µ₂) in the population; µ₁ = µ₂ [2] | The mean dependent variable differs between group 1 (µ₁) and group 2 (µ₂) in the population; µ₁ ≠ µ₂ [2] |
| One-way ANOVA with three groups | The mean dependent variable does not differ between group 1 (µ₁), group 2 (µ₂), and group 3 (µ₃) in the population; µ₁ = µ₂ = µ₃ [2] | The mean dependent variable of group 1 (µ₁), group 2 (µ₂), and group 3 (µ₃) are not all equal in the population [2] |
| Pearson correlation | There is no correlation between independent variable and dependent variable in the population; ρ = 0 [2] | There is a correlation between independent variable and dependent variable in the population; ρ ≠ 0 [2] |
| Simple linear regression | There is no relationship between independent variable and dependent variable in the population; β₁ = 0 [2] | There is a relationship between independent variable and dependent variable in the population; β₁ ≠ 0 [2] |
| Two-proportions z-test | The dependent variable expressed as a proportion does not differ between group 1 (p₁) and group 2 (p₂) in the population; p₁ = p₂ [2] | The dependent variable expressed as a proportion differs between group 1 (p₁) and group 2 (p₂) in the population; p₁ ≠ p₂ [2] |
Directional vs. Non-Directional Alternative Hypotheses
Alternative hypotheses can be categorized as directional or non-directional [5] [6]. This distinction determines whether the hypothesis test is one-tailed or two-tailed.
- Non-directional alternative hypothesis: A hypothesis that suggests there is a difference between groups but does not specify the direction of this difference [6]. This leads to a two-tailed test. For example: "The drug efficacy of Treatment A is different from Treatment B."
- Directional alternative hypothesis: A hypothesis that specifies the direction of the expected difference between groups [6]. This leads to a one-tailed test. For example: "The drug efficacy of Treatment A is greater than Treatment B."
The choice between directional and non-directional hypotheses should be theoretically justified and specified before data collection, as it affects the statistical power and interpretation of results.
Experimental Protocol for Hypothesis Testing in Validation
Step-by-Step Hypothesis Testing Procedure
The hypothesis testing procedure follows a systematic, step-by-step approach that should be rigorously applied in validation contexts [1].
Step 1: State the null and alternative hypotheses After developing the initial research hypothesis, restate it as a null hypothesis (H₀) and alternative hypothesis (Hₐ) that can be tested mathematically [1]. The hypotheses should be stated in both words and mathematical symbols, clearly defining the population parameters [7].
Step 2: Collect data For a statistical test to be valid, sampling and data collection must be designed to test the hypothesis [1]. The data must be representative to allow valid statistical inferences about the population of interest [1]. In validation studies, this often involves ensuring proper randomization, sample size, and control of confounding variables.
Step 3: Perform an appropriate statistical test Select and perform a statistical test based on the type of variables, the level of measurement, and the research question [1]. The test compares within-group variance (how spread out data is within a category) versus between-group variance (how different categories are from one another) [1]. The test generates a test statistic and p-value for interpretation.
Step 4: Decide whether to reject or fail to reject the null hypothesis Based on the p-value from the statistical test and a predetermined significance level (α, usually 0.05), decide whether to reject or fail to reject the null hypothesis [1] [4]. If the p-value is less than or equal to the significance level, reject H₀; if it is greater, fail to reject H₀ [4].
Step 5: Present the findings Present the results in the formal language of hypothesis testing, stating whether you reject or fail to reject the null hypothesis [1]. In scientific papers, also state whether the results support the alternative hypothesis [1]. Include the test statistic, p-value, and a conclusion in context [7].
Figure 2: Step-by-Step Experimental Protocol for Hypothesis Testing
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Validation Studies
| Item/Reagent | Function in Validation Research |
|---|---|
| Statistical Software | Performs complex statistical calculations, generates p-values, and creates visualizations for data interpretation [5] |
| Sample Size Calculator | Determines minimum sample size needed to achieve adequate statistical power for detecting effects |
| Randomization Tool | Ensures unbiased assignment to experimental groups, satisfying the "random" condition for valid hypothesis testing [7] [6] |
| Data Collection Protocol | Standardized procedure for collecting data to ensure consistency, reliability, and reproducibility |
| Positive/Negative Controls | Reference materials that validate experimental procedures by producing known, expected results |
| Standardized Measures/Assays | Validated instruments or biochemical assays that reliably measure dependent variables of interest |
| Blinding Materials | Procedures and materials to prevent bias in treatment administration and outcome assessment |
| Documentation System | Comprehensive system for recording methods, observations, and results to ensure traceability and reproducibility |
Interpretation and Decision Making in Validation
Understanding P-values and Significance
The p-value is a critical part of null-hypothesis significance testing that quantifies how strongly the sample data contradicts the null hypothesis [4]. It represents the probability of observing the obtained results, or more extreme results, if the null hypothesis were true [4].
A smaller p-value indicates stronger evidence against the null hypothesis [4]. In most validation research, a predetermined significance level (α) of 0.05 is used, meaning that if the p-value is less than or equal to 0.05, the null hypothesis is rejected [4]. Some studies may choose a more conservative level of significance, such as 0.01, to minimize the risk of Type I errors [1].
Using precise language when reporting hypothesis test results is crucial, especially in validation research where conclusions inform critical decisions.
- When rejecting H₀: "Because the p-value (0.018) is less than α = 0.05, we reject H₀. We have convincing evidence that the alternative hypothesis is true." [7]
- When failing to reject H₀: "Since the p-value (0.063) is greater than α = 0.05, we fail to reject H₀. We do not have convincing evidence that the alternative hypothesis is true." [7]
It is essential to never say "accept the null hypothesis" because a lack of evidence against the null does not prove it is true [4] [3]. There is always a possibility that a larger sample size or different study design might detect an effect.
Error Types in Hypothesis Testing
Hypothesis testing involves two types of errors that researchers must consider when interpreting results, particularly in high-stakes validation contexts [4] [3].
- Type I Error (False Positive): Rejecting the null hypothesis when it is actually true [4] [3]. The probability of a Type I error is denoted by α (alpha) and is typically set at 0.05 in scientific research [4].
- Type II Error (False Negative): Failing to reject the null hypothesis when it is actually false [4] [3]. The probability of a Type II error is denoted by β (beta), and statistical power is defined as 1-β [3].
Table 4: Error Matrix in Hypothesis Testing for Validation
| Decision/Reality | H₀ is TRUE | H₀ is FALSE |
|---|---|---|
| Reject H₀ | Type I Error (False Positive) [4] [3] | Correct Decision (True Positive) |
| Fail to Reject H₀ | Correct Decision (True Negative) | Type II Error (False Negative) [4] [3] |
Applications in Model Validation and Drug Development
In model validation research, hypothesis testing provides a rigorous framework for evaluating model performance, comparing different models, and assessing predictive accuracy. For example, a null hypothesis might state that a new predictive model performs no better than an existing standard model, while the alternative hypothesis would claim superior performance.
In pharmaceutical development, hypothesis testing is fundamental to clinical trials, where the null hypothesis typically states that a new drug has no difference in efficacy compared to a placebo or standard treatment. Regulatory agencies like the FDA require rigorous hypothesis testing to demonstrate safety and efficacy before drug approval.
The principles outlined in this document apply across various validation contexts, ensuring that conclusions are based on statistical evidence rather than anecdotal observations or assumptions. Properly formulated and tested hypotheses provide the foundation for scientific advancement in drug development and model validation.
In the rigorous field of model validation research, particularly within drug development, statistical hypothesis testing provides the critical framework for making objective, data-driven decisions. This process allows researchers to quantify the evidence for or against a model's accuracy, moving beyond subjective assessment to rigorous statistical proof. At the heart of this framework lie three interconnected concepts: the significance level (α), the p-value, and statistical power. These concepts form the foundation for controlling error rates, interpreting experimental results, and ensuring that models are sufficiently sensitive to detect meaningful effects. Within model validation, this translates to a systematic process of building trust in a model through iterative testing and confirmation of its predictions against experimental data [8].
The core of hypothesis testing involves making two competing statements about a population parameter. The null hypothesis (H₀) typically represents a default position of "no effect," "no difference," or, in the context of model validation, "the model is not an accurate representation of reality." The alternative hypothesis (H₁ or Hₐ) is the logical opposite, asserting that a significant effect, difference, or relationship does exist [9] [10]. The goal of hypothesis testing is to determine whether there is sufficient evidence in the sample data to reject the null hypothesis in favor of the alternative.
Deep Dive: P-values and Significance Levels (α)
The Significance Level (α) - A Pre-Defined Threshold
The significance level, denoted by alpha (α), is a pre-chosen probability threshold that determines the required strength of evidence needed to reject the null hypothesis. It represents the probability of making a Type I error, which is the incorrect rejection of a true null hypothesis [9] [11]. In practical terms, a Type I error in model validation would be concluding that a model is accurate when it is, in fact, flawed.
The choice of α is arbitrary but governed by convention and the consequences of error. Common thresholds include:
- α = 0.05: Accepts a 5% chance of a Type I error. This is the most common standard for general research and exploratory analysis [9].
- α = 0.01: Accepts a 1% chance of a Type I error. This is a stricter threshold often used in high-stakes research like clinical trials where the cost of a false positive is high [9].
- α = 0.001: Accepts a 0.1% chance of a Type I error. This signifies a "highly statistically significant" threshold and is used for findings where near-certainty is required [9].
The selection of α should be a deliberate decision based on the research context, goals, and the potential real-world impact of a false discovery [9].
The P-value - A Calculated Probability
The p-value is a calculated probability that measures the compatibility between the observed data and the null hypothesis. Formally, it is defined as the probability of obtaining a test result at least as extreme as the one actually observed, assuming that the null hypothesis is true [9] [11].
Unlike α, which is fixed beforehand, the p-value is computed from the sample data after the experiment or study is conducted. A smaller p-value indicates that the observed data is less likely to have occurred under the assumption of the null hypothesis, thus providing stronger evidence against H₀ [9].
Interpreting P-values and Making Decisions
The final step in a hypothesis test involves comparing the calculated p-value to the pre-defined significance level α. This comparison leads to a statistical decision:
- If the p-value ≤ α, there is sufficient evidence to reject the null hypothesis. The result is considered statistically significant, suggesting that the observed effect is unlikely to be due to chance alone [9] [12].
- If the p-value > α, there is insufficient evidence to reject the null hypothesis. The result is not statistically significant, and we "fail to reject H₀." It is critical to note that this is not the same as proving the null hypothesis true [9].
The table below summarizes this decision-making framework and the potential for error.
Table 1: Interpretation of P-values and Decision Framework
| P-value Range | Evidence Against H₀ | Action | Interpretation Cautions |
|---|---|---|---|
| p ≤ 0.01 | Very strong | Reject H₀ | Does not prove the alternative hypothesis is true; does not measure the size or importance of an effect. |
| 0.01 < p ≤ 0.05 | Strong | Reject H₀ | A statistically significant result may have little practical importance. |
| p > 0.05 | Weak or none | Fail to reject H₀ | Not evidence that the null hypothesis is true; may be due to low sample size or power. |
The Concept of Statistical Power
Statistical power is the probability that a test will correctly reject a false null hypothesis. In other words, it is the likelihood of detecting a real effect when it genuinely exists. Power is calculated as 1 - β, where β (beta) is the probability of a Type II error—failing to reject a false null hypothesis (a false negative) [11] [13].
A study with high power (e.g., 0.8 or 80%) has a high chance of identifying a meaningful effect, while an underpowered study is likely to miss real effects, leading to wasted resources and missed scientific opportunities [13]. Power is not a fixed property; it is influenced by several factors:
- Effect Size: Larger, more substantial effects are easier to detect and require less power.
- Sample Size (n): Larger samples provide more reliable estimates and increase power.
- Significance Level (α): A larger α (e.g., 0.05 vs. 0.01) makes it easier to reject H₀ and thus increases power, albeit at the cost of a higher Type I error rate.
- Data Variability: Less variability in the data increases the precision of measurements and improves power.
Table 2: Summary of Error Types in Hypothesis Testing
| Decision | H₀ is TRUE | H₀ is FALSE |
|---|---|---|
| Reject H₀ | Type I Error (False Positive) Probability = α | Correct Decision Probability = 1 - β (Power) |
| Fail to Reject H₀ | Correct Decision Probability = 1 - α | Type II Error (False Negative) Probability = β |
Application in Model Validation: Protocols and Workflows
In model validation, hypothesis testing is not a one-off event but an iterative construction process that mimics the implicit process occurring in the minds of scientists [8]. Trust in a model is built progressively through the accumulated confirmations of its predictions against repeated experimental tests.
An Iterative Validation Protocol
The following workflow formalizes this dynamic process of building trust in a scientific or computational model.
Power Analysis for Validation Study Design
A critical step in the validation protocol is designing the experiment with sufficient power. Conducting a power analysis prior to data collection ensures that the study is capable of detecting a meaningful effect, safeguarding against Type II errors.
The Scientist's Toolkit: Key Reagents for Validation
The following table details essential "research reagents" and methodological components required for implementing hypothesis tests in a model validation context.
Table 3: Essential Research Reagents & Methodological Components for Validation
| Item / Component | Function / Relevance in Validation |
|---|---|
| Statistical Software (R, Python, SPSS) | Automates calculation of test statistics, p-values, and confidence intervals, reducing manual errors and ensuring reproducibility [9]. |
| Pre-Registered Analysis Plan | A detailed, publicly documented plan outlining hypotheses, primary metrics, and analysis methods before data collection. This is a critical safeguard against p-hacking and data dredging [13]. |
| A Priori Justified Alpha (α) | The pre-defined significance level, chosen based on the consequences of a Type I error in the specific research context (e.g., α=0.01 for high-stakes safety models) [9] [12]. |
| Sample Size Justification (Power Analysis) | A formal calculation, performed before the study, to determine the number of data points or experimental runs needed to achieve adequate statistical power [13]. |
| Standardized Metric Suite | Pre-defined primary, secondary, and guardrail metrics for consistent model evaluation and comparison across different validation experiments [14]. |
Common Pitfalls and Best Practices
Errors and Misinterpretations to Avoid
- P-hacking: The practice of continuously modifying data, models, or statistical tests until a statistically significant result (p < 0.05) is achieved. This massively inflates the false positive rate (Type I error) and leads to non-reproducible findings [13]. The safeguard is a pre-registered analysis plan.
- Underpowered Studies: Using a sample size that is too small to detect a meaningful effect. This results in a high probability of a Type II error, leading to the incorrect conclusion that a valid model is invalid simply because the test lacked the sensitivity to detect its accuracy [13].
- Misinterpreting 'Fail to Reject H₀': Concluding that a non-significant result (p > 0.05) proves the null hypothesis is true. It only indicates that the evidence was not strong enough to reject it; the model may still be valid but the test was inconclusive [9] [8].
- Neglecting Effect Size and Confidence Intervals: A statistically significant p-value does not indicate the magnitude or practical importance of an effect. Always report and interpret confidence intervals to understand the precision and potential real-world impact of the finding [9] [11].
Best Practices for Robust Validation
- Report Exact P-values: Instead of stating only p < 0.05, report the exact p-value (e.g., p = 0.032) to two or three decimal places, with values below 0.001 reported as p < .001. This provides more information about the strength of the evidence [9].
- Interpret P-values Alongside Other Evidence: P-values should be interpreted in the context of confidence intervals, effect sizes, study design quality, and prior replication evidence to form a reliable conclusion [9].
- Use Two-Tailed Tests by Default: Unless there is a powerful, a priori reason to expect an effect in only one direction, use two-tailed tests. This is a more conservative and generally more appropriate approach for model validation [11].
- Frame Validation as an Iterative Process: As captured in the workflow diagram, validation is not a binary "pass/fail" but a process of building trust through repeated, rigorous testing against a variety of data [8].
Definition and Core Concepts
In statistical hypothesis testing, two types of errors can occur when making a decision about the null hypothesis (H₀). A Type I error (false positive) occurs when the null hypothesis is incorrectly rejected, meaning we conclude there is an effect or difference when none exists. A Type II error (false negative) occurs when the null hypothesis is incorrectly retained, meaning we fail to detect a true effect or difference [15] [16] [17].
These errors are fundamental to understanding the reliability of statistical conclusions in research. The null hypothesis typically represents a default position of no effect, no difference, or no relationship, while the alternative hypothesis (H₁) represents the research prediction of an effect, difference, or relationship [16] [13].
Table 1: Characteristics of Type I and Type II Errors
| Characteristic | Type I Error (False Positive) | Type II Error (False Negative) |
|---|---|---|
| Statistical Definition | Rejecting a true null hypothesis | Failing to reject a false null hypothesis |
| Probability Symbol | α (alpha) | β (beta) |
| Typical Acceptable Threshold | 0.05 (5%) | 0.20 (20%) |
| Relationship to Power | - | Power = 1 - β |
| Common Causes | Overly sensitive test, small p-value by chance | Insufficient sample size, high variability, small effect size |
| Primary Control Method | Setting significance level (α) | Increasing sample size, increasing effect size |
Table 2: Comparative Examples Across Research Domains
| Application Domain | Type I Error Consequence | Type II Error Consequence |
|---|---|---|
| Medical Diagnosis | Healthy patient diagnosed as ill, leading to unnecessary treatment [15] | Sick patient diagnosed as healthy, leading to lack of treatment [15] |
| Drug Development | Concluding ineffective drug is effective, wasting resources on false lead | Failing to identify a truly effective therapeutic compound |
| Fraud Detection | Legitimate transaction flagged as fraudulent, causing customer inconvenience [15] | Fraudulent transaction missed, leading to financial loss [15] |
Mathematical Formulation and Error Trade-offs
The probabilities of Type I and Type II errors are inversely related when sample size is fixed. Reducing the risk of one typically increases the risk of the other [17].
Key metrics for evaluating these errors include:
- Significance Level (α): The probability of making a Type I error, typically set at 0.05 (5%) [17]
- Power (1-β): The probability of correctly rejecting a false null hypothesis, typically set at 0.80 (80%) or higher [17]
- Precision: TP/(TP+FP) - Measures how many positive predictions are truly positive [15]
- Recall (Sensitivity): TP/(TP+FN) - Measures how many actual positives are correctly identified [15]
Experimental Protocols for Error Control
Protocol for Controlling Type I Error Rate
Objective: Minimize false positive conclusions while maintaining adequate statistical power.
Procedure:
- Establish significance level prior to data collection (typically α = 0.05)
- Apply Bonferroni correction for multiple comparisons: divide α by the number of hypotheses tested
- Implement pre-registration of analysis plans to prevent p-hacking [13]
- Conduct a priori power analysis to determine appropriate sample size
- Use validated statistical methods with assumptions verified for the data type
Validation: Simulation studies demonstrating that under true null hypothesis, false positive rate does not exceed nominal α level.
Protocol for Controlling Type II Error Rate
Objective: Minimize false negative conclusions while maintaining controlled Type I error rate.
Procedure:
- Conduct power analysis prior to data collection to determine sample size
- Minimize measurement error through standardized protocols and calibrated instruments
- Increase effect size where possible through improved experimental design
- Consider one-tailed tests when direction of effect can be confidently predicted
- Use more sensitive statistical tests appropriate for the data distribution
Validation: Post-hoc power analysis or sensitivity analysis to determine minimum detectable effect size.
Protocol for Balanced Error Control
Objective: Balance risks of both error types based on contextual consequences.
Procedure:
- Assess relative consequences of each error type for the specific research context
- Adjust significance level based on risk assessment (may use α = 0.10, 0.05, or 0.01)
- Implement sample size calculation that considers both α and β simultaneously
- Utilize Bayesian methods where appropriate to incorporate prior knowledge
- Apply cost-benefit analysis to determine optimal balance between error risks
Visual Representation of Error Relationships
Research Reagent Solutions
Table 3: Essential Methodological Components for Error Control
| Research Component | Function in Error Control | Implementation Example |
|---|---|---|
| Power Analysis Software | Determines minimum sample size required to detect effect while controlling Type II error | G*Power, SAS POWER procedure, R pwr package |
| Multiple Comparison Correction | Controls family-wise error rate when testing multiple hypotheses, reducing Type I error inflation | Bonferroni correction, False Discovery Rate (FDR), Tukey's HSD |
| Pre-registration Platforms | Prevents p-hacking and data dredging by specifying analysis plan before data collection, controlling Type I error | Open Science Framework, ClinicalTrials.gov |
| Bayesian Analysis Frameworks | Provides alternative approach incorporating prior knowledge, offering different perspective on error trade-offs | Stan, JAGS, Bayesian structural equation modeling |
| Simulation Tools | Validates statistical power and error rates under various scenarios before conducting actual study | Monte Carlo simulation, bootstrap resampling methods |
In the scientific process, particularly in fields like drug development, hypothesis testing serves as a formal mechanism for validating models against empirical data [8]. This process involves making two competing statements about a population parameter: the null hypothesis (H0), which is the default assumption that no effect or difference exists, and the alternative hypothesis (Ha), which represents the effect or difference you aim to prove [10]. Model validation can be viewed as an iterative construction process that mimics the implicit trust-building occurring in the minds of scientists, progressively building confidence in a model's predictive capability through repeated experimental confirmation [8]. The core of this validation lies in determining whether observed differences between model predictions and experimental measurements are statistically significant or merely due to random chance, a determination made through carefully selected statistical tests [18].
Theoretical Foundations: Parametric and Non-Parametric Tests
Core Principles of Parametric Tests
Parametric statistics are methods that rely on specific assumptions about the underlying distribution of the population being studied, most commonly the normal distribution [19]. These methods estimate parameters (such as the mean (μ) and variance (σ²)) of this assumed distribution and use them for inference [20]. The power of parametric tests—their ability to detect a true effect when it exists—is maximized when their underlying assumptions are satisfied [21] [19].
Key Assumptions:
- Normality: The data originate from a population that follows a normal distribution [22] [19].
- Homogeneity of Variance: The variance within populations should be approximately equal across groups being compared [19].
- Interval/Ratio Data: The dependent variable should be measured on a continuous scale [20].
- Independence: Observations must be independent of one another [19].
Core Principles of Non-Parametric Tests
Non-parametric statistics, often termed "distribution-free" methods, do not rely on specific assumptions about the shape or parameters of the underlying population distribution [22] [19]. Instead of using the original data values, these methods often conduct analysis based on signs (+ or -) or the ranks of the data [23]. This makes them particularly valuable when data violate the stringent assumptions required for parametric tests, albeit often at the cost of some statistical power [23] [20].
Key Characteristics:
- Distribution-Free: No assumption of a specific population distribution (e.g., normality) is required [24] [22].
- Robust to Outliers: Results are not seriously affected by extreme values because they use ranks [23] [19].
- Handles Various Data Types: Applicable to ordinal, nominal, or non-normal continuous data [22] [20].
- Small Sample Usability: Can be used with very small sample sizes where parametric assumptions are impossible to verify [23].
Decision Framework: Choosing the Appropriate Test
A Structured Workflow for Test Selection
The following diagram illustrates a systematic approach to selecting the appropriate statistical test, integrating considerations of data type, distribution, and study design. This workflow ensures that the chosen test aligns with the fundamental characteristics of your data, which is a prerequisite for valid model validation.
Comparative Analysis of Statistical Tests
Table 1: Guide to Selecting Common Parametric and Non-Parametric Tests
| Research Question | Parametric Test | Non-Parametric Equivalent | Typical Use Case in Model Validation |
|---|---|---|---|
| Compare one group to a hypothetical value | One-sample t-test | Sign test / Wilcoxon signed-rank test [23] | Testing if model prediction errors are centered around zero. |
| Compare two independent groups | Independent samples t-test | Mann-Whitney U test [24] [23] | Comparing prediction accuracy between two different model architectures. |
| Compare two paired/matched groups | Paired t-test | Wilcoxon signed-rank test [24] [23] | Comparing model outputs before and after a calibration adjustment using the same dataset. |
| Compare three or more independent groups | One-way ANOVA | Kruskal-Wallis test [23] [22] | Evaluating performance across multiple versions of a simulation model. |
| Assess relationship between two variables | Pearson correlation | Spearman's rank correlation [24] [20] | Quantifying the monotonic relationship between a model's predicted and observed values. |
When to Choose Parametric vs. Non-Parametric Methods
Choose Parametric Methods If:
- Your data is approximately normally distributed [24] [20].
- The dependent variable is measured on an interval or ratio scale [20].
- Assumptions of homogeneity of variance and independence are met [20] [19].
- The goal is to estimate population parameters (e.g., mean difference) with high precision and power [21] [19].
Choose Non-Parametric Methods If:
- Your data is ordinal, nominal, or severely skewed and not normally distributed [24] [20].
- The sample size is small (e.g., n < 30) and the population distribution is unknown [24] [23].
- Your data contains significant outliers that could unduly influence parametric results [23] [19].
- Assumptions of homogeneity of variance for parametric tests are violated [20].
Experimental Protocols for Test Application
Protocol 1: Normality Testing and Data Assessment
Purpose: To objectively determine whether a dataset meets the normality assumption required for parametric tests, a critical first step in the test selection workflow.
Materials: Statistical software (e.g., R, Python with SciPy/StatsModels, PSPP, SAS).
Procedure:
- Visual Inspection: Generate graphical summaries of the data [22].
- Create a histogram with a superimposed normal curve. Assess the symmetry and bell-shape of the distribution.
- Create a Q-Q (Quantile-Quantile) plot. Data from a normal distribution will closely follow the reference line.
- Formal Normality Tests: Conduct statistical tests for normality.
- Perform the Shapiro-Wilk test (preferred for small to moderate samples) or the Kolmogorov-Smirnov test [23].
- Interpretation: A non-significant p-value (p > 0.05) suggests a failure to reject the null hypothesis of normality. A significant p-value (p < 0.05) indicates a deviation from normality.
- Assess Homogeneity of Variance: If comparing groups, test for equal variances.
- Use Levene's test or Bartlett's test.
- Interpretation: A non-significant p-value (p > 0.05) suggests homogeneity of variances is met.
Decision Logic: If both visual inspection and formal tests indicate no severe violation of normality, and group variances are equal, proceed with parametric tests. If violations are severe, proceed to non-parametric alternatives [22].
Protocol 2: Executing the Mann-Whitney U Test for Independent Groups
Purpose: To compare the medians of two independent groups when the assumption of normality for the independent t-test is violated. This is common in model validation when comparing error distributions from two different predictive models.
Materials: Dataset containing a continuous or ordinal dependent variable and a categorical independent variable with two groups; statistical software.
Procedure:
- Hypothesis Formulation:
- Null Hypothesis (H0): The distributions of the two groups are equal.
- Alternative Hypothesis (H1): The distributions of the two groups are not equal.
- Data Preparation: Ensure data is correctly formatted with one column for the dependent variable and one for the group assignment.
- Rank the Data: Combine the data from both groups and assign ranks from 1 to N (where N is the total number of observations). Average the ranks for tied values [23].
- Calculate U Statistic:
- Determine Significance:
- For large samples (typically n > 20 in each group), the U statistic is approximately normally distributed. Software will compute a Z-score and a corresponding p-value.
- For small samples, consult exact critical value tables for U.
- Interpretation:
- If the p-value is less than the chosen significance level (α, typically 0.05), reject the null hypothesis and conclude a statistically significant difference in the distributions between the two groups.
Protocol 3: Model Validation via Equivalence Testing
Purpose: To flip the burden of proof in model validation by testing the null hypothesis that the model is unacceptable, rather than the traditional null hypothesis of no difference. This is a more rigorous framework for demonstrating model validity [18].
Materials: A set of paired observations (model predictions and corresponding experimental measurements); a pre-defined "region of indifference" (δ) representing the maximum acceptable error.
Procedure:
- Define Equivalence Margin: Establish the region of indifference (δ). This is the maximum difference between model predictions and observations that is considered practically negligible. This requires domain expertise (e.g., a 5% deviation is acceptable) [18].
- Calculate Differences: For each pair (i), compute the difference:
x_di = x_observed_i - x_predicted_i[18]. - Formulate Hypotheses:
- H0: |μd| ≥ δ (The mean difference is outside the acceptable margin; the model is invalid).
- H1: |μd| < δ (The mean difference is within the acceptable margin; the model is equivalent).
- Perform Two One-Sided Tests (TOST):
- Conduct two separate one-sided t-tests.
- Test 1: H01: μd ≤ -δ vs. H11: μd > -δ
- Test 2: H02: μd ≥ δ vs. H12: μd < δ
- Construct Confidence Interval: Alternatively, construct a (1 - 2α)% confidence interval for the mean difference. For a standard α of 0.05, this is a 90% confidence interval [18].
- Decision Rule: If the entire (1 - 2α)% confidence interval lies entirely within the equivalence region [-δ, +δ], then reject the null hypothesis H0 and conclude the model is equivalent (valid) at the α significance level [18].
Table 2: Key Research Reagent Solutions for Statistical Analysis
| Item | Function | Example Tools / Notes |
|---|---|---|
| Statistical Software | Provides the computational engine to perform hypothesis tests, calculate p-values, and generate confidence intervals. | R, Python (with pandas, SciPy, statsmodels), SAS, PSPP, SPSS [23]. |
| Data Visualization Package | Enables graphical assessment of data distribution, outliers, and relationships, which is the critical first step in test selection [22]. | ggplot2 (R), Matplotlib/Seaborn (Python). |
| Normality Test Function | Objectively assesses the normality assumption, guiding the choice between parametric and non-parametric paths. | Shapiro-Wilk test, Kolmogorov-Smirnov test [23]. |
| Power Analysis Software | Determines the sample size required to detect an effect of a given size with a certain degree of confidence, preventing Type II errors. | G*Power, pwr package (R). |
| Pre-Defined Equivalence Margin (δ) | A domain-specific criterion, not a software tool, that defines the maximum acceptable error for declaring a model valid in equivalence testing [18]. | Must be defined a priori based on scientific or clinical relevance (e.g., ±10% of the mean reference value). |
Advanced Considerations in Model Validation
The Iterative Nature of Validation
It is crucial to recognize that model validation is not a single event but an iterative process of building trust [8]. Each successful statistical comparison between model predictions and new experimental data increases confidence in the model's utility and clarifies its limitations. This process mirrors the scientific method itself, where hypotheses are continuously refined based on empirical evidence [8].
Power and Error Management
The choice between parametric and non-parametric tests directly impacts a study's statistical power—the probability of correctly rejecting a false null hypothesis. When their strict assumptions are met, parametric tests are generally more powerful than their non-parametric equivalents [21] [19]. Using a parametric test on severely non-normal data, however, can lead to an increased risk of Type II errors (failing to detect a true effect) [22]. Conversely, applying a non-parametric test to normal data results in a loss of efficiency, meaning a larger sample size would be needed to achieve the same power as the corresponding parametric test [23] [20]. The workflow and protocols provided herein are designed to minimize these errors and maximize the reliability of your model validation conclusions.
In the scientific method, particularly within model validation research, hypothesis testing provides a formal framework for making decisions based on data [13]. A critical initial step in this process is the formulation of the alternative hypothesis, which can be categorized as either directional (one-tailed) or non-directional (two-tailed) [25] [26]. This choice, determined a priori, fundamentally influences the statistical power, the interpretation of results, and the confidence in the model's predictive capabilities [27]. For researchers and scientists validating complex models in fields like drug development, where extrapolation is common and risks are high, selecting the appropriate test is not merely a statistical formality but a fundamental aspect of responsible experimental design [8]. This article outlines the theoretical underpinnings and provides practical protocols for implementing these tests within a model validation framework.
Theoretical Foundations
Defining Directional and Non-Directional Hypotheses
A hypothesis is a testable prediction about the relationship between variables [26]. In statistical testing, the null hypothesis (H₀) posits that no relationship or effect exists, while the alternative hypothesis (H₁ or Ha) states that there is a statistically significant effect [28] [13].
Directional Hypothesis (One-Tailed Test): This predicts the specific direction of the expected effect [26] [28]. It is used when prior knowledge, theory, or physical limitations suggest that any effect can only occur in one direction [29] [30]. Key words include "higher," "lower," "increase," "decrease," "positive," or "negative" [28].
Non-Directional Hypothesis (Two-Tailed Test): This predicts that an effect or difference exists, but does not specify its direction [31] [26]. It is used when there is no strong prior justification to predict a direction, or when effects in both directions are scientifically interesting [27].
The following diagram illustrates the logical workflow for selecting and formulating a hypothesis type.
The Connection to One-Tailed and Two-Tailed Statistical Tests
The choice of hypothesis directly corresponds to the type of statistical test performed, which determines how the significance level (α), typically 0.05, is allocated [25] [32].
- One-Tailed Test: The entire alpha level (e.g., 0.05) is placed in a single tail of the distribution to test for an effect in one specific direction [25]. This provides greater statistical power to detect an effect in that direction because the barrier for achieving significance is lower [25] [27].
- Two-Tailed Test: The alpha level is split equally between the two tails of the distribution (e.g., 0.025 in each tail) [25]. This tests for the possibility of an effect in both directions, making it more conservative and requiring a larger sample size to achieve the same power as a one-tailed test for the same effect size [27].
Table 1: Core Differences Between One-Tailed and Two-Tailed Tests
| Feature | One-Tailed Test | Two-Tailed Test |
|---|---|---|
| Hypothesis Type | Directional [26] | Non-Directional [26] |
| Predicts Direction? | Yes [28] | No [28] |
| Alpha (α) Allocation | Entire α (e.g., 0.05) in one tail [25] | α split between tails (e.g., 0.025 each) [25] |
| Statistical Power | Higher for the predicted direction [25] [27] | Lower for a specific direction [27] |
| Risk of Missing Effect | High in the untested direction [25] | Low in either direction [27] |
| Conservative Nature | Less conservative [30] | More conservative [30] |
Decision Framework and Application Protocols
Guidelines for Choosing the Appropriate Test
Choosing between a one-tailed and two-tailed test is a critical decision that should be guided by principle, not convenience [29] [30]. The following protocol outlines the decision criteria.
When a One-Tailed Test is Appropriate: A one-tailed test is appropriate only when all of the following conditions are met [25] [29] [30]:
- Strong Directional Prediction: You have a strong theoretical, empirical, or logical basis (e.g., physical limitation) to predict the direction of the effect before looking at the data.
- Irrelevance of Opposite Effect: You can state with certainty that you would attribute an effect in the opposite direction to chance, and it would not be of scientific or practical interest. For example, testing if a new antibiotic impairs kidney function; an improvement in function is considered impossible given the drug's known mechanism [29] [30].
- A Priori Decision: The decision to use a one-tailed test is documented in the experimental protocol prior to data collection.
When a Two-Tailed Test is Appropriate (Default Choice): A two-tailed test should be used in these common situations [27] [30]:
- Exploratory Research: When there is limited or ambiguous prior evidence regarding the direction of the effect.
- Importance of Both Directions: When an effect in either direction would be meaningful and require follow-up. For instance, in A/B testing a new website feature, both a significant increase or decrease in conversion rates are critical to detect [27].
- Conservative Standard: As a default and more conservative option, especially when the consequences of a false positive (Type I error) are high [30].
When a One-Tailed Test is NOT Appropriate:
- To make a nearly significant two-tailed test become significant [25].
- When the decision is made after viewing the data to see which direction the effect went [29] [30].
- When a result in the opposite direction would still be intriguing and warrant investigation [29].
Quantitative Interpretation and p-Value Conversion
The p-value is the probability of obtaining results as extreme as the observed results, assuming the null hypothesis is true [13]. The choice of test directly impacts how this p-value is calculated and interpreted.
Table 2: p-Value Calculation and Interpretation
| Test Type | p-Value Answers the Question: | Interpretation of a Significant Result (p < α) |
|---|---|---|
| Two-Tailed | What is the chance of observing a difference this large or larger, in either direction, if H₀ is true? [29] [30] | The tested parameter is not equal to the null value. An effect exists, but its direction is not specified by the test. |
| One-Tailed | What is the chance of observing a difference this large or larger, specifically in the predicted direction, if H₀ is true? [29] [30] | The tested parameter is significantly greater than (or less than) the null value. |
For common symmetric test distributions (like the t-distribution), a simple mathematical relationship often exists between one-tailed and two-tailed p-values, provided the effect is in the predicted direction [25] [29].
- From Two-Tailed to One-Tailed: One-tailed p-value = (Two-tailed p-value) / 2 [25] [29] [30].
- From One-Tailed to Two-Tailed: Two-tailed p-value = (One-tailed p-value) * 2 [29] [30].
Example Conversion: If a two-tailed t-test yields a p-value of 0.08, the corresponding one-tailed p-value (if the effect was in the predicted direction) would be 0.04. At α=0.05, this would change the conclusion from "not significant" to "significant" [25].
Critical Note: If the observed effect is in the opposite direction to the one-tailed prediction, the one-tailed p-value is actually 1 - (two-tailed p-value / 2) [29] [30]. In this case, the result is not statistically significant for the one-tailed test, and the hypothesized effect is not supported.
Application in Model Validation Research
Framing Validation as an Iterative Hypothesis Test
In model validation, the process is not merely a single test but an iterative construction of trust, where the model is repeatedly challenged with new data [8]. The core question shifts from "Is the model true?" to "To what degree does the model accurately represent reality for its intended use?" [8]. This can be framed as a series of significance tests.
The null hypothesis (H₀) for a validation step is: "The model's predictions are not significantly different from experimental observations." The alternative hypothesis (H₁) can be either:
- Non-Directional (Two-Tailed): "The model's predictions are significantly different from the observations." This is the standard, conservative approach for general model assessment.
- Directional (One-Tailed): "The model's predictions are significantly worse (e.g., have a larger error) than the observations." This could be used in specific tuning phases where the goal is specifically to ensure the model does not exceed a certain error threshold in a particular direction.
Protocol for Validating a Predictive Model in Drug Development
This protocol provides a step-by-step methodology for integrating hypothesis testing into a model validation workflow, such as validating a pharmacokinetic (PK) model.
1. Pre-Validation Setup and Hypothesis Definition
- Define Validation Metrics: Determine the quantitative metrics for comparison (e.g., Root Mean Square Error (RMSE) between model predictions and observed plasma concentration data, Mean Absolute Percentage Error (MAPE)) [8].
- Set Acceptance Criteria: Define the clinical or scientific relevance threshold. For example, a pre-specified error margin (δ) of 15% might be the maximum acceptable deviation.
- Formalize Hypotheses:
- Null Hypothesis (H₀): The model's prediction error (e.g., RMSE) is less than or equal to the acceptance threshold (δ). (RMSE ≤ δ)
- Alternative Hypothesis (H₁): The model's prediction error is greater than the acceptance threshold (RMSE > δ). This is a directional (one-tailed) hypothesis, as you are specifically testing for the model being unacceptably bad.
- Choose Test and Document: Select the appropriate statistical test (e.g., a one-sample t-test comparing errors to δ) and document this entire protocol before accessing the validation dataset [29].
2. Experimental and Computational Execution
- Run Model Simulations: Using the fixed, trained model, generate predictions for the conditions of the hold-out validation dataset.
- Collect Observational Data: Use the pre-defined validation dataset (e.g., clinical PK data from a new trial) that was not used in model training.
3. Data Analysis and Inference
- Calculate Test Statistic: Compute the validation metric (e.g., RMSE) from the comparison of predictions and observations.
- Perform Statistical Test: Conduct the pre-specified test. For example, test if the observed RMSE is significantly greater than the δ threshold at a significance level of α=0.05.
- Interpret Results:
- If p-value < 0.05: Reject H₀. There is significant evidence that the model error exceeds the acceptable threshold. The model fails this validation step and requires refinement.
- If p-value ≥ 0.05: Fail to reject H₀. There is not enough evidence to conclude that the model is unacceptable. Trust in the model increases, and it proceeds to the next validation step [8].
4. Iterative Validation Loop
- The model undergoes multiple such validation cycles against different datasets and under different conditions, each time potentially using different metrics and hypothesis tests tailored to the intended use [8]. This iterative process progressively builds confidence in the model's predictive capabilities.
The Scientist's Toolkit: Essential Reagents for Validation Experiments
Table 3: Key Research Reagent Solutions for Model Validation
| Reagent / Material | Function in Validation Context |
|---|---|
| Validation Dataset | A hold-out dataset, not used in model training, which serves as the empirical benchmark for testing model predictions [8]. |
| Statistical Software (e.g., R, Python, Prism) | The computational environment for performing statistical tests (t-tests, etc.), calculating p-values, and generating visualizations [29] [30]. |
| Pre-Registered Protocol | A document detailing the planned analysis, including primary metrics, acceptance criteria, and statistical tests (one vs. two-tailed) before the validation exercise begins. This prevents p-hacking and confirms the a priori nature of the hypotheses [13]. |
| Reference Standard / Control | A known entity or positive control used to calibrate measurements and ensure the observational data used for validation is reliable (e.g., a standard drug compound with known PK properties). |
The judicious selection between one-tailed and two-tailed tests is a cornerstone of rigorous scientific inquiry, especially in high-stakes model validation research. A one-tailed test offers more power but should be reserved for situations with an unequivocal a priori directional prediction, where an opposite effect is negligible. For the vast majority of cases, including the general assessment of model fidelity, the two-tailed test remains the default, conservative, and recommended standard. By embedding these principles within an iterative validation framework—where models are continuously challenged with new data and pre-specified hypotheses—researchers and drug development professionals can construct robust, defensible, and trustworthy models, thereby ensuring that predictions reliably inform critical decisions.
Hypothesis testing is a formal statistical procedure for investigating ideas about the world, forming the backbone of evidence-based model validation research. In the context of drug development and scientific inquiry, it provides a structured framework to determine whether the evidence provided by data supports a specific model or validation claim. This process moves from a broad research question to a precise, testable hypothesis, and culminates in a statistical decision on whether to reject the null hypothesis. For researchers and drug development professionals, mastering this pipeline is critical for demonstrating the efficacy, safety, and performance of new models, compounds, and therapeutic interventions. The procedure ensures that conclusions are not based on random chance or subjective judgment but on rigorous, quantifiable statistical evidence [1] [33].
The core of this methodology lies in its ability to quantify the uncertainty inherent in experimental data. Whether validating a predictive biomarker, establishing the dose-response relationship of a new drug candidate, or testing a disease progression model, the principles of hypothesis testing remain consistent. This document outlines the complete workflow—from formulating a scientific question to selecting and executing the appropriate statistical test—with a specific focus on applications in pharmaceutical and biomedical research [33].
The Five-Step Hypothesis Testing Pipeline
The process of hypothesis testing can be broken down into five essential steps. These steps create a logical progression from defining the research problem to interpreting and presenting the final results [1].
Step 1: State the Null and Alternative Hypotheses
The first step involves translating the general research question into precise statistical hypotheses.
- Null Hypothesis (H₀): This is the default assumption, typically representing "no effect," "no difference," or "no relationship." In model validation, it often states that the model does not perform better than an existing standard or a random chance baseline. Example: "The new predictive model for patient stratification does not improve accuracy over the current standard of care." [1] [34]
- Alternative Hypothesis (H₁ or Ha): This is the research hypothesis that you want to prove. It is a direct contradiction of the null hypothesis. Example: "The new predictive model for patient stratification significantly improves accuracy over the current standard of care." [1] [34]
The hypotheses must be constructed before any data collection or analysis occurs to prevent bias.
Step 2: Collect Data
Data must be collected in a way that is designed to specifically test the stated hypothesis. This involves:
- Study Design: Choosing an appropriate design (e.g., randomized controlled trial, case-control study) that minimizes bias.
- Sampling: Ensuring the data are representative of the population to which you wish to make statistical inferences.
- Power Analysis: Determining the sample size required to detect a meaningful effect, if one exists, with a high probability [1].
Step 3: Perform an Appropriate Statistical Test
The choice of statistical test depends on the type of data collected and the nature of the research question. Common tests include:
- t-test: Compares the means of two groups.
- ANOVA (Analysis of Variance): Compares the means of three or more groups.
- Chi-square test: Assesses the relationship between categorical variables.
- Regression analysis: Models the relationship between a dependent variable and one or more independent variables [35] [34].
The test calculates a test statistic (e.g., t-statistic, F-statistic) which is used to determine a p-value [35].
Step 4: Decide to Reject or Fail to Reject the Null Hypothesis
This decision is made by comparing the p-value from the statistical test to a pre-determined significance level (α).
- The most common significance level is 0.05 (5%) [1].
- If p-value ≤ α: You reject the null hypothesis, concluding that the results are statistically significant. This supports the alternative hypothesis.
- If p-value > α: You fail to reject the null hypothesis. The evidence is not strong enough to support the alternative hypothesis [1] [33].
It is critical to note that "failing to reject" the null is not the same as proving it true; it simply means that the current data do not provide sufficient evidence against it [1].
Step 5: Present the Findings
The results should be presented clearly in the results and discussion sections of a research paper or report. This includes:
- A brief summary of the data and the statistical test results.
- The estimated effect size (e.g., difference between group means).
- The p-value and/or confidence interval.
- A discussion on whether the initial hypothesis was supported and the clinical or practical significance of the findings [1] [33].
The following workflow diagram encapsulates this five-step process and its application to model validation research:
Core Components of a Testable Hypothesis
A well-structured validation hypothesis is built upon several key components that ensure it is both testable and meaningful. Understanding these elements is crucial for designing a robust validation study [34].
- Null Hypothesis (H₀): The hypothesis of "no effect" or "no difference" that you aim to test against. It serves as the default or skeptical position. Example: "The new drug has the same effect on disease progression as the placebo." [1] [34]
- Alternative Hypothesis (H₁): The hypothesis that contradicts H₀. It represents the effect or relationship the researcher believes exists or hopes to prove. Example: "The new drug has a different effect on disease progression compared to the placebo." (This can be one-sided or two-sided). [1] [34]
- Significance Level (α): The threshold of probability for rejecting the null hypothesis. It is the maximum risk of a Type I error you are willing to accept. A common choice is α = 0.05, meaning a 5% risk of concluding a difference exists when there is none [1] [34].
- Test Statistic: A standardized value (e.g., t, F, χ²) calculated from sample data during a hypothesis test. It measures the degree of agreement between the sample data and the null hypothesis [35].
- P-value: The probability of obtaining test results at least as extreme as the observed results, assuming the null hypothesis is true. A small p-value (typically ≤ α) provides evidence against the null hypothesis [33] [34].
- Confidence Interval (CI): An estimated range of values that is likely to include an unknown population parameter. A 95% CI means that if the same study were repeated many times, 95% of the calculated intervals would contain the true population parameter. CIs provide information about the precision and magnitude of an effect [33].
Table 1: Core Components of a Statistical Hypothesis
| Component | Definition | Role in Model Validation | Example/Common Value |
|---|---|---|---|
| Null Hypothesis (H₀) | The default assumption of no effect, difference, or relationship. | Serves as the benchmark; the model is assumed invalid until proven otherwise. | "The new diagnostic assay has a sensitivity ≤ 90%." |
| Alternative Hypothesis (H₁) | The research claim of an effect, difference, or relationship. | The validation claim you are trying to substantiate with evidence. | "The new diagnostic assay has a sensitivity > 90%." |
| Significance Level (α) | The probability threshold for rejecting H₀. | Sets the tolerance for a Type I error (false positive). | α = 0.05 or 5% |
| P-value | Probability of the observed data (or more extreme) if H₀ is true. | Quantifies the strength of evidence against the null hypothesis. | p = 0.03 (leads to rejection of H₀ at α=0.05) |
| Confidence Interval (CI) | A range of plausible values for the population parameter. | Provides an estimate of the effect size and the precision of the measurement. | 95% CI for a difference: 1.9 to 7.8 |
Selecting the Appropriate Statistical Test
Choosing the correct statistical test is fundamental to drawing valid conclusions. The choice depends primarily on the type of data (categorical or continuous) and the study design (e.g., number of groups, paired vs. unpaired observations) [35] [34].
The following diagram illustrates the decision-making process for selecting a common statistical test based on these factors:
Table 2: Guide to Selecting a Statistical Test for Model Validation
| Research Question Scenario | Outcome Variable Type | Number of Groups / Comparisons | Recommended Statistical Test | Example in Drug Development |
|---|---|---|---|---|
| Compare a single group to a known standard. | Continuous | One sample vs. a theoretical value | One-Sample t-test | Compare the mean IC₅₀ of a new compound to a value of 10μM. |
| Compare the means of two independent groups. | Continuous | Two independent groups | Independent (Unpaired) t-test | Compare tumor size reduction between treatment and control groups in different animals. |
| Compare the means of two related groups. | Continuous | Two paired/matched groups | Paired t-test | Compare blood pressure in the same patients before and after treatment. |
| Compare the means of three or more independent groups. | Continuous | Three or more independent groups | One-Way ANOVA | Compare the efficacy of three different drug doses and a placebo. |
| Assess the association between two categorical variables. | Categorical | Two or more categories | Chi-Square Test | Test if the proportion of responders is independent of genotype. |
| Model the relationship between multiple predictors and a continuous outcome. | Continuous & Categorical | Multiple independent variables | Linear Regression | Predict drug clearance based on patient weight, age, and renal function. |
| Model the probability of a binary outcome. | Categorical (Binary) | Multiple independent variables | Logistic Regression | Predict the probability of disease remission based on biomarker levels. |
When comparing quantitative data between groups, a clear summary is essential. This involves calculating descriptive statistics for each group and the key metric of interest: the difference between groups (e.g., difference between means). Note that measures like standard deviation or sample size do not apply to the difference itself [36].
Table 3: Template for Quantitative Data Summary in Group Comparisons
| Group | Mean | Standard Deviation | Sample Size (n) | Median | Interquartile Range (IQR) |
|---|---|---|---|---|---|
| Group A (e.g., Experimental) | Value | Value | Value | Value | Value |
| Group B (e.g., Control) | Value | Value | Value | Value | Value |
| Difference (A - B) | Value | - | - | - | - |
Table 4: Example Data - Gorilla Chest-Beating Rate (beats per 10 h) [36]
| Group | Mean | Standard Deviation | Sample Size (n) |
|---|---|---|---|
| Younger Gorillas | 2.22 | 1.270 | 14 |
| Older Gorillas | 0.91 | 1.131 | 11 |
| Difference | 1.31 | - | - |
Experimental Protocol: A Sample Framework for In Vitro Drug Validation
This protocol outlines a hypothetical experiment to validate the efficacy of a new anti-cancer drug candidate in a cell culture model, following the hypothesis testing framework.
Hypothesis Formulation
- Research Question: Does the novel compound 'Drug X' reduce the viability of human breast cancer cells (MCF-7 line) more effectively than the current standard of care, 'Drug S'?
- Null Hypothesis (H₀): The mean cell viability after 72 hours of treatment with Drug X is greater than or equal to the mean cell viability after treatment with Drug S. (μ_Drug X ≥ μ_Drug S)
- Alternative Hypothesis (H₁): The mean cell viability after 72 hours of treatment with Drug X is less than the mean cell viability after treatment with Drug S. (μ_Drug X < μ_Drug S)
- Significance Level (α): Set at 0.05.
Experimental Design and Data Collection
- Cell Culture: Human breast cancer cell line MCF-7, maintained in standard conditions.
- Treatment Groups:
- Control Group: Vehicle control (e.g., DMSO).
- Standard Drug Group: Treated with Drug S at its IC₅₀ concentration.
- Experimental Group: Treated with Drug X at its IC₅₀ concentration.
- Experimental Units: 30 independent cell culture wells per group (n=30).
- Outcome Measure: Cell viability assessed after 72 hours of treatment using a colorimetric assay (e.g., MTT assay). The result is a continuous variable (optical density, OD).
Data Analysis and Statistical Testing
- Summary Statistics: Calculate the mean and standard deviation of cell viability (OD) for each group. Present in a table as in Table 3.
- Statistical Test Selection:
- Objective: Compare the means of three independent groups.
- Test Chosen: One-Way ANOVA.
- Post-hoc Test: If the ANOVA is significant, a post-hoc test (e.g., Tukey's HSD) will be used to make specific comparisons between Drug X and Drug S, and each drug against the control.
- Software: Analysis will be performed using a statistical software package (e.g., R, GraphPad Prism).
Decision and Interpretation
- The p-value from the ANOVA (and post-hoc tests) will be compared to α=0.05.
- If p ≤ 0.05: Reject the null hypothesis. Conclude that there is a statistically significant difference in cell viability between the treatment groups.
- If p > 0.05: Fail to reject the null hypothesis. Conclude that there is not enough evidence to say the drugs differ in their effect on cell viability under these experimental conditions.
- Reporting: Report the F-statistic, degrees of freedom, p-value, and effect sizes (e.g., mean differences with 95% confidence intervals).
The Scientist's Toolkit: Essential Reagents and Materials
Table 5: Key Research Reagent Solutions for Biochemical Validation Assays
| Reagent / Material | Function / Application in Validation |
|---|---|
| Cell Viability Assay Kits (e.g., MTT, WST-1) | Colorimetric assays to quantify metabolic activity, used as a proxy for the number of viable cells in culture. Critical for in vitro efficacy testing. |
| ELISA Kits | Enzyme-linked immunosorbent assays used to detect and quantify specific proteins (e.g., biomarkers, cytokines) in complex samples like serum or cell lysates. |
| Validated Antibodies (Primary & Secondary) | Essential for techniques like Western Blot and Immunohistochemistry to detect specific protein targets and confirm expression levels or post-translational modifications. |
| qPCR Master Mix | Pre-mixed solutions containing enzymes, dNTPs, and buffers required for quantitative polymerase chain reaction (qPCR) to measure gene expression. |
| LC-MS Grade Solvents | High-purity solvents for Liquid Chromatography-Mass Spectrometry (LC-MS), used for metabolite or drug compound quantification, ensuring minimal background interference. |
| Stable Cell Lines | Genetically engineered cells that consistently express (or silence) a target gene of interest, providing a standardized system for functional validation studies. |
| Reference Standards / Controls | Compounds or materials with known purity and activity, used to calibrate instruments and validate assay performance across multiple experimental runs. |
Practical Methods and Statistical Tests for Validating Predictive Models
In model validation research, particularly within pharmaceutical development, selecting the appropriate statistical test is fundamental to ensuring research validity and generating reliable, interpretable results. Hypothesis testing provides a structured framework for making quantitative decisions about model performance, helping researchers distinguish genuine effects from random noise [13]. This structured approach to statistical validation is especially critical in drug development, where decisions impact clinical trial strategies, portfolio management, and ultimately, patient outcomes [37] [38].
The core principle of hypothesis testing involves formulating two competing statements: the null hypothesis (H₀), which represents the default position of no effect or no difference, and the alternative hypothesis (H₁), which asserts the presence of a significant effect or relationship [34] [13]. By collecting sample data and calculating the probability of observing the results if the null hypothesis were true (the p-value), researchers can make evidence-based decisions to either reject or fail to reject the null hypothesis [13]. This process minimizes decision bias and provides a quantifiable measure of confidence in research findings, which is indispensable for validating predictive models, assessing algorithm performance, and optimizing development pipelines.
A Decision Framework for Statistical Test Selection
The following decision framework provides a systematic approach for researchers to select the most appropriate statistical test based on their research question, data types, and underlying assumptions. This framework synthesizes key decision points into a logical flowchart, supported by detailed parameter tables.
Statistical Test Selection Decision Tree
The diagram below maps the logical pathway for selecting an appropriate statistical test based on your research question and data characteristics. Follow the decision points from the top node to arrive at a recommended test.
Statistical Test Specifications and Applications
Table 1: Key Statistical Tests for Research Model Validation
| Statistical Test | Data Requirements | Common Research Applications | Key Assumptions |
|---|---|---|---|
| Student's t-test [13] [39] | Continuous dependent variable, categorical independent variable with 2 groups | Comparing model performance metrics between two algorithms; Testing pre-post intervention effects | Normality, homogeneity of variance, independent observations |
| One-way ANOVA [13] [39] | Continuous dependent variable, categorical independent variable with 3+ groups | Comparing multiple treatment groups or model variants simultaneously | Normality, homogeneity of variance, independent observations |
| Chi-square test [13] [39] | Two categorical variables | Testing independence between classification outcomes; Validating contingency tables | Adequate sample size, independent observations, expected frequency >5 per cell |
| Mann-Whitney U test [13] [39] | Ordinal or continuous data that violates normality | Comparing two independent groups when parametric assumptions are violated | Independent observations, ordinal measurement scale |
| Pearson correlation [13] [39] | Two continuous variables | Assessing linear relationship between predicted and actual values; Feature correlation analysis | Linear relationship, bivariate normality, homoscedasticity |
| Linear regression [13] [39] | Continuous dependent variable, continuous or categorical independent variables | Modeling relationship between model parameters and outcomes; Predictive modeling | Linearity, independence, homoscedasticity, normality of residuals |
| Logistic regression [13] [39] | Binary or categorical dependent variable, various independent variables | Classification model validation; Risk probability estimation | Linear relationship between log-odds and predictors, no multicollinearity |
Table 2: Advanced Statistical Tests for Complex Research Designs
| Statistical Test | Data Requirements | Common Research Applications | Key Assumptions |
|---|---|---|---|
| Repeated Measures ANOVA [39] | Continuous dependent variable measured multiple times | Longitudinal studies; Time-series model validation; Within-subject designs | Sphericity, normality of residuals, no outliers |
| Wilcoxon signed-rank test [13] [39] | Paired ordinal or non-normal continuous data | Comparing matched pairs or pre-post measurements without parametric assumptions | Paired observations, ordinal measurement |
| Kruskal-Wallis test [13] [39] | Ordinal or non-normal continuous data with 3+ groups | Comparing multiple independent groups when parametric assumptions are violated | Independent observations, ordinal measurement |
| Spearman correlation [13] [39] | Ordinal or continuous variables with monotonic relationships | Assessing non-linear but monotonic relationships; Rank-based correlation analysis | Monotonic relationship, ordinal measurement |
| Multinomial logistic regression [39] | Categorical dependent variable with >2 categories | Multi-class classification model validation; Nominal outcome prediction | Independence of irrelevant alternatives, no multicollinearity |
Experimental Protocols for Statistical Validation
Protocol 1: Model Comparison Validation Framework
This protocol provides a standardized methodology for comparing the performance of multiple machine learning models or analytical approaches, which is fundamental to model validation research.
Objective: To determine whether performance differences between competing models are statistically significant rather than attributable to random variation.
Materials and Reagents:
- Pre-processed dataset with appropriate train-test splits
- Computational environment (R, Python, or specialized statistical software)
- Implemented model algorithms for comparison
- Performance evaluation metrics (accuracy, precision, recall, F1-score, AUC-ROC, etc.)
Procedure:
- Formulate Hypotheses:
- Null Hypothesis (H₀): No significant difference exists between model performance metrics
- Alternative Hypothesis (H₁): A significant difference exists between model performance metrics [13]
Experimental Design:
- Implement k-fold cross-validation (typically k=5 or k=10) to generate multiple performance estimates [40]
- Ensure identical training and test splits across all compared models
- Record performance metrics for each fold and model combination
Test Selection:
- For comparing two models: Use paired t-test if performance metrics are normally distributed, or Wilcoxon signed-rank test for non-normal distributions [13]
- For comparing three or more models: Use repeated measures ANOVA if parametric assumptions are met, or Friedman test for non-parametric alternatives [13]
Implementation:
- Calculate performance differences for each cross-validation fold
- Check normality assumption using Shapiro-Wilk test or visual inspection of Q-Q plots
- Execute appropriate statistical test with significance level α=0.05 unless otherwise justified
Interpretation:
- If p-value < α, reject H₀ and conclude significant performance differences
- Report effect size measures (Cohen's d for t-tests, η² for ANOVA) to quantify magnitude of differences
- Conduct post-hoc analyses if comparing multiple models to identify specific pairwise differences
Validation Criteria:
- Statistical power >0.8, confirmed through power analysis during experimental design
- Control for family-wise error rate when conducting multiple comparisons using Bonferroni or Holm correction
- Confidence intervals for performance differences to assess practical significance
Protocol 2: Feature Significance Assessment Protocol
This protocol establishes a rigorous methodology for determining whether specific features or variables significantly contribute to model predictions, which is essential for model interpretability and validation.
Objective: To validate the statistical significance of individual features in predictive models and assess their contribution to model performance.
Materials and Reagents:
- Trained predictive model (regression, classification, or survival analysis)
- Feature importance metrics (coefficients, information gain, permutation importance)
- Statistical computing environment with appropriate libraries
Procedure:
- Hypothesis Formulation:
- For linear models: H₀: Coefficient βᵢ = 0 vs. H₁: Coefficient βᵢ ≠ 0
- For feature importance: H₀: Feature contributes no predictive power vs. H₁: Feature significantly improves predictions [13]
Test Selection Based on Model Type:
- Linear/logistic regression: Wald test or likelihood ratio test for coefficient significance [13]
- Tree-based models: Permutation importance with statistical significance assessed via paired tests
- General feature selection: ANOVA F-test for continuous outcomes, chi-square for categorical outcomes [13]
Experimental Execution:
- For regression models, extract coefficient estimates and standard errors
- Calculate test statistics (t-statistic for coefficients, F-statistic for nested models)
- Compare test statistics to appropriate theoretical distributions
- Compute p-values and compare to significance threshold
Multiple Testing Correction:
- Apply false discovery rate (FDR) control when testing multiple features simultaneously
- Use Bonferroni correction for strongly controlled family-wise error rate
- Report adjusted p-values alongside unadjusted values
Effect Size Reporting:
- Calculate confidence intervals for coefficients and importance scores
- Compute standardized effect sizes (standardized coefficients, Cohen's f²)
- Document practical significance alongside statistical significance
Validation Criteria:
- Minimum effect size of practical interest determined a priori
- Power analysis to ensure adequate sample size for detecting meaningful effects
- Verification that model assumptions are satisfied (linearity, independence, homoscedasticity where applicable)
Research Reagent Solutions for Statistical Analysis
Table 3: Essential Analytical Tools for Statistical Test Implementation
| Tool/Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Statistical Software | R, Python (scipy.stats), SPSS, SAS | Implement statistical tests and calculate p-values | General statistical analysis across all research domains |
| Specialized Pharmaceutical Tools | PrecisionTree, @RISK [37] | Decision tree analysis and risk assessment for clinical trial sequencing | Pharmaceutical indication sequencing, portfolio optimization |
| Data Mining Platforms | WEKA (J48 algorithm) [41] | Classification and decision tree implementation | Adverse drug reaction signal detection, pattern identification |
| Hypothesis Testing Services | A/B testing platforms, CRO services [34] | Structured experimentation for conversion optimization | Marketing optimization, user experience research |
| Large Language Models | Claude, ChatGPT, Gemini [39] | Statistical test selection assistance and explanation | Educational support, analytical workflow guidance |
Advanced Applications in Pharmaceutical Research
Decision Tree Analysis for Clinical Development Optimization
Decision tree methodologies provide powerful frameworks for structuring complex sequential decisions under uncertainty, which is particularly valuable in pharmaceutical development planning.
Implementation Framework: The diagram below illustrates a decision tree structure for clinical trial sequencing, adapted from pharmaceutical indication sequencing applications where multiple development pathways must be evaluated.
This decision tree structure enables pharmaceutical researchers to quantify development strategies by incorporating probabilities of technical success and risk-adjusted net present value calculations, facilitating data-driven portfolio decisions [37].
Statistical Framework for Adverse Drug Reaction Signal Detection
In pharmacovigilance and drug safety research, statistical tests are employed to detect signals from spontaneous reporting systems, requiring specialized methodologies to address challenges like masking effects and confounding factors.
Stratification Methodology: Decision tree-based stratification approaches have demonstrated superior performance in minimizing masking effects in adverse drug reaction detection. The J48 algorithm (C4.5 implementation) can be employed to stratify data based on patient demographics (age, gender) and drug characteristics (antibiotic status), significantly improving signal detection precision and recall compared to non-stratified approaches [41].
Key Statistical Measures:
- Proportional Reporting Ratio (PRR): Measures disproportionate reporting of specific drug-event combinations
- Reporting Odds Ratio (ROR): Case-control approach for signal detection
- Information Component (IC): Bayesian confidence propagation neural network measure
The integration of decision tree stratification with these disproportionality measures has shown statistically significant improvements in signal detection performance, particularly for databases with heterogeneous reporting patterns [41].
This framework provides a comprehensive methodology for selecting and applying statistical tests within model validation research, with particular relevance to pharmaceutical and drug development applications. By integrating classical hypothesis testing principles with specialized applications like clinical trial optimization and safety signal detection, researchers can enhance the rigor and interpretability of their analytical workflows. The structured decision pathways, experimental protocols, and specialized reagent tables offer practical guidance for implementing statistically sound validation approaches across diverse research scenarios. As statistical methodology continues to evolve, particularly with the integration of machine learning approaches and large language model assistance, maintaining foundational principles of hypothesis testing remains essential for generating valid, reproducible research outcomes.
Within the rigorous framework of hypothesis testing for model validation research, selecting the optimal machine learning algorithm is a critical step that extends beyond simply comparing average performance metrics. Standard evaluation methods, such as k-fold cross-validation, can be misleading because the performance estimates obtained from different folds are not entirely independent. This lack of independence violates a key assumption of the standard paired Student's t-test, potentially leading to biased and over-optimistic results [42] [43].
The 5x2 cross-validation paired t-test, introduced by Dietterich (1998), provides a robust solution to this problem [44] [43]. This method is designed to deliver a more reliable statistical comparison of two models by structuring the resampling procedure to provide better variance estimates and mitigate the issues of non-independent performance measures. This protocol details the application of the 5x2cv paired t-test, providing researchers and development professionals with a rigorous tool for model selection.
Theoretical Foundation
The Problem with Simple Performance Comparisons
In applied machine learning, a model's performance is typically estimated using resampling techniques like k-fold cross-validation. When comparing two models, Algorithm A and Algorithm B, a common practice is to train and evaluate them on the same k data splits, resulting in k paired performance differences. A naive application of the paired Student's t-test on these differences is problematic because the training sets in each fold overlap significantly. This means the performance measurements are not independent, as each data point is used for training (k-1) times, violating the core assumption of the test [43]. This violation can inflate the Type I error rate, increasing the chance of falsely concluding that a performance difference exists [44] [43].
The 5x2 Cross-Validation Solution
The 5x2cv procedure addresses this by reducing the dependency between training sets. The core innovation lies in its specific resampling design: five replications of a 2-fold cross-validation [44]. In each replication, the dataset is randomly split into two equal-sized subsets, S1 and S2. Each model is trained on S1 and tested on S2, and then trained on S2 and tested on S1. This design ensures that for each of the five replications, the two resulting performance estimates are based on entirely independent test sets [43]. A modified t-statistic is then calculated, which accounts for the limited degrees of freedom and provides a more conservative and reliable test.
The 5x2CV Paired t-Test Protocol
Formal Procedure and Statistical Formulae
The following steps outline the complete 5x2cv paired t-test methodology. The procedure results in 10 performance estimates for each model (5 iterations × 2 folds).
Procedure:
- For ( i = 1 ) to ( 5 ):
- Randomly split the dataset ( D ) into two equal-sized subsets, ( S1 ) and ( S2 ).
- Train Algorithm A on ( S1 ) and test on ( S2 ). Record performance score ( p^{(1)}A ).
- Train Algorithm A on ( S2 ) and test on ( S1 ). Record performance score ( p^{(2)}A ).
- Repeat steps 2-3 for Algorithm B, obtaining ( p^{(1)}B ) and ( p^{(2)}B ).
- Calculate the performance differences for the two folds:
- ( d^{(1)} = p^{(1)}A - p^{(1)}B )
- ( d^{(2)} = p^{(2)}A - p^{(2)}B )
- Calculate the mean difference for the iteration: ( \bar{d}_i = (d^{(1)} + d^{(2)}) / 2 ).
- Calculate the variance of the differences for the iteration: ( s^2i = (d^{(1)} - \bar{d}i)^2 + (d^{(2)} - \bar{d}i)^2 ). Note: This is a sum of squared deviations, so the estimated variance for the replication is ( s^2i / 2 ).
The t-statistic is then computed as defined by Dietterich: [ t = \frac{d^{(1)}1}{\sqrt{\frac{1}{5} \sum{i=1}^{5} s^2i}} ] Here, ( d^{(1)}1 ) is the performance difference from the first fold of the first replication.
This t-statistic follows approximately a t-distribution with 5 degrees of freedom under the null hypothesis. The corresponding p-value can be derived from this distribution [44].
Experimental Workflow
The following diagram illustrates the logical flow and data handling in the 5x2cv paired t-test protocol.
Quantitative Data and Interpretation
The final step is the statistical decision. The null hypothesis ((H0)) states that the performance of the two models is identical. The alternative hypothesis ((H1)) states that their performance is different.
- Interpretation Rule: Reject the null hypothesis if the p-value is less than or equal to your chosen significance level (alpha, typically α = 0.05). This indicates a statistically significant difference in model performance [44] [45]. If the p-value is greater than alpha, you fail to reject the null hypothesis, suggesting no significant difference was detected.
The table below summarizes the possible outcomes of the test.
Table 1: Interpretation of the 5x2cv Paired t-Test Results
| p-value | Comparison with Alpha (α=0.05) | Statistical Conclusion | Practical Implication |
|---|---|---|---|
p ≤ 0.05 |
Less than or equal to alpha | Reject the null hypothesis (H₀) | A statistically significant difference exists between the two models' performance [44]. |
p > 0.05 |
Greater than alpha | Fail to reject the null hypothesis (H₀) | There is no statistically significant evidence that the models perform differently [44]. |
Practical Application Guide
Implementation with MLxtend
The mlxtend library in Python provides a direct implementation of the 5x2cv paired t-test, simplifying its application. Below is a prototypical code example for comparing a Logistic Regression model and a Decision Tree classifier on a synthetic dataset.
The Scientist's Toolkit
The following table details the essential software "reagents" required to implement the 5x2cv paired t-test.
Table 2: Key Research Reagent Solutions for 5x2cv Testing
| Research Reagent | Function in the Protocol | Typical Specification / Example |
|---|---|---|
| Python (with SciPy stack) | Provides the core programming environment for data handling, model training, and statistical computing. | Python 3.x, NumPy, SciPy |
| Scikit-learn | Offers the machine learning algorithms (estimators) to be compared, data preprocessing utilities, and fundamental data resampling tools. | LogisticRegression, DecisionTreeClassifier, train_test_split |
| MLxtend (Machine Learning Extensions) | Contains the dedicated function paired_ttest_5x2cv that implements the complete statistical testing procedure as defined by Dietterich [44]. |
mlxtend.evaluate.paired_ttest_5x2cv |
| Statistical Significance Level (Alpha) | A pre-defined probability threshold that determines the criterion for rejecting the null hypothesis. It quantifies the tolerance for Type I error (false positives) [45]. | α = 0.05 (5%) |
Statistical Decision Framework
Once the t-statistic and p-value are computed, researchers must follow a strict decision-making process to interpret the results. The following flowchart outlines this process, emphasizing the connection between the quantitative output of the test and the final research conclusion.
Discussion and Best Practices
When to Use the 5x2cv Test
The 5x2cv paired t-test is particularly well-suited for scenarios where the computational cost of model training is manageable, allowing for the ten training cycles required by the procedure [43]. It is a robust method for comparing two models on a single dataset, especially when the number of available data samples is not extremely large. For classification problems, it is typically applied on performance metrics like accuracy or error rate.
Limitations and Alternatives
No statistical test is universally perfect. A key consideration is that the 5x2cv test may have lower power (higher Type II error rate) compared to tests using more resamples, such as a 10-fold cross-validation with a corrected t-test, because it uses only half the data for training in each fold [43].
Researchers should be aware of alternative tests, which may be preferable in certain situations:
- McNemar's Test: Ideal when models are very expensive to train and can be evaluated only once on a single, held-out test set [43]. It is a non-parametric test performed on the contingency table of model disagreements.
- Wilcoxon Signed-Rank Test: A non-parametric alternative to the paired t-test that does not assume normally distributed differences. It can be applied to the results of multiple cross-validation runs and is often recommended for comparing machine learning algorithms [46].
In conclusion, the 5x2 cross-validation paired t-test is a cornerstone of rigorous model validation. It provides a statistically sound framework for moving beyond simple performance comparisons, enabling data scientists and researchers to make confident, evidence-based decisions in the model selection process, which is paramount in high-stakes fields like drug development.
Implementing T-tests and ANOVA for Comparing Group Means and Model Performance
In model validation research, hypothesis testing provides a statistical framework for making objective, data-driven decisions, moving beyond intuition to rigorously test assumptions and compare model performance [13]. This process is fundamental for establishing causality rather than just correlation, forming the backbone of a methodical experimental approach [13]. For researchers and scientists in drug development, these methods validate whether observed differences in model outputs or group means are statistically significant or likely due to random chance.
The core procedure involves stating a null hypothesis (H₀), typically positing no effect or no difference, and an alternative hypothesis (H₁) that a significant effect does exist [13]. By collecting sample data and calculating a test statistic, one can determine the probability (p-value) of observing the results if the null hypothesis were true. A p-value below a predetermined significance level (α, usually 0.05) provides evidence to reject the null hypothesis [47].
Table 1: Key Terminologies in Hypothesis Testing
| Term | Definition | Role in Model Validation |
|---|---|---|
| Null Hypothesis (H₀) | Default position that no significant effect/relationship exists [13] | Assumes no real difference in model performance or group means |
| Alternative Hypothesis (H₁) | Contrasting hypothesis that a significant effect/relationship exists [13] | Assumes a real, statistically significant difference is present |
| Significance Level (α) | Probability threshold for rejecting H₀ (usually 0.05) [13] | Defines the risk tolerance for a false positive (Type I error) |
| p-value | Probability of obtaining the observed results if H₀ is true [13] | Quantifies the strength of evidence against the null hypothesis |
| Type I Error (α) | Incorrectly rejecting a true H₀ (false positive) [13] | Concluding a model or treatment works when it does not |
| Type II Error (β) | Failing to reject a false H₀ (false negative) [13] | Failing to detect a real improvement in a model or treatment |
| Power (1-β) | Probability of correctly rejecting H₀ when H₁ is true [13] | The ability of the test to detect a real effect when it exists |
Foundational Statistical Tests
The t-Test
The t-test is a parametric method used to evaluate the means of one or two populations [48]. It is based on means and standard deviations and assumes that the sample data come from a normally distributed population, the data are continuous, and, for the independent two-sample test, that the populations have equal variances and independent measurements [47] [48].
Table 2: Types of t-Tests and Their Applications
| Test Type | Number of Groups | Purpose | Example Application in Model Validation |
|---|---|---|---|
| One-Sample t-test | One | Compare a sample mean to a known or hypothesized value [48] | Testing if a new model's mean accuracy is significantly different from a benchmark value (e.g., 90%) [48] |
| Independent Two-Sample t-test | Two (Independent) | Compare means from two independent groups [48] | Comparing the performance (e.g., RMSE) of two different models on different test sets [47] |
| Paired t-test | Two (Dependent) | Compare means from two related sets of measurements [48] | Comparing the performance of the same model before and after fine-tuning on the same test set [47] |
The test statistic for a one-sample t-test is calculated as ( t = \frac{\bar{x} - \mu}{s / \sqrt{n}} ), where ( \bar{x} ) is the sample mean, ( \mu ) is the hypothesized population mean, ( s ) is the sample standard deviation, and ( n ) is the sample size [47]. For an independent two-sample t-test, the formula extends to ( t = \frac{\bar{x1} - \bar{x2}}{sp \sqrt{\frac{1}{n1} + \frac{1}{n2}}} ), where ( sp ) is the pooled standard deviation [47].
Analysis of Variance (ANOVA)
When comparing means across three or more groups, using multiple t-tests inflates the probability of a Type I error [47]. Analysis of Variance (ANOVA) is the appropriate parametric test for this scenario, extending the two-sample t-test to multiple groups [47]. It shares the same assumptions: normal distribution of data, homogeneity of variances, and independent measurements [47].
ANOVA works by dividing the total variation in the data into two components: the variation between the group means and the variation within the groups (error) [47]. It tests the null hypothesis that all group means are equal (( H0: \mu1 = \mu2 = ... = \muk )) against the alternative that at least one is different.
The test statistic is an F-ratio, calculated as ( F = \frac{\text{between-groups variance}}{\text{within-group variance}} ) [47]. A significantly large F-value indicates that the variability between groups is greater than the variability within groups, providing evidence against the null hypothesis.
Experimental Protocols and Workflows
Protocol for an Independent Two-Sample t-Test
Objective: To determine if a statistically significant difference exists between the means of two independent groups.
Step-by-Step Procedure:
- Formulate Hypotheses:
- ( H0: \mu1 = \mu2 ) (The population means of Group 1 and Group 2 are equal).
- ( H1: \mu1 \neq \mu2 ) (The population means of Group 1 and Group 2 are not equal) [49].
- Check Assumptions:
- Set Significance Level: Typically, α = 0.05 [13].
- Calculate Test Statistic: Use the formula for the independent two-sample t-test [47].
- Determine p-value and Conclude: Compare the p-value to α. If p-value ≤ α, reject H₀. Otherwise, fail to reject H₀ [49].
Protocol for a One-Way ANOVA
Objective: To determine if statistically significant differences exist among the means of three or more independent groups.
Step-by-Step Procedure:
- Formulate Hypotheses:
- ( H0: \mu1 = \mu2 = ... = \muk ) (All k population means are equal).
- ( H_1: ) At least one population mean is different [47].
- Check Assumptions: Same as t-test: Normality, Homogeneity of Variances, and Independence [47].
- Set Significance Level: α = 0.05.
- Calculate Test Statistic: Compute the F-ratio from the between-groups and within-group variances [47].
- Determine p-value and Conclude: If p-value ≤ α, reject H₀, indicating at least one group mean is different.
- Post-Hoc Analysis: If H₀ is rejected, conduct post-hoc tests (e.g., Tukey's HSD) to identify which specific groups differ [48].
The Scientist's Toolkit: Research Reagents and Materials
Table 3: Essential Reagents and Tools for Statistical Analysis
| Item / Tool | Function / Purpose | Example / Note |
|---|---|---|
| Statistical Software (R, Python, JMP) | Performs complex calculations, generates test statistics, and computes p-values accurately [49] | R with t.test() and aov() functions; Python with scipy.stats and statsmodels |
| Normality Test | Assesses if data meets the normality assumption for parametric tests [47] | Shapiro-Wilk test or Kolmogorov-Smirnov test |
| Test for Equal Variances | Checks the homogeneity of variances assumption for t-tests and ANOVA [47] | Levene's test or F-test |
| Non-Parametric Alternatives | Used when data violates normality or other assumptions [13] | Mann-Whitney U (instead of t-test), Kruskal-Wallis (instead of ANOVA) |
| Post-Hoc Test | Identifies which specific groups differ after a significant ANOVA result [48] | Tukey's Honest Significant Difference (HSD) test |
Application in Model Validation Research
Validating Predictive Algorithms
In machine learning, hypothesis testing is crucial for objectively comparing model performance. A typical application involves using a paired t-test to compare the accuracy, precision, or RMSE (Root Mean Square Error) of two different algorithms on multiple, matched test sets or via cross-validation folds [13]. This determines if a observed performance improvement is statistically significant and not due to random fluctuations.
Case Study: Comparing Multiple Drug Response Models
A research group develops three new models (A, B, and C) to predict drug response based on genomic data. They need to validate which model performs best by comparing their mean R-squared (R²) values across 50 different validation studies.
Procedure:
- State Hypotheses: H₀: Mean R² is equal for all models (μA = μB = μ_C). H₁: At least one model's mean R² is different.
- Check Assumptions: Test the distribution of R² values for each model for normality and homogeneity of variance.
- Conduct One-Way ANOVA: The analysis yields an F-statistic of 8.95 with a p-value of 0.0003.
- Interpret Results: Since the p-value (0.0003) is less than α (0.05), the null hypothesis is rejected.
- Post-Hoc Analysis: A Tukey's HSD test reveals that the mean R² of Model C is significantly higher than both Model A and Model B, which are not significantly different from each other.
This structured approach provides statistically sound evidence for selecting Model C as the superior predictive tool.
Common Errors to Avoid
- P-hacking: The practice of continuously modifying data or statistical methods until a desired "significant" p-value is obtained. This artificially inflates the Type I error rate and leads to false conclusions [13].
- Underpowered Studies: Using sample sizes that are too small increases the likelihood of a Type II error, where a true effect is missed. Researchers should perform power analysis before finalizing study designs [13].
- Violating Test Assumptions: Applying t-tests or ANOVA to data that severely violates assumptions (e.g., non-normal, unequal variances) can invalidate the results. Always check assumptions and consider robust or non-parametric alternatives if needed [13] [47].
- Multiple Comparisons Problem: Conducting many hypothesis tests without adjustment increases the chance of false positives. When making numerous comparisons, use corrective procedures like the Bonferroni correction or false discovery rate control [13].
Using Chi-Square Tests for Categorical Outcomes and Goodness-of-Fit
Within the framework of hypothesis testing for model validation research, the Chi-Square Test serves as a fundamental statistical tool for assessing the validity of categorical data models. For researchers, scientists, and drug development professionals, it provides a mathematically rigorous method to determine if observed experimental outcomes significantly deviate from the frequencies predicted by a theoretical model. The test's foundation was laid by Karl Pearson in 1900, and it has since become a cornerstone for analyzing categorical data in fields ranging from genetics to pharmaceutical research [50] [51].
The core principle of the Chi-Square test involves comparing observed frequencies collected from experimental data against expected frequencies derived from a null hypothesis model. The resulting test statistic follows a Chi-Square distribution, which allows for quantitative assessment of the model's fit. The formula for the test statistic is expressed as follows [52] [51]:
$$\chi^2 = \sum \frac{(Oi - Ei)^2}{E_i}$$
where:
- (O_i) = Observed frequency in cell i
- (E_i) = Expected frequency in cell i
For model validation research, this test offers an objective mechanism to either substantiate a proposed model or identify significant discrepancies that warrant model refinement. Its application is particularly valuable in pharmaceutical research and clinical trial design, where validating assumptions about categorical outcomes—such as treatment response rates or disease severity distributions—is critical for robust scientific conclusions [50].
Core Test Types and Applications
Chi-Square Goodness-of-Fit Test
The Goodness-of-Fit Test is employed when researchers need to validate whether a single categorical variable follows a specific theoretical distribution. This one-sample test compares the observed frequencies in various categories against the frequencies expected under the null hypothesis model [53]. The procedural steps are methodical [53]:
- Hypotheses: State the null hypothesis ((H0)) that the observed frequency distribution matches the expected/theoretical distribution. The alternative hypothesis ((Ha)) is that at least one of the category proportions differs from the specified model.
- Significance Level: Choose an alpha level (α), commonly 0.05, representing the probability of a Type I error.
- Test Statistic: Calculate the Chi-Square statistic using the formula ( \chi^2 = \sum \frac{(O - E)^2}{E} ).
- Degrees of Freedom: Determine the degrees of freedom as (df = k - 1), where (k) is the number of categories.
- P-value and Conclusion: Obtain the p-value and compare it to α. If the p-value ≤ α, reject (H_0), indicating the model does not fit the data well.
This test is widely applicable, for instance, in genetics to check if observed phenotypic ratios match Mendelian inheritance patterns (e.g., 3:1 ratio), or in public health to validate if the severity distribution of a pre-diabetic condition in a sample matches known population parameters [52] [50].
Chi-Square Test for Independence
The Test for Independence is a two-sample test used to determine if there is a significant association between two categorical variables. This test is crucial for model validation when the research question involves investigating relationships, such as between a treatment and an outcome [50] [51]. The test uses a contingency table to organize the data. The calculation of the expected frequency for any cell in this table is based on the assumption that the two variables are independent, using the formula [50]:
[E = \frac{(\text{Row Total}) \times (\text{Column Total})}{\text{Grand Total}}]
The degrees of freedom for this test are calculated as (df = (r - 1) \times (c - 1)), where (r) is the number of rows and (c) is the number of columns in the contingency table [51]. A significant result suggests an association between the variables, implying that one variable may depend on the other. For example, in the pharmaceutical industry, this test can be used to investigate whether the effectiveness of a new dietary supplement is independent of the baseline severity of a pre-diabetes condition [50].
Table 1: Key Characteristics of Chi-Square Tests
| Feature | Goodness-of-Fit Test | Test for Independence |
|---|---|---|
| Purpose | Compare a distribution to a theoretical model | Assess association between two categorical variables |
| Number of Variables | One | Two |
| Typical Research Question | "Do my observed counts match the expected model?" | "Are these two variables related?" |
| Degrees of Freedom (df) | (k - 1) (k: number of categories) | ((r-1) \times (c-1)) (r: rows, c: columns) |
| Common Application in Model Validation | Validating assumed population proportions | Testing model assumptions of variable independence |
Experimental Protocol and Sample Size Considerations
Protocol for Chi-Square Goodness-of-Fit Test
A standardized protocol ensures the reliability and reproducibility of the test, which is critical for model validation research.
- Define the Model and Hypotheses: Precisely state the theoretical model to be validated, defining the null hypothesis ((H_0)) which specifies the expected proportions for each category.
- Collect and Categorize Data: Gather experimental data and sort the observations into the predefined categorical levels. Ensure data is collected objectively to avoid bias.
- Check Assumptions: Verify that the data meets the test's critical assumptions:
- Independence of observations: Each data point must belong to only one category and be independent of others.
- Sufficient sample size: All expected frequencies should be at least 5. If this condition is not met, categories may need to be combined, or an exact test (like Fisher's exact test) might be required [54].
- Calculate Expected Frequencies: Compute the expected count for each category using the formula (Ei = n \times pi), where (n) is the total sample size and (pi) is the probability for category (i) under (H0) [53].
- Compute the Test Statistic: For each category, calculate (\frac{(Oi - Ei)^2}{E_i}). Sum these values across all categories to obtain the final Chi-Square statistic.
- Determine the P-value and Conclude: Using the calculated ( \chi^2 ) value and the degrees of freedom, find the p-value. Compare it to the significance level α (e.g., 0.05) and draw a conclusion about the model's validity [53].
Sample Size and Power Analysis
Adequate sample size is paramount to ensure the test has sufficient statistical power—the probability of correctly rejecting a false null hypothesis. An underpowered study may fail to detect meaningful model deviations, compromising validation efforts [54] [51].
Power analysis helps determine the minimum sample size needed. For the Chi-Square test, this depends on several factors [51]:
- Effect size (w): A measure of the strength of the association or the deviation from the model, as defined by Cohen.
- Significance level (α): The risk of a Type I error (typically 0.05).
- Power (1-β): The desired probability of detecting an effect (typically 0.8 or 80%).
- Degrees of freedom (df): Determined by the number of categories.
Cohen's provides conventional values for small (w=0.1), medium (w=0.3), and large (w=0.5) effect sizes [51]. The relationship between these factors and sample size is complex, based on the non-central Chi-Square distribution. Researchers can use specialized software (e.g., G*Power) or online calculators to perform this calculation efficiently [54] [51].
Table 2: Essential Research Reagent Solutions for Chi-Square Analysis
| Reagent / Tool | Function in Analysis |
|---|---|
| Statistical Software (R, Python, SPSS) | Automates computation of test statistics, p-values, and expected frequencies, reducing manual calculation errors. |
| Sample Size Calculator (e.g., G*Power) | Determines the minimum sample required to adequately power the study for reliable model validation. |
| Contingency Table | A structured matrix (rows x columns) to organize and display the relationship between two categorical variables. |
| Cohen's w Effect Size | A standardized metric to quantify the degree of model deviation or association strength, crucial for power analysis. |
| Chi-Square Distribution Table | Provides critical values for determining statistical significance, useful for quick reference or when software is unavailable. |
Visualization of Workflows and Decision Processes
Chi-Square Goodness-of-Fit Test Workflow
Chi-Square Test Selection and Application
A/B Testing and Experimental Design for Clinical and Biomarker Validation
A/B testing, also known as split testing or randomized controlled experimentation, is a systematic research method that compares two or more variants of a single variable to determine which one performs better against a predefined metric [55]. While traditionally associated with marketing and web development, this methodology is increasingly recognized for its potential in clinical research and biomarker development. In the context of biomarker validation and clinical tool development, A/B testing provides a framework for making evidence-based decisions that can optimize recruitment strategies, improve clinical decision support systems, and validate diagnostic approaches [56] [57].
The fundamental principle of A/B testing involves randomly assigning subjects to either a control group (variant A) or an experimental group (variant B) and comparing their responses based on specific outcome measures. This approach aligns with the broader thesis of hypothesis testing for model validation research by providing a structured methodology for testing assumptions and generating empirical evidence [13]. The adoption of A/B testing in clinical environments represents a shift toward more agile, data-driven research practices that can accelerate innovation while maintaining scientific rigor.
Experimental Design Frameworks
Core Components of A/B Testing
Implementing a robust A/B testing framework in clinical and biomarker research requires careful consideration of several key components that form the foundation of valid experimental design [58]:
Hypothesis Development: Formulating specific, testable, and falsifiable hypotheses about expected outcomes based on preliminary research and theoretical frameworks. A well-constructed hypothesis typically states the change being made, the target population, and the expected impact on a specific metric.
Variable Selection: Identifying appropriate independent variables (the intervention being tested) and dependent variables (the outcomes being measured). In biomarker research, this might involve testing different assay formats, measurement techniques, or diagnostic thresholds.
Randomization Strategy: Implementing proper randomization procedures to assign participants or samples to control and experimental groups, thereby minimizing selection bias and confounding variables.
Sample Size Determination: Calculating appropriate sample sizes prior to experimentation to ensure adequate statistical power for detecting clinically meaningful effects while considering practical constraints.
Success Metrics Definition: Establishing clear, predefined primary and secondary endpoints that will determine the success or failure of the experimental intervention, aligned with clinical or research objectives.
Statistical Considerations
The statistical foundation of A/B testing relies on hypothesis testing methodology, which provides a framework for making quantitative decisions about experimental results [13]. The process begins with establishing a null hypothesis (H₀) that assumes no significant difference exists between variants, and an alternative hypothesis (H₁) that proposes a meaningful difference. Researchers must select appropriate statistical tests based on their data type and distribution, with common tests including Welch's t-test for continuous data, Fisher's exact test for binary outcomes, and chi-squared tests for categorical data [55].
Determining statistical significance requires setting a confidence level (typically 95% in clinical applications, corresponding to α = 0.05) that represents the threshold for rejecting the null hypothesis [58]. The p-value indicates the probability of observing the experimental results if the null hypothesis were true, with p-values below the significance threshold providing evidence against the null hypothesis. Additionally, researchers should calculate statistical power (generally target ≥80%) to minimize the risk of Type II errors (false negatives), particularly when testing biomarkers with potentially subtle effects [13].
Table 1: Common Statistical Tests for Different Data Types in Clinical A/B Testing
| Data Type | Example Use Case | Standard Test | Alternative Test |
|---|---|---|---|
| Gaussian | Average revenue per user, continuous laboratory values | Welch's t-test | Student's t-test |
| Binomial | Click-through rate, response rates | Fisher's exact test | Barnard's test |
| Poisson | Transactions per paying user | E-test | C-test |
| Multinomial | Number of each product purchased | Chi-squared test | G-test |
| Unknown distribution | Non-normal biomarker levels | Mann-Whitney U test | Gibbs sampling |
Applications in Clinical Research
Clinical Trial Recruitment Optimization
A/B testing methodologies have demonstrated significant value in optimizing patient recruitment for clinical trials through systematic testing of digital outreach materials. In one implementation for the STURDY trial, researchers conducted two sequential A/B testing experiments on the trial's recruitment website [56]. The first experiment compared two different infographic versions against the original landing page, randomizing 2,605 web users to these three conditions. The second experiment tested three video versions featuring different staff members on 374 website visitors. The research team measured multiple engagement metrics, including requests for more information, completion of screening visits, and eventual trial enrollment.
The results revealed that different versions of the recruitment materials significantly influenced user engagement behaviors. Specifically, response to the online interest form differed substantially based on the infographic version displayed, while the various video presentations affected how users engaged with website content and pages [56]. This application demonstrates how A/B testing can efficiently identify the most effective communication strategies for specific target populations, potentially improving recruitment efficiency and enhancing diversity in clinical trial participation.
Clinical Decision Support System Optimization
A/B testing methodologies have been successfully adapted for optimizing clinical decision support (CDS) systems within electronic health records (EHRs) [57]. Researchers at NYU Langone Health developed a structured framework combining user-centered design principles with rapid-cycle randomized trials to test and improve CDS tools. In one application, they tested multiple versions of an influenza vaccine alert targeting nurses, followed by a tobacco cessation alert aimed at outpatient providers.
The implementation process involved several stages: initial usability testing through interviews and observations of users interacting with existing alerts; ideation sessions to develop potential improvements; creation of lightweight prototypes; iterative refinement based on stakeholder feedback; and finally, randomized testing of multiple versions within the live EHR environment [57]. This approach led to significant improvements in alert effectiveness, including one instance where targeted modifications reduced alert firings per patient per day from 23.1 to 7.3, substantially decreasing alert fatigue while maintaining clinical efficacy.
Table 2: Clinical A/B Testing Applications and Outcome Measures
| Application Area | Tested Variables | Primary Outcome Measures | Key Findings |
|---|---|---|---|
| Clinical Trial Recruitment [56] | Website infographics, staff introduction videos | Information requests, screening completion, enrollment | Significant differences in engagement based on material type |
| Influenza Vaccine CDS [57] | Alert text, placement, dismissal options | Alert views, acceptance rates, firings per patient | Reduced firings from 23.1 to 7.3 per patient per day |
| Tobacco Cessation CDS [57] | Message framing (financial, quality, regulatory), images | Counseling documentation, prescription rates, referrals | No significant difference in acceptance based on message framing |
Applications in Biomarker Validation
Diagnostic Biomarker Validation
The validation of novel biomarker-based diagnostics represents a promising application for A/B testing methodologies in clinical research. A recent study evaluating TriVerity, an AI-based blood testing device for diagnosing and prognosticating acute infection and sepsis, demonstrates principles compatible with A/B testing frameworks [59]. The SEPSIS-SHIELD study prospectively enrolled 1,441 patients across 22 emergency departments to validate the device's ability to determine likelihoods of bacterial infection, viral infection, and need for critical care interventions within seven days.
In this validation study, the TriVerity test demonstrated superior accuracy compared to traditional biomarkers like C-reactive protein, procalcitonin, and white blood cell count for diagnosing bacterial infection (AUROC = 0.83) and viral infection (AUROC = 0.91) [59]. The severity score also showed significant predictive value for critical care interventions (AUROC = 0.78). The study design incorporated elements consistent with A/B testing principles, including clear predefined endpoints, statistical power considerations, and comparative effectiveness assessment against established standards.
Novel Biomarker Discovery and Verification
Advanced bioinformatics approaches integrated with experimental validation represent a powerful methodology for biomarker discovery that can be enhanced through A/B testing principles. In one investigation of sepsis-induced myocardial dysfunction (SIMD), researchers combined analysis of multiple GEO datasets with machine learning algorithms to identify cuproptosis-related biomarkers [60]. They utilized differential expression analysis, weighted gene co-expression network analysis (WGCNA), and three machine learning models (SVM-RFE, LASSO, and random forest) to select diagnostic markers, which were then validated in animal models.
This integrated approach identified PDHB and DLAT as key cuproptosis-related biomarkers for SIMD, with PDHB showing particularly high diagnostic accuracy (AUC = 0.995 in the primary dataset) [60]. The research workflow exemplifies how computational methods can be combined with experimental validation to discover and verify novel biomarkers, with potential for A/B testing frameworks to optimize various stages of this process, including assay conditions, measurement techniques, and diagnostic thresholds.
Experimental Protocols
Protocol for A/B Testing Clinical Trial Recruitment Materials
This protocol provides a structured approach for optimizing clinical trial recruitment through A/B testing of digital materials, based on methodologies implemented in the STURDY trial [56]:
Step 1: Research and Baseline Establishment
- Analyze existing recruitment data to identify bottlenecks and opportunities for improvement
- Establish baseline conversion rates for current recruitment materials
- Define target population demographics and recruitment goals
Step 2: Hypothesis and Variant Development
- Formulate specific hypotheses about how changes to recruitment materials might improve engagement
- Develop multiple variants of the material (e.g., different infographics, videos, or text)
- Ensure variants test specific, isolated elements to maintain clear interpretation
Step 3: Experimental Setup
- Implement randomization framework using A/B testing platforms (e.g., Optimizely, Google Analytics)
- Determine sample size requirements using power analysis
- Define equal distribution of variants among website visitors
Step 4: Metric Collection and Analysis
- Track primary engagement metrics: information requests, screening completion, enrollment
- Monitor secondary metrics: time on page, bounce rate, navigation patterns
- Run experiment until statistically significant sample size is achieved
- Analyze results using appropriate statistical tests (e.g., Fisher's exact test for conversion rates)
Step 5: Interpretation and Implementation
- Identify winning variant based on predefined success metrics
- Implement successful variant as new standard
- Document lessons learned and iterate with new tests
Protocol for Biomarker Assay Validation
This protocol outlines a structured approach for validating biomarker assays using A/B testing principles, incorporating elements from recent biomarker research [59] [60]:
Step 1: Assay Configuration Comparison
- Prepare identical sample sets for parallel testing
- Configure multiple assay conditions (e.g., different reagents, incubation times, detection methods)
- Establish randomization scheme for sample processing
Step 2: Performance Metric Definition
- Define primary accuracy metrics: sensitivity, specificity, AUC
- Establish precision metrics: intra-assay and inter-assay CV
- Set acceptability thresholds based on clinical requirements
Step 3: Experimental Execution
- Process samples according to predefined randomization scheme
- Implement blinding procedures to minimize bias
- Collect raw data using standardized documentation
Step 4: Statistical Analysis
- Compare performance metrics between assay configurations
- Assess statistical significance using appropriate tests (e.g., DeLong's test for AUC comparison)
- Evaluate confidence intervals for point estimates
Step 5: Clinical Validation
- Test superior assay configuration in clinical samples
- Validate against reference standard
- Assess clinical utility in relevant patient population
Visualization of Workflows
Clinical A/B Testing Workflow
Biomarker Validation with A/B Testing
Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Clinical A/B Testing
| Category | Specific Tools | Application in Research | Key Features |
|---|---|---|---|
| A/B Testing Platforms | Optimizely [56], Google Analytics [56] | Randomization and metric tracking for digital recruitment | Real-time analytics, user segmentation, statistical significance calculators |
| Bioinformatics Tools | Limma [61] [60], WGCNA [60], clusterProfiler [61] [60] | Biomarker discovery and differential expression analysis | Multiple testing correction, functional enrichment, network analysis |
| Machine Learning Algorithms | SVM-RFE [61] [60], LASSO [61] [60], Random Forest [61] [60] | Feature selection and biomarker validation | Handling high-dimensional data, variable importance ranking |
| Statistical Analysis | R [61] [60], Python statsmodels | Experimental design and result interpretation | Comprehensive statistical tests, visualization capabilities |
| EHR Integration Tools | Epic, Cerner, custom APIs [57] | Clinical decision support testing | Patient-level randomization, alert modification, outcome tracking |
A/B testing provides a robust methodological framework for optimizing clinical research and biomarker validation processes. By implementing structured comparative experiments, researchers can make evidence-based decisions that enhance patient recruitment, improve clinical decision support systems, and accelerate biomarker development. The protocols and applications outlined in this document demonstrate how these methodologies can be successfully adapted from their digital origins to address complex challenges in clinical and translational research. As the field advances, the integration of A/B testing principles with emerging technologies like artificial intelligence and multi-omics approaches holds significant promise for accelerating medical discovery and improving patient care.
The transition of machine learning (ML) models from research to clinical practice represents a significant challenge in modern healthcare. This application note details a structured framework for validating a diagnostic ML model against the existing standard of care, focusing on a real-world oncology use case. The core premise is that a model must not only demonstrate statistical superiority but also temporal robustness in the face of evolving clinical practices, patient populations, and data structures [62]. In highly dynamic environments like oncology, rapid changes in therapies, technologies, and disease classifications can lead to data shifts, potentially degrading model performance post-deployment if not properly addressed during validation [62]. This document provides a comprehensive protocol for a temporally-aware validation study, framing the evaluation within a rigorous hypothesis-testing paradigm to ensure that model performance and clinical utility are thoroughly vetted for real-world application.
Validation Framework and Hypothesis Testing
Study Objective and Use Case Definition
The primary objective is to determine whether a novel diagnostic ML model for predicting Acute Care Utilization (ACU) in cancer patients demonstrates a statistically significant improvement in performance and operational longevity compared to the existing standard of care clinical criteria. A strong use case must satisfy three criteria, as shown in Table 1 [63].
Table 1: Core Components of a Defined Clinical Use Case
| Component | Description | Application in ACU Prediction |
|---|---|---|
| Patient-Centered Outcome | The model predicts outcomes that matter to patients and clinicians. | ACU (emergency department visits or hospitalizations) is a significant patient burden and healthcare cost driver [62]. |
| Modifiable Outcome | The outcome is plausibly modifiable through available interventions. | Early identification of high-risk patients allows for proactive interventions like outpatient support or scheduled visits [63]. |
| Actionable Prediction | A clear mechanism exists for predictions to influence decision-making. | Model output could integrate into EHR to flag high-risk patients for care team review, enabling pre-emptive care [62]. |
Formulating the Hypotheses
The validation is structured around a formal hypothesis test to ensure statistical rigor.
- Null Hypothesis (H₀): There is no statistically significant difference in the area under the receiver operating characteristic curve (AUC-ROC) for predicting 180-day ACU between the diagnostic ML model and the standard of care.
- Alternative Hypothesis (Hₐ): The diagnostic ML model demonstrates a statistically significant improvement in AUC-ROC for predicting 180-day ACU compared to the standard of care.
A P-value of less than 0.05 will be considered evidence to reject the null hypothesis, indicating a statistically significant improvement. This P-value threshold represents a 5% alpha risk, the accepted probability of making a Type I error (falsely rejecting the null hypothesis) [64].
Performance Metrics and Comparison
Model performance should be evaluated on a hold-out test set representing a subsequent time period to assess temporal validity. Key metrics must be reported for both the ML model and the standard-of-care benchmark.
Table 2: Quantitative Performance Metrics for Model Validation
| Metric | Diagnostic ML Model | Standard of Care | P-Value |
|---|---|---|---|
| AUC-ROC | 0.78 | 0.72 | 0.003 |
| Sensitivity | 0.75 | 0.65 | - |
| Specificity | 0.76 | 0.74 | - |
| F1-Score | 0.71 | 0.64 | - |
| Brier Score | 0.18 | 0.21 | - |
Longitudinal Performance Analysis
A critical aspect of validation is assessing model longevity. This involves retraining and testing models on temporally distinct blocks of data to simulate real-world deployment over time. The following workflow and data illustrate this process.
Table 3: Longitudinal Model Performance on Temporal Test Sets
| Model Version | Training Data Period | Test Data Period | AUC-ROC | Performance Drift vs. Internal Validation |
|---|---|---|---|---|
| v1 | 2010-2016 | 2017-2018 (Internal) | 0.78 | Baseline |
| v1 | 2010-2016 | 2019-2020 | 0.76 | -2.6% |
| v1 | 2010-2016 | 2021-2022 | 0.73 | -6.4% |
| v2 (Retrained) | 2010-2018 | 2021-2022 | 0.77 | -1.3% |
Experimental Protocols
Core Experimental Workflow
The following protocol outlines the end-to-end process for validating the diagnostic model, from data preparation to final analysis.
Detailed Methodologies
Cohort Curation and Data Extraction
- Population: Identify patients diagnosed with solid cancer diseases who received systemic antineoplastic therapy within a defined health system [62].
- Inclusion Criteria: Adult patients (≥18 years) with at least five encounters in the two years preceding therapy initiation and at least six encounters during the 180-day follow-up period to mitigate censoring [62].
- Exclusion Criteria: Patients diagnosed externally or with hematologic malignancies [62].
- Data Source: Extract structured data from the Electronic Health Record (EHR), including demographics, medications, laboratory results, vitals, diagnosis, and procedure codes from the 180 days preceding therapy initiation [62].
Feature and Label Engineering
- Feature Construction: Use the most recent value recorded for each feature in the 180-day look-back period. One-hot encode categorical variables. Impute missing values using the sample mean from the training set or a k-nearest neighbor (KNN) approach [62].
- Label Definition (ACU): The label is a binary outcome (y=1) defined as an emergency department visit or hospitalization within 1-180 days of therapy initiation, associated with at least one symptom/diagnosis from a standardized list (e.g., CMS OP-35 criteria) [62].
Temporal Data Splitting
- Internal Validation Set: Randomly hold out 10% of data from the same time period as the training cohort [62].
- Prospective Validation Sets: Reserve data from subsequent, distinct time periods (e.g., 2019-2020, 2021-2022) as independent test sets to evaluate temporal robustness [62].
Model Training and Hyperparameter Tuning
- Algorithm Selection: Implement multiple model types, such as LASSO, Random Forest, and Extreme Gradient Boosting (XGBoost), to ensure model-agnostic validation [62].
- Hyperparameter Optimization: Perform nested 10-fold cross-validation within the training set to optimize hyperparameters. Refit the final model with the best parameters on the entire training set [62].
Statistical Hypothesis Testing
- Test Selection: Use a DeLong's test to compare the AUC-ROC of the ML model and the standard of care, as it is specifically designed for correlated ROC curves [64].
- Interpretation: Reject the null hypothesis if the P-value is less than the 0.05 significance level, concluding a statistically significant performance difference [64].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Computational and Data Resources for Clinical Model Validation
| Tool / Resource | Function | Application in Validation Protocol |
|---|---|---|
| Structured EHR Data | Provides the raw, high-dimensional clinical data for feature engineering and label definition. | Source for demographics, lab results, and codes to predict ACU [62]. |
| Statistical Software (R/Python) | Environment for data cleaning, model training, statistical analysis, and hypothesis testing. | Used for all analytical steps, from cohort summary to calculating P-values [64]. |
| Machine Learning Libraries (scikit-learn, XGBoost) | Provide implementations of algorithms (LASSO, RF, XGBoost) and performance metrics (AUC). | Enable model training, hyperparameter tuning, and initial performance evaluation [62]. |
| Hex Color Validator | Ensures color codes used in data visualizations meet accessibility contrast standards. | Validates that colors in model performance dashboards are perceivable by all users [65]. |
| Reporting Guidelines (TRIPOD/TRIPOD-AI) | A checklist to ensure transparent and complete reporting of prediction model studies. | Framework for documenting the study to ensure reproducibility and scientific rigor [63]. |
Python and R Code Snippets for Key Validation Tests
Validation is a critical step in ensuring the integrity of data and models, especially in scientific research and drug development. It encompasses a range of techniques, from checking the quality and structure of datasets to assessing the statistical significance of model outcomes. For researchers, scientists, and drug development professionals, employing rigorous validation tests is fundamental to generating reliable, reproducible, and regulatory-compliant results. This document provides application notes and experimental protocols for key validation tests, framed within the broader context of hypothesis testing for model validation research.
The Scientist's Toolkit: Essential Libraries for Validation
The choice of library for data validation often depends on the specific task, whether it's validating the structure of a dataset, an individual email address, or the results of a statistical test. The following table summarizes key tools available in Python and R.
Table 1: Key Research Reagent Solutions for Data and Model Validation
| Category | Library/Package | Language | Primary Function | Key Features |
|---|---|---|---|---|
| Data Validation | Pandera [66] |
Python | DataFrame/schema validation | Statistical testing, type-safe schema definitions, integration with Pandas/Polars [66]. |
Pointblank [66] |
Python | Data quality validation | Interactive reports, threshold management, stakeholder communication [66]. | |
Patito [66] |
Python | Model-based validation | Pydantic integration, row-level object modeling, familiar syntax [66]. | |
Great Expectations [67] |
Python | Data validation | Production-grade validation, wide range of expectations, triggers actions on failure [67]. | |
Pydantic [67] |
Python | Schema validation & settings management | Data validation for dictionaries/JSON, uses Python type hints, arbitrarily complex objects [67]. | |
| Email Validation | email-validator [68] |
Python | Email address validation | Checks basic format, DNS records, and domain validity [68]. |
| Statistical Testing | Pingouin [69] |
Python | Statistical analysis | T-tests, normality tests, ANOVA, linear regression, non-parametric tests [69]. |
scipy.stats (e.g., norm) |
Python | Statistical functions | Calculation of p-values from Z-scores and other statistical distributions [70]. | |
stats (e.g., t.test, wilcox.test) |
R | Statistical analysis | Comprehensive suite for T-tests, U-tests, and other hypothesis tests [71]. |
Experimental Protocols and Code Snippets
Protocol: Dataset Schema Validation with Pandera
Validating the structure and content of a dataset is a crucial first step in any data pipeline. This protocol uses Pandera to define a schema and validate a Polars DataFrame.
Application Note: Schema validation ensures your data conforms to expected formats, data types, and value ranges before analysis, preventing errors downstream [66].
Code Snippet: Python
Workflow Diagram: Dataset Schema Validation
Protocol: Statistical Hypothesis Testing with Student's t-test
The Student's t-test is used to determine if there is a significant difference between the means of two groups. This is fundamental in clinical trials, for example, to compare outcomes between a treatment and control group [69].
Application Note: A low p-value (typically ≤ 0.05) provides strong evidence against the null hypothesis (that the group means are equal), allowing researchers to reject it [69] [71].
Code Snippet: Python (using Pingouin)
Code Snippet: R (using built-in t.test)
Workflow Diagram: Hypothesis Testing Logic
Protocol: Email Address Validation with email-validator
In research involving human subjects, validating contact information is essential. This protocol checks if an email address is properly formatted and has a valid domain.
Application Note: While regular expressions can check basic format, dedicated libraries like email-validator can perform more robust checks, including DNS validation, which helps catch typos and non-existent domains [68].
Code Snippet: Python
Table 2: Common Statistical Tests for Model and Data Validation
| Test Name | Language | Use Case | Null Hypothesis (H₀) | Key Function(s) |
|---|---|---|---|---|
| Student's t-test | Python | Compare means of two groups. | The means of the two groups are equal. | pingouin.ttest() [69] |
| R | Compare means of two groups. | The means of the two groups are equal. | t.test() [71] |
|
| Mann-Whitney U Test | Python | Non-parametric alternative to t-test. | The distributions of the two groups are equal. | pingouin.mwu() [69] |
| R | Non-parametric alternative to t-test. | The distributions of the two groups are equal. | wilcox.test() [71] |
|
| Analysis of Variance (ANOVA) | Python | Compare means across three or more groups. | All group means are equal. | pingouin.anova() [69] |
| Linear Regression | Python | Model relationship between variables. | The slope of the regression line is zero (no effect). | pingouin.linear_regression() [69] |
| Shapiro-Wilk Test | Python | Test for normality of data. | The sample comes from a normally distributed population. | pingouin.normality() [69] |
| Z-test (via Simulation) | Python/R | Compare sample mean to population mean. | The sample mean is equal to the population mean. | Custom simulation [70] or scipy.stats / stats |
Table 3: Key Concepts in Hypothesis Testing
| Concept | Description | Typical Threshold in Research |
|---|---|---|
| Null Hypothesis (H₀) | The default assumption that there is no effect or no difference [69] [71]. | N/A |
| Alternative Hypothesis (H₁ or Ha) | The hypothesis that contradicts H₀, stating there is an effect or a difference [71]. | N/A |
| Significance Level (α) | The probability of rejecting H₀ when it is actually true (Type I error / false positive) [69] [71]. | 0.05 (5%) |
| P-value | The probability of obtaining the observed results if the null hypothesis is true. A small p-value is evidence against H₀ [71]. | ≤ 0.05 |
| Type I Error (α) | Rejecting a true null hypothesis (false positive) [69]. | Controlled by α |
| Type II Error (β) | Failing to reject a false null hypothesis (false negative) [69] [71]. | N/A |
| Power (1-β) | The probability of correctly rejecting a false null hypothesis [71]. | Typically desired ≥ 0.8 |
Avoiding Common Pitfalls and Optimizing Validation Study Design
The credibility of scientific research, particularly in fields involving model validation and drug development, is threatened by data dredging and p-hacking. Data dredging, also known as data snooping or p-hacking, is the misuse of data analysis to find patterns in data that can be presented as statistically significant, thus dramatically increasing and understating the risk of false positives [72]. This is often done by performing many statistical tests on a single dataset and only reporting those that come back with significant results [72]. Common practices include optional stopping (collecting data until a desired p-value is reached), post-hoc grouping of data features, and multiple modelling approaches without proper statistical correction [72].
These practices undermine the scientific process because conventional statistical significance tests are based on the probability that a particular result would arise if chance alone were at work. When large numbers of tests are performed, some will produce false results by chance alone; 5% of randomly chosen hypotheses might be erroneously reported as statistically significant at the 5% significance level [72]. Pre-registration and transparent reporting have emerged as core solutions to these problems by making the research process more transparent and accountable.
Theoretical Foundations: Linking Hypothesis Testing to Model Validation
The Traditional Hypothesis Testing Framework
Hypothesis testing provides a formal structure for validating models and drawing conclusions from data. The process begins with formulating two competing statements: the null hypothesis (H0), which is the default assumption that no effect or difference exists, and the alternative hypothesis (Ha), which represents the effect or difference the researcher aims to detect [10]. The analysis calculates a p-value, representing the probability of obtaining an effect as extreme as or more extreme than the observed effect, assuming the null hypothesis is true [10].
In model validation, this traditional framework has been criticized for placing the burden of proof on the wrong side. The standard null hypothesis—that there is no difference between the model predictions and the real-world process—is unsatisfactory because failure to reject it could mean either the model is acceptable or the test has low power [18]. This is particularly problematic in contexts like ecological modelling and drug development, where validating predictive accuracy is crucial.
Equivalence Testing: A Superior Framework for Model Validation
A more robust approach for model validation uses equivalence tests, which flip the burden of proof. Instead of testing for any difference, equivalence tests use the null hypothesis of dissimilarity—that the model is unacceptable [18]. The model must then provide sufficient evidence that it meets predefined accuracy standards.
The key innovation in equivalence testing is the subjective choice of a region of indifference within which differences between test and reference data are considered negligible [18]. For example, a researcher might specify that if the absolute value of the mean differences between model predictions and observations is less than 25% of the standard deviation, the difference is negligible. The test then determines whether a confidence interval for the metric is completely contained within this region [18].
Table 1: Comparison of Traditional Hypothesis Testing vs. Equivalence Testing for Model Validation
| Feature | Traditional Hypothesis Testing | Equivalence Testing |
|---|---|---|
| Null Hypothesis | No difference between model and reality (model is acceptable) | Model does not meet accuracy standards (model is unacceptable) |
| Burden of Proof | On the data to show the model is invalid | On the model to show it is valid |
| Interpretation of Non-Significant Result | Model is acceptable (may be due to low power) | Model is not acceptable |
| Practical Implementation | Tests for any statistically significant difference | Tests if difference is within a pre-specified negligible range |
| Suitable For | Initial screening for gross inadequacies | Formal validation against predefined accuracy requirements |
Bayesian Approaches to Hypothesis Testing
Bayesian statistics offers alternative approaches that avoid some pitfalls of frequentist methods. Rather than testing point hypotheses (e.g., whether an effect is exactly zero), Bayesian methods focus on continuous parameters and ask: "How big is the effect?" and "How likely is it that the effect is larger than a practically significant threshold?" [73]. These approaches include:
- Determining a Region of Practical Equivalence (ROPE): Establishing a range of effect sizes considered practically irrelevant and computing the posterior probability that the effect lies within this range [73].
- Bayesian Model Comparison: Using methods like Bayesian stacking to combine predictions from multiple models rather than selecting just one, thereby acknowledging uncertainty in model selection [73].
- Posterior Predictive Checks: Assessing how well models reproduce qualitative features of the data, not just quantitative fits [73].
Pre-registration: Protocols and Implementation
The Concept and Purpose of Pre-registration
Pre-registration involves documenting research hypotheses, methods, and analysis plans before data collection or analysis begins. When implemented effectively, it goes beyond bureaucratic compliance to become a substantive scientific activity. Proper pre-registration involves constructing a hypothetical world—a complete generative model of the process under study—and simulating fake data to test and refine analysis methods [74]. This process, sometimes called "fake-data simulation" or "design analysis," helps researchers clarify their theories and ensure their proposed analyses can recover parameters of interest [74].
Registered Reports
A particularly powerful form of pre-registration is the Registered Report, which involves peer review of a study protocol and analysis plan before research is undertaken, with pre-acceptance by a publication outlet [75]. This format aligns incentives toward research quality rather than just dramatic results, as publication decisions are based on the methodological rigor rather than the outcome.
Implementation Protocol: Creating an Effective Pre-registration
Table 2: Essential Components of a Research Pre-registration
| Component | Description | Level of Detail Required |
|---|---|---|
| Research Hypotheses | Clear statement of primary and secondary hypotheses | Specify exact relationships between variables with directionality |
| Study Design | Experimental or observational design structure | Include sample size, allocation methods, control conditions |
| Variables | All measured and manipulated variables | Define how each variable is operationalized and measured |
| Data Collection Procedures | Protocols for data acquisition | Detail equipment, settings, timing, and standardization methods |
| Sample Size Planning | Justification for number of subjects/samples | Include power analysis or precision calculations |
| Statistical Analysis Plan | Complete analysis workflow | Specify all models, tests, software, and criteria for interpretations |
| Handling of Missing Data | Procedures for incomplete data | Define prevention methods and analysis approaches |
| Criteria for Data Exclusion | Rules for removing outliers or problematic data | Establish objective, pre-specified criteria |
The following workflow diagram illustrates the complete pre-registration and research process:
Research Workflow with Pre-registration
Transparent Reporting Frameworks and Standards
The TOP Guidelines Framework
The Transparency and Openness Promotion (TOP) Guidelines provide a policy framework for advancing open science practices across research domains. Updated in 2025, TOP includes seven Research Practices, two Verification Practices, and four Verification Study types [75]. The guidelines use a three-level system of increasing transparency:
Table 3: TOP Guidelines Framework for Research Transparency
| Practice | Level 1: Disclosed | Level 2: Shared and Cited | Level 3: Certified |
|---|---|---|---|
| Study Registration | Authors state whether study was registered | Researchers register study and cite registration | Independent party certifies registration was timely and complete |
| Study Protocol | Authors state if protocol is available | Researchers publicly share and cite protocol | Independent certification of complete protocol |
| Analysis Plan | Authors state if analysis plan is available | Researchers publicly share and cite analysis plan | Independent certification of complete analysis plan |
| Materials Transparency | Authors state if materials are available | Researchers cite materials in trusted repository | Independent certification of material deposition |
| Data Transparency | Authors state if data are available | Researchers cite data in trusted repository | Independent certification of data with metadata |
| Analytic Code Transparency | Authors state if code is available | Researchers cite code in trusted repository | Independent certification of documented code |
| Reporting Transparency | Authors state if reporting guideline was used | Authors share completed reporting checklist | Independent certification of guideline adherence |
CONSORT and SPIRIT for Clinical Trials
For randomized clinical trials, the CONSORT (Consolidated Standards of Reporting Trials) and SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) statements provide specialized guidance. The 2025 updates to both guidelines include new sections on open science that clarify requirements for trial registration, statistical analysis plans, and data availability [76].
CONSORT 2025 provides a checklist and flow diagram for reporting completed trials, while SPIRIT 2025 focuses on protocol completeness to facilitate trial replication, reduce protocol amendments, and provide accountability for trial design, conduct, and data dissemination [76]. Key enhancements in the 2025 versions include:
- Explicit open science requirements for data and code sharing
- Enhanced reporting of patient and public involvement in trial design
- Greater emphasis on accessibility of study information
- Living document approach to accommodate evolving research methodologies
Protocol for Implementing Transparent Reporting
The following diagram outlines the process for ensuring transparent reporting throughout the research lifecycle:
Transparent Research Reporting Process
Table 4: Essential Research Reagent Solutions for Transparent Science
| Tool Category | Specific Solutions | Function and Application |
|---|---|---|
| Pre-registration Platforms | Open Science Framework (OSF), ClinicalTrials.gov | Create time-stamped, immutable study registrations |
| Data Repositories | Dryad, Zenodo, OSF, institutional repositories | Store and share research data with persistent identifiers |
| Code Sharing Platforms | GitHub, GitLab, Code Ocean | Share and version control analysis code |
| Reporting Guidelines | CONSORT, SPIRIT, TOP Guidelines | Ensure complete and transparent research reporting |
| Statistical Software | R, Python, Stan, JASP | Conduct reproducible statistical analyses |
| Dynamic Documentation | R Markdown, Jupyter Notebooks, Quarto | Integrate code, results, and narrative in reproducible documents |
| Validation Tools | EQUATOR Network, CONSORT Checklist | Verify reporting completeness and adherence to standards |
Experimental Protocol: Equivalence Testing for Model Validation
Background and Principles
Equivalence testing provides a statistically sound framework for model validation by setting the null hypothesis as "the model is not valid" and requiring the model to provide sufficient evidence to reject this hypothesis [18]. This approach is particularly valuable for validating computational models, statistical models, and clinical prediction tools.
Materials and Equipment
- Dataset for model training and testing
- Computational resources for model implementation
- Statistical software (R, Python, or equivalent)
- Pre-specified equivalence margins based on domain knowledge
Step-by-Step Procedure
Define the Performance Metric: Select an appropriate metric for comparing model predictions to observations (e.g., mean absolute error, accuracy, AUC).
Establish the Equivalence Margin: Define the region of indifference (Δ) within which differences are considered negligible. This should be based on:
- Clinical or practical significance
- Domain expertise
- Regulatory requirements where applicable
Collect Validation Data: Obtain an independent dataset not used in model development.
Generate Predictions: Run the model on the validation data to obtain predictions.
Calculate Discrepancies: Compute differences between predictions and observations.
Construct Confidence Interval: Calculate a (1-2α)×100% confidence interval for the performance metric. For the two one-sided test (TOST) procedure, use a 90% confidence interval for α=0.05.
Test for Equivalence: Determine if the entire confidence interval falls within the equivalence margin (-Δ, +Δ).
Interpret Results:
- If the confidence interval is completely within (-Δ, +Δ), conclude equivalence
- Otherwise, fail to establish equivalence
Example Application
For a forest growth model validation, researchers might define the equivalence margin as ±25% of the standard deviation of observed growth measurements [18]. They would then collect tree increment core measurements, generate model predictions, calculate the mean difference between predictions and observations, construct a 90% confidence interval for this difference, and check if it falls entirely within the predetermined equivalence margin.
Pre-registration and transparent reporting represent paradigm shifts in how researchers approach hypothesis testing and model validation. By moving from secretive, flexible analytical practices to open, predetermined plans, these methods address the root causes of p-hacking and data dredging. When implemented as substantive scientific activities rather than bureaucratic formalities, they strengthen the validity of research conclusions and enhance the cumulative progress of science. The frameworks and protocols outlined here provide practical pathways for researchers to adopt these practices, particularly in the context of model validation research where methodological rigor is paramount.
Addressing the Multiple Comparisons Problem and False Discovery Rate Control
In model validation research, the simultaneous statistical testing of multiple hypotheses presents a significant methodological challenge. When researchers conduct numerous hypothesis tests simultaneously—whether comparing multiple treatment groups, assessing many performance indicators, or evaluating thousands of features in high-throughput experiments—the probability of obtaining false positive results increases substantially. This phenomenon, known as the multiple comparisons problem, poses particular challenges in pharmaceutical development and biomedical research where erroneous conclusions can have profound consequences [77].
The fundamental issue arises from the inflation of Type I errors (false positives) as the number of hypotheses increases. In the most general case where all null hypotheses are true and tests are independent, the probability of making at least one false positive conclusion approaches near certainty as the number of tests grows. For example, when testing 100 true independent hypotheses at a significance level of α=0.05, the probability of at least one false positive is approximately 99.4% rather than the nominal 5% [78] [77]. This error inflation occurs because each individual test carries its own chance of a Type I error, and these probabilities accumulate across the entire family of tests being conducted.
The multiple comparisons problem manifests in various research scenarios common to model validation, including: comparing therapeutic effects of multiple drug doses against standard treatment; evaluating treatment-control differences across multiple outcome measurements; determining differential expression among tens of thousands of genes in genomic studies; and assessing multiple biomarkers in early drug development [78]. In all these cases, proper statistical adjustment is necessary to maintain the integrity of research conclusions and ensure that seemingly significant findings represent genuine effects rather than random noise.
Understanding Error Rates and Correction Approaches
Defining Key Error Metrics
Statistical approaches for addressing multiple comparisons focus on controlling different types of error rates. Understanding these metrics is crucial for selecting appropriate correction methods in model validation research.
Family-Wise Error Rate (FWER) represents the probability of making at least one Type I error (false positive) among the entire family of hypothesis tests [79] [78]. Traditional correction methods like Bonferroni focus on controlling FWER, ensuring that the probability of any false positive remains below a pre-specified significance level (typically α=0.05). This approach provides stringent control against false positives but comes at the cost of reduced statistical power, potentially leading to missed true effects (Type II errors) [79].
False Discovery Rate (FDR) represents the expected proportion of false positives among all hypotheses declared significant [79] [80] [81]. If R is the total number of rejected hypotheses and V is the number of falsely rejected null hypotheses, then FDR = E[V/R | R > 0] · P(R > 0) [80]. Rather than controlling the probability of any false positive (as with FWER), FDR methods control the proportion of errors among those hypotheses declared significant, offering a less conservative alternative that is particularly useful in exploratory research settings [79] [81].
Table 1: Outcomes When Testing Multiple Hypotheses
| Null Hypothesis True | Alternative Hypothesis True | Total | |
|---|---|---|---|
| Test Declared Significant | V (False Positives) | S (True Positives) | R |
| Test Not Declared Significant | U (True Negatives) | T (False Negatives) | m-R |
| Total | m₀ | m-m₀ | m |
Comparison of Multiple Comparison Correction Methods
Different correction approaches offer varying balances between false positive control and statistical power, making them suitable for different research contexts in model validation.
Table 2: Comparison of Multiple Comparison Correction Methods
| Method | Error Rate Controlled | Key Principle | Advantages | Limitations |
|---|---|---|---|---|
| Bonferroni | FWER | Adjusts significance level to α/m for m tests | Simple implementation; strong control of false positives | Overly conservative; low power with many tests [78] [82] |
| Holm | FWER | Stepwise rejection with adjusted α/(m-i+1) | More powerful than Bonferroni; controls FWER | Still relatively conservative [78] |
| Dunnett | FWER | Specific for multiple treatment-control comparisons | Higher power for its specific application | Limited to specific experimental designs [79] |
| Benjamini-Hochberg (BH) | FDR | Ranks p-values; rejects up to largest k where p₍ₖ₎ ≤ (k/m)α | Good balance of power and error control; widely applicable | Requires independent tests for exact control [79] [80] |
| Benjamini-Yekutieli | FDR | Modifies BH with dependency factor c(m)=∑(1/i) | Controls FDR under arbitrary dependence | More conservative than BH; lower power [80] |
| Storey's q-value | FDR | Estimates proportion of true null hypotheses (π₀) | Increased power by incorporating π₀ estimation | Requires larger number of tests for reliable estimation [83] [81] |
The choice between FWER and FDR control depends on the research context and consequences of errors. FWER methods are preferable in confirmatory studies where any false positive would have serious implications, such as in late-stage clinical trials. In contrast, FDR methods are more suitable for exploratory research where identifying potential leads for further investigation is valuable, and a proportion of false positives can be tolerated [79] [81].
Protocols for Implementing FDR Control in Model Validation
Benjamini-Hochberg Procedure Protocol
The Benjamini-Hochberg (BH) procedure provides a straightforward method for controlling the False Discovery Rate in multiple hypothesis testing scenarios. The following protocol details its implementation for model validation research.
Materials and Reagents:
- Statistical software (R, Python, or equivalent)
- Dataset with multiple hypothesis tests
- P-values for each hypothesis test
Procedure:
- P-value Calculation: Compute raw p-values for all m hypothesis tests using appropriate statistical methods.
- Rank Ordering: Sort the p-values in ascending order: p₍₁₎ ≤ p₍₂₎ ≤ ... ≤ p₍ₘ₎.
- Critical Value Calculation: For each ranked p-value, calculate the BH critical value as (i/m) × α, where i is the rank, m is the total number of tests, and α is the desired FDR level (typically 0.05).
- Significance Determination: Identify the largest k such that p₍ₖ₎ ≤ (k/m) × α.
- Hypothesis Rejection: Reject all null hypotheses for i = 1, 2, ..., k.
Validation and Quality Control:
- Verify independence assumption between test statistics
- Confirm that p-values are uniformly distributed under the null hypothesis
- Check for potential dependencies that might require modified procedures
Figure 1: Benjamini-Hochberg Procedure Workflow
Modern Covariate-Adjusted FDR Control Protocol
Modern FDR methods incorporate complementary information as informative covariates to increase statistical power while maintaining false discovery control. These approaches are particularly valuable in high-dimensional model validation studies.
Materials and Reagents:
- Statistical software with FDR packages (R: IHW, BL, AdaPT; Python: statsmodels)
- Dataset with hypothesis test results and informative covariates
- Computational resources for resampling or empirical null estimation
Procedure:
- Covariate Selection: Identify informative covariates that are independent of p-values under the null hypothesis but informative about power or prior probability of being non-null.
- Method Selection: Choose appropriate covariate-aware method based on data structure:
- Independent Hypothesis Weighting (IHW) for general multiple testing
- Boca and Leek's FDR Regression (BL) for genomic applications
- Adaptive p-value Thresholding (AdaPT) for complex dependencies
- Adaptive Shrinkage (ASH) for effect sizes and standard errors
- Parameter Tuning: Set method-specific parameters (e.g., folds for IHW, model specification for AdaPT).
- FDR Estimation: Implement chosen method to compute adjusted q-values or significance thresholds.
- Validation: Assess FDR control using synthetic null data or negative controls where possible.
Validation and Quality Control:
- Verify covariate appropriateness: should be independent of p-values under null
- Check FDR control using negative controls or simulated null data
- Compare results with classic FDR methods to assess improvement
- Evaluate sensitivity to parameter choices through robustness checks
Figure 2: Modern Covariate-Adjusted FDR Methods Workflow
Power and Sample Size Considerations Protocol
Proper experimental design incorporating power analysis is essential for reliable multiple testing corrections in model validation research.
Materials and Reagents:
- Power analysis software (R: pwr, simr; Python: statsmodels)
- Pilot data or effect size estimates
- Computational resources for simulation studies
Procedure:
- Effect Size Specification: Define meaningful effect sizes based on biological or clinical significance.
- Power Calculation: Estimate statistical power for individual tests using conventional methods.
- Multiple Testing Adjustment: Incorporate planned multiple comparison correction into power calculations.
- Sample Size Determination: Calculate required sample sizes to achieve desired power (typically 80-90%) after multiple testing adjustment.
- Sensitivity Analysis: Evaluate how power changes with different effect sizes, sample sizes, and correction methods.
Validation and Quality Control:
- Verify power calculations using simulation where possible
- Consider trade-offs between false positives and false negatives
- Assess feasibility of required sample sizes given experimental constraints
- Document all assumptions in power calculations
Practical Applications and Case Studies in Model Validation
Case Study: Pharmaceutical Development Simulation
To illustrate the practical implications of different multiple comparison approaches, consider a simulated pharmaceutical development scenario with 10 treatment groups compared to a single control, where only 3 treatments have true effects.
Table 3: Simulation Results for Different Multiple Comparison Methods
| Method | FWER | FDR | Power | Suitable Applications |
|---|---|---|---|---|
| No Correction | 0.65 | 0.28 | 0.85 | Not recommended for formal studies |
| Bonferroni | 0.03 | 0.01 | 0.45 | Confirmatory studies; regulatory submissions |
| Dunnett | 0.04 | 0.02 | 0.58 | Multiple treatment-control comparisons |
| Benjamini-Hochberg | 0.22 | 0.04 | 0.72 | Exploratory research; biomarker identification |
Simulation parameters: 1 control group, 7 null-effect treatments, 3 true-effect treatments (2.5% uplift), α=0.05, 1000 simulations [79]. The results demonstrate the trade-off between error control and detection power, with Bonferroni providing stringent FWER control at the cost of power, while BH methods offer a balanced approach with controlled FDR and higher power.
Case Study: Genomic Applications in Drug Development
In genomic studies during early drug development, researchers often face extreme multiple testing problems with tens of thousands of hypotheses. A typical differential expression analysis might test 20,000 genes, where only 200-500 are truly differentially expressed.
Implementation Considerations:
- Storey's q-value method typically identifies 30-50% more true positives than Bonferroni correction at the same nominal error rate [83] [81]
- Independent Hypothesis Weighting (IHW) using mean expression level as a covariate can improve power by 15-25% over standard BH procedure [83]
- In metabolomics data with high feature correlation, standard FDR control may exhibit instability, with false positive proportions sometimes exceeding 50% when dependencies are strong [84]
Research Reagent Solutions for Multiple Testing Studies
Table 4: Essential Research Reagents and Computational Tools
| Reagent/Tool | Function | Application Context |
|---|---|---|
| R stats package | Basic p-value adjustment | Bonferroni, Holm, BH procedures |
| q-value package (R) | Storey's FDR method | Genomic studies with many tests |
| IHW package (R) | Covariate-aware FDR control | Leveraging informative covariates |
| AdaPT package (R) | Adaptive FDR control | Complex dependency structures |
| Python statsmodels | Multiple testing corrections | Python-based analysis pipelines |
| Benjamini-Yekutieli method | FDR under arbitrary dependence | When test independence is questionable |
| Simulation frameworks | Power analysis and validation | Experimental design and method validation |
Advanced Considerations and Recent Developments
Addressing Dependencies and Assumption Violations
Recent research has highlighted important limitations of standard FDR methods in the presence of strong dependencies between hypothesis tests. While the Benjamini-Hochberg procedure maintains FDR control under positive regression dependency, arbitrary dependencies can lead to counterintuitive results [80] [84].
In high-dimensional biological data with correlated features (e.g., gene expression, methylation arrays), BH correction can sometimes produce unexpectedly high numbers of false positives despite formal FDR control. In metabolomics data with strong correlations, false discovery proportions can reach 85% in certain instances, particularly when sample sizes are small and correlations are high [84].
Recommendations for Dependent Data:
- Use Benjamini-Yekutieli procedure for arbitrary dependencies
- Consider permutation-based approaches for complex dependency structures
- Employ empirical null methods using negative controls
- Implement hierarchical FDR control that accounts for known dependency structures
Emerging Methods and Future Directions
Recent developments in FDR methodology focus on increasing power while maintaining error control through more sophisticated use of auxiliary information. Mirror statistics represent a promising p-value-free approach that defines a mirror statistic based on data-splitting and uses its symmetry under the null hypothesis to control FDR [85]. This method is particularly valuable in high-dimensional settings where deriving valid p-values is challenging, such as confounder selection in observational studies for drug safety research.
Other emerging approaches include:
- Knockoff filters for controlled variable selection
- Deep learning-based multiple testing procedures
- Federated FDR methods for distributed data analysis
- Spatial FDR control for imaging and spatial transcriptomics
These advanced methods show particular promise for model validation in pharmaceutical contexts where complex data structures and high-dimensional feature spaces are common.
Addressing the multiple comparisons problem through appropriate false discovery rate control is essential for rigorous model validation in pharmaceutical and biomedical research. The choice between conservative FWER methods and more powerful FDR approaches should be guided by research context, consequence of errors, and study objectives. Modern covariate-aware FDR methods offer increased power while maintaining error control, particularly valuable in high-dimensional exploratory research. As methodological developments continue, researchers should stay informed of emerging approaches that offer improved error control for complex data structures while implementing robust validation practices to ensure the reliability of research findings.
In the realm of hypothesis testing for model validation research, determining an appropriate sample size is a critical prerequisite that directly impacts the scientific validity, reproducibility, and ethical integrity of research findings. Sample size calculation, often referred to as power analysis, ensures that a study can detect a biologically or clinically relevant effect with a high probability if it truly exists [86]. For researchers, scientists, and drug development professionals, navigating the complexities of sample size determination is essential for designing robust experiments that can withstand regulatory scrutiny.
Inadequate sample sizes undermine research in profound ways. Under-powered studies waste precious resources, lead to unnecessary animal suffering in preclinical research, and result in erroneous biological conclusions by failing to detect true effects (Type II errors) [87]. Conversely, over-powered studies may detect statistically significant differences that lack biological relevance, potentially leading to misleading conclusions about model validity [87]. This guide provides comprehensive application notes and protocols for determining appropriate sample sizes within the context of hypothesis testing for model validation research.
Foundational Concepts and Definitions
Key Statistical Parameters
Table 1: Fundamental Parameters in Sample Size Determination
| Parameter | Symbol | Definition | Common Values | Interpretation |
|---|---|---|---|---|
| Type I Error | α | Probability of rejecting a true null hypothesis (false positive) | 0.05, 0.01 | 5% or 1% risk of detecting an effect that doesn't exist |
| Type II Error | β | Probability of failing to reject a false null hypothesis (false negative) | 0.2, 0.1 | 20% or 10% risk of missing a true effect |
| Power | 1-β | Probability of correctly rejecting a false null hypothesis | 0.8, 0.9 | 80% or 90% probability of detecting a true effect |
| Effect Size | ES | Magnitude of the effect of practical/clinical significance | Varies by field | Minimum difference considered biologically meaningful |
| Standard Deviation | σ | Variability in the outcome measure | Estimated from pilot data | Measure of data dispersion around the mean |
The Hypothesis Testing Framework
In statistical hypothesis testing, two complementary hypotheses are formulated: the null hypothesis (H₀), which typically states no effect or no difference, and the alternative hypothesis (H₁), which states the presence of an effect or difference [88]. The balance between Type I and Type II errors is crucial; reducing the risk of one typically increases the risk of the other, necessitating a careful balance based on the research context [88].
Figure 1: Hypothesis Testing Error Matrix illustrating the relationship between statistical decisions and reality
Sample Size Calculation Protocol
Pre-Calculation Considerations
Before performing sample size calculations, researchers must address several foundational elements that inform the statistical approach:
Define Study Purpose and Objectives: Clearly articulate whether the study aims to explore new relationships or confirm established hypotheses, as this determines the statistical approach [89]. For model validation research, this typically involves specifying the key parameters the model aims to predict or explain.
Identify Primary Endpoints: Select one or two primary outcome measures that directly address the main research question [89]. In model validation, these might include measures of predictive accuracy, goodness-of-fit indices, or comparison metrics against established models.
Determine Study Design: Specify the experimental design (e.g., randomized controlled, cohort, case-control, cross-sectional), as this significantly influences the sample size calculation method [86] [89].
Establish Statistical Hypotheses: Formulate specific, testable null and alternative hypotheses in measurable terms [89]. For example: "H₀: The new predictive model does not improve accuracy compared to the existing standard (difference in AUC = 0); H₁: The new model provides superior accuracy (difference in AUC > 0.05)."
Define Minimum Clinically Meaningful Effect: Determine the smallest effect size that would be considered biologically or clinically relevant [89]. This value should be based on field-specific knowledge rather than statistical convenience.
Parameter Estimation Guidelines
Table 2: Practical Approaches for Parameter Estimation
| Parameter | Estimation Method | Application Notes |
|---|---|---|
| Effect Size | • Pilot studies• Previous literature• Cohen's conventions• Clinical judgment | For model validation, consider minimum important differences in performance metrics (e.g., ΔAUC > 0.05, ΔR² > 0.1) |
| Variability (SD) | • Pilot data• Previous similar studies• Literature reviews | If no prior data exists, consider conservative estimates (larger SD) to ensure adequate power |
| Significance Level (α) | • Conventional (0.05)• Adjusted for multiple comparisons• More stringent (0.01) for high-risk applications | For exploratory model validation, α=0.05 may suffice; for confirmatory studies, consider α=0.01 |
| Power (1-β) | • Standard (0.8)• Higher (0.9) for critical endpoints• Lower (0.75) for pilot studies | Balance resource constraints with need for reliable conclusions; 0.8 is widely accepted |
Calculation Methods by Study Design
Different research questions and study designs require specific statistical approaches for sample size calculation:
Comparative Studies (Two Groups)
For studies comparing means between two independent groups (e.g., validating a model against a standard approach):
Formula: $$n = \frac{2\sigma^2(Z{1-\alpha/2} + Z{1-\beta})^2}{\Delta^2}$$ Where σ = standard deviation, Δ = effect size (difference in means), Z = critical values from standard normal distribution [88].
Protocol:
- Estimate the standard deviation (σ) from pilot data or literature
- Determine the minimum meaningful difference (Δ) in outcome measures
- Set α (typically 0.05) and power (typically 0.8)
- Calculate required sample size per group
- Adjust for anticipated dropout or missing data (typically 10-20%)
Descriptive/Prevalence Studies
For studies estimating proportions or prevalence in a population:
Formula: $$n = \frac{Z_{1-\alpha/2}^2 P(1-P)}{d^2}$$ Where P = estimated proportion, d = precision (margin of error) [90].
Application Notes: When P is unknown, use P = 0.5 for maximum sample size. For small P (<10%), use precision = P/4 or P/5 rather than arbitrary values like 5% [90].
Correlation Studies
For studies examining relationships between continuous variables:
Formula: $$n = \left[\frac{Z{1-\alpha/2} + Z{1-\beta}}{0.5 \times \ln(\frac{1+r}{1-r})}\right]^2 + 3$$ Where r = expected correlation coefficient [88].
Implementation Workflow
Figure 2: Sample Size Determination Workflow for model validation research
The Researcher's Toolkit
Software Solutions for Power Analysis
Table 3: Statistical Software for Sample Size Calculation
| Software Tool | Application Scope | Key Features | Access |
|---|---|---|---|
| G*Power [86] [91] | t-tests, F-tests, χ² tests, z-tests, exact tests | Free, user-friendly, effect size calculation, graphical output | Free download |
| PASS [92] | Over 1200 statistical test scenarios | Comprehensive, validated procedures, extensive documentation | Commercial |
| OpenEpi [86] | Common study designs in health research | Web-based, freely accessible, multiple calculation methods | Free online |
| PS Power and Sample Size Calculation [86] | Dichotomous, continuous, survival outcomes | Practical tools for common clinical scenarios | Free |
| R Statistical Package (pwr) | Various statistical tests | Programmatic approach, reproducible analyses, customizable | Open source |
Effect Size Conventions
Table 4: Cohen's Standardized Effect Size Conventions
| Effect Size Category | Cohen's d | Percentage Overlap | Application Context |
|---|---|---|---|
| Small | 0.2 | 85% | Minimal clinically important difference |
| Medium | 0.5 | 67% | Moderate effects typically sought in research |
| Large | 0.8 | 53% | Substantial, easily detectable effects |
For laboratory animal research, more realistic conventions have been suggested: small (d=0.5), medium (d=1.0), and large (d=1.5) effects [87].
Advanced Considerations in Model Validation Research
Special Considerations for Model Validation
When determining sample sizes for model validation studies, researchers should address these specific considerations:
Multi-stage Validation Processes: For complex models requiring internal and external validation, allocate sample size across development, validation, and testing cohorts while maintaining adequate power at each stage.
Multiple Comparison Adjustments: When validating multiple model components or performance metrics simultaneously, adjust significance levels using Bonferroni, False Discovery Rate, or other correction methods to maintain overall Type I error rate.
Model Complexity Considerations: More complex models with greater numbers of parameters typically require larger sample sizes to ensure stable performance estimates and avoid overfitting.
Reference Standard Quality: The accuracy and reliability of the reference standard used for model comparison impacts required sample size; imperfect reference standards may necessitate larger samples.
Common Pitfalls and Mitigation Strategies
Table 5: Troubleshooting Sample Size Issues
| Pitfall | Consequence | Mitigation Strategy |
|---|---|---|
| Underestimated variability | Underpowered study, false negatives | Use conservative estimates; conduct pilot studies |
| Overoptimistic effect sizes | Underpowered study, missed effects | Base estimates on biological relevance, not convenience |
| Ignoring dropout/missing data | Final sample size insufficient | Inflate initial sample by expected attrition rate (10-20%) |
| Multiple primary endpoints | Inflated Type I error or inadequate power | Designate single primary endpoint; adjust α for multiple comparisons |
| Post-hoc power calculations | Misleading interpretation of negative results | Always perform a priori sample size calculation |
Regulatory and Ethical Considerations
In regulated environments such as drug development, sample size justification is not merely a statistical exercise but a regulatory requirement. ISO 14155:2020 for clinical investigation of medical devices requires explicit sample size justification in the clinical investigation plan [89]. Similarly, FDA guidelines emphasize the importance of appropriate sample size for demonstrating safety and effectiveness.
From an ethical perspective, sample size calculation balances competing concerns: too few participants may expose individuals to research risks without answering the scientific question, while too many may unnecessarily waste resources and potentially expose excess participants to risk [86] [88]. This is particularly important in preclinical research, where principles of reduction in animal use must be balanced against scientific validity [87].
Adequate sample size determination is a fundamental component of rigorous model validation research. By following the protocols outlined in this guide—clearly defining research questions, selecting appropriate endpoints, estimating parameters from reliable sources, and using validated calculation methods—researchers can optimize resource utilization, enhance research credibility, and contribute to reproducible science. Proper sample size planning ensures that model validation studies have the appropriate sensitivity to detect meaningful effects while controlling error rates, ultimately supporting robust scientific conclusions in drug development and biomedical research.
Statistical hypothesis testing provides a foundational framework for model validation research in scientific and drug development contexts. The validity of these tests, however, is contingent upon satisfying core statistical assumptions—normality, independence, and homoscedasticity. This application note presents comprehensive protocols for diagnosing and remediating violations of these critical assumptions. We provide structured methodologies for conducting assumption checks, practical strategies for addressing violations when they occur, and visual workflows to guide researchers through the diagnostic process. By establishing standardized procedures for verifying statistical assumptions, this protocol enhances the reliability and interpretability of research findings in hypothesis-driven investigations.
Statistical hypothesis testing serves as the backbone for data-driven decision-making in scientific research and drug development, enabling researchers to make inferences about population parameters based on sample data [13]. The process typically involves formulating null and alternative hypotheses, setting a significance level, calculating a test statistic, and making a data-backed decision to either reject or fail to reject the null hypothesis [93] [13]. However, the integrity of this process depends critically on satisfying underlying statistical assumptions—particularly normality, independence, and homoscedasticity.
When these assumptions are violated, the results of statistical tests can be misleading or completely erroneous [94]. For instance, violating normality assumptions can distort p-values in parametric tests, while independence violations can inflate Type I error rates, leading to false positive findings. Homoscedasticity violations (heteroscedasticity) can result in inefficient parameter estimates and invalid standard errors [95] [96]. In model validation research, where accurate inference is paramount, such distortions can compromise study conclusions and subsequent decision-making.
This application note addresses these challenges by providing detailed protocols for detecting and addressing violations of the three core statistical assumptions. The guidance is specifically framed within the context of hypothesis testing for model validation research, with particular attention to the needs of researchers, scientists, and drug development professionals who must ensure the statistical rigor of their analytical approaches.
Core Assumptions in Statistical Testing
Theoretical Foundations
Statistical tests rely on distributional assumptions to derive their sampling distributions and critical values. Parametric tests, including t-tests, ANOVA, and linear regression, assume that the underlying data meets specific distributional criteria [94]. The three assumptions central to many statistical procedures are:
- Normality: The assumption that data follow a normal distribution, or more specifically for regression, that model residuals are normally distributed [95] [94]. This assumption is particularly important for the validity of t-tests and confidence intervals.
- Independence: The requirement that observations are not correlated with each other, meaning the value of one observation does not influence or predict the value of another observation [96] [94]. Violations frequently occur in time-series data, clustered data, or repeated measurements.
- Homoscedasticity: Also known as homogeneity of variance, this assumes constant variance of errors (residuals) across all levels of the independent variables [95] [96]. When this assumption is violated, the data exhibit heteroscedasticity, which can undermine the efficiency of parameter estimates.
These assumptions are interconnected, with violations of one often exacerbating problems with others. For example, non-normal data may exhibit heteroscedasticity, and clustered data violate both independence and homoscedasticity assumptions.
Consequences of Assumption Violations
Ignoring statistical assumptions can lead to several problematic outcomes in research:
- Inaccurate p-values: Violations can cause test statistics to follow different distributions than assumed, leading to incorrect significance conclusions [94].
- Biased parameter estimates: Model coefficients may be systematically over- or under-estimated when assumptions are violated [96].
- Invalid confidence intervals: The coverage probability of confidence intervals may not match the nominal level (e.g., 95%) when assumptions are not met.
- Reduced statistical power: Tests may become less sensitive to detecting genuine effects when assumptions are violated [13].
In drug development and model validation research, these consequences can translate to flawed efficacy conclusions, compromised safety assessments, and poor decision-making in the research pipeline.
Diagnostic Protocols for Assumption Violations
Comprehensive Diagnostic Workflow
The following diagram illustrates a systematic approach to diagnosing statistical assumption violations:
Normality Assessment
The normality assumption requires that data or model residuals follow a normal distribution. The following protocols outline methods for assessing normality:
Graphical Methods
- Q-Q Plots (Quantile-Quantile Plots): Plot quantiles of the observed data against quantiles of a theoretical normal distribution. Data that follow a normal distribution will approximate a straight line, while deviations indicate departures from normality [95].
- Histograms: Create frequency distributions of the data or residuals and visually assess the shape for the characteristic bell curve of a normal distribution. Histograms should be symmetric with the highest frequency in the center [95].
- P-P Plots (Probability-Probability Plots): Plot the cumulative proportions of the observed data against the cumulative proportions of a theoretical normal distribution.
Statistical Tests
- Shapiro-Wilk Test: Particularly effective for small to moderate sample sizes, this test compares the observed distribution to a normal distribution with the same mean and variance [95].
- Kolmogorov-Smirnov Test: Compares the empirical cumulative distribution function of the data with the cumulative distribution function of a normal distribution [95].
- Anderson-Darling Test: A modification of the Kolmogorov-Smirnov test that gives more weight to the tails of the distribution.
For model validation research, it is recommended to use both graphical and formal statistical tests, as they provide complementary information about the nature and extent of non-normality.
Table 1: Normality Assessment Methods and Interpretation
| Method | Procedure | Interpretation of Normal Data | Common Violation Patterns |
|---|---|---|---|
| Q-Q Plot | Plot sample quantiles vs. theoretical normal quantiles | Points follow straight diagonal line | S-shaped curve (heavy tails), curved pattern (skewness) |
| Histogram | Frequency distribution of data/residuals | Bell-shaped, symmetric distribution | Skewed distribution, multiple peaks (bimodal) |
| Shapiro-Wilk Test | Formal statistical test for normality | p-value > 0.05 (fails to reject null hypothesis of normality) | p-value < 0.05 (suggests significant deviation from normality) |
| Kolmogorov-Smirnov Test | Compares empirical and theoretical CDFs | p-value > 0.05 | p-value < 0.05 |
Independence Verification
The independence assumption requires that observations are not correlated with each other. Violations commonly occur in longitudinal data, spatial data, and clustered sampling designs.
Assessment Methods
- Durbin-Watson Test: Primarily used for time-series data or regression residuals to detect autocorrelation. The test statistic ranges from 0 to 4, with values around 2 indicating no autocorrelation, values approaching 0 indicating positive autocorrelation, and values approaching 4 indicating negative autocorrelation [95].
- Residual Plots: Plot residuals against time order or other potential grouping factors. Random scatter suggests independence, while patterns or trends suggest violations.
- Design Evaluation: Carefully consider the study design and data collection process. Clustered data (e.g., multiple measurements from the same patient) inherently violate the independence assumption and require specialized analytical approaches [97].
In dental and medical research, for example, multiple measurements taken from the same patient represent a common independence violation that must be addressed through appropriate statistical methods [97].
Homoscedasticity Evaluation
Homoscedasticity requires that the variance of errors is constant across all levels of the independent variables. The following methods assess this assumption:
Diagnostic Approaches
- Residual vs. Fitted Values Plot: Plot regression residuals against predicted values. The spread of residuals should be relatively constant across all predicted values, with no discernible pattern (such as fanning or cone shapes) [95] [96].
- Scale-Location Plot: Plot the square root of the absolute standardized residuals against fitted values. This enhances the visualization of potential heteroscedasticity patterns.
- Statistical Tests: Breusch-Pagan test and White test formally evaluate the presence of heteroscedasticity in regression models. These tests examine whether the variance of errors is related to the independent variables.
- Goldfeld-Quandt Test: Splits the data into two groups and tests whether the variances of the residuals are similar across the groups [95].
Table 2: Homoscedasticity Assessment Methods
| Method | Procedure | Homoscedastic Pattern | Heteroscedastic Pattern |
|---|---|---|---|
| Residuals vs. Fitted Plot | Plot residuals against predicted values | Constant spread of points across all X values | Fan-shaped pattern (increasing/decreasing spread) |
| Breusch-Pagan Test | Formal test for heteroscedasticity | p-value > 0.05 (homoscedasticity) | p-value < 0.05 (heteroscedasticity) |
| Goldfeld-Quandt Test | Compare variance in data subsets | Similar variances across groups (p-value > 0.05) | Significantly different variances (p-value < 0.05) |
| Grouped Boxplots | Compare spread across categories | Similar box sizes across groups | Substantially different box sizes across groups |
Remediation Strategies for Assumption Violations
Addressing Normality Violations
When data violate the normality assumption, several remediation strategies are available:
Data Transformations
- Logarithmic Transformation: Effective for right-skewed data, the log transformation can normalize distributions where variance increases with the mean. Commonly used for biological measurements and concentration data [95].
- Square Root Transformation: Useful for count data and moderate right skewness.
- Box-Cox Transformation: A family of power transformations that automatically identifies the optimal transformation parameter (λ) to normalize the data.
- Inverse Transformation: Particularly effective for severe right skewness.
Alternative Statistical Approaches
- Non-parametric Tests: Distribution-free methods that do not rely on normality assumptions. These include the Mann-Whitney U test (alternative to t-test), Kruskal-Wallis test (alternative to ANOVA), and Spearman's rank correlation (alternative to Pearson's correlation) [13] [94].
- Robust Statistical Methods: Techniques that are less sensitive to departures from normality, such as trimmed means, M-estimators, and bootstrapping procedures.
- Generalized Linear Models (GLMs): Extend linear regression to non-normal error distributions, including Poisson regression for count data and logistic regression for binary outcomes [93].
Addressing Independence Violations
When independence assumptions are violated, consider these approaches:
Statistical Modeling Solutions
- Mixed Effects Models: Incorporate both fixed effects and random effects to account for correlated data structures, such as repeated measurements within subjects or clustering within institutions [97].
- Generalized Estimating Equations (GEE): Population-averaged models that account for within-cluster correlation while estimating population parameters.
- Time Series Models: For temporal autocorrelation, ARIMA (AutoRegressive Integrated Moving Average) models can properly account for the correlation structure.
- Cluster-Robust Standard Errors: Adjust standard errors to account for clustering in the data, providing valid inference even when independence assumptions are violated.
In studies where multiple measurements are taken from the same unit (e.g., several teeth from the same patient), the unit of investigation should be the patient, not the individual measurement, unless specialized methods for correlated data are employed [97].
Addressing Homoscedasticity Violations
When faced with heteroscedasticity, consider these remediation strategies:
Variance-Stabilizing Approaches
- Weighted Least Squares (WLS): Modifies ordinary least squares regression to assign different weights to observations based on their variance, giving less weight to observations with higher variance [95].
- Data Transformations: As with normality violations, transformations such as log, square root, or Box-Cox can often address both normality and heteroscedasticity simultaneously.
- Heteroscedasticity-Consistent Standard Errors: Also known as "robust standard errors," these provide valid inference even when homoscedasticity is violated, by adjusting standard errors to account for heteroscedasticity.
Implementation Protocols for Model Validation Research
Integrated Diagnostic and Remediation Workflow
For model validation research in scientific and drug development contexts, the following comprehensive workflow ensures thorough handling of statistical assumptions:
Research Reagent Solutions: Statistical Tools for Assumption Management
The following table outlines essential methodological tools for addressing statistical assumption violations in research:
Table 3: Research Reagent Solutions for Statistical Assumption Management
| Reagent Category | Specific Methods/Tools | Primary Function | Application Context |
|---|---|---|---|
| Normality Assessment | Shapiro-Wilk test, Q-Q plots, Kolmogorov-Smirnov test | Evaluate normal distribution assumption | Initial data screening, regression diagnostics |
| Independence Verification | Durbin-Watson test, ACF plots, study design evaluation | Detect autocorrelation and clustering effects | Time-series data, repeated measures, spatial data |
| Homoscedasticity Evaluation | Breusch-Pagan test, residual plots, Goldfeld-Quandt test | Assess constant variance assumption | Regression modeling, group comparisons |
| Data Transformation | Logarithmic, square root, Box-Cox transformations | Normalize distributions and stabilize variance | Skewed data, count data, proportional data |
| Non-parametric Alternatives | Mann-Whitney U, Kruskal-Wallis, Spearman correlation | Distribution-free hypothesis testing | Ordinal data, non-normal continuous data |
| Advanced Modeling Approaches | Mixed effects models, GEE, robust regression, WLS | Address multiple assumption violations simultaneously | Correlated data, heteroscedasticity, clustered samples |
Documentation and Reporting Standards
For model validation research, comprehensive documentation of assumption checks and remediation procedures is essential:
- Transparent Reporting: Clearly document all statistical methods used, including specific tests for assumption verification and any remediation steps applied [97].
- Supplementary Materials: Consider including diagnostic plots and test results as supplementary materials to support the validity of statistical conclusions.
- Methodological Justification: Provide rationale for the selection of specific remediation strategies, particularly when employing advanced or less common statistical approaches.
- Sensitivity Analysis: When appropriate, conduct analyses with and without transformations or outlier adjustments to demonstrate the robustness of findings to different analytical approaches.
Ethical statistical practice requires transparency about assumptions, methods, and limitations to ensure the validity and interpretability of research findings [98].
Navigating violations of statistical assumptions is not merely a technical exercise but a fundamental component of rigorous scientific research and model validation. By implementing systematic diagnostic protocols and appropriate remediation strategies, researchers can enhance the validity and interpretability of their findings. This application note provides structured methodologies for assessing and addressing violations of normality, independence, and homoscedasticity—three core assumptions underlying many statistical tests used in hypothesis-driven research.
For researchers in drug development and scientific fields, where decisions often have significant implications, robust statistical practices that properly account for assumption violations are essential. The protocols outlined here serve as a comprehensive guide for maintaining statistical rigor while acknowledging and addressing the real-world challenges posed by imperfect data. Through careful attention to these principles, researchers can strengthen the evidentiary value of their statistical conclusions and contribute to more reliable scientific knowledge.
The Perils of Underpowered Studies and How to Avoid Them
In the context of hypothesis testing for model validation research, statistical power is a fundamental methodological principle. Statistical power is defined as the probability that a study will reject the null hypothesis when the alternative hypothesis is true; that is, the probability of detecting a genuine effect when it actually exists [99]. For researchers and drug development professionals, an underpowered study—one with an insufficient sample size to answer the research question—carries significant risks. It fails to detect true effects of practical importance and results in a larger variance of parameter estimates, making the literature inconsistent and often misleading [100]. Conversely, an overpowered study wastes scarce research resources, can report statistically significant but clinically meaningless effects, and raises ethical concerns when involving human or animal subjects [101] [100]. The convention for sufficient statistical power is typically set at ≥80%, though some funders now request ≥90% [101]. Despite this, empirical assessments reveal that many fields struggle with underpowered research, with some analyses indicating median statistical power as low as 23% [101].
The Critical Consequences of Underpowered Research
Primary Perils and Their Impact on Scientific Inference
- Failure to Detect True Effects: The most direct consequence of low statistical power is the failure to identify effects of practical or clinical importance. This can lead to the erroneous abandonment of promising model validation pathways or therapeutic candidates [100].
- Increased Variance of Estimates: Underpowered studies produce effect size estimates with higher variance. When the null hypothesis is rejected in an underpowered study, the observed effect size tends to be exaggerated compared to the true population parameter [100].
- Contribution to Irreproducible Literature: The combination of high false-negative rates and inflated effect sizes when results are significant creates an inconsistent and potentially misleading body of literature. This phenomenon has been identified as a contributing factor to the replication crisis affecting various scientific disciplines [101] [102].
- Wasted Resources and Ethical Concerns: Conducting studies that have a low probability of providing definitive answers represents an inefficient allocation of scarce research resources. For clinical trials or animal studies, underpowered designs raise ethical concerns by exposing participants to potential risks without a reasonable expectation of generating meaningful knowledge [100].
Quantitative Relationships in Statistical Power
Table 1: Fundamental Parameters Affecting Statistical Power
| Parameter | Relationship to Power | Practical Consideration in Model Validation |
|---|---|---|
| Sample Size | Positive correlation | Larger samples increase power, but resource constraints often limit feasible sample sizes [101]. |
| Effect Size | Positive correlation | Smaller effect sizes require substantially larger samples to maintain equivalent power [101]. |
| Significance Level (α) | Negative correlation | More stringent alpha levels (e.g., 0.01 vs. 0.05) reduce power [99]. |
| Measurement Precision | Positive correlation | Reducing measurement error through improved protocols increases effective power [103]. |
| Data Structure | Varies | Using multiple measurements per subject or covariates can improve power [103]. |
Table 2: Illustrative Power Calculations for Common Scenarios in Model Validation Research
| Test Type | Effect Size | Sample Size per Group | Power Achieved | Practical Implication |
|---|---|---|---|---|
| Two-group t-test | Cohen's d = 0.5 | 64 | 80% | Adequate for moderate effects |
| Two-group t-test | Cohen's d = 0.5 | 50 | 70% | Questionable reliability |
| Two-group t-test | Cohen's d = 0.2 | 50 | 17% | Highly likely to miss real effect |
| Two-group t-test | Cohen's d = 0.8 | 26 | 80% | Efficient for large effects |
| ANOVA (3 groups) | f = 0.25 | 52 (per group) | 80% | Suitable for moderate effects |
| Correlation test | r = 0.3 | 85 | 80% | Appropriate for modest relationships |
A Protocol for Power Analysis in Model Validation Research
Experimental Protocol: A Priori Power Analysis
Purpose: To determine the appropriate sample size required for a model validation study during the planning phase, ensuring sufficient statistical power to detect effects of practical significance.
Materials and Equipment:
- Statistical software with power analysis capabilities (e.g., G*Power, PASS, R with pwr package)
- Preliminary estimates of effect size from pilot studies, literature, or theoretical expectations
- Specification of statistical test(s) to be employed in the primary analysis
- Definition of significance criterion (α level, typically 0.05)
Procedure:
- Define the Primary Hypothesis: Clearly state the null and alternative hypotheses in precise terms relevant to the model validation context.
- Select the Statistical Test: Identify the appropriate statistical procedure for testing the primary hypothesis (e.g., t-test, ANOVA, correlation, regression).
- Specify the Significance Criterion: Set the Type I error rate (α), typically 0.05 for most applications.
- Determine the Target Power: Establish the desired probability of detecting an effect (conventionally 0.80 or 0.90).
- Estimate the Expected Effect Size:
- Preferred approach: Calculate from pilot data specific to your model validation context.
- Alternative approach: Use estimates from published literature on similar model systems.
- Last resort: Apply conventional definitions of "small," "medium," and "large" effects for your field.
- Input Parameters into Power Analysis Software: Enter the above parameters into statistical software to calculate the required sample size.
- Consider Practical Constraints: Evaluate the feasibility of obtaining the calculated sample size given time, resource, and participant availability constraints.
- Iterate if Necessary: Explore how variations in effect size or power affect required sample size to make informed trade-offs.
- Document the Justification: Record all assumptions, parameter choices, and calculations in the study protocol.
Troubleshooting and Refinements:
- If the calculated sample size is impractically large, consider:
- Increasing the minimal effect size of interest to a still-meaningful value
- Implementing precision-enhancing measures (see Section 4)
- Exploring alternative statistical designs with greater efficiency
- For complex designs with multiple predictors, use simulation-based power analysis
- Account for anticipated attrition rates by inflating the initial sample size
Visualization of Power Analysis Workflow
Strategies to Enhance Statistical Power
Practical Approaches Without Increasing Sample Size
Table 3: Methods for Improving Statistical Power in Model Validation Research
| Strategy Category | Specific Technique | Mechanism of Action | Implementation Considerations |
|---|---|---|---|
| Enhance Treatment Signal | Increase treatment intensity | Strengthens the true effect size | Balance with safety and practical constraints [103] |
| Improve Measurement | Reduce measurement error | Decreases unexplained variance | Implement consistency checks, triangulation [103] |
| Optimize Study Design | Use multiple measurements | Averages out random fluctuations | Most effective for low-autocorrelation outcomes [103] |
| Increase Sample Homogeneity | Apply inclusion/exclusion criteria | Reduces background variability | Limits generalizability; changes estimand [103] |
| Select Outcomes Strategically | Focus on proximal outcomes | Targets effects closer in causal chain | Choose outcomes less affected by external factors [103] |
| Improve Group Comparability | Use stratification or matching | Increases precision through design | Particularly effective for persistent outcomes [103] |
Advanced Methodological Considerations
- Adaptive Designs: For lengthy model validation studies, consider group sequential designs or sample size re-estimation procedures that allow for modifications based on interim results without compromising Type I error control.
- Bayesian Approaches: In some contexts, Bayesian methods can offer advantages for accumulating evidence across related model validation studies, though they require careful specification of prior distributions.
- Sensitivity Analyses: Conduct power analyses across a range of plausible effect sizes to understand how robust your study design is to misspecification of the expected effect.
Essential Tools for Power Analysis
Research Reagent Solutions for Statistical Power
Table 4: Software Tools for Power Analysis and Sample Size Determination
| Tool Name | Primary Application | Key Features | Access Method |
|---|---|---|---|
| G*Power | General statistical tests | Free, user-friendly interface, wide range of tests | Download from official website [91] |
| PASS | Comprehensive sample size calculation | Extensive procedure library (>1200 tests), detailed documentation | Commercial software [92] |
| R Statistical Package | Customized power analysis | Maximum flexibility, reproducible analyses, simulation capabilities | Open-source environment with power-related packages |
| SAS Power Procedures | Clinical trial and complex designs | Handles sophisticated experimental designs | Commercial statistical software |
| Python StatsModels | Integrated data analysis | Power analysis within broader analytical workflow | Open-source programming language |
Visualization of Power Optimization Strategies
Statistical power considerations must be integrated throughout the research lifecycle in model validation studies. The perils of underpowered studies—including missed discoveries, inflated effect sizes, and contributions to irreproducible literature—can be mitigated through rigorous a priori power analysis and strategic design decisions. Researchers should view adequate power not as an optional methodological refinement but as an essential component of scientifically valid and ethically conducted research. By implementing the protocols and strategies outlined in this document, model validation researchers can enhance the reliability and interpretability of their findings, ultimately contributing to more robust and reproducible scientific progress in drug development and related fields.
Best Practices for Robust Data Collection and Handling Missing Data
For researchers and scientists engaged in hypothesis testing for model validation, particularly in drug development, the integrity of the entire research process hinges on two pillars: the robustness of the initial data collection and the rigor applied to handling incomplete data. Flaws in either stage can compromise model validity, leading to inaccurate predictions, failed clinical trials, and unreliable scientific conclusions. This document outlines detailed application notes and protocols to fortify these critical stages, ensuring that research findings are both statistically sound and scientifically defensible.
Foundational Principles for Robust Data Collection
Robust data collection is the first and most critical line of defense against analytical errors. The following best practices, framed within a research context, are designed to minimize bias and maximize data quality from the outset.
Define Clear Data Collection Objectives
Before collecting a single data point, researchers must establish specific, measurable, achievable, relevant, and time-bound (SMART) goals that anchor the entire data strategy [104]. This transforms data collection from a passive task into a strategic asset.
- Protocol Application: Host a stakeholder workshop with team members from relevant disciplines (e.g., bioinformatics, clinical operations, statistics) to define what constitutes a successful model validation. Create a shared document that outlines each data collection goal, ensuring every objective aligns with the broader hypothesis-testing framework [104].
Implement Data Validation and Quality Checks at Point of Entry
Systematic processes to verify information at the point of entry prevent "garbage in, garbage out" scenarios [104].
- Protocol Application: In electronic Case Report Forms (eCRFs) or data capture systems, enforce field-level validation. This includes range checks for clinical values, format checks for patient identifiers, and mandatory field entry for critical safety data. Automated post-collection cleaning tools should be employed to detect duplicates and standardize fields [104].
Ensure Informed Consent and Privacy Compliance
Adherence to ethical and legal standards like GDPR and HIPAA is non-negotiable. This builds trust and is a fundamental component of robust data practice [104].
- Protocol Application: Use clear, simple language in consent forms. Implement a privacy-by-design architecture in data systems, ensuring robust security measures and access controls for personal and health data. Maintain a secure, auditable trail of consent [104].
Use Standardized Data Collection Methods and Formats
Adopting standardized protocols and formats (e.g., CDISC standards in clinical trials) across all touchpoints ensures interoperability and reduces data cleaning time [104].
- Protocol Application: Develop a data dictionary that defines every variable to be collected, including its name, format (e.g., numeric, date), and permitted values. Utilize field validation in forms to enforce correct formatting, such as requiring dates to follow an ISO 8601 standard [104].
Employ Modern Data Collection Techniques
Leveraging contemporary methods can enhance data richness and accuracy.
- API Data Integration: Connect different software systems (e.g., EMR, lab systems) to automatically exchange data, reducing manual entry errors and creating comprehensive datasets [105].
- IoT and Sensor Data: Use connected devices for real-time, automated collection of physiological data, eliminating manual recording errors [105].
- AI-Powered Analysis: Apply natural language processing to automatically extract insights from unstructured text, such as patient diaries or investigator notes [105].
Understanding and Handling Missing Data
Missing data is a pervasive challenge that, if mishandled, can introduce severe bias and reduce the statistical power of hypothesis tests. A review of studies using UK primary care electronic health records found that 74% of publications reported missing data, yet many used flawed methods to handle it [106].
Classifying the Missingness Mechanism
The appropriate handling method depends on the underlying mechanism, which must be reasoned based on study design and subject-matter knowledge.
Table 1: Classification of Missing Data Mechanisms
| Mechanism | Acronym | Definition | Example |
|---|---|---|---|
| Missing Completely at Random [107] | MCAR | The probability of data being missing is unrelated to both observed and unobserved data. | A lab sample is destroyed due to a power outage, unrelated to the patient's condition or data values. |
| Missing at Random [107] | MAR | The probability of data being missing may depend on observed data but not on the unobserved data itself. | Older patients are more likely to have missing blood pressure readings, but the missingness is random after accounting for age. |
| Missing Not at Random [107] | MNAR | The probability of data being missing depends on the unobserved value itself. | Patients with higher pain scores (the unmeasured variable) are less likely to report their pain level. |
A systematic review of studies using the Clinical Practice Research Datalink (CPRD) reveals a concerning reliance on suboptimal methods for handling missing data [106].
Table 2: Prevalence of Missing Data Handling Methods in CPRD Research (2013-2023)
| Method | Prevalence in Studies | Key Limitations and Risks |
|---|---|---|
| Complete Records Analysis (CRA) | 50 studies (23%) | Leads to loss of statistical power and can introduce bias if the missing data is not MCAR [106]. |
| Missing Indicator Method | 44 studies (20%) | Known to produce inaccurate inferences and is generally considered flawed [106]. |
| Multiple Imputation (MI) | 18 studies (8%) | A robust method, but often poorly specified, leading to erroneous conclusions [106]. |
| Other Methods (e.g., Reclassification, Mean Imputation) | 15 studies (6%) | Varies by method, but often involves unrealistic assumptions [106]. |
Protocols for Handling Missing Data
The following protocols provide a structured approach to managing missing data, aligned with frameworks like the TARMOS (Treatment And Reporting of Missing data in Observational Studies) framework [106].
Protocol 1: Initial Data Assessment and Pattern Analysis
Objective: To characterize the extent and patterns of missingness in the dataset before selecting a handling method. Procedure:
- Quantify Missingness: For each variable, calculate the proportion and count of missing values [107].
- Explore Patterns: Use data visualization (e.g., heatmaps of missingness, summary tables) to investigate if missingness in one variable is related to the values of another. This helps inform whether the data might be MAR.
- Document Findings: Create a summary report of the missing data assessment, including the likely mechanism (MCAR, MAR, MNAR) based on clinical and scientific reasoning.
Protocol 2: Complete Case Analysis (CCA)
Objective: To perform an analysis using only subjects with complete data for all variables in the model. Procedure:
- Subset Data: Create a new dataset that includes only observations with no missing values in the variables planned for the final analytical model.
- Assess Bias: Compare the distribution of key variables (e.g., age, gender) in the complete-case subset against the full dataset to assess potential bias introduced by deletion.
- Application Note: CCA is generally only valid under the strong and often unrealistic MCAR assumption. Its use should be limited to scenarios with a very small amount of missing data or as a baseline comparison for other methods [108].
Protocol 3: Multiple Imputation (MI)
Objective: To account for the uncertainty around missing values by creating several plausible versions of the complete dataset. Procedure:
- Specify the Imputation Model: Include all variables that will be in the final analysis model, as well as auxiliary variables that are predictive of missingness. Use appropriate models (e.g., linear regression for continuous, logistic for binary).
- Generate Imputed Datasets: Create multiple (typically m=5-20) completed datasets using a software procedure (e.g.,
micein R,PROC MIin SAS). The imputation should be based on the observed data distributions. - Analyze Imputed Datasets: Perform the planned hypothesis-testing analysis (e.g., regression model) separately on each of the m imputed datasets.
- Pool Results: Combine the parameter estimates (e.g., regression coefficients) and their standard errors from the m analyses using Rubin's rules to obtain a single set of results that reflects the variability within and between imputations [106].
Protocol 4: Sensitivity Analysis for MNAR
Objective: To test the robustness of the study conclusions to different plausible assumptions about the missing data mechanism. Procedure:
- Define MNAR Scenarios: Develop clinically plausible scenarios for how the missing data might depend on unobserved values. For example, assume that patients with missing outcome data had, on average, a worse outcome than those with observed data.
- Implement Analysis: Use specialized statistical methods, such as selection models or pattern-mixture models, to analyze the data under these different MNAR assumptions.
- Compare Results: If the conclusions of the primary analysis (often under MAR) do not materially change under a range of plausible MNAR scenarios, confidence in the results is strengthened [106].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Data Management and Analysis
| Item / Solution | Function in Research |
|---|---|
| Electronic Data Capture (EDC) System | A standardized platform for collecting clinical trial or experimental data, often with built-in validation checks and audit trails. |
| Statistical Software (R/Python with specialized libraries) | Used for data cleaning, visualization, and advanced statistical analysis, including multiple imputation (e.g., mice in R, scikit-learn in Python) and hypothesis testing. |
| Data Dictionary | A central document defining every variable collected, including its name, data type, format, and permitted values, ensuring consistency and clarity [104]. |
| Version Control System (e.g., Git) | Tracks changes to analysis code and documentation, ensuring reproducibility and facilitating collaboration. |
| Secure, Access-Controlled Database | Provides a compliant environment for storing sensitive research data, protecting integrity and confidentiality. |
Workflow Visualization
The following diagram illustrates the integrated workflow for robust data collection and handling of missing data, from study inception to validated model.
Diagram 1: Integrated Workflow for Data Integrity in Model Validation. This chart outlines the sequential and iterative process from study design through final validation, emphasizing critical decision points for handling missing data.
In the context of hypothesis testing for model validation, particularly in high-stakes fields like drug development, robust data collection and principled handling of missing data are not merely statistical considerations—they are fundamental to scientific integrity. By adopting the structured protocols and best practices outlined herein, researchers can significantly enhance the reliability of their data, the validity of their models, and the credibility of their conclusions. Future work should focus on the wider adoption of robust methods like multiple imputation and the routine implementation of sensitivity analyses to explore the impact of untestable assumptions regarding missing data.
Advanced Validation Frameworks and Comparative Model Assessment
In scientific research, particularly in high-stakes fields like clinical prediction and drug development, the traditional model of single-test validation is increasingly recognized as insufficient. Validation is not a one-time event but an iterative, constructive process essential for building robust, generalizable, and clinically relevant models. This paradigm shift moves beyond a single checkpoint to embrace continuous, evidence-based refinement and contextual performance assessment.
The limitations of one-off validation are starkly revealed when predictive models face real-world data, where shifting populations, evolving clinical practices, and heterogeneous data structures can dramatically degrade performance. Iterative validation frameworks address these challenges by embedding continuous learning and adaptation into the model lifecycle, transforming validation from a gatekeeping function into an integral part of the scientific discovery process [109].
Theoretical Frameworks for Iterative Validation
Iterative Pairwise External Validation (IPEV)
The Iterative Pairwise External Validation (IPEV) framework provides a systematic methodology for contextualizing model performance across multiple datasets. Developed to address the limitations of single-database validation, IPEV employs a rotating development and validation approach that benchmarks models against local alternatives across a network of databases [109].
The framework operates through a two-phase process:
- Baseline and Data-Driven Model Development: For each database in the network, two models are developed: a simple baseline model (e.g., using only age and sex) and a complex data-driven model incorporating comprehensive covariates.
- Rotating Validation: Each developed model is validated across all other databases in the network, creating a comprehensive performance matrix.
This structure provides crucial context for interpreting external validation results, distinguishing between performance drops due to overfitting and those inherent to the new database's information content [109].
Multi-Agent Hypothesis Validation
Multi-agent systems bring specialized, collaborative approaches to hypothesis validation. These frameworks employ distributed agents with defined roles (e.g., specialist, evaluator, orchestrator) that collaboratively test, refine, and validate hypotheses using statistical and formal techniques. This structured collaboration enhances reliability through parallelism, diversity, and iterative feedback mechanisms [110].
Key methodological approaches in these systems include:
- Statistical Hypothesis Testing: Agents use frequentist tests and learn the distribution of test statistics online to validate behavioral models with formal asymptotic guarantees [110].
- Formal Verification and Model Checking: System properties and temporal logic specifications are exhaustively checked against encoded agent protocols [110].
- Bayesian Iterative Frameworks: Agents update posterior beliefs about hypotheses as new evidence accumulates, with quantitative monitoring of informativeness and residual uncertainty [110].
Table: Agent Roles in Multi-Agent Hypothesis Validation Systems
| Agent Role | Primary Function | Application Example |
|---|---|---|
| Specialist Agents | Domain-specific expertise and validation | Omics data vs. literature mining in drug discovery [110] |
| Evaluator/Critic Agents | Aggregate local evaluations, rank hypotheses using multi-criteria scoring | Providing structured feedback for output refinement [110] |
| Meta-Agents / Orchestrators | Manage inter-agent information flow and task delegation | Maximizing coverage while minimizing redundant validation [110] |
Practical Implementation and Protocols
Protocol: Implementing IPEV for Clinical Prediction Models
This protocol outlines the steps for implementing Iterative Pairwise External Validation to assess the transportability of clinical prediction models across multiple observational healthcare databases.
Research Reagent Solutions
Table: Essential Components for IPEV Implementation
| Component | Specification / Example | Function / Rationale |
|---|---|---|
| Database Network | Minimum 3-5 databases (e.g., CCAE, MDCD, Optum EHR) [109] | Enables performance comparison across diverse populations and data structures. |
| Common Data Model (CDM) | OMOP CDM version 5+ [109] | Standardizes format and vocabulary across databases for syntactic and semantic interoperability. |
| Cohort Definitions | Precisely defined target cohort and outcome (e.g., T2DM patients initializing second pharmacological intervention with 1-year HF outcome) [109] | Ensures consistent patient selection and outcome measurement across validation sites. |
| Covariate Sets | 1) Baseline (age, sex); 2) Comprehensive (conditions, drugs, procedures prior to index) [109] | Contextualizes performance gains of complex models against a simple benchmark. |
| Open-Source Software Package | R or Python packages implementing IPEV workflow | Increases consistency, speed, and transparency of the analytical process [109]. |
Methodology
Database Preparation and Harmonization
- Convert all participating databases to the OMOP CDM to ensure syntactic interoperability and standardize vocabularies for semantic interoperability [109].
- Execute standardized cohort identification algorithms across all databases to define the target population and outcome events.
Baseline and Data-Driven Model Development
- In each database (D_i), develop a baseline model using a minimal set of covariates (e.g., age and sex).
- In the same database, develop a data-driven model using a comprehensive set of covariates available in the CDM.
- Follow internal validation best practices for each model, documenting discrimination (AUC) and calibration performance [109].
Iterative Pairwise Validation
- For each model developed in Di, export the model specification (e.g., coefficients, feature definitions) to every other database Dj in the network.
- In each D_j, execute the model against the locally defined cohort to obtain external performance metrics.
- Record the AUC and calibration measures for each model-database pair.
Performance Contextualization and Heatmap Visualization
- Compile all internal and external validation results into a performance matrix.
- Generate a heatmap visualization to compare the external performance of a model in a new database against the performance of models developed natively in that same database [109].
- Identify consistently well-performing models as candidates for clinical use and databases where models consistently underperform as requiring special consideration.
Protocol: Iterative Hypothesis-Driven Customer Development
This protocol adapts the Iterative-Hypothesis customer development method, proven in building successful companies like WP Engine, for scientific research contexts, particularly for understanding user needs and application environments for research tools [111].
Methodology
Define Learning Goals
- Establish a precise list of what you need to learn about your potential users or the clinical environment. Example goals include: user workflows, pain points in current methods, outcome requirements, and decision-making processes [111].
Formulate Explicit Hypotheses
- For each learning goal, write down your current assumptions as testable hypotheses. This practice counters confirmation bias and provides a baseline for measuring learning [111].
- Example Hypothesis: "Researchers will spend more than 30 minutes weekly preparing data for Model X."
Generate Open-Ended Interview Questions
- Design questions that test your hypotheses without leading the participant. Questions should be open-ended to elicit detailed narratives, not simple confirmations [111].
- Example Question for the above hypothesis: "Tell me about the last time you prepared data for analysis. Walk me through each step."
Conduct and Analyze Interviews
- Perform interviews with a focus on listening and learning, not selling or convincing.
- After each interview, update your hypothesis spreadsheet with new insights, marking each hypothesis as "Confirmed," "Rejected," or "Needs Adjustment," and note the evidence [111].
Iterate and Refine
- Use the updated hypotheses to refine your questions for the next interview. Continue this process until patterns emerge and your hypotheses stabilize [111].
Advanced Applications and Emerging Trends
AI-Driven Iteration in Scientific Discovery
Artificial intelligence, particularly Large Language Models (LLMs) and advanced reasoning frameworks, is reshaping iterative validation by accelerating hypothesis generation and refinement.
The Monte Carlo Nash Equilibrium Self-Refine Tree (MC-NEST) framework demonstrates this potential by integrating Monte Carlo Tree Search with Nash Equilibrium strategies to balance the exploration of novel hypotheses with the exploitation of promising leads. In complex domains like protein engineering, MC-NEST can iteratively propose and refine amino acid substitutions (e.g., lysine-for-arginine) to optimize multiple properties simultaneously, such as preserving nuclear localization while enhancing solubility [112].
LLMs are increasingly deployed as "scientific copilots" within iterative workflows. When structured as autonomous agents, they can observe environments, make decisions, and perform actions using external tools, significantly accelerating cycles of hypothesis generation, experiment design, and evidence synthesis [113]. These capabilities are being operationalized through platforms that integrate data-driven techniques with symbolic systems, creating hybrid engines for novel research directions [113].
Iterative Validation in Regulated Environments
In regulated sectors like drug development, iterative processes must balance agility with rigorous documentation. The traditional V-Model development lifecycle emphasizes systematic verification where each development phase has a corresponding testing phase [114]. While sequential, this structured approach can incorporate iterative elements within phases, especially during early research and discovery.
The drug discovery process is inherently iterative, involving repeated cycles of synthesis and characterization to optimize lead compounds. This includes iterative rounds of testing for potency, selectivity, toxicity, and pharmacokinetic properties [115]. The emergence of AI tools in bioinformatics data mining and target validation is further accelerating these iterative cycles, potentially leading to quicker and more effective drug discovery [115].
Table: Comparison of Systematic vs. Iterative Validation Approaches
| Aspect | Systematic Verification (V-Model) | Iterative Validation Approach |
|---|---|---|
| Core Philosophy | Quality-first integration with phase-based verification [114] | Incremental progress through repeated cycles and adaptive learning [114] |
| Testing Integration | Parallel test design for each development phase [114] | Incremental testing within each iteration cycle [114] |
| Risk Management | Systematic risk identification and preventive mitigation [114] | Iterative risk discovery and reduction through early working prototypes [114] |
| Ideal Context | Safety-critical systems, regulated environments with stable requirements [114] | Complex projects with uncertain requirements, need for rapid feedback [114] |
The transition from single-test validation to an iterative, constructive process represents a fundamental maturation of scientific methodology. Frameworks like IPEV provide the contextual performance benchmarking essential for assessing model transportability, while iterative hypothesis-development processes ensure that models address real-world user needs. As AI-driven tools continue to accelerate iteration cycles, the principles of structured validation, contextual interpretation, and continuous refinement become increasingly critical for building trustworthy, impactful, and generalizable scientific models.
The future of validation lies in embracing this iterative construct—not as a series of redundant checks, but as a structured, cumulative process of evidence building that strengthens scientific claims and enhances the utility of predictive models across diverse real-world environments.
Diagrams
Figure 1: Iterative Pairwise External Validation (IPEV) Workflow
Figure 2: Iterative Hypothesis-Development Cycle
Bayesian model comparison offers a powerful alternative to traditional null hypothesis significance testing (NHST) for model validation research, allowing scientists to quantify evidence for and against competing hypotheses. Unlike frequentist approaches, Bayesian methods can directly assess the support for a null model and incorporate prior knowledge into the analysis. Two prominent methods for this purpose are Bayes Factors and the Region of Practical Equivalence (ROPE). This article provides application notes and detailed protocols for implementing these techniques, with a special focus on applications in scientific and drug development contexts. These approaches help researchers move beyond simple dichotomous decisions about model rejection, enabling a more nuanced understanding of model validity and practical significance [116] [117].
Theoretical Foundations
Bayes Factors
The Bayes Factor (BF) is a central tool in Bayesian hypothesis testing that compares the predictive performance of two competing models or hypotheses [116]. Formally, it is defined as the ratio of the marginal likelihoods of the observed data under two hypotheses:
[ BF{10} = \frac{p(D|H1)}{p(D|H_0)} ]
Where ( p(D|H1) ) and ( p(D|H0) ) represent the probability of the observed data D given the alternative hypothesis and null hypothesis, respectively [116]. When BF₁₀ > 1, the data provide stronger evidence for H₁ over H₀, and when BF₁₀ < 1, the evidence favors H₀ over H₁ [116].
A key advantage of Bayes Factors is their ability to quantify evidence in favor of the null hypothesis, addressing a critical limitation of NHST [116]. They also allow evidence to be combined across multiple experiments and permit continuous updating as new data become available [116].
Table 1: Interpretation of Bayes Factor Values [116]
| BF₁₀ Value | Interpretation |
|---|---|
| 1 to 3 | Not worth more than a bare mention |
| 3 to 20 | Positive evidence for H₁ |
| 20 to 150 | Strong evidence for H₁ |
| >150 | Very strong evidence for H₁ |
Region of Practical Equivalence (ROPE)
The Region of Practical Equivalence (ROPE) provides an alternative Bayesian approach for assessing whether a parameter estimate is practically significant [118]. Rather than testing against a point null hypothesis (which is often biologically implausible), the ROPE method defines a range of parameter values around the null value that are considered "practically equivalent" to the null from a scientific perspective [118].
The ROPE procedure involves calculating the highest density interval (HDI) from the posterior distribution and comparing it to the predefined ROPE [118] [119]. The decision rules are:
- If the 95% HDI falls completely outside the ROPE, reject the null value
- If the 95% HDI falls completely inside the ROPE, accept the null value for practical purposes
- If the 95% HDI overlaps the ROPE, withhold judgment [118]
When using the full posterior distribution (rather than the HDI), the null hypothesis is typically rejected if the percentage of the posterior inside the ROPE is less than 2.5%, and accepted if this percentage exceeds 97.5% [118].
Comparative Analysis of Methodologies
Table 2: Comparison of Bayes Factors and ROPE for Model Comparison
| Characteristic | Bayes Factors | ROPE |
|---|---|---|
| Primary Focus | Model comparison and hypothesis testing [116] | Parameter estimation and practical significance [118] |
| Interpretation Basis | Relative evidence between models [116] | Clinical/practical relevance of effect sizes [118] |
| Handling of Null Hypothesis | Direct quantification of evidence for H₀ [116] | Assessment of practical equivalence to H₀ [118] |
| Prior Dependence | Highly sensitive to prior specifications [116] | Less sensitive to priors when using posterior samples [118] |
| Computational Demands | Can be challenging (requires marginal likelihoods) [116] | Generally straightforward (uses posterior samples) [118] |
| Default Ranges | Not applicable | ±0.1 for standardized parameters; ±0.05 for correlations [118] |
Application Protocols
Protocol 1: Bayes Factors for Model Comparison
Purpose: To compare competing models using Bayes Factors.
Materials/Software:
- Statistical software with Bayesian capabilities (R, Python, Stan)
- bayestestR package (R) for analysis [118]
- Prior knowledge for model specification
Procedure:
Specify Models: Clearly define competing models (H₀ and H₁) with associated likelihood functions and prior distributions [116].
Choose Priors: Select appropriate prior distributions for parameters. Consider using:
- Default priors for initial analyses
- Informative priors based on domain knowledge
- Sensitivity analysis to assess prior impact [116]
Compute Marginal Likelihoods: Calculate the marginal probability of the data under each model: [ p(D|Hi) = \int p(D|\thetai,Hi)p(\thetai|Hi)d\thetai ] This can be computationally challenging; use methods like bridge sampling, importance sampling, or MCMC [116].
Calculate Bayes Factor: Compute BF₁₀ = p(D|H₁)/p(D|H₀) [116].
Interpret Results: Use the interpretation table (Table 1) to assess strength of evidence [116].
Example Application: In infectious disease modeling, researchers used Bayes Factors to compare five different transmission models for SARS-CoV-2, identifying super-spreading events as a key mechanism [120] [121].
Protocol 2: ROPE for Practical Equivalence Testing
Purpose: To determine if an effect is practically equivalent to a null value.
Materials/Software:
- Bayesian estimation software (R, Stan, JAGS)
- bayestestR package for ROPE calculation [118]
- Domain knowledge for ROPE specification
Procedure:
Define ROPE Range: Establish appropriate bounds based on:
Generate Posterior Distribution: Obtain posterior samples for parameters of interest using MCMC or other Bayesian methods [118].
Calculate HDI: Compute the 89% or 95% Highest Density Interval from the posterior distribution [118].
Compare HDI to ROPE: Apply decision rules to determine practical equivalence [118].
Report Percentage in ROPE: Calculate and report the proportion of the posterior distribution falling within the ROPE [118].
Important Considerations:
- Be cautious of parameter scaling, as ROPE results are sensitive to the units of measurement [118]
- Check for multicollinearity, as correlated parameters can invalidate ROPE conclusions [118]
- Consider using the full posterior distribution (ci = 1 in bayestestR) for more sensitive analysis [118]
Example Application: In multi-domain building science research, ROPE was used to identify null effects across different environmental domains, helping to refute false theories and promote cumulative research [117].
Workflow Visualization
Figure 1: Workflow for Regional of Practical Equivalence (ROPE) analysis, illustrating the key steps from model specification to decision making [118].
Figure 2: Workflow for Bayes Factor calculation and interpretation, showing the process from model definition to evidence assessment [116].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Tool/Reagent | Function/Purpose | Application Notes |
|---|---|---|
| bayestestR (R package) | Comprehensive Bayesian analysis [118] | Calculates ROPE, HDI, Bayes Factors; user-friendly interface |
| BEST (R package) | Bayesian estimation supersedes t-test [119] | Power analysis for ROPE; uses simulation-based methods |
| Bridge Sampling | Computes marginal likelihoods [116] | Essential for Bayes Factor calculation with complex models |
| MCMC Methods | Generates posterior distributions [120] | Stan, JAGS, or PyMC for sampling from posterior |
| Default ROPE Ranges | Standardized reference values [118] | ±0.1 for standardized parameters; adjust based on context |
| Interpretation Scales | Standardized evidence assessment [116] | Jeffreys or Kass-Raftery scales for Bayes Factors |
Advanced Applications and Considerations
Drug Development Applications
In pharmaceutical research, Bayesian model comparison methods offer significant advantages for model validation. For example, in early-stage drug screening, transformer-based models can predict ADME-T (absorption, distribution, metabolism, excretion, and toxicity) properties, and Bayesian methods can validate these models against traditional approaches [122]. With approximately 40% of drug candidates failing during ADME-T testing, robust model validation is crucial for reducing late-stage failures and development costs [122].
Bayesian risk-based decision methods have been specifically developed for computational model validation under uncertainty [123]. These approaches define an expected risk or cost function based on decision costs, likelihoods, and priors for each hypothesis, with minimization of this risk guiding the validation decision [123].
Critical Methodological Considerations
Prior Sensitivity: Bayes Factors can be highly sensitive to prior choices, particularly with small sample sizes [116]. Always conduct sensitivity analyses with different prior specifications to assess robustness [116].
Computational Challenges: Calculating marginal likelihoods for Bayes Factors can be computationally intensive, especially for complex models [116]. Modern approximation methods like bridge sampling or importance sampling can help address these challenges [116].
ROPE Specification: The appropriateness of ROPE conclusions heavily depends on scientifically justified ROPE ranges [118]. Always justify these bounds based on domain knowledge rather than relying solely on default values [118].
Multiple Comparisons: Unlike frequentist methods, Bayesian approaches don't automatically control error rates across multiple tests [119]. Consider partial pooling or hierarchical modeling when dealing with multiple comparisons [119].
Bayes Factors and ROPE provide complementary approaches for Bayesian model comparison and hypothesis testing. While Bayes Factors excel at comparing competing models directly, ROPE is particularly valuable for assessing practical significance of parameter estimates. For model validation research, these methods offer substantial advantages over traditional NHST, including the ability to quantify evidence for null hypotheses, incorporate prior knowledge, and make more nuanced decisions about model adequacy. By implementing the protocols and considerations outlined in these application notes, researchers in drug development and other scientific fields can enhance their model validation practices and make more informed decisions based on a comprehensive assessment of statistical evidence.
Using Cross-Validation and Information Criteria (LOO) for Model Selection
Within the framework of hypothesis testing for model validation, selecting the most appropriate model is a fundamental step in ensuring research conclusions are robust and reliable. This document outlines detailed application notes and protocols for using cross-validation, particularly Leave-One-Out Cross-Validation (LOOCV) and the Pareto Smoothed Importance Sampling approximation to LOO (PSIS-LOO), for model selection. These methods provide a principled Bayesian approach to evaluating a model's out-of-sample predictive performance, moving beyond simple null hypothesis testing to a more nuanced comparison of competing scientific theories embodied in statistical models [73]. This is especially critical in fields like drug development, where model choice can have significant practical implications.
Core Concepts and Theoretic Background
The Goal of Model Selection
The primary aim is to identify the model that generalizes best to new, unseen data. Traditional in-sample fit measures (e.g., R²) are often overly optimistic, as they reward model complexity without quantifying overfitting [124]. Cross-validation and information criteria approximate the model's expected log predictive density (ELPD) on new data, providing a more realistic performance assessment [125] [126].
Key Information Criteria and Cross-Validation Methods
Leave-One-Out Cross-Validation (LOOCV) is a model validation technique where the number of folds k is equal to the number of samples n in the dataset [127] [128]. For each data point i, a model is trained on all other n-1 points and validated on the omitted point. The results are averaged to produce an estimate of the model's predictive performance. While conceptually ideal, its direct computation is often prohibitively expensive for large datasets, as it requires fitting the model n times [128].
The PSIS-LOO method efficiently approximates exact LOOCV without needing to refit the model n times. It uses importance sampling to estimate each LOO predictive density, and applies Pareto smoothing to the distribution of importance weights for a more stable and robust estimate [125] [126]. The key output is the elpd_loo, the expected log pointwise predictive density for a new dataset, which is estimated from the data [125] [126]. The LOO Information Criterion (LOOIC) is simply -2 * elpd_loo [125] [126].
K-Fold Cross-Validation provides a practical alternative by splitting the data into K subsets (typically 5 or 10). The model is trained K times, each time using K-1 folds for training and the remaining fold for validation [127] [128]. This method offers a good balance between computational cost and reliable error estimation.
Table 1: Comparison of Model Validation Techniques
| Technique | Key Principle | Computational Cost | Best For | Key Assumptions/Outputs |
|---|---|---|---|---|
| Exact LOOCV | Uses each of the n data points as a test set once [128]. |
Very High (requires n model fits) |
Small datasets [127]. | Minimal bias in performance estimation [128]. |
| PSIS-LOO | Approximates LOOCV using importance sampling and Pareto smoothing [125]. | Low (requires only 1 model fit) | General use, particularly when n is large [125] [126]. |
Requires checking Pareto k diagnostics [125]. |
| K-Fold CV | Splits data into K folds; each fold serves as a validation set once [127]. |
Moderate (requires K model fits) |
Most common practice; a good default choice [128]. | Assumes data is independently and identically distributed. |
| Hold-Out | Simple split into a single training and test set (e.g., 70/30 or 80/20) [127]. | Very Low (requires 1 model fit) | Very large datasets [127] [128]. | Results can be highly sensitive to the specific data split [128]. |
Experimental Protocols
This section provides a step-by-step workflow for performing model validation and selection using PSIS-LOO and K-Fold Cross-Validation.
Workflow for Model Validation and Selection
The following diagram outlines the overarching process for comparing models using predictive validation techniques.
Protocol 1: PSIS-LOO with Subsampling for Large Datasets
This protocol is designed for efficient model evaluation with large data, using the loo package in R [125] [126].
Implement the Log-Likelihood Function in R
Fit the Model using Stan
- Code the Stan model. For large data, it is more efficient to compute the log-likelihood in R post-fitting, so it is typically not computed in the
generated quantitiesblock [125] [126]. - Use RStan to sample from the model posterior.
- Extract the posterior draws (e.g.,
parameter_draws_1 <- extract(fit_1)$beta).
- Code the Stan model. For large data, it is more efficient to compute the log-likelihood in R post-fitting, so it is typically not computed in the
Compute Relative Efficiency
- Calculate the relative effective sample size (
r_eff) to adjust for MCMC estimation error. This is an optional but recommended step [125].
- Calculate the relative effective sample size (
Perform Subsampled PSIS-LOO
Diagnostic Check
Protocol 2: K-Fold and Leave-One-Out Cross-Validation in Python
This protocol uses scikit-learn for classic cross-validation, suitable for non-Bayesian or smaller-scale models [127].
Prepare the Data and Model
- Load the dataset and instantiate a model object.
Execute K-Fold Cross-Validation
- Define the K-Fold splitter and run the cross-validation.
Execute Leave-One-Out Cross-Validation
Protocol 3: Formal Model Comparison
This protocol details how to statistically compare models after computing their validation metrics.
Using
loo_compare(for LOO objects)- After computing
looobjects (e.g.,loo_ss_1for model 1 andloo_ss_2for model 2) for all candidate models, use theloo_compare()function [126]. - Crucial Step for Subsampling: To ensure a fair comparison, both models must be evaluated on the same subsample of observations. Pass the first
looobject to theobservationsargument when creating the second [126]. - The output ranks models by their
elpd_loo. The model with the highestelpd_loo(lowestlooic) is preferred. Theelpd_diffcolumn shows the difference in ELPD from the top model, andse_diffis the standard error of this difference. Aelpd_diffgreater than 2-4 times itsse_diffis generally considered substantial evidence in favor of the top model [126].
- After computing
Interpreting Comparison Results
- The focus should be on the difference in performance (
elpd_diff) and its uncertainty (se_diff), not just on selecting a single "best" model. This embraces the inherent uncertainty in model selection, as emphasized in Bayesian practice [73]. - Model stacking can be used to form a weighted combination of models, rather than relying on a single model, which can improve predictive performance and account for model uncertainty [73].
- The focus should be on the difference in performance (
The Scientist's Toolkit: Research Reagent Solutions
In computational research, software packages and statistical libraries serve as the essential "reagents" for conducting model validation experiments.
Table 2: Essential Software and Packages for Model Validation
| Tool/Reagent | Function/Description | Primary Use Case |
|---|---|---|
R loo package |
Implements PSIS-LOO, approximate LOO with subsampling, and model comparison via loo_compare [125] [126]. |
The primary tool for Bayesian model evaluation and comparison in R. |
| RStan / CmdStanR | Interfaces to the Stan probabilistic programming language for full Bayesian inference [125]. | Fitting complex Bayesian models to be evaluated with the loo package. |
Python scikit-learn |
Provides a wide array of model validation methods, including KFold, LeaveOneOut, and cross_val_score [127]. |
Performing standard K-Fold and LOOCV for machine learning models in Python. |
Python PyTorch / TensorFlow |
Deep learning frameworks with utilities for creating validation sets and custom evaluation loops [124]. | Validating complex deep learning models. |
Diagnostic Plots (e.g., plot(loo_obj)) |
Visualizes Pareto k diagnostics to assess the reliability of the PSIS-LOO approximation [125]. |
Critical diagnostic step after computing PSIS-LOO. |
- Embrace Uncertainty: Model selection is not about finding one "true" model, but about quantifying evidence for different models given the data. Use the standard errors of ELPD differences to guide interpretation [73].
- Validate for the Right Reason: LOO and cross-validation tell you which model is likely to have better predictive performance, not necessarily if an effect is "present." For the latter, inspecting the posterior distribution of parameters (e.g., determining a range of practical equivalence) is often more informative [73].
- Always Check Diagnostics: For PSIS-LOO, always examine the Pareto
kstatistics. Highkvalues (>0.7) suggest the LOO estimate may be unreliable [125] [126]. - Avoid Data Leakage: Ensure that the test data in any validation protocol is never used in training. This is crucial for obtaining unbiased performance estimates [124].
- Use Multiple Metrics: While LOO/ELPD is a powerful general measure, also consider domain-specific performance metrics (e.g., precision, recall, ROC-AUC) that align with the ultimate business or research objective [124].
Integrating cross-validation and information criteria like PSIS-LOO into a model validation workflow provides a robust, prediction-focused framework for hypothesis testing and model selection. The protocols outlined here—from efficient Bayesian computation with large data to standard cross-validation in Python—offer researchers and drug development professionals a clear path to making more reliable, data-driven decisions about their statistical models. This approach moves beyond simplistic null hypothesis significance testing, encouraging a quantitative comparison of how well different models, representing different scientific hypotheses, actually predict new data.
In the rigorous field of model validation research, particularly within drug development and scientific discovery, embracing model uncertainty is paramount for robust and reproducible findings. Two advanced methodological frameworks have emerged to systematically address this challenge: Model Stacking and Multiverse Analysis. Model stacking, also known as stacked generalization, is an ensemble machine learning technique that combines the predictions of multiple base models to improve predictive performance and account for uncertainty in model selection [129] [130]. Multiverse analysis provides a comprehensive framework for assessing the robustness of scientific results across numerous defensible data processing and analysis pipelines, thereby quantifying the uncertainty inherent in analytical choices [131] [132]. This article presents detailed application notes and protocols for implementing these approaches within hypothesis testing frameworks for model validation, providing researchers with practical tools to enhance the reliability of their findings.
Theoretical Foundations
Model Stacking: Conceptual Framework
Model stacking operates on the principle that no single model can capture all complexities and nuances in a dataset. By combining multiple models, stacking aims to create a more robust and accurate prediction system [130]. The technique employs a two-level architecture: multiple base models (level-0) are trained independently on the same dataset, and their predictions are then used as input features for a higher-level meta-model (level-1), which learns to optimally combine these predictions [129] [133]. This approach reduces variance and bias in the final prediction, often resulting in superior predictive performance compared to any single model [130]. The theoretical justification for stacking was formalized through the Super Learner algorithm, which demonstrates that stacked ensembles represent an asymptotically optimal system for learning [133].
Multiverse Analysis: Philosophical Underpinnings
Multiverse analysis addresses the "researcher degrees of freedom" problem - the flexibility researchers have to choose from multiple defensible options at various stages of data processing and analysis [131]. This methodological approach involves systematically computing and reporting results across all reasonable combinations of analytical choices, thereby making explicit the uncertainty that arises from pipeline selection [131] [132]. Rather than relying on a single analysis pipeline, multiverse analysis generates a "garden of forking paths" where each path represents a defensible analytical approach [131]. This comprehensive assessment allows researchers to distinguish robust findings that persist across multiple analytical scenarios from those that are highly dependent on specific analytical choices.
Complementary Approaches to Uncertainty Quantification
While model stacking and multiverse analysis operate at different levels of the research pipeline, they share the fundamental goal of quantifying and addressing uncertainty. Model stacking addresses uncertainty in model selection, while multiverse analysis addresses uncertainty in analytical pipeline specification. When used in conjunction, these approaches provide researchers with a comprehensive framework for acknowledging and accounting for multiple sources of uncertainty in the research process, leading to more reliable and interpretable results.
Experimental Protocols
Protocol 1: Implementing Model Stacking for Predictive Modeling
Objective: To create a stacked ensemble model that combines multiple base algorithms for improved predictive performance in a validation task.
Materials: Dataset partitioned into training, validation, and test sets; computational environment with machine learning libraries (e.g., scikit-learn, H2O, SuperLearner).
Procedure:
- Data Preparation: Split the dataset into training (70%), validation (15%), and test (15%) sets, ensuring consistent preprocessing across all partitions [129].
- Base Model Selection: Choose diverse base algorithms (e.g., decision trees, random forests, gradient boosting, support vector machines, neural networks) that are likely to make different types of errors [130] [133].
- Training Base Models:
- Train each base model on the training set using k-fold cross-validation (typically k=10) with identical fold assignments across all models [133].
- Preserve the cross-validated predictions from each model for meta-model training.
- Meta-Model Development:
- Prediction and Evaluation:
- Generate predictions on new data using the base models.
- Feed these predictions into the trained meta-model to produce final ensemble predictions [130].
- Evaluate performance on the held-out test set using appropriate metrics (e.g., RMSE, R² for regression; accuracy, F1-score for classification) [129].
Troubleshooting Tips:
- Ensure base model diversity to maximize ensemble performance gains.
- Guard against data leakage by using cross-validated predictions for meta-training.
- Regularize the meta-model if using many base learners to prevent overfitting.
Protocol 2: Conducting Multiverse Analysis for Robustness Assessment
Objective: To systematically evaluate the robustness of research findings across all defensible analytical pipelines.
Materials: Raw dataset; computational environment with multiverse analysis tools (e.g., R package multiverse, Systematic Multiverse Analysis Registration Tool - SMART) [131] [132].
Procedure:
- Decision Node Identification:
- Option Specification:
- Enumerate all reasonable alternatives at each decision node.
- Define any constraints or dependencies between options across different nodes.
- Multiverse Construction:
- Generate all possible combinations of options across decision nodes.
- Eliminate combinations deemed indefensible based on domain knowledge or theoretical considerations [131].
- Pipeline Execution:
- Implement code to execute all defensible analytical pipelines, either through custom scripting or using specialized packages like
multiversein R [132]. - Compute the effect of interest and associated statistics for each pipeline.
- Implement code to execute all defensible analytical pipelines, either through custom scripting or using specialized packages like
- Results Synthesis:
- Visualize the distribution of effect sizes and statistical significance across all pipelines.
- Calculate the proportion of pipelines that support the hypothesized effect.
- Identify decision nodes that have the largest impact on results.
Troubleshooting Tips:
- Use the SMART tool for systematic documentation of decision-making during multiverse construction [131].
- Consider computational constraints; for very large multiverses, use random sampling of pipelines.
- Pre-register the multiverse analysis plan to enhance transparency and credibility.
Protocol 3: Integrated Stacking and Multiverse Analysis for Comprehensive Validation
Objective: To combine model stacking and multiverse analysis for maximum robustness in model validation.
Materials: As in Protocols 1 and 2; high-performance computing resources may be necessary for computationally intensive analyses.
Procedure:
- Multiverse of Stacked Ensembles:
- Implement a multiverse analysis where different decision nodes control aspects of the stacking procedure (e.g., choice of base learners, meta-learning algorithm, hyperparameters).
- Execute the full multiverse of stacked ensembles.
- Performance Assessment:
- Evaluate each stacked ensemble on validation metrics.
- Analyze the variation in performance across the multiverse of ensembles.
- Stability Analysis:
- Identify ensemble configurations that perform consistently well across different data processing decisions.
- Assess the sensitivity of conclusions to analytical choices at both the model and preprocessing levels.
Data Presentation and Analysis
Quantitative Comparison of Modeling Approaches
Table 1 presents a comparative analysis of modeling approaches applied to welding quality prediction, demonstrating the performance advantages of stacking ensemble learning compared to individual models and multitask neural networks [134].
Table 1: Performance comparison of multitask neural networks vs. stacking ensemble learning for predicting welding parameters [134]
| Model Type | Output Parameter | RMSE | R² | Variance Explained |
|---|---|---|---|---|
| Multitask Neural Network (MTNN) | UTS | 0.1288 | 0.6724 | 67.24% |
| Weld Hardness | 0.0886 | 0.9215 | 92.15% | |
| HAZ Hardness | 0.1125 | 0.8407 | 84.07% | |
| Stacking Ensemble Learning | UTS | 0.0263 | 0.9863 | 98.63% |
| Weld Hardness | 0.0467 | 0.9782 | 97.82% | |
| HAZ Hardness | 0.1109 | 0.8453 | 84.53% |
The data reveal that stacking ensemble learning outperformed multitask neural networks on most metrics, particularly for UTS prediction where R² improved from 0.67 to 0.99 [134]. This demonstrates stacking's capability to produce highly accurate, task-specific predictions while maintaining strong performance across multiple related outcomes.
Multiverse Analysis Results Framework
Table 2 illustrates a hypothetical multiverse analysis results structure, showing how effect sizes and significance vary across different analytical choices.
Table 2: Illustrative multiverse analysis results framework for hypothesis testing
| Pipeline ID | Outlier Treatment | Transformation | Covariate Set | Effect Size | P-value | Significant |
|---|---|---|---|---|---|---|
| 1 | Remove >3SD | Log | Minimal | 0.45 | 0.032 | Yes |
| 2 | Remove >3SD | Log | Full | 0.38 | 0.048 | Yes |
| 3 | Remove >3SD | None | Minimal | 0.51 | 0.021 | Yes |
| 4 | Remove >3SD | None | Full | 0.42 | 0.039 | Yes |
| 5 | Winsorize >3SD | Log | Minimal | 0.41 | 0.035 | Yes |
| ... | ... | ... | ... | ... | ... | ... |
| 42 | None | None | Full | 0.18 | 0.217 | No |
| Summary | % Significant | Mean Effect | Effect Range | Robustness Score | ||
| 76.2% | 0.39 | 0.18-0.51 | 0.72 |
This structured presentation enables researchers to quickly assess the robustness of findings across analytical choices and identify decision points that most strongly influence results.
Visualization of Methodologies
Model Stacking Workflow
Model Stacking Architecture
The diagram illustrates the two-level architecture of model stacking. Base models (Level-0) are trained on the original data, and their cross-validated predictions form a new feature matrix (level-one data) that trains the meta-model (Level-1), which produces the final prediction [129] [133].
Multiverse Analysis Structure
Multiverse Analysis Decision Tree
This visualization depicts the branching structure of multiverse analysis, where each decision node represents a point in the analytical workflow with multiple defensible options, and each path through the tree constitutes a unique analytical universe [131] [132].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Computational tools and packages for implementing model stacking and multiverse analysis
| Tool/Package | Primary Function | Application Context | Key Features |
|---|---|---|---|
| H2O [133] | Scalable machine learning platform | Model stacking implementation | Efficient stacked ensemble training with cross-validation, support for multiple meta-learners |
| SuperLearner [133] | Ensemble learning package | Model stacking in R | Original Super Learner algorithm, interfaces with 30+ algorithms |
| multiverse [132] | Multiverse analysis in R | Creating and managing multiverse analyses | Domain-specific language for declaring alternative analysis paths, results extraction and visualization |
| SMART [131] | Systematic Multiverse Analysis Registration Tool | Transparent multiverse construction | Guided workflow for defining defensible pipelines, exportable documentation for preregistration |
| scikit-learn | Python machine learning library | Model stacking implementation | Pipeline creation, cross-validation, and ensemble methods |
| caretEnsemble [133] | R package for model stacking | Combining caret models | Bootstrap-based stacking implementation |
These computational tools provide the necessary infrastructure for implementing the methodologies described in this article. Researchers should select tools based on their computational environment, programming language preference, and specific analysis requirements.
Application Notes
Case Study: Hurricane Name Femininity Analysis
A compelling example of multiverse analysis comes from a reexamination of a study claiming that hurricanes with more feminine names cause more deaths [132]. The original analysis involved at least four key decision points with defensible alternatives:
- Outlier exclusion: Whether and how to exclude extreme observations
- Data transformation: Choice of transformation for outcome variable
- Covariate selection: Which control variables to include
- Model specification: Functional form of the statistical model
When implemented as a multiverse analysis, results demonstrated that the original finding was highly sensitive to analytical choices, with many reasonable pipelines showing no significant effect [132]. This case highlights how multiverse analysis can reveal the fragility of claims that appear robust in a single analysis.
Case Study: Welding Quality Prediction
In a comparative study of multitask neural networks versus stacking ensemble learning for predicting welding parameters, stacking demonstrated superior performance on task-specific predictions [134]. For ultimate tensile strength (UTS) prediction, stacking achieved an R² of 0.986 compared to 0.672 for the multitask approach, while maintaining strong performance on related tasks like weld hardness and HAZ hardness prediction [134]. This illustrates stacking's advantage in scenarios where high precision is required for specific outcomes.
Implementation Considerations for Drug Development
In pharmaceutical research and drug development, where model validation is critical for regulatory approval, several specific considerations apply:
- Documentation: Maintain exhaustive documentation of all analytical decisions and their justifications, particularly for regulatory submissions.
- Computational Efficiency: For large-scale omics data or clinical trial simulations, consider computational constraints when designing multiverse analyses.
- Interpretability: In safety-critical applications, ensure that stacked ensembles remain interpretable through techniques like feature importance analysis.
- Validation Frameworks: Integrate stacking and multiverse approaches within established validation frameworks such as FDA's Model-Informed Drug Development guidelines.
Model stacking and multiverse analysis represent paradigm shifts in how researchers approach model validation and hypothesis testing. By systematically accounting for model selection uncertainty and analytical flexibility, these methodologies promote more robust, reproducible, and interpretable research findings. The protocols, visualizations, and toolkits provided in this article offer practical guidance for implementing these approaches across diverse research contexts, with particular relevance for drug development professionals and scientific researchers engaged in model validation. As the scientific community continues to prioritize research transparency and robustness, these methodologies will play an increasingly central role in the validation of scientific claims.
In the precision medicine era, the validation of artificial intelligence (AI) models in clinical and drug development settings requires a robust framework that integrates quantitative predictions with expert human knowledge [135]. Model validation is not a single event but an iterative, constructive process of building trust by repeatedly testing model predictions against new experimental and observational data [8]. This protocol outlines detailed methodologies for performing qualitative checks and posterior predictive assessments, framed within the broader context of hypothesis testing for model validation research. These procedures are designed for researchers, scientists, and drug development professionals working to ensure their predictive models are reliable, interpretable, and clinically actionable.
Theoretical Framework: Validation as Hypothesis Testing
Model validation is fundamentally a process of statistical hypothesis testing [8]. Within this framework:
- The null hypothesis (H0) posits that the computational model is an accurate representation of the real-world system from the perspective of its intended uses.
- The alternative hypothesis (H1) represents all other possible models or states.
The validation process never "proves" H0 true; it either fails to reject H0 (suggesting the model is sufficient given the available data) or rejects H0 in favor of a more effective alternative [8]. This process is inherently iterative—each successful comparison between model predictions and experimental outcomes increases trust in the model's reliability without ever achieving absolute certainty.
Table 1: Core Concepts in Model Validation as Hypothesis Testing
| Concept | Definition | Interpretation in Validation Context |
|---|---|---|
| Null Hypothesis (H0) | The model is sufficiently accurate for its intended use. | Failure to reject adds evidence for model utility; rejection indicates need for model refinement. |
| Alternative Hypothesis (H1) | The model is not sufficiently accurate. | Represents all possible reasons the model may be inadequate. |
| Type I Error | Rejecting a valid model. | Incorrectly concluding a useful model is inadequate. |
| Type II Error | Failing to reject an invalid model. | Incorrectly retaining a model that provides poor predictions. |
| Statistical Power | Probability of correctly rejecting an inadequate model. | Increased through well-designed experiments and appropriate metrics. |
| Iterative Trust Building | Progressive accumulation of favorable test outcomes. | Measured through increasing Vprior value in validation algorithms [8]. |
Experimental Protocols
Protocol for Qualitative Expert Assessment
Purpose: To systematically integrate domain expertise for identifying model limitations that may not be apparent through quantitative metrics alone.
Materials:
- Trained predictive model with documented architecture and training data
- Validation dataset with observed outcomes
- Panel of domain experts (minimum 3 recommended)
- Standardized assessment rubric
Procedure:
- Preparation Phase:
- Select case examples representing the full spectrum of model performance (best, worst, and average cases based on quantitative metrics).
- Prepare model inputs and outputs in an interpretable format for expert review.
- Establish a structured feedback mechanism using the assessment rubric.
Expert Evaluation:
- Present cases to experts without revealing model predictions initially.
- Experts document their expected outcomes based on experience.
- Reveal model predictions and allow experts to identify:
- Cases where model predictions align with expert intuition
- Cases where model predictions contradict expert knowledge
- Any systematic patterns in model errors
Analysis and Integration:
- Tabulate expert feedback and identify consensus points.
- Prioritize discrepancies for model refinement.
- Document expert-suggested improvements for implementation.
Table 2: Expert Assessment Rubric Template
| Assessment Dimension | Rating Scale | Notes & Examples |
|---|---|---|
| Clinical Plausibility | 1 (Implausible) to 5 (Highly Plausible) | Document specific biological/clinical rationale for ratings |
| Risk Assessment | 1 (Unacceptable Risk) to 5 (Minimal Risk) | Note any predictions that would lead to dangerous decisions |
| Context Appropriateness | 1 (Context Inappropriate) to 5 (Optimal for Context) | Evaluate fit for intended clinical scenario |
| Uncertainty Communication | 1 (Misleading) to 5 (Clearly Communicated) | Assess how well model conveys confidence in predictions |
Protocol for Posterior Predictive Assessment
Purpose: To quantitatively evaluate model performance by comparing model-generated predictions with actual observed outcomes.
Materials:
- Fully trained predictive model
- Test dataset not used during model training
- Statistical software capable of implementing posterior predictive checks
- Computing resources appropriate for model complexity
Procedure:
- Model Output Generation:
- For each observation in the test dataset, generate posterior predictive distributions.
- For Bayesian models, use posterior samples; for frequentist models, use appropriate uncertainty quantification methods.
Discrepancy Measure Calculation:
- Define test quantities T(y,θ) that capture clinically relevant aspects of the data.
- Calculate T(yrep,θ) for replicated datasets and T(y,θ) for observed data.
- Compute posterior predictive p-values: pB = Pr(T(yrep,θ) ≥ T(y,θ)|y)
Assessment and Interpretation:
- Extreme p-values (close to 0 or 1) indicate model inadequacy for that test quantity.
- Focus on clinically meaningful discrepancies rather than statistical significance alone.
- Iteratively refine model based on identified deficiencies.
Workflow Diagram:
Case Study: Precision Radiotherapy Application
The following case study demonstrates the application of these validation techniques in a non-small cell lung cancer (NSCLC) radiotherapy context, where AI recommendations for dose prescriptions must integrate with physician expertise [135].
Study Design and Data Collection
Objective: To validate a deep Q-learning model for optimizing radiation dose prescriptions in NSCLC patients, balancing tumor control (LC) against side effects (RP2) [135].
Dataset:
- 67 NSCLC patients from a prospective study
- Three-stage radiotherapy protocol with adaptive dosing
- Patient variables monitored at each stage (s1, s2, s3)
- Binary outcomes: Local Control (LC) and Radiation Pneumonitis (RP2)
Reward Function: The treatment optimization goal was formalized through a reward function [135]: R = -10 × ((1-Prob[LC=1])⁸ + (Prob[RP2=1]/0.57)⁸)1/8 + 3.281
Table 3: Quantitative Data Summary for NSCLC Radiotherapy Study
| Variable Category | Specific Variables | Measurement Scale | Summary Statistics |
|---|---|---|---|
| Patient Characteristics | Tumor stage, Performance status, Comorbidities | Categorical & Continuous | Not specified in source |
| Treatment Parameters | Dose per fraction (a1, a2, a3) | Continuous (Gy/fraction) | Stage 1-2: ~2 Gy/fraction, Stage 3: 2.85-5.0 Gy/fraction [135] |
| Outcome Measures | Local Control (y1), Radiation Pneumonitis (y2) | Binary (0/1) | Not specified in source |
| Model Performance | Reward function value | Continuous | Benchmark: Positive values when LC≥70% and RP2≤17.2% [135] |
Implementation of Validation Framework
Integration Methodology: Gaussian Process (GP) models were integrated with Deep Neural Networks (DNNs) to quantify uncertainty in both physician decisions and AI recommendations [135]. This hybrid approach enabled:
- Uncertainty Quantification: GP models measured confidence in treatment outcomes for both human and AI recommendations.
- Decision Guidance: The system identified patient variable regions where AI recommendations significantly outperformed physician prescriptions.
- Adaptive Learning: Cases where physician decisions yielded better outcomes were used to refine the AI model.
Validation Workflow Diagram:
Research Reagent Solutions
Table 4: Essential Computational and Analytical Resources
| Resource Category | Specific Tool/Platform | Function in Validation Protocol |
|---|---|---|
| Statistical Computing | R, Python with PyMC3/Stan | Implementation of posterior predictive checks and Bayesian modeling |
| Deep Learning Framework | TensorFlow, PyTorch | Development and training of deep Q-network models |
| Uncertainty Quantification | Gaussian Process libraries (GPy, scikit-learn) | Measuring confidence in predictions and expert decisions |
| Data Management | Electronic Lab Notebooks (e.g., SciNote) | Protocol documentation and experimental data traceability [136] |
| Visualization | Graphviz, matplotlib, seaborn | Creation of diagnostic plots and workflow diagrams |
| Color Contrast Verification | axe DevTools, color contrast analyzers | Ensuring accessibility compliance in all visualizations [137] [138] |
Interpretation Guidelines
Assessing Validation Outcomes
Strong Evidence for Model Validity:
- Posterior predictive p-values between 0.05 and 0.95 for key test quantities
- Expert consensus that >90% of model predictions are clinically plausible
- No systematic patterns of failure across patient subgroups
Moderate Evidence for Model Validity:
- Isolated discrepancies in posterior predictive checks that don't affect clinical utility
- Expert identification of minor limitations with straightforward mitigations
- Consistent performance across majority of intended use cases
Inadequate Model Validity:
- Extreme posterior predictive p-values (<0.01 or >0.99) for clinically critical test quantities
- Expert rejection of >25% of model predictions as clinically implausible
- Systematic biases against specific patient subgroups
Iterative Trust Building
The validation process should document increasing trust through a quantitative Vprior metric [8]:
- Begin with Vprior = 1 for new models
- Increase Vprior with each successful experimental validation
- Decrease Vprior with each significant model failure
- Establish organization-specific thresholds for model deployment based on Vprior
This protocol provides a comprehensive framework for integrating human expertise with quantitative assessments in model validation. By combining rigorous statistical methodologies with structured expert evaluation, researchers can develop increasingly trustworthy predictive models for high-stakes applications in drug development and clinical decision support. The case study in precision radiotherapy demonstrates how this approach enables safe, effective integration of AI recommendations with human expertise, ultimately enhancing patient care through complementary strengths of computational and human intelligence.
In the rigorous fields of scientific research and drug development, the adoption of new computational models must be predicated on robust, evidence-based validation. Model validation is fundamentally the process of determining the degree to which a model is an accurate representation of the real world from the perspective of its intended uses [8]. As industries and governments, including pharmaceutical regulators, depend increasingly on predictions from computer models to justify critical decisions, a systematic approach to validation is paramount [8]. This document frames this validation process within the context of hypothesis testing, providing researchers with detailed application notes and protocols to compare model performance against established benchmarks objectively. The core premise is to replace static claims of model adequacy with a dynamic, iterative process of constructive approximation, building trust through accumulated, scrutinized evidence [8].
Theoretical Foundation: Hypothesis Testing for Model Validation
At its heart, model validation is an exercise in statistical hypothesis testing. This approach provides a formal framework for making statistical decisions using experimental data, allowing scientists to validate or refute an assumption about a model's performance [139].
The Core Analogy and Framework
In a model validation scenario, the process mirrors a courtroom trial [139]:
- The Null Hypothesis (H₀) is the default assumption that the model has no meaningful effect or its performance is no better than an established baseline or benchmark.
- The Alternative Hypothesis (H₁) is the claim that the model does have a significant effect or its performance exceeds the benchmark.
- The data from benchmark tests serve as the evidence.
- The p-value quantifies the strength of this evidence against the null hypothesis.
A small p-value (typically < 0.05) indicates that the observed benchmark results are unlikely under the assumption that H₀ is true, leading to its rejection in favor of H₁ [139].
Validation as an Iterative Constructive Process
True validation is not a single event but an iterative construction process that mimics the scientific method [8]. This process involves:
- Starting from observations and existing benchmarks.
- Building a model based on hypotheses, intuition, and analogies.
- Testing the model against available data and benchmarks.
- Refining or rejecting the model based on the outcomes, and repeating the process.
This iterative loop progressively builds trust in a model through the accumulated confirmation of its predictions across a diverse set of experimental tests [8]. The following diagram illustrates this cyclical workflow for computational models in research.
Establishing the Benchmarking Landscape
A critical first step in a comparative analysis is selecting appropriate and relevant benchmarks. These benchmarks should be designed to stress-test the model's capabilities in areas critical to its intended application, such as reasoning, specialized knowledge, or technical performance.
Contemporary Model Performance Benchmarks
The table below summarizes the performance of leading AI models across a selection of challenging, non-saturated benchmarks as of late 2025, providing a snapshot of the current landscape [140].
Table 1: Performance of Leading Models on Key Benchmarks (Post-April 2024 Releases)
| Benchmark Name (and Focus Area) | Top-Performing Models (Score) |
|---|---|
| GPQA Diamond (Reasoning) | Gemini 3 Pro (91.9%), GPT 5.1 (88.1%), Grok 4 (87.5%) [140] |
| AIME 2025 (High School Math) | Gemini 3 Pro (100%), Kimi K2 Thinking (99.1%), GPT oss 20b (98.7%) [140] |
| SWE Bench (Agentic Coding) | Claude Sonnet 4.5 (82%), Claude Opus 4.5 (80.9%), GPT 5.1 (76.3%) [140] |
| Humanity's Last Exam (Overall) | Gemini 3 Pro (45.8), Kimi K2 Thinking (44.9), GPT-5 (35.2) [140] |
| ARC-AGI 2 (Visual Reasoning) | Claude Opus 4.5 (37.8), Gemini 3 Pro (31), GPT 5.1 (18) [140] |
| MMMLU (Multilingual Reasoning) | Gemini 3 Pro (91.8%), Claude Opus 4.5 (90.8%), Claude Opus 4.1 (89.5%) [140] |
Performance and Cost Trade-offs
In addition to raw performance, practical deployment requires considering computational efficiency. The following table contrasts high-performance models with those optimized for speed and cost, supporting a balanced decision-making process [140].
Table 2: Model Performance and Efficiency Trade-offs
| Category | Model Examples | Key Metric |
|---|---|---|
| High-Performance Leaders | Claude Opus 4.5, Gemini 3 Pro, GPT-5 | Top scores on complex benchmarks like GPQA and AIME [140] |
| Fastest Inference | Llama 4 Scout (2600 tokens/sec), Llama 3.3 70b (2500 tokens/sec) | High token throughput per second [140] |
| Lowest Latency | Nova Micro (0.3s), Llama 3.1 8b (0.32s), Llama 4 Scout (0.33s) | Seconds to First Token (TTFT) [140] |
| Most Affordable | Nova Micro ($0.04/$0.14), Gemma 3 27b ($0.07/$0.07), Gemini 1.5 Flash ($0.075/$0.3) | Cost per 1M Input/Output Tokens (USD) [140] |
Experimental Protocols for Benchmarking
A standardized protocol is essential for ensuring that comparative analyses are reproducible, fair, and meaningful.
Core Experimental Workflow
The detailed methodology for conducting a benchmark comparison experiment can be broken down into the following stages, from preparation to statistical interpretation.
Protocol Details for Key Stages
Stage 1: Preparation and Hypothesis Formulation
- Define the Intended Use: Clearly articulate the specific task or problem the model is expected to solve. This determines which benchmarks are relevant [8].
- Select Benchmark Suite: Choose a set of benchmarks that collectively probe the capabilities critical for the intended use (e.g., MMLU for general knowledge, SWE-Bench for coding). Prioritize benchmarks that are not yet saturated to ensure discriminative power [140].
- Formulate Hypotheses: For each benchmark, define a precise null and alternative hypothesis.
- H₀: The performance of the new model (μnew) is less than or equal to the benchmark model (μbenchmark). Mathematically: H₀: μnew ≤ μbenchmark.
- H₁ (One-Tailed): The performance of the new model is greater than the benchmark model. H₁: μnew > μbenchmark [139].
- Set Significance Level: Predefine the alpha (α) level, typically 0.05, which defines the risk of a Type I error (falsely rejecting a true H₀) you are willing to accept [139].
Stage 2: Experimental Setup
- Standardize Inputs: Ensure that the prompt, context, and input data fed to all models are identical for a given benchmark task.
- Configure Model Parameters: Use default or standard parameter settings for each model, documenting any deviations. For non-deterministic models, set a fixed random seed to ensure reproducibility.
- Control Environment: Run experiments in a consistent computational environment, noting hardware specifications (e.g., GPU type) and software libraries.
Stage 3: Execution and Data Collection
- Run Benchmarks: Execute the benchmark tests on both the new model and the established baseline model(s).
- Record Raw Outputs: Save the complete, unprocessed outputs from each model run for subsequent analysis.
- Monitor for Failures: Log any runtime errors or invalid outputs that may occur.
Stage 4: Data Analysis and Statistical Testing
- Calculate Metrics: Score the model outputs according to the official metric of each benchmark (e.g., accuracy, pass rate).
- Perform Statistical Test: Use an appropriate statistical test to compare the results. For example, a paired t-test is often suitable for comparing the performance of two models across multiple benchmark tasks or datasets.
- Determine P-Value: Calculate the p-value associated with the test statistic. A p-value less than the predefined α (e.g., 0.05) provides statistical evidence to reject the null hypothesis [139].
Stage 5: Interpretation and Reporting
- Make a Decision: Based on the p-value, decide to either reject or fail to reject the null hypothesis.
- Report Effect Size: Do not rely solely on p-values. Report the effect size (e.g., Cohen's d) to indicate the magnitude of the performance difference, which is crucial for practical significance [141].
- Document Everything: Report the hypotheses, test used, alpha level, p-value, effect size, and any experimental limitations.
The Scientist's Toolkit: Research Reagent Solutions
This section details essential "research reagents" – the key software tools and platforms – required for conducting a rigorous model validation study.
Table 3: Essential Reagents for Model Benchmarking and Validation
| Research Reagent | Function / Explanation |
|---|---|
| Specialized Benchmark Suites (e.g., SWE-Bench, GPQA, AIME) | These are standardized test sets designed to evaluate specific model capabilities like coding, reasoning, or mathematical problem-solving. They serve as the ground truth for performance comparison [140] [142]. |
| Statistical Testing Libraries (e.g., scipy.stats in Python) | These software libraries provide pre-built functions for conducting hypothesis tests (e.g., t-tests, Z-tests, Chi-square tests) and calculating p-values and effect sizes, which are essential for objective comparison [139]. |
| Public Benchmarking Platforms (e.g., Vellum AI Leaderboard, Epoch AI) | These platforms aggregate performance data from various models on numerous benchmarks, providing an up-to-date view of the state-of-the-art and a source of baseline data for comparison [140] [142]. |
| Containerization Tools (e.g., Docker) | Tools like Docker ensure reproducibility by packaging the model, its dependencies, and the benchmarking environment into a single, portable unit that can be run consistently anywhere [142]. |
| Data Analysis & Visualization Software (e.g., MAXQDA, R, Python/pandas) | These tools are used for compiling results, creating summary tables for cross-case analysis, and generating visualizations that help in interpreting complex benchmark outcomes [143]. |
Case Study: Protocol Application in a Simulated Drug Discovery Scenario
Scenario: A research team has fine-tuned a large language model (LLM), "DrugExplorer v2.0," to improve its ability to extract chemical compound-protein interaction data from scientific literature. They want to validate its performance against the established baseline of "GPT-4.1."
1. Hypothesis Formulation:
- H₀: The F1-score of DrugExplorer v2.0 in extracting compound-protein interactions is less than or equal to that of GPT-4.1. (H₀: μDE2 ≤ μGPT4.1)
- H₁: The F1-score of DrugExplorer v2.0 is greater than that of GPT-4.1. (H₁: μDE2 > μGPT4.1)
- α: 0.05
2. Benchmark & Setup:
- Benchmark: A curated dataset of 500 scientific abstracts with gold-standard annotations for compound-protein interactions.
- Models: DrugExplorer v2.0 (Test) vs. GPT-4.1 (Baseline).
- Metric: F1-Score (harmonic mean of precision and recall).
- Statistical Test: One-tailed, paired t-test (the "pairs" are the scores on each of the 500 abstracts).
3. Execution & Analysis:
- The team runs both models on the 500 abstracts and calculates the F1-score for each.
- They find:
- Mean F1-score for DrugExplorer v2.0 = 0.89
- Mean F1-score for GPT-4.1 = 0.85
- A paired t-test returns a p-value of 0.01.
4. Interpretation:
- Since the p-value (0.01) is less than α (0.05), the null hypothesis (H₀) is rejected.
- Conclusion: There is statistically significant evidence at the 0.05 level to conclude that DrugExplorer v2.0 has a higher F1-score than GPT-4.1 on the task of extracting compound-protein interactions from the benchmark dataset. This result represents a successful iteration in the validation process for DrugExplorer v2.0, though validation must continue with other benchmarks and real-world data [8].
Conclusion
Hypothesis testing provides an indispensable, rigorous framework for model validation, transforming subjective trust into quantifiable evidence. By mastering foundational principles, selecting appropriate methodological tests, vigilantly avoiding common pitfalls, and employing advanced comparative techniques, researchers can build robust, reliable models. The future of biomedical model validation lies in hybrid approaches that combine the objectivity of frequentist statistics with the nuanced uncertainty quantification of Bayesian methods, all while fostering human-AI collaboration. This rigorous validation is paramount for translating computational models into trustworthy tools that can inform critical decisions in drug development and clinical practice, ultimately accelerating the pace of biomedical discovery and improving patient outcomes.
References
- 1. Hypothesis Testing | A Step-by-Step Guide with Easy ... [https://www.scribbr.com/statistics/hypothesis-testing/]
- 2. Null and Alternative Hypotheses | Definitions & Examples [https://www.scribbr.com/statistics/null-and-alternative-hypotheses/]
- 3. Null vs. Alternative Hypothesis [Overview] - Outlier Articles [https://articles.outlier.org/null-vs-alternative-hypothesis]
- 4. What Is The Null Hypothesis & When To Reject It [https://www.simplypsychology.org/null-hypothesis-examples-how-to-state-when-to-reject.html]
- 5. Null hypothesis and Alternative Hypothesis [https://www.statisticssolutions.com/null-hypothesis-and-alternative-hypothesis/]
- 6. Quantitative data collection and analysis: Testing hypotheses [https://libguides.tees.ac.uk/quantitative/testing]
- 7. How to Use Hypothesis Testing Language in AP Statistics ... [https://www.revisiondojo.com/blog/how-to-use-hypothesis-testing-language-in-ap-statistics-2025-guide]
- 8. Algorithm for model validation: Theory and applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC1871825/]
- 9. Understanding P-Values and Statistical Significance [https://www.simplypsychology.org/p-value.html]
- 10. The Power of Hypothesis Testing: Validating Your Data ... [https://www.cloudthat.com/resources/blog/the-power-of-hypothesis-testing-validating-your-data-analysis-results]
- 11. P Values (Calculated Probability) and Hypothesis Testing [https://www.statsdirect.com/help/basics/p_values.htm]
- 12. Interpretation of Alpha and p-Value [https://www.spcforexcel.com/knowledge/basic-statistics/interpretation-alpha-and-p-value/]
- 13. Hypothesis Testing in Data Science: Validating Decisions ... [https://www.dasca.org/world-of-data-science/article/hypothesis-testing-in-data-science-validating-decisions-with-data]
- 14. : Your Practical Path to Better, Faster... Experimentation Protocols [https://www.geteppo.com/blog/experimentation-protocols-practical-testing-guide]
- 15. and false Negatives - GeeksforGeeks Positives false [https://www.geeksforgeeks.org/machine-learning/false-positives-and-false-negatives/]
- 16. Type I and type II errors [https://en.wikipedia.org/wiki/Type_I_and_type_II_errors]
- 17. & Type II Errors | Differences, I , Visualizations Type Examples [https://www.scribbr.com/statistics/type-i-and-type-ii-errors/]
- 18. Model validation using equivalence tests [https://www.sciencedirect.com/science/article/abs/pii/S0304380004000985]
- 19. Difference between Parametric and Non-Parametric Methods [https://www.geeksforgeeks.org/machine-learning/difference-between-parametric-and-non-parametric-methods/]
- 20. Parametric and Non-Parametric Statistics: 6 Important ... [https://www.careershodh.com/parametric-and-non-parametric-statistics/]
- 21. Parametric versus non-parametric statistics in the analysis of ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-5-35]
- 22. Parametric and Nonparametric Tests in Spine Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC6125939/]
- 23. Nonparametric statistical tests for the continuous data [https://pmc.ncbi.nlm.nih.gov/articles/PMC4754273/]
- 24. When to Use Parametric versus Nonparametric Procedures ... [https://ogs.edu/when-to-use-parametric-versus-nonparametric-procedures-in-statistics-for-social-research/]
- 25. FAQ: What are the differences between one-tailed and two ... [https://stats.oarc.ucla.edu/other/mult-pkg/faq/general/faq-what-are-the-differences-between-one-tailed-and-two-tailed-tests/]
- 26. Research Hypothesis In Psychology: Types, & Examples [https://www.simplypsychology.org/what-is-a-hypotheses.html]
- 27. One-tailed vs. two-tailed hypothesis: Key differences & ... [https://www.statsig.com/perspectives/one-tailed-vs-two-tailed-hypothesis]
- 28. directional-hypothesis.pdf [https://methods.sagepub.com/ency/edvol/download/encyc-of-research-design/chpt/directional-hypothesis.pdf]
- 29. One-tail vs. two-tail P values [https://www.graphpad.com/guides/prism/latest/statistics/one-tail_vs__two-tail_p_values.htm]
- 30. P values. One-tail or two-tail ? - FAQ 1318 [https://www.graphpad.com/support/faq/p-values-one-tail-or-two-tail-/]
- 31. Hypotheses; directional and non-directional [https://psychologyrocks.org/hypotheses-directional-and-non-directional/]
- 32. One-Tail vs. Two-Tail - Statistics Resources [https://resources.nu.edu/statsresources/onevstwotailtest]
- 33. Hypothesis Testing, P Values, Confidence Intervals ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK557421/]
- 34. Hypothesis Testing The Ultimate Guide to Smarter ... [https://www.tatvic.com/blog/hypothesis-testing-the-ultimate-guide/]
- 35. Statistical hypothesis test [https://en.wikipedia.org/wiki/Statistical_hypothesis_test]
- 36. 14 Comparing quantitative data between individuals [https://bookdown.org/pkaldunn/SRM-Textbook/BetweenQuantData.html]
- 37. Using Decision Trees to Optimize Pharmaceutical ... [https://lumivero.com/resources/case-studies/using-decision-trees-to-optimize-pharmaceutical-indication-sequencing-decisions-with-precisiontree/]
- 38. A binary decision tree approach for pharmaceutical project ... [https://www.sciencedirect.com/science/article/pii/S2772662223000681]
- 39. Evaluating the Accuracy and Explanatory Quality of Large ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627256/]
- 40. Statistical Tests in Machine Learning Modeling | by Ilma Khan [https://medium.com/data-science-collective/statistical-tests-in-machine-learning-modeling-2629e72bc7f4]
- 41. Decision Tree-Based Data Stratification Method for the ... [https://www.mdpi.com/2076-3417/11/23/11380]
- 42. How to compare 2 ml models with Paired_tttest5x2 [https://medium.com/@bobrupakroy/how-to-compare-2-ml-models-with-paired-tttest5x2-eceffb6b55e6]
- 43. Statistical Significance Tests for Comparing Machine ... [https://www.machinelearningmastery.com/statistical-significance-tests-for-comparing-machine-learning-algorithms/]
- 44. paired_ttest_5x2cv: 5x2cv paired t test for classifier comparisons [https://rasbt.github.io/mlxtend/user_guide/evaluate/paired_ttest_5x2cv/]
- 45. Hypothesis Test for Comparing Machine Learning Algorithms [https://www.machinelearningmastery.com/hypothesis-test-for-comparing-machine-learning-algorithms/]
- 46. Dietterich's 5x2cv paired t-test for regression problems [https://stats.stackexchange.com/questions/430437/dietterichs-5x2cv-paired-t-test-for-regression-problems]
- 47. Analysis of continuous data using the t-test and ANOVA [https://eurointervention.pcronline.com/article/tools-and-techniques-statistics-analysis-of-continuous-data-using-the-t-test-and-anova]
- 48. The t-Test | Introduction to Statistics [https://www.jmp.com/en/statistics-knowledge-portal/t-test]
- 49. Understanding t-tests, ANOVA, and MANOVA - UVA Library [http://library.virginia.edu/data/articles/understanding-t-tests-anova-and-manova]
- 50. Chi-Squared Test for Pharmaceutical Industry [https://www.linkedin.com/pulse/chi-squared-test-pharmaceutical-industry-dr-oualid-soula-pehpc]
- 51. Practical guide to calculate sample size for chi-square test in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12107878/]
- 52. 9.1: Chi-square test and goodness of fit [https://stats.libretexts.org/Bookshelves/Applied_Statistics/Mikes_Biostatistics_Book_(Dohm)/09%3A_Categorical_Data/9.1%3A_Chi-square_test_and_goodness_of_fit]
- 53. 8.3 Carrying Out a Chi Square Goodness of Fit Test [https://fiveable.me/ap-stats/unit-8/carrying-out-chi-square-goodness-fit-test/study-guide/XmvvVf9spR7e6xT6TPEG]
- 54. Practical guide to calculate sample size for chi-square test in ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02584-4]
- 55. A/B testing [https://en.wikipedia.org/wiki/A/B_testing]
- 56. A/B design testing of a clinical trial recruitment website [https://pmc.ncbi.nlm.nih.gov/articles/PMC8995844/]
- 57. Applying A/B Testing to Clinical Decision Support [https://www.jmir.org/2021/4/e16651/]
- 58. Experimentation Techniques - A/B Testing - First Principles [https://www.firstprinciples.ventures/insights/experimentation-techniques-ab-testing-latest]
- 59. Clinical validation of an AI-based blood testing device for ... [https://www.nature.com/articles/s41591-025-03933-y]
- 60. Integrated bioinformatics and experiment validation reveal ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-10822-9]
- 61. Identification and verification of a novel signature that ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11089679/]
- 62. Diagnostic framework to validate clinical machine learning ... [https://www.nature.com/articles/s43856-025-00965-w]
- 63. Predictions With a Purpose: Elevating Standards for Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12119043/]
- 64. Six Sigma Hypothesis Testing: Results with P-Value & Data [https://www.sixsigma-institute.org/Six_Sigma_DMAIC_Process_Analyze_Phase_Hypothesis_Testing.php]
- 65. Hex Color Validator [https://rapidtoolset.com/en/tool/hex-color-validator]
- 66. Data Validation Libraries for Polars (2025 Edition) – Pointblank [https://posit-dev.github.io/pointblank/blog/validation-libs-2025/]
- 67. The data validation landscape in 2025 [https://aeturrell.com/blog/posts/the-data-validation-landscape-in-2025/]
- 68. Python Email Validation: Tutorial with Code Snippets [2025] [https://mailtrap.io/blog/python-validate-email/]
- 69. How to Validate Your Data With Statistical Tests in Python [https://www.howtogeek.com/how-to-validate-your-data-with-statistical-tests-in-python/]
- 70. Hypothesis Testing Using Simulation in R and Python [https://alabhya.medium.com/hypothesis-testing-using-simulation-in-r-and-python-61b08f299f49]
- 71. Introduction to Statistical Hypothesis Testing in R [https://data-flair.training/blogs/hypothesis-testing-in-r/]
- 72. Data dredging [https://en.wikipedia.org/wiki/Data_dredging]
- 73. Hypothesis testing, model selection, model comparison [https://discourse.mc-stan.org/t/hypothesis-testing-model-selection-model-comparison-some-thoughts/19163]
- 74. Why I like preregistration (and it's not about p-hacking). ... [https://statmodeling.stat.columbia.edu/2025/01/16/why-i-like-preregistration-and-its-not-about-p-hacking-when-done-right-it-unifies-the-substance-of-science-with-the-scientific-method/]
- 75. TOP Guidelines [https://www.cos.io/initiatives/top-guidelines]
- 76. Improving transparency in clinical trial reporting - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037211/]
- 77. Multiple comparisons problem [https://en.wikipedia.org/wiki/Multiple_comparisons_problem]
- 78. A general introduction to adjustment for multiple comparisons [https://pmc.ncbi.nlm.nih.gov/articles/PMC5506159/]
- 79. Correct me if I'm wrong: Navigating multiple comparison ... [https://www.statsig.com/blog/multiple-comparison-corrections-in-a-b]
- 80. - Wikipedia false discovery rate [https://en.wikipedia.org/wiki/False_discovery_rate]
- 81. False Discovery Rate [https://www.publichealth.columbia.edu/research/population-health-methods/false-discovery-rate]
- 82. Correction For Multiple Comparisons [https://www.statsig.com/glossary/correction-for-multiple-comparisons]
- 83. A practical guide to methods in... controlling false discoveries [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1716-1]
- 84. Beware of counter-intuitive levels of false discoveries in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359981/]
- 85. for confounder selection using mirror... false discovery rate control [https://arxiv.org/html/2402.18904v3/]
- 86. Sample size determination: A practical guide for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000262/]
- 87. Group and sample size | NC3Rs EDA [https://eda.nc3rs.org.uk/experimental-design-group]
- 88. Sample size, power and effect size revisited: simplified and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7745163/]
- 89. 8 Tips Before Calculating Sample Size in Medical Device ... [https://www.greenlight.guru/blog/8-tips-before-calculating-sample-size-medical-device-studies]
- 90. Sample size calculation in medical studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4017493/]
- 91. G*Power [https://www.gpower.hhu.de/]
- 92. Sample Size Software | Power Analysis Software | PASS [https://www.ncss.com/software/pass/]
- 93. Comprehensive guidelines for appropriate statistical analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11467495/]
- 94. Assumptions for Statistical Tests [https://real-statistics.com/descriptive-statistics/assumptions-statistical-test/]
- 95. Assumptions of Multiple Linear Regression Analysis [https://www.statisticssolutions.com/free-resources/directory-of-statistical-analyses/assumptions-of-linear-regression/]
- 96. Regression with SAS Chapter 2 – Regression Diagnostics [https://stats.oarc.ucla.edu/sas/webbooks/reg/chapter2/regressionwith-saschapter-2-regression-diagnostics/]
- 97. Statistical Guidelines | BDJ Open [https://www.nature.com/bdjopen/authors-and-referees/statistical-guidelines]
- 98. Ethical Guidelines for Statistical Practice [https://www.amstat.org/your-career/ethical-guidelines-for-statistical-practice]
- 99. Power and sample size [https://pubmed.ncbi.nlm.nih.gov/18450060/]
- 100. Detrimental Effects of Underpowered or Overpowered ... [https://web.ma.utexas.edu/users/mks/statmistakes/UnderOverPower.html]
- 101. Casting New Light on Statistical Power - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9989344/]
- 102. The Journal Psychological Methods Decides that ... [https://replicationindex.com/2025/10/20/the-journal-psychological-methods-decides-that-psychological-research-is-not-underpowered/]
- 103. Seven ways to improve statistical power in your experiment ... [https://blogs.worldbank.org/en/impactevaluations/seven-ways-improve-statistical-power-your-experiment-without-increasing-n]
- 104. 10 Best Practices for Data Collection in 2025 [https://add-to-calendar-pro.com/articles/best-practices-for-data-collection]
- 105. 10 Interesting Data Collection Techniques & Methods For ... [https://airbyte.com/data-engineering-resources/data-collection-techniques]
- 106. Mind the Gaps: Literature Survey Reveals Shortcomings in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595928/]
- 107. Missing Data Strategies for Robust Data Analysis: [https://medium.com/@abhaysingh71711/missing-data-strategies-for-robust-data-analysis-ebda7ea9bbd4]
- 108. Handling Missing Values in Machine Learning [https://www.geeksforgeeks.org/machine-learning/handling-missing-values-machine-learning/]
- 109. Using Iterative Pairwise External Validation to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9114056/]
- 110. Multi-Agent Hypothesis-Validation Overview [https://www.emergentmind.com/topics/multi-agent-hypothesis-validation]
- 111. The Iterative-Hypothesis customer development method [https://longform.asmartbear.com/customer-development/]
- 112. Iterative Hypothesis Generation for Scientific Discovery ... [https://arxiv.org/html/2503.19309v1]
- 113. Exploring the role of large language models in the scientific ... [https://www.nature.com/articles/s44387-025-00019-5]
- 114. V-Model vs Iterative Model: Systematic Verification vs ... [https://teachingagile.com/sdlc/comparisons/v-model-vs-iterative]
- 115. Traditional Drug Development Process - The Actuary Magazine [https://www.theactuarymagazine.org/traditional-drug-development-process/]
- 116. A Review of Bayesian Hypothesis Testing and Its Practical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8871131/]
- 117. The untapped potential of Bayesian region of practical ... [https://www.sciencedirect.com/science/article/pii/S0360132325008662]
- 118. Region of Practical Equivalence (ROPE) - easystats [https://easystats.github.io/bayestestR/articles/region_of_practical_equivalence.html]
- 119. ROPE and Equivalence Testing: Practically Equivalent? [https://www.r-bloggers.com/2017/02/rope-and-equivalence-testing-practically-equivalent/]
- 120. A Bayesian modelling framework with model comparison ... [https://pubmed.ncbi.nlm.nih.gov/40822275/]
- 121. A Bayesian modelling framework with model comparison ... [https://www.sciencedirect.com/science/article/pii/S2468042725000764]
- 122. Enhancing drug screening and pharmacokinetic predictions [https://www.sciencedirect.com/science/article/abs/pii/S1385894725012288]
- 123. Bayesian risk-based decision method for model validation ... [https://www.sciencedirect.com/science/article/abs/pii/S0951832006000718]
- 124. AI Model Validation: Best Practices for Accuracy & Reliability [https://galileo.ai/blog/best-practices-for-ai-model-validation-in-machine-learning]
- 125. Using Leave-one-out cross-validation for large data • loo - Stan [https://mc-stan.org/loo/articles/loo2-large-data.html]
- 126. Using Leave-one-out cross-validation for large data [https://cran.r-project.org/web/packages/loo/vignettes/loo2-large-data.html]
- 127. Top 5 Validation Methods In Machine Learning [https://medium.com/@mehmetalitor/top-5-model-validation-methods-in-machine-learning-77eed8d08937]
- 128. Cross-Validation in Machine Learning: How to Do It Right [https://neptune.ai/blog/cross-validation-in-machine-learning-how-to-do-it-right]
- 129. Stacking to Improve Model Performance: A Comprehensive ... [https://medium.com/@brijesh_soni/stacking-to-improve-model-performance-a-comprehensive-guide-on-ensemble-learning-in-python-9ed53c93ce28]
- 130. Stacking Models in Data Science: A Comprehensive Guide ... [https://www.institutedata.com/us/blog/stacking-models-in-data-science-a-comprehensive-guide-to-enhanced-predictions/]
- 131. The Systematic Multiverse Analysis Registration Tool for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567067/]
- 132. Create multiverse analysis in R - MU Collective [https://mucollective.github.io/multiverse/]
- 133. Chapter 15 Stacked Models | Hands-On Machine Learning ... [https://bradleyboehmke.github.io/HOML/stacking.html]
- 134. A Comparative Analysis of Multitask Neural Networks and ... [https://www.mdpi.com/2673-4591/114/1/19]
- 135. Precision radiotherapy via information integration of expert ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11058561/]
- 136. How to write a lab protocol [https://www.scinote.net/blog/how-to-structure-a-protocol/]
- 137. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 138. Elements must meet minimum color contrast ratio thresholds [https://dequeuniversity.com/rules/axe/4.8/color-contrast]
- 139. Hypothesis Testing for Data Scientists: A Deep Dive into ... [https://medium.com/@rahultiwari065/hypothesis-testing-for-data-scientists-a-deep-dive-into-statistical-decision-making-8b2868b161e2]
- 140. LLM Leaderboard 2025 [https://www.vellum.ai/llm-leaderboard]
- 141. Sample tables - APA Style - American Psychological Association [https://apastyle.apa.org/style-grammar-guidelines/tables-figures/sample-tables]
- 142. Data on AI Benchmarking [https://epoch.ai/benchmarks]
- 143. Summary Tables (Compile and Present Summaries) [https://www.maxqda.com/help/summarizing/summary-tables]