Internal vs External Validation in Drug Development: A Scientific Framework for Predictive Model Assessment
This article provides researchers, scientists, and drug development professionals with a comprehensive examination of validation methodologies for clinical prediction models and AI tools.
Internal vs External Validation in Drug Development: A Scientific Framework for Predictive Model Assessment
Abstract
This article provides researchers, scientists, and drug development professionals with a comprehensive examination of validation methodologies for clinical prediction models and AI tools. It explores the foundational distinctions between internal and external validation, presents rigorous methodological approaches for implementation, addresses common challenges in model optimization, and offers comparative analysis of validation strategies. Through case studies and empirical evidence, the content establishes a scientific framework for ensuring model reliability, generalizability, and regulatory acceptance throughout the therapeutic development pipeline.
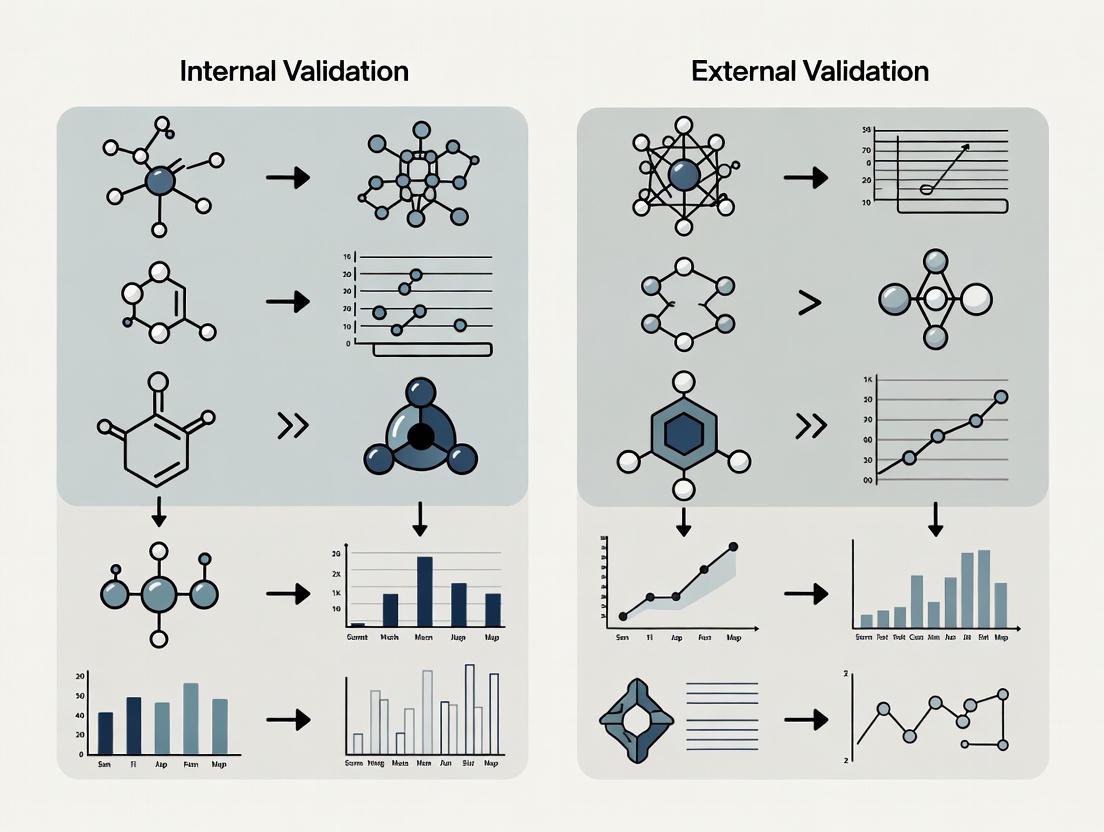
Core Principles: Defining Validation Paradigms in Biomedical Research
In the scientific development of predictive models, particularly in clinical and biomedical research, validation is a critical process that assesses the reliability and generalizability of a model's predictions. The scientific paradigm strictly differentiates between internal validation, which evaluates a model's performance on data from the same source as its development sample, and external validation, which tests the model on entirely independent data collected from different populations or settings [1] [2]. This distinction forms the cornerstone of rigorous predictive modeling, as a model must demonstrate both internal consistency and external transportability to be considered scientifically useful.
The fundamental trade-off between these validation types hinges on optimism bias (the tendency for models to perform better on the data they were trained on) and generalizability (the ability to maintain performance across diverse settings) [1]. This technical guide delineates the core definitions, methodologies, and applications of internal and external validation within the context of predictive model research for scientific professionals.
Core Definitions and Conceptual Framework
Internal Validation
Internal validation refers to a set of statistical procedures used to estimate the optimism or overfit of a predictive model when applied to new samples drawn from the same underlying population as the original development dataset [1]. Its primary purpose is to provide a realistic performance assessment that corrects for the over-optimism inherent in "apparent performance" (performance measured on the very same data used for model development) [1]. Internal validation is considered a mandatory minimum requirement for any proposed prediction model, as many failed external validations could be foreseen through rigorous internal validation procedures [1].
External Validation
External validation assesses the transportability of a model's predictive performance to data that were not used in any part of the model development process, typically originating from different locations, time periods, or populations [1] [2]. This process evaluates whether the model maintains its discriminative ability and calibration when applied to new settings, thus testing its generalizability beyond the original development context [3] [2]. External validation represents the strongest evidence for a model's potential clinical utility and real-world applicability across diverse settings.
Key Conceptual Differences
The table below summarizes the fundamental distinctions between internal and external validation approaches:
Table 1: Fundamental Characteristics of Internal versus External Validation
| Aspect | Internal Validation | External Validation |
|---|---|---|
| Data Source | Same population as development data [1] | Truly independent data from different populations, centers, or time periods [1] [2] |
| Primary Objective | Correct for overfitting/optimism bias [1] | Assess generalizability/transportability [1] [2] |
| Timing | During model development [1] | After model development, using data unavailable during development [1] |
| Performance Expectation | Expected to be slightly lower than apparent performance | Ideally similar to internally validated performance; often worse in practice [1] |
| Interpretation | Tests reproducibility within the same data context [1] | Tests generalizability to new contexts [1] |
Internal Validation Methods and Protocols
Internal validation employs resampling techniques to simulate the application of a model to new samples from the same population. These methods vary in their stability, computational intensity, and suitability for different sample sizes.
Technical Methodologies
Bootstrap Validation
Bootstrap validation involves repeatedly drawing samples with replacement from the original dataset (typically of the same size as the original dataset) [1]. The model is developed on each bootstrap sample and then tested on both the bootstrap sample and the original dataset. The average optimism (difference in performance) across iterations is subtracted from the model's apparent performance to obtain an optimism-corrected estimate [1]. Conventional bootstrap may be over-optimistic, while the 0.632+ bootstrap method can be overly pessimistic, particularly with small sample sizes [4].
K-Fold Cross-Validation
In k-fold cross-validation, the dataset is randomly partitioned into k equally sized folds. The model is trained on k-1 folds and validated on the remaining fold. This process is repeated k times, with each fold used exactly once as the validation data [4]. The average performance across all k folds provides the internal validation estimate. Studies have shown that k-fold cross-validation demonstrates greater stability compared to other methods, particularly with larger sample sizes [4].
Nested Cross-Validation
Nested cross-validation (also known as double cross-validation) features an inner loop for model selection/tuning and an outer loop for performance estimation [4]. This approach is particularly important when model development involves hyperparameter optimization (e.g., in penalized regression or machine learning). The outer loop provides a nearly unbiased performance estimate, while the inner loop selects optimal parameters for each training set [4]. Performance can fluctuate depending on the regularization method used for model development [4].
Comparative Performance in Simulation Studies
Simulation studies provide quantitative evidence for selecting appropriate internal validation methods based on sample size and data characteristics:
Table 2: Internal Validation Method Performance Based on Simulation Studies [4]
| Method | Recommended Sample Size | Stability | Optimism Correction | Key Considerations |
|---|---|---|---|---|
| Train-Test Split | Very large only (n > 1000) [1] | Unstable, especially with small holdout sets [4] | Moderate | "Only works when not needed" - inefficient in small samples [1] |
| Conventional Bootstrap | Medium to Large (n > 500) | Moderate | Can be over-optimistic [4] | Requires 100+ iterations [4] |
| 0.632+ Bootstrap | Medium to Large (n > 500) | Moderate | Overly pessimistic with small samples (n=50-100) [4] | Complex weighting scheme |
| K-Fold Cross-Validation | Small to Large (n=75+) [4] | High stability [4] | Appropriate | Preferred for Cox penalized models in high-dimensional settings [4] |
| Nested Cross-Validation | Small to Large (n=75+) [4] | Moderate, with fluctuations [4] | Appropriate | Essential when model selection is part of fitting [4] |
Implementation Workflow
The following diagram illustrates the workflow for k-fold cross-validation, one of the recommended internal validation methods:
External Validation Methods and Protocols
Validation Typology
External validation encompasses several distinct approaches based on the relationship between development and validation datasets:
- Full External Validation: Conducted by different investigators using completely independent data collected after model development [1] [2]. This represents the strongest form of validation.
- Temporal Validation: The model is validated on data from the same institution(s) but collected from a later time period than the development data [1].
- Geographic Validation: Validation performed on data from different centers or geographic locations than where the model was developed [2].
- Internal-External Cross-Validation: A hybrid approach where data are repeatedly split by natural groupings (e.g., centers in a multicenter study), with each group left out once for validation of a model developed on the remaining groups [1].
Performance Assessment Metrics
External validation requires comprehensive assessment of both discrimination and calibration:
Table 3: Key Metrics for External Validation Performance Assessment
| Metric Category | Specific Measures | Interpretation | Application Example |
|---|---|---|---|
| Discrimination | Area Under ROC Curve (AUC/AUROC) [3] | Ability to distinguish between outcome classes | CSM-4 sepsis model: AUROC=0.80 at 4h [3] |
| Discrimination | Concordance Index (C-index) [2] | Overall ranking accuracy of predictions | AI lung cancer model: Superior to TNM staging [2] |
| Calibration | Brier Score [4] | Overall accuracy of probability estimates | Integrated Brier score for time-to-event data [4] |
| Calibration | Calibration Plots/Slope | Agreement between predicted and observed risks | Slope <1 indicates overfitting [1] |
| Clinical Utility | Hazard Ratios [2] | Risk stratification performance | AI model: HR=3.34 vs 1.98 for TNM in stage I [2] |
Implementation Workflow
The external validation process follows a systematic approach to ensure comprehensive assessment:
Case Studies in Biomedical Research
Internal Validation: High-Dimensional Prognosis Models
A simulation study focusing on transcriptomic data in head and neck tumors (n=76 patients) compared internal validation strategies for Cox penalized regression models with time-to-event endpoints [4]. The study simulated datasets with clinical variables and 15,000 transcripts at sample sizes of 50, 75, 100, 500, and 1000 patients, with 100 replicates each [4]. Key findings included:
- Train-test validation showed unstable performance across sample sizes
- Conventional bootstrap was over-optimistic in its performance estimates
- 0.632+ bootstrap was overly pessimistic, particularly with small samples (n=50 to n=100)
- K-fold cross-validation and nested cross-validation improved performance with larger sample sizes, with k-fold demonstrating greater stability [4]
The study concluded that k-fold cross-validation and nested cross-validation are recommended for internal validation of Cox penalized models in high-dimensional time-to-event settings [4].
External Validation: Sepsis Mortality Prediction Models
A 2025 external validation study assessed eight different mortality prediction models in intensive care units for 750 patients with sepsis [3]. The study clarified which variables from each model were routinely collected in medical care and externally validated the models by calculating AUROC for predicting 30-day mortality. Key results demonstrated:
- The CSM-4 model performed best 4 hours after ICU admission (AUROC=0.80) using few frequently collected variables
- The ANZROD 24 model performed best 24 hours after admission (AUROC=0.83)
- Time after admission determines which prediction model is most useful
- Early after ICU admission, sepsis-specific models performed slightly better, while at 24 hours, general models not specific for sepsis performed well [3]
External Validation: AI for Lung Cancer Recurrence Risk
A 2025 study externally validated a machine learning-based survival model that incorporated preoperative CT images and clinical data to predict recurrence after surgery in patients with lung cancer [2]. The model was developed on 1,015 patients and validated on an external cohort of 252 patients. Key findings included:
- The ML model outperformed conventional TNM staging for stratifying stage I patients into high- and low-risk groups
- Higher hazard ratios were observed in external validation (HR=3.34) compared to conventional staging by tumor size (HR=1.98)
- The model showed significant correlations with established pathologic risk factors for recurrence (poor differentiation, lymphovascular invasion, pleural invasion) [2]
- The model successfully identified high-risk stage I patients who might benefit from more personalized treatment decisions and follow-up strategies [2]
Essential Research Reagents and Computational Tools
The implementation of rigorous validation methodologies requires specific technical resources and computational tools:
Table 4: Essential Research Reagents and Solutions for Validation Studies
| Category | Specific Tool/Reagent | Function in Validation | Technical Specifications |
|---|---|---|---|
| Data Management | HL7/API Interfaces [5] | Real-time data integration from laboratory systems | Standardized healthcare data exchange protocols |
| Computational | K-fold Cross-Validation [4] | Robust internal performance estimation | Typically 5-10 folds; repeated for stability |
| Computational | Bootstrap Resampling [1] | Optimism correction for model performance | 100+ iterations recommended [4] |
| Biomarkers | Transcriptomic Data [4] | High-dimensional predictors for prognosis | 15,000+ transcripts in simulation studies [4] |
| Imaging | CT Radiomic Features [2] | Image-derived biomarkers for AI models | Preoperative CT scans for recurrence prediction [2] |
| Molecular | BioFire Molecular Panels [5] | Standardized inputs for infectious disease models | FDA-approved comprehensive molecular panels |
| Validation | Human-in-the-Loop (HITL) [5] | Expert oversight of ML training data | Multiple infectious disease experts for consistency |
Integration Framework for Comprehensive Validation
The most robust validation strategy incorporates both internal and external components throughout the model development lifecycle. The following framework illustrates this integrated approach:
This integrated approach emphasizes that internal and external validation are complementary rather than competing processes. Internal validation provides the necessary foundation for model refinement and optimism correction, while external validation establishes generalizability and real-world applicability [1]. The scientific community increasingly recognizes that both components are essential for establishing a prediction model's credibility and potential clinical utility.
The Critical Role of Validation in Clinical Prediction Models and AI Tools
Clinical prediction models (CPMs) and artificial intelligence (AI) tools are transforming healthcare by forecasting individual patient risks for diagnostic and prognostic outcomes. Their safe and effective integration into clinical practice hinges on rigorous validation—the systematic process of evaluating a model's performance and reliability. Validation provides the essential evidence that a predictive algorithm is accurate, reliable, and fit for its intended clinical purpose [6] [7]. Without proper validation, there is a substantial risk of deploying models with optimistic or unknown performance, potentially leading to harmful clinical decisions [1].
The scientific discourse on validation centers on a crucial dichotomy: internal validation, which assesses model performance on data from the same underlying population used for development, and external validation, which evaluates performance on data from new, independent populations and settings [6]. This whitepaper provides an in-depth technical guide to these validation paradigms, offering researchers, scientists, and drug development professionals with the methodologies and frameworks necessary to robustly validate clinical predictive algorithms.
Core Concepts: Internal versus External Validation
Defining the Paradigms
Internal Validation: Internal validation assesses the reproducibility of an algorithm's performance on data distinct from the development set but derived from the exact same underlying population. Its primary goal is to quantify and correct for in-sample optimism or overfitting, which is the tendency of a model to perform better on its training data than on unseen data from the same population [6] [7]. It provides an optimism-corrected estimate of performance for the original setting [6].
External Validation: External validation assesses the transportability of a model to other settings beyond those considered during its development [6]. It examines whether the model's predictions hold true in different settings, such as new healthcare institutions, patient populations from different geographical regions, or data collected at a later point in time [1] [6]. It is often regarded as a gold standard for establishing model credibility [7].
The table below summarizes the key characteristics of and recommended methodologies for internal and external validation.
Table 1: Comparison of Internal and External Validation
| Aspect | Internal Validation | External Validation |
|---|---|---|
| Core Question | How well will the model perform in the source population? | Will the model work in a new, target population/setting? |
| Primary Goal | Quantify and correct for overfitting (optimism) [7]. | Assess transportability and generalizability [6]. |
| Key Terminology | Reproducibility, Optimism-Correction [6] [7]. | Transportability, Generalizability [6] [7]. |
| Recommended Methods | Bootstrapping, Cross-Validation [1] [6]. | Temporal, Geographical, and Domain Validation [6]. |
Methodologies for Internal Validation
Internal validation is not merely a box-ticking exercise; it is a necessary component of model development that provides a realistic estimate of performance in the absence of a readily available external dataset [1]. A robust internal validation is often sufficient, especially when the development dataset is large and the intended use population matches the development population [7].
Detailed Experimental Protocols
Protocol 1: Bootstrapping
Bootstrapping is widely considered the preferred approach for internal validation as it makes efficient use of the available data and provides a reliable estimate of optimism [1].
- Resampling: Generate a large number (typically 500-2000) of bootstrap samples from the original development dataset. Each sample is drawn with replacement and is of the same size as the original dataset [6].
- Model Development: On each bootstrap sample, develop a new model following the exact same steps used to create the original model. This includes any data pre-processing, variable selection, and parameter estimation procedures [1].
- Performance Assessment: Evaluate the performance (e.g., discrimination, calibration) of each bootstrap-derived model on two sets:
- The bootstrap sample (test performance).
- The original development dataset (training performance).
- Optimism Calculation: Calculate the optimism for each bootstrap sample as the difference between the test performance and the training performance.
- Optimism Correction: Average the optimism estimates from all bootstrap samples and subtract this value from the apparent performance (the performance of the original model on the original data) to obtain the optimism-corrected performance estimate [1].
Protocol 2: k-Fold Cross-Validation
This method is particularly useful when the sample size is limited, but it can be computationally intensive and may show more variability than bootstrapping.
- Data Partitioning: Randomly split the entire development dataset into k equally sized, mutually exclusive folds (common choices are k=5 or k=10).
- Iterative Training and Testing: For each of the k iterations:
- Designate one fold as the temporary validation set.
- Combine the remaining k-1 folds to form the training set.
- Develop a model on the training set using the full pre-specified modeling strategy.
- Test this model on the held-out validation fold and record its performance.
- Performance Aggregation: Aggregate the performance metrics (e.g., average them) from the k iterations to obtain a single cross-validated performance estimate. To enhance stability, the entire k-fold procedure can be repeated multiple times (e.g., 10x10-fold cross-validation) [6].
The Scientist's Toolkit: Internal Validation Reagents
Table 2: Essential Components for Internal Validation
| Item / Concept | Function / Explanation |
|---|---|
| Development Dataset | The single, source dataset containing the patient population used for initial model training. |
| Bootstrap Sample | A sample drawn with replacement from the development dataset, used to simulate new training sets. |
| Optimism | The difference between a model's performance on its training data vs. new data from the same population; the quantity to be estimated and corrected. |
| Optimism-Corrected Performance | The final, more realistic estimate of how the model would be expected to perform in the source population. |
| Discrimination Metric (e.g., C-index) | A measure of the model's ability to distinguish between cases and non-cases. |
| Calibration Metric | A measure of the agreement between predicted probabilities and observed outcomes. |
Methodologies for External Validation
External validation moves beyond the source data to test a model's performance in real-world conditions. It is the only way to truly assess a model's generalizability and is critical for determining its potential for broad clinical implementation [6].
A Framework for External Validity: Types of Generalizability
External validity can be broken down into three distinct types, each serving a unique goal and answering a specific question about the model's applicability [6].
- Temporal Validity: Assesses the performance of an algorithm over time at the development setting or in a new setting. This is crucial for understanding and detecting data drift—changes in the data distribution or patient population over time that can degrade model performance. It is typically assessed by testing the algorithm on a dataset from the same institution(s) but from a later time period [6].
- Geographical Validity: Assesses the generalizability of an algorithm to a different physical location, such as a new hospital, region, or country. This type of validation investigates heterogeneity across places and is required when an algorithm is intended for use outside its original development location. A powerful design for this is leave-one-site-out cross-validation within a multicenter study [6].
- Domain Validity: Assesses the generalizability of an algorithm to a different clinical context. This could involve changes in the medical background (e.g., emergency vs. surgical patients), medical setting (e.g., nursing home vs. hospital), or patient demographics (e.g., adult vs. pediatric populations). Performance is often better in "closely related" domains than in "distantly related" ones [6].
Detailed Experimental Protocol: The Internal-External Cross-Validation
This hybrid approach, often used in individual participant data meta-analysis (IPD-MA) or multicenter studies, provides a robust and efficient method for assessing external validity during the development phase [1] [6].
- Data Structuring: Assemble a dataset comprising multiple natural clusters. These could be different clinical studies (in an IPD-MA), different hospitals (in a multicenter study), or data from different calendar years [1].
- Iterative Validation Loop: For each cluster i in the dataset:
- Training Set: Designate all data except that from cluster i as the training set.
- Test Set: Designate the data from cluster i as the validation set.
- Model Development: Develop a model from scratch using only the training set.
- Model Testing: Validate this model on the held-out test set (cluster i) and record its performance.
- Performance Synthesis: Synthesize the performance metrics obtained from each of the held-out clusters to understand the model's performance variation across different settings.
- Final Model Development: After completing the loop, develop the final model to be used or published on the entire, pooled dataset. This final model is considered an 'internally-externally validated model' [1].
The Scientist's Toolkit: External Validation Reagents
Table 3: Essential Components for External Validation
| Item / Concept | Function / Explanation |
|---|---|
| Target Population | The clearly defined intended population and setting for the model's use; the focus of "targeted validation" [7]. |
| External Validation Dataset | A completely independent dataset from the target population, not used in any phase of model development. |
| Heterogeneity Assessment | The evaluation of differences in case-mix, baseline risk, and predictor-outcome associations across settings. |
| Model Updating | Techniques (e.g., recalibration, refitting) to adjust a model's performance for a new local setting. |
| Open Datasets (e.g., VitalDB) | Publicly accessible datasets that provide a highly practical resource for performing external validation, as demonstrated in a study predicting acute kidney injury [8]. |
Quantitative Data in Validation Studies
The performance of a clinical prediction model is quantified using specific metrics that evaluate different aspects of its predictive ability. The table below summarizes common performance metrics and their interpretation, providing a framework for comparing models across validation studies.
Table 4: Key Performance Metrics in Model Validation
| Metric Category | Specific Metric | Interpretation and Purpose | Example from Literature |
|---|---|---|---|
| Discrimination | C-index (AUC/AUROC) | Measures the model's ability to distinguish between patients with and without the outcome. A value of 0.5 is no better than chance; 1.0 is perfect discrimination [7] [8]. | A model for AKI prediction achieved an internal AUROC of 0.868 and an external AUROC of 0.757 on the VitalDB dataset, indicating good but reduced discrimination in the external population [8]. |
| Calibration | Calibration Slope & Intercept | Assesses the agreement between predicted probabilities and observed outcomes. A slope of 1 and intercept of 0 indicate perfect calibration. Deviations suggest over- or under-prediction [6]. | Poor calibration in a new setting often necessitates model updating (recalibration) before local implementation [6]. |
| Overall Performance | Brier Score | The mean squared difference between predicted probabilities and actual outcomes. Ranges from 0 to 1, where 0 represents perfect accuracy. | A lower Brier score indicates better overall accuracy of probabilistic predictions. |
| Clinical Usefulness | Net Benefit | A decision-analytic measure that quantifies the clinical value of using a prediction model for decision-making, by weighting true positives against false positives at a specific probability threshold [6]. | Used to compare the model against default strategies of "treat all" or "treat none" and to evaluate the impact of different decision thresholds. |
Validation is the cornerstone of credible clinical prediction models and AI tools. A rigorous, multi-faceted approach is non-negotiable. This begins with robust internal validation via bootstrapping to quantify optimism, providing a realistic performance baseline [1]. This must be followed by targeted external validation efforts designed to explicitly test performance in the model's intended clinical environment, whether that involves assessing temporal, geographical, or domain generalizability [6] [7].
The future of validation will be shaped by several key developments. The concept of "targeted validation" sharpens the focus on the intended use population, potentially reducing research waste and preventing misleading conclusions from irrelevant validation studies [7]. Furthermore, the adoption of structured reporting guidelines like TRIPOD and the forthcoming TRIPOD-AI will enhance the transparency, quality, and reproducibility of prediction model studies [6]. Finally, the strategic use of open datasets for external validation, as demonstrated in contemporary research, provides a viable and powerful pathway for demonstrating model generalizability in an era of data access challenges [8]. By adhering to these rigorous validation principles, researchers and drug developers can ensure that clinical predictive algorithms are not only statistically sound but also safe, effective, and reliable in diverse real-world settings.
In the scientific method as applied to predictive model development, validation is the cornerstone that separates speculative concepts from reliable tools. The process establishes that a model works satisfactorily for individuals other than those from whose data it was derived [9]. Within a broader thesis on validation research, this whitepaper addresses the critical pathway from internal checks to external verification, providing researchers and drug development professionals with rigorous methodologies for assessing model performance and generalizability.
The fundamental challenge in prediction model development lies in overcoming overfitting—where models correspond too closely to idiosyncrasies in the development dataset [10]. Internal validation focuses on reproducibility and overfitting within the original patient population, while external validation focuses on transportability and potential clinical benefit in new settings [9]. Without proper validation, models may produce inaccurate predictions and interpretations despite appearing successful during development [11].
Theoretical Foundations: Internal Versus External Validation
Defining the Validation Spectrum
Validation strategies vary in rigor and purpose, creating a spectrum from internal reproducibility checks to external generalizability assessments:
- Internal Validation: Makes use of the same data from which the model was derived, primarily focusing on quantifying and reducing optimism in performance estimates [10]. Common approaches include split-sample, cross-validation, and bootstrapping [10].
- Temporal Validation: An intermediate approach where the validation cohort is sampled at a different time point from the development cohort, for instance by developing a model on patients treated from 2010-2015 and validating on patients from the same hospital from 2015-2020 [10].
- External Validation: Tests the original prediction model in a structurally different set of new patients, which may come from different regions, care settings, or have different underlying diseases [10]. Independent external validation occurs when the validation cohort was assembled completely separately from the development cohort [10].
Conceptual Workflow for Model Validation
The following diagram illustrates the logical relationships and progression through different validation stages in a comprehensive model assessment strategy:
Quantitative Performance Metrics for Model Assessment
Core Metrics for Classification and Survival Models
A multifaceted approach to performance assessment is essential, as no single metric comprehensively captures model quality [12]. The following table summarizes key performance metrics across different model types:
| Metric Category | Specific Metric | Interpretation | Application Context |
|---|---|---|---|
| Discrimination | Area Under ROC (AUROC) | Probability model ranks random positive higher than random negative; 0.5=random, 1.0=perfect | Binary classification |
| Concordance Index (C-index) | Similar to AUROC for time-to-event data | Survival models | |
| F1 Score | Harmonic mean of precision and recall | Imbalanced datasets | |
| Calibration | Calibration Plot | Agreement between predicted probabilities and observed frequencies | Risk prediction models |
| Integrated Brier Score | Overall measure of prediction error | Survival models | |
| Clinical Utility | Net Benefit Analysis | Clinical value weighing benefits vs. harms | Decision support tools |
| Decision Curve Analysis | Net benefit across probability thresholds | Clinical implementation |
Performance Benchmarks from Validation Studies
Recent validation studies across medical domains demonstrate the expected performance differential between internal and external validation:
| Study Context | Internal Validation Performance | External Validation Performance | Performance Gap |
|---|---|---|---|
| Cervical Cancer OS Prediction [13] | C-index: 0.882 (95% CI: 0.874-0.890)3-year AUC: 0.913 | C-index: 0.872 (95% CI: 0.829-0.915)3-year AUC: 0.892 | C-index: -0.010AUC: -0.021 |
| Early-Stage Lung Cancer Recurrence [2] | Hazard Ratio: 1.71 (stage I)1.85 (stage I-III) | Hazard Ratio: 3.34 (stage I)3.55 (stage I-III) | HR improvement in external cohort |
| COVID-19 Diagnostic Model [14] | Not specified | Average AUC: 0.84Average calibration: 0.17 | Moderate impact from data similarity |
Experimental Protocols for Validation Studies
Internal Validation Methodologies
Split-Sample Validation
A cohort of patients is randomly divided into development and internal validation cohorts, typically with two-thirds of patients used for model development and one-third for validation [10]. This approach is generally inefficient in small datasets as it develops a poorer model on reduced sample size and provides unstable validation findings [1].
Cross-Validation
In k-fold cross-validation, the model is developed on k-1 folds of the population and tested on the remaining fold. This process is repeated k times, with each fold serving as the test set once [10]. For high-dimensional settings with limited samples, k-fold cross-validation demonstrates greater stability than train-test or bootstrap approaches [4].
Bootstrapping
Bootstrapping is a resampling method where numerous "new" cohorts are randomly selected by sampling with replacement from the original development population [10]. The model performance is tested in each resampled cohort and results are pooled to determine internal validation performance. The 0.632+ bootstrap method provides a bias-corrected estimate [4].
External Validation Protocol
A rigorous external validation protocol involves these critical methodological steps:
Model Selection: Choose an existing prediction model with clearly documented predictor variables and their coefficients, or the complete model equation [10].
Validation Cohort Definition: Assemble a new patient cohort that structurally differs from the development cohort through different locations, care settings, or time periods [10].
Predicted Risk Calculation: Compute the predicted risk for each individual in the external validation cohort using the original prediction formula and local predictor values [10].
Performance Assessment: Compare predicted risks to observed outcomes using discrimination, calibration, and clinical utility metrics [10] [12].
Heterogeneity Evaluation: Assess differences in patient characteristics, outcome incidence, and predictor effects between development and validation cohorts [1].
The following workflow details the complete experimental protocol for end-to-end model validation:
The Scientist's Toolkit: Research Reagent Solutions
Essential methodological components for rigorous validation studies include:
| Research Reagent | Function in Validation | Implementation Considerations |
|---|---|---|
| Bootstrap Resampling | Estimates optimism correction by sampling with replacement | Preferred for internal validation; requires 100+ iterations [10] |
| k-Fold Cross-Validation | Robust performance estimation in limited samples | Recommended for high-dimensional settings; k=5 or 10 typically [4] |
| Time-Dependent ROC Analysis | Evaluates discrimination for time-to-event data | Accounts for censoring in survival models [13] |
| Calibration Plots | Visualizes agreement between predicted and observed risks | Should include smoothed loess curves with confidence intervals [12] |
| Decision Curve Analysis | Quantifies clinical net benefit across threshold probabilities | Evaluates clinical utility, not just statistical performance [12] |
| Similarity Metrics | Quantifies covariate shift between development and validation datasets | Essential for interpreting external validation results [14] |
Methodological Pitfalls and Mitigation Strategies
Critical Errors in Validation Design
Several methodological pitfalls can severely compromise validation results while remaining undetectable during internal evaluation [11]:
Violation of Independence Assumption: Applying oversampling, feature selection, or data augmentation before data splitting creates data leakage. For example, applying oversampling before data splitting artificially inflated F1 scores by 71.2% for predicting local recurrence in head and neck cancer [11].
Inappropriate Performance Metrics: Using accuracy for imbalanced datasets or relying solely on discrimination without assessing calibration. In imbalanced datasets, a model that always predicts the majority class can have high accuracy while being clinically useless [12].
Batch Effects: Systematic differences in data collection or processing between development and validation cohorts. One pneumonia detection model achieved an F1 score of 98.7% internally but correctly classified only 3.86% of samples from a new dataset of healthy patients due to batch effects [11].
Recommended Mitigation Approaches
Temporal Splitting: Instead of random data splitting, use temporal validation where the validation cohort comes from a later time period than the development cohort [1] [10].
Multiple Performance Metrics: Report discrimination, calibration, and clinical utility metrics together for a comprehensive assessment [12].
Internal-External Cross-Validation: In multicenter studies, leave out each center once for validation of a model developed on the remaining centers, with the final model based on all available data [1].
The validation of prediction models deserves more recognition in the scientific process [9]. Despite methodological advances, external validation remains uncommon—only about 5% of prediction model studies mention external validation in their title or abstract [10]. This validation gap hinders the emergence of critical, well-founded knowledge on clinical prediction models' true value.
Researchers should consider that developing a new model with insufficient sample size is often less valuable than conducting a rigorous validation of an existing model [9]. As we move toward personalized medicine with rapidly evolving therapeutic options, validation must be recognized not as a one-time hurdle but as an ongoing process throughout a model's lifecycle [14] [9]. Through rigorous validation practices, the scientific community can ensure that prediction models fulfill their promise to enhance patient care and treatment outcomes.
In the realm of statistical prediction and machine learning, the ultimate goal is to develop models that generalize effectively to new, unseen data. However, this objective is persistently challenged by the dual problems of overfitting and optimism. Overfitting occurs when a model learns not only the underlying patterns in the training data but also the noise and random fluctuations, essentially "memorizing" the training set rather than learning to generalize [15] [16]. This phenomenon is particularly problematic in scientific research and drug development, where models must reliably inform critical decisions.
The statistical concept of "optimism" refers to the systematic overestimation of a model's performance when evaluated on the same data used for its training. This optimism bias arises because the model has already seen and adapted to the specific peculiarities of the training sample, performance metrics appear better than they would on independent data [1]. Understanding and correcting for this optimism is fundamental to building trustworthy predictive models in clinical research, where inaccurate predictions can directly impact patient care and therapeutic development.
This paper situates the discussion of overfitting and optimism within the broader framework of model validation, distinguishing between internal validation—assessing model performance on data from the same population—and external validation—evaluating performance on data from different populations, institutions, or time periods [17] [9]. While internal validation techniques aim to quantify and correct for optimism, external validation provides the ultimate test of a model's transportability and real-world utility.
The Statistical Nature of Overfitting and the Bias-Variance Tradeoff
Conceptual Foundations of Overfitting
Overfitting represents a fundamental failure in model generalization. An overfit model exhibits low bias but high variance, meaning it performs exceptionally well on training data but poorly on unseen test data [15] [18]. This occurs when a model becomes excessively complex relative to the amount and quality of training data, allowing it to capture spurious relationships that do not reflect true underlying patterns.
The analogy of student learning effectively illustrates this concept: a student who memorizes textbook answers without understanding underlying concepts will ace practice tests but fail when confronted with novel questions on the final exam [15]. Similarly, an overfit model memorizes the training data but cannot extrapolate to new situations.
The Bias-Variance Tradeoff
The concepts of overfitting and its opposite, underfitting, are governed by the bias-variance tradeoff, which represents a core challenge in statistical modeling [15] [16]. This framework helps understand the relationship between model complexity and generalization error:
- High Bias (Underfitting): The model is too simple to capture underlying patterns, leading to high errors on both training and test data.
- High Variance (Overfitting): The model is too complex and sensitive to training data fluctuations, leading to low training error but high test error.
- Balanced Model: Achieves optimal complexity with low bias and low variance, performing well on both training and test data [15].
Table 1: Characteristics of Model Fit States
| Feature | Underfitting | Overfitting | Good Fit |
|---|---|---|---|
| Performance | Poor on train & test | Great on train, poor on test | Great on train & test |
| Model Complexity | Too Simple | Too Complex | Balanced |
| Bias | High | Low | Low |
| Variance | Low | High | Low |
| Primary Fix | Increase complexity/features | Add more data/regularize | Optimal achieved |
The following diagram illustrates the conceptual relationship between model complexity, error, and the bias-variance tradeoff:
Quantifying Optimism in Predictive Performance
The Optimism Principle
Statistical optimism refers to the difference between a model's apparent performance (measured on the training data) and its true performance (expected performance on new data) [1]. This bias emerges because the same data informs both model building and performance assessment, creating an overoptimistic view of model accuracy. The optimism principle states that:
Optimism = E[Apparent Performance] - E[True Performance]
Where E[Apparent Performance] represents expected performance on training data and E[True Performance] represents expected performance on new data. In practice, optimism is always positive, meaning models appear better than they truly are.
Mathematical Formulations
For common performance metrics, optimism can be quantified mathematically. In linear regression, the relationship between expected prediction error and model complexity follows known distributions that allow for optimism correction. The expected optimism increases with model complexity (number of parameters) and decreases with sample size [1].
For logistic regression models predicting binary outcomes, the optimism can be quantified through measures like the overfitting-induced bias in hazard ratios or odds ratios. Research has shown that very high odds ratios (e.g., 36.0 or more) are often required for a new biomarker to substantially improve predictive ability beyond existing markers, highlighting how standard significance testing (small p-values) can be misleading without proper validation [17].
Internal Validation Techniques for Optimism Correction
Core Methodologies
Internal validation techniques aim to provide realistic estimates of model performance by correcting for optimism within the available dataset. These methods include:
4.1.1 Bootstrapping Techniques Bootstrapping is widely considered the preferred approach for internal validation of prediction models [1]. This method involves repeatedly sampling from the original dataset with replacement to create multiple bootstrap samples. The model building process is applied to each bootstrap sample, and performance is evaluated on both the bootstrap sample and the original dataset. The average difference between these performances provides an estimate of the optimism, which can then be subtracted from the apparent performance.
Table 2: Internal Validation Methods Comparison
| Method | Procedure | Advantages | Limitations |
|---|---|---|---|
| Bootstrapping | Repeated sampling with replacement; full modeling process on each sample | Most efficient use of data; preferred for small samples | Computationally intensive |
| K-fold Cross-Validation | Data divided into K subsets; iteratively use K-1 for training, 1 for validation [16] | Reduced variance compared to single split | Can be optimistic if modeling steps not repeated |
| Split-Sample | Random division into training and test sets (e.g., 70/30) | Simple to implement | Inefficient data use; unstable in small samples [1] |
| Internal-External Cross-Validation | Natural splits by study, center, or time period | Provides assessment of transportability | Requires multiple natural partitions |
4.1.2 Cross-Validation Protocols In k-fold cross-validation, the dataset is partitioned into k equally sized folds or subsets [16]. The model is trained on k-1 folds and validated on the remaining fold, repeating this process k times with each fold serving once as the validation set. The performance estimates across all k folds are then averaged to produce a more robust assessment less affected by optimism.
Implementation Considerations
The key to effective internal validation lies in repeating the entire model building process—including any variable selection, transformation, or hyperparameter tuning steps—within each validation iteration [1]. Failure to do so can lead to substantial underestimation of optimism. For small datasets (median sample size in many clinical prediction models is only 445 subjects), bootstrapping is particularly recommended over split-sample methods, which perform poorly when sample size is limited [1].
External Validation: Beyond Optimism to Generalizability
The External Validation Imperative
While internal validation corrects for statistical optimism, external validation assesses a model's generalizability to different populations, settings, or time periods [17] [9]. External validation involves applying the model to completely independent data that played no role in model development and ideally was unavailable to the model developers.
True external validation requires "transportability" assessment—evaluating whether the model performs satisfactorily in different clinical settings, patient populations, or with variations in measurement techniques [9]. This is distinct from "reproducibility," which assesses performance in similar settings.
Methodological Approaches
5.2.1 Temporal and Geographic Validation Temporal validation assesses model performance on patients from the same institutions but from a later time period, testing stability over time. Geographic validation evaluates performance on patients from different institutions or healthcare systems, testing transportability across settings [1].
5.2.2 Internal-External Cross-Validation In datasets with natural clustering (e.g., multiple centers in a clinical trial), internal-external cross-validation systematically leaves out one cluster at a time (e.g., one clinical center), develops the model on the remaining data, and validates on the left-out cluster [1]. This approach provides insights into a model's potential generalizability while still using all data for final model development.
5.2.3 Heterogeneity Assessment More direct than global performance measures are tests for heterogeneity in predictor effects across settings or time. This can be achieved through random effects models (with many studies) or testing interaction terms (e.g., "predictor × study" or "predictor × calendar time") [1].
The following workflow diagram illustrates the comprehensive validation process from model development through to external validation:
Experimental Protocols for Validation Studies
Sample Size Considerations
Adequate sample size is critical for both model development and validation. For external validation studies, sample size calculations should ensure sufficient precision for performance measure estimates [9]. One framework recommends that external validation studies require a minimum of 100 events and 100 non-events for binary outcomes to precisely estimate key performance measures like the C-statistic and calibration metrics.
For model development, the events per variable (EPV) ratio—the number of events divided by the number of candidate predictor parameters—should ideally be at least 10-20 to minimize overfitting [1]. In biomarker studies with high-dimensional data (e.g., genomic markers), regularized regression methods (LASSO, ridge regression) are preferred to conventional variable selection to mitigate overfitting.
Performance Measures and Evaluation
Comprehensive validation requires multiple performance measures to assess different aspects of model performance:
6.2.1 Discrimination Measures
- C-statistic (AUC): For binary outcomes, measures the model's ability to distinguish between cases and non-cases
- R²: Proportion of variance explained (for continuous outcomes)
6.2.2 Calibration Measures
- Calibration-in-the-large: Comparison of average predicted risk versus observed risk
- Calibration slope: Degree of overfitting/underfitting (ideal value = 1)
- Calibration plots: Visual assessment of predicted versus observed risks
6.2.3 Clinical Utility
- Decision curve analysis: Net benefit across different decision thresholds
- Classification measures: Sensitivity, specificity, predictive values at clinically relevant thresholds
Research Reagent Solutions: Methodological Toolkit
Table 3: Essential Methodological Tools for Validation Studies
| Tool Category | Specific Methods | Function/Purpose |
|---|---|---|
| Internal Validation | Bootstrapping, k-fold cross-validation, repeated hold-out | Estimates and corrects for optimism in performance measures |
| Regularization Methods | Ridge regression, LASSO, elastic net | Prevents overfitting in high-dimensional data; performs variable selection |
| Performance Measures | C-statistic, Brier score, calibration plots, decision curve analysis | Comprehensively assesses discrimination, calibration, and clinical utility |
| Software/Computational | R packages (rms, glmnet, caret), Python (scikit-learn), Amazon SageMaker [16] | Implements validation protocols; detects overfitting automatically |
| Statistical Frameworks | TRIPOD+AI statement [9], REMARK guidelines (biomarkers) [17] | Reporting standards ensuring complete and transparent methodology |
The statistical underpinnings of overfitting and optimism reveal fundamental truths about the limitations of predictive modeling. While internal validation techniques provide essential corrections for optimism, they cannot fully replace the rigorous assessment provided by external validation [9]. The scientific community, particularly in high-stakes fields like drug development, must prioritize both internal and external validation to establish trustworthy prediction models.
Future directions should emphasize ongoing validation as a continuous process rather than a one-time event, especially given the dynamic nature of medical practice and evolving patient populations [9]. Furthermore, impact studies assessing whether prediction models actually improve patient outcomes when implemented in clinical practice represent the ultimate validation of a model's value beyond statistical performance metrics.
By understanding and addressing the statistical challenges of overfitting and optimism, researchers can develop more robust, reliable predictive models that genuinely advance scientific knowledge and improve decision-making in drug development and clinical care.
In contemporary drug development, the translation of preclinical findings into clinically effective therapies remains a significant challenge. Validation strategies are paramount in bridging this gap, ensuring that predictive models and experimental results are both reliable and generalizable. The validation process is fundamentally divided into two complementary phases: internal validation, which assesses a model's performance on the originating dataset and aims to mitigate optimism bias, and external validation, which evaluates its performance on entirely independent data, establishing generalizability and real-world applicability [13] [4]. Despite recognized frameworks, critical gaps persist, particularly in the transition from internal to external validation and in the handling of high-dimensional data, which can lead to failed clinical trials and inefficient resource allocation. This paper examines these gaps within the current drug development landscape, provides a quantitative analysis of prevailing methodologies, and outlines detailed experimental protocols and tools to bolster validation robustness.
Quantitative Landscape of Validation in Current Drug Development
An analysis of the active Alzheimer's disease (AD) drug development pipeline for 5 reveals a vibrant ecosystem with 138 drugs across 182 clinical trials [19]. This landscape provides a context for understanding the scale at which robust validation is required. The following tables summarize key quantitative data from recent studies, highlighting the performance of prognostic models and the characteristics of the current drug pipeline.
Table 1: Performance Metrics of a Validated Prognostic Model in Cervical Cancer (Sample Size: 13,592 patients from SEER database) [13]
| Validation Cohort | Sample Size | C-Index (95% CI) | 3-Year OS AUC | 5-Year OS AUC | 10-Year OS AUC |
|---|---|---|---|---|---|
| Training (TC) | 9,514 | 0.882 (0.874–0.890) | 0.913 | 0.912 | 0.906 |
| Internal (IVC) | 4,078 | 0.885 (0.873–0.897) | 0.916 | 0.910 | 0.910 |
| External (EVC) | 318 | 0.872 (0.829–0.915) | 0.892 | 0.896 | 0.903 |
Table 2: Simulation Study of Internal Validation Methods for High-Dimensional Prognosis Models (Head and Neck Cancer Transcriptomic Data) [4]
| Validation Method | Sample Size (N) | Performance Stability | Key Finding / Recommendation |
|---|---|---|---|
| Train-Test (70/30) | 50 - 1000 | Unstable | Showed unstable performance across sample sizes. |
| Conventional Bootstrap | 50 - 100 | Over-optimistic | Particularly over-optimistic with small samples. |
| 0.632+ Bootstrap | 50 - 100 | Over-pessimistic | Particularly over-pessimistic with small samples. |
| K-Fold Cross-Validation | 500 - 1000 | Stable | Recommended for its greater stability. |
| Nested Cross-Validation | 500 - 1000 | Fluctuating | Performance fluctuated with the regularization method. |
Table 3: Profile of the 2025 Alzheimer's Disease Drug Development Pipeline [19]
| Category | Number of Agents | Percentage of Pipeline | Notes |
|---|---|---|---|
| Total Novel Drugs | 138 | - | Across 182 clinical trials. |
| Small Molecule DTTs | ~59 | 43% | Disease-Targeted Therapies. |
| Biological DTTs | ~41 | 30% | e.g., Monoclonal antibodies, vaccines. |
| Cognitive Enhancers | ~19 | 14% | Symptomatic therapies. |
| Neuropsychiatric Symptom Drugs | ~15 | 11% | e.g., For agitation, psychosis. |
| Repurposed Agents | ~46 | 33% | Approved for another indication. |
| Trials Using Biomarkers | ~49 | 27% | As primary outcomes. |
Detailed Experimental Protocols for Internal and External Validation
Protocol 1: Internal-External Validation of a Clinical Prognostic Model
This protocol is based on a retrospective study developing a nomogram for predicting overall survival (OS) in cervical cancer [13].
- Objective: To develop and validate a prognostic model for predicting 3-year, 5-year, and 10-year overall survival in cervical cancer patients.
- Data Source and Cohort Selection:
- Primary data was extracted from the Surveillance, Epidemiology, and End Results (SEER) database for patients diagnosed between 2000 and 2020.
- Inclusion Criteria: Primary tumor site clearly identified as the cervix (C53), diagnosis between 2000-2020, and behavior code indicating malignancy.
- Exclusion Criteria: Non-cancer-related deaths, missing data (tumor type, grade, size, treatment), and incomplete survival records.
- A total of 13,592 patient records were obtained and randomly split into a training cohort (TC, n=9,514) and an internal validation cohort (IVC, n=4,078) using a 7:3 ratio and random number tables.
- Predictor Variables and Endpoint:
- Ten initial predictors were selected: age, histologic subtype, FIGO 2018 stage, tumor size, tumor grade, lymph node metastasis (LNM), lymph-vascular space invasion (LVSI), invasion, radiation therapy, and chemotherapy.
- The primary endpoint was overall survival (OS).
- Statistical Analysis and Model Development:
- Univariate Cox regression analysis was performed on the TC to identify significant predictors.
- Statistically significant factors from the univariate analysis were entered into a multivariate Cox regression model to identify independent prognostic factors. The final model was selected based on the highest concordance index (C-index).
- A nomogram was constructed to visualize the model and predict 3-, 5-, and 10-year OS probabilities.
- Validation and Performance Assessment:
- Internal Validation: The nomogram was applied to the IVC.
- External Validation: The model was tested on an external validation cohort (EVC) of 318 patients from Yangming Hospital Affiliated to Ningbo University (2008-2020).
- Performance was assessed using the C-index, time-dependent receiver operating characteristic (ROC) curves, calibration charts, and decision curve analysis (DCA).
Protocol 2: Internal Validation of a High-Dimensional Prognostic Model
This protocol is derived from a simulation study focusing on internal validation strategies for transcriptomic-based prognosis models in head and neck tumors [4].
- Objective: To compare internal validation strategies for Cox penalized regression models in high-dimensional time-to-event settings and provide recommendations.
- Data Simulation:
- A simulation study was conducted using real data parameters from the SCANDARE head and neck cohort (n=76).
- Simulated datasets included clinical variables (age, sex, HPV status, TNM staging) and transcriptomic data (15,000 transcripts).
- Disease-free survival was simulated with a realistic cumulative baseline hazard.
- Sample sizes of N=50, 75, 100, 500, and 1000 were simulated, with 100 replicates for each sample size.
- Model Development:
- Cox penalized regression (e.g., Lasso, Ridge, Elastic Net) was performed for model selection on each simulated dataset.
- Internal Validation Strategies Compared:
- Train-Test Validation: 70% of data for training, 30% for testing.
- Bootstrap Validation: 100 bootstrap iterations.
- 0.632+ Bootstrap Validation: An enhanced bootstrap method to correct optimism.
- K-Fold Cross-Validation: 5-fold cross-validation.
- Nested Cross-Validation: 5x5 nested cross-validation.
- Performance Metrics:
- Discrimination: Assessed using the C-Index and time-dependent Area Under the Curve (AUC).
- Calibration: Assessed using the 3-year integrated Brier Score.
Visualization of Validation Workflows and Method Selection
The following diagrams, generated with Graphviz, illustrate the logical relationships and workflows for the validation strategies discussed.
Diagram 1: Clinical Model Validation Workflow
Diagram 2: Internal Validation Method Selection
The Scientist's Toolkit: Essential Research Reagents and Materials
This section details key reagents, datasets, and software tools essential for conducting robust validation in drug development, as referenced in the featured studies and broader context.
Table 4: Key Research Reagent Solutions for Validation Studies
| Item / Solution | Function / Application | Example from Context |
|---|---|---|
| SEER Database | A comprehensive cancer registry database providing incidence, survival, and treatment data for a significant portion of the US population. Used for developing and internally validating large-scale prognostic models. | Source of 13,592 cervical cancer patient records for model development and internal validation [13]. |
| ClinicalTrials.gov | A federally mandated registry of clinical trials. Serves as the primary source for analyzing the drug development pipeline, including trial phases, agents, and biomarkers. | Primary data source for profiling the 2025 Alzheimer's disease pipeline (182 trials, 138 drugs) [19]. |
| Institutional Patient Registries | Hospital or university-affiliated databases containing detailed clinical, pathological, and outcome data. Critical for external validation of models developed from larger public databases. | External validation cohort (N=318) from Yangming Hospital used to test the generalizability of the cervical cancer nomogram [13]. |
| R Software with Survival Packages | Open-source statistical computing environment. Essential for performing complex survival analyses, Cox regression, and generating nomograms and validation metrics. | Used for all statistical analyses, including univariate/multivariate Cox regression and nomogram construction [13]. |
| Cox Penalized Regression Algorithms | Statistical methods (e.g., Lasso, Ridge, Elastic Net) used for model selection and development in high-dimensional settings where the number of predictors (p) far exceeds the number of observations (n). | Used for model selection in the high-dimensional transcriptomic simulation study [4]. |
| Biomarker Assays | Analytical methods (e.g., immunoassays, genomic sequencing) to detect physiological or pathological states. Used for patient stratification and as outcomes in clinical trials. | Biomarkers were used as primary outcomes in 27% of active AD trials and for establishing patient eligibility [19]. |
Implementation Strategies: Rigorous Validation Techniques for Predictive Models
In the realm of statistical modeling and machine learning, the ultimate test of a model's value lies not in its performance on the data used to create it, but in its ability to make accurate predictions on new, unseen data. This principle is especially critical in fields like pharmaceutical research and drug development, where model predictions can influence significant clinical decisions. Internal validation provides a framework for estimating this future performance using only the data available at the time of model development, before committing to costly external validation studies or real-world deployment [20] [21].
Internal validation exists within a broader validation framework that includes external validation. While internal validation assesses how the model will perform on new data drawn from the same population, external validation tests the model on data collected by different researchers, in different settings, or from different populations [20] [21] [22]. A model must first demonstrate adequate performance in internal validation before the resource-intensive process of external validation is justified. Without proper internal validation, researchers risk deploying models that suffer from overfitting—a situation where a model learns the noise specific to the development dataset rather than the underlying signal, resulting in poor performance on new data [23].
This technical guide provides an in-depth examination of the two predominant internal validation methodologies: bootstrapping and cross-validation. We will explore their theoretical foundations, detailed implementation protocols, comparative strengths and weaknesses, and practical applications specifically for research scientists and drug development professionals.
Theoretical Foundations: Bootstrapping vs. Cross-Validation
The Bootstrap Methodology
Bootstrapping is a resampling technique that estimates the sampling distribution of a statistic by repeatedly drawing new samples with replacement from the original dataset. In the context of internal validation, it is primarily used to estimate and correct for the optimism bias in apparent model performance (the performance measured on the same data used for training) [24] [22].
The fundamental principle behind bootstrap validation is that each bootstrap sample, created by sampling with replacement from the original dataset of size N, contains approximately 63.2% of the unique original observations, with the remaining 36.8% forming the out-of-bag (OOB) sample that can be used for validation [22]. By comparing the performance of a model fitted on the bootstrap sample when applied to that same sample (optimistic estimate) versus when applied to the original dataset or the OOB sample (pessimistic estimate), we can calculate an optimism statistic. This optimism is then subtracted from the apparent performance to obtain a bias-corrected performance estimate [24] [25].
Several variations of the bootstrap exist for model validation, with the .632 and .632+ estimators being particularly important. The standard bootstrap .632 estimator combines the apparent performance and the out-of-bag performance using fixed weights (0.368 and 0.632 respectively), while the more sophisticated .632+ estimator uses adaptive weights based on the relative overfitting rate to provide a less biased estimate, particularly for models that perform little better than random guessing [22].
The Cross-Validation Methodology
Cross-validation (CV) provides an alternative approach to internal validation by systematically partitioning the available data into complementary subsets for training and validation. The most common implementation, k-fold cross-validation, divides the dataset into k roughly equal-sized folds or segments [26] [23].
In each of the k iterations, k-1 folds are used to train the model, while the remaining single fold is held back for validation. This process is repeated k times, with each fold serving exactly once as the validation set. The performance metrics from all k iterations are then averaged to produce a single estimate of model performance [26]. This approach ensures that every observation in the dataset is used for both training and validation, making efficient use of limited data.
Common variants of cross-validation include:
- Stratified K-Fold: Maintains the same class distribution in each fold as in the complete dataset, particularly important for imbalanced datasets [26].
- Leave-One-Out Cross-Validation (LOOCV): A special case where k equals the number of observations (N), providing nearly unbiased estimates but with high computational cost and variance, especially for large datasets [26].
- Repeated K-Fold: Performs multiple rounds of k-fold CV with different random splits of the data, providing more robust performance estimates at increased computational cost [25].
Methodological Protocols and Implementation
Bootstrap Validation Protocol
The bootstrap validation process follows a systematic protocol to obtain a bias-corrected estimate of model performance. The following workflow outlines the key steps in this procedure, with specific emphasis on the calculation of the optimism statistic.
Figure 1: Workflow diagram of the bootstrap validation process for estimating model optimism.
Detailed Step-by-Step Protocol
Model Development on Original Data: Begin by fitting the model to the entire original dataset (Dorig) and calculate the apparent performance (θapparent) by evaluating the model on this same data. This initial performance estimate is typically optimistically biased [24] [22].
Bootstrap Resampling: Generate B bootstrap samples (typically B = 200-400) by sampling N observations with replacement from the original dataset. Each bootstrap sample (D_boot) contains approximately 63.2% of the unique original observations, with some observations appearing multiple times [24] [22].
Bootstrap Model Training and Validation: For each bootstrap sample b = 1 to B:
- Fit the model to the bootstrap sample D_boot^b
- Calculate the bootstrap performance (θboot^b) by evaluating this model on Dboot^b itself
- Calculate the test performance (θtest^b) by evaluating the model on the original dataset Dorig
Optimism Calculation: Compute the optimism statistic for each bootstrap iteration: O^b = θboot^b - θtest^b. The average optimism across all B iterations is given by: Ō = (1/B) × ΣO^b [24].
Bias-Corrected Performance: Subtract the average optimism from the apparent performance to obtain the optimism-corrected performance estimate: θcorrected = θapparent - Ō [24].
For enhanced accuracy, particularly with models showing significant overfitting, the .632+ estimator can be implemented, which uses adaptive weighting between the apparent and out-of-bag performances based on the relative overfitting rate [22].
Essential Research Reagents: Computational Tools for Bootstrap Validation
Table 1: Essential computational tools and their functions for implementing bootstrap validation
| Tool/Platform | Primary Function | Implementation Example |
|---|---|---|
| R Statistical Software | Comprehensive environment for statistical computing and graphics | boot package for bootstrap procedures [24] |
| rms Package (R) | Regression modeling strategies with built-in validation functions | validate() function for automated bootstrap validation [24] |
| Python Scikit-Learn | Machine learning library with resampling capabilities | Custom implementation using resample function |
| Stata | Statistical software for data science | bootstrap command for resampling and validation [25] |
Cross-Validation Protocol
The k-fold cross-validation method provides a structured approach to assessing model performance through systematic data partitioning. The following workflow illustrates the process for a single k-fold cross-validation cycle.
Figure 2: Workflow diagram of the k-fold cross-validation process for model performance estimation.
Detailed Step-by-Step Protocol
Data Partitioning: Randomly shuffle the dataset and partition it into k roughly equal-sized folds or segments. For stratified k-fold CV (recommended for classification problems), ensure that each fold maintains approximately the same class distribution as the complete dataset [26] [23].
Iterative Training and Validation: For each fold i = 1 to k:
- Designate fold i as the validation set, and the remaining k-1 folds as the training set
- Fit the model using the training set (k-1 folds)
- Evaluate the fitted model on the validation set (fold i)
- Record the performance metric (e.g., accuracy, AUC) for this iteration
Performance Aggregation: Calculate the final cross-validation performance estimate by averaging the performance metrics across all k iterations: θcv = (1/k) × Σθi [26] [23].
Optional Repetition: For increased reliability, particularly with smaller datasets, repeat the entire k-fold process multiple times (e.g., 10×10-fold CV or 100×10-fold CV) with different random partitions, and average the results across all repetitions [25].
Essential Research Reagents: Computational Tools for Cross-Validation
Table 2: Essential computational tools and their functions for implementing cross-validation
| Tool/Platform | Primary Function | Implementation Example |
|---|---|---|
| Python Scikit-Learn | Machine learning library with comprehensive CV utilities | cross_val_score, KFold, StratifiedKFold [23] |
| R caret Package | Classification and regression training with CV support | trainControl function with CV method [26] |
| R Statistical Software | Base environment for statistical computing | Custom implementation with loop structures |
| Weka | Collection of machine learning algorithms | Built-in cross-validation evaluation option |
Comparative Analysis and Practical Applications
Quantitative Comparison of Methodologies
The choice between bootstrap and cross-validation methods depends on various factors including dataset characteristics, computational resources, and the specific modeling objectives. The following table provides a structured comparison to guide methodology selection.
Table 3: Comprehensive comparison of bootstrap and cross-validation methods for internal validation
| Characteristic | Bootstrap Validation | K-Fold Cross-Validation |
|---|---|---|
| Primary Strength | Optimism correction, uncertainty estimation [24] [22] | Reduced bias, reliable performance estimation [26] [23] |
| Sample Size Suitability | Excellent for small samples (n < 200) [27] | Preferred for medium to large datasets [27] |
| Computational Efficiency | Moderate (200-400 iterations typically) [24] | Varies with k; generally efficient for k=5 or 10 [26] |
| Performance Estimate Bias | Can be biased with highly imbalanced data [27] | Lower bias with appropriate k [26] |
| Variance Properties | Lower variance, stable estimates [25] | Higher variance, especially with small k [26] |
| Data Utilization | Models built with ~63.2% of unique observations [22] | Models built with (k-1)/k of data in each iteration [23] |
| Key Advantage | Validates model built on full sample size N [25] | Efficient use of all data for training and testing [26] |
| Implementation Complexity | Moderate (requires custom programming) [24] | Low (readily available in most ML libraries) [23] |
Applications in Pharmaceutical Research and Drug Development
The selection of appropriate internal validation methods has particular significance in pharmaceutical research, where predictive models inform critical development decisions:
Clinical Prediction Models: Bootstrap methods are particularly valuable for validating clinical prediction models developed from limited patient cohorts, common in rare disease research or early-phase clinical trials [27]. The bootstrap's ability to provide confidence intervals for performance metrics alongside bias-corrected point estimates makes it invaluable for assessing model robustness with limited data.
Biomarker Discovery and Genomic Applications: In high-dimensional settings such as genomics and proteomics (e.g., GWAS, transcriptomic analyses), where the number of features (p) far exceeds the number of observations (N), repeated k-fold cross-validation is often preferred as it remains effective even when N < p [25]. The stratification capability of k-fold CV also helps maintain class balance in imbalanced biomarker validation studies.
Causal Inference and Treatment Effect Estimation: While both methods have applications in causal modeling, bootstrap is particularly widely used for quantifying variability in treatment effect estimates (e.g., bootstrapped confidence intervals for Average Treatment Effects) [27]. Cross-validation finds application in assessing the predictive accuracy of propensity score models or outcome regressions within causal frameworks.
Bayesian Models: For Bayesian approaches, which naturally quantify uncertainty through posterior distributions, leave-one-out cross-validation (LOOCV) and its approximations (e.g., WAIC, PSIS-LOO) are commonly employed, while bootstrap validation is less frequently used as the posterior samples already account for parameter uncertainty [27].
Internal validation through bootstrapping and cross-validation represents a critical phase in the model development lifecycle, providing essential estimates of how well a model will perform on new data from the same population. While bootstrap methods excel in small-sample settings and provide robust optimism correction, cross-validation techniques offer efficient performance estimation with reduced bias for medium to large datasets.
In practical applications, the choice between these methodologies should be guided by dataset characteristics, computational constraints, and the specific inferential goals of the modeling exercise. For regulatory submissions in drug development, where model transparency and robustness are paramount, implementing rigorous internal validation using either approach—or sometimes both in complementary fashion—strengthens the evidentiary basis for models intended to inform clinical decision-making.
As the field advances, hybrid approaches and enhancements to both bootstrap and cross-validation methodologies continue to emerge, offering researchers an expanding toolkit for ensuring that their predictive models will deliver reliable performance when deployed in real-world settings. Regardless of the specific technique employed, the commitment to rigorous internal validation remains fundamental to building trustworthy predictive models in pharmaceutical research and development.
Within the broader framework of internal versus external validation research, split-sample validation remains a commonly used yet often misunderstood methodology. This technical guide provides a comprehensive examination of split-sample validation, with particular focus on its applications and limitations in large datasets. We synthesize current methodological research to clarify when random data partitioning is statistically justified and when alternative validation approaches are preferable. For researchers and drug development professionals, this review offers evidence-based protocols and decision frameworks to enhance validation practices in prognostic model development.
Validation of predictive models represents a cornerstone of scientific rigor in clinical and translational research. Within this domain, a fundamental distinction exists between internal validation (assessing model performance for a single underlying population) and external validation (assessing generalizability to different populations) [28]. Split-sample validation, which randomly partitions available data into development and validation sets, represents one approach to internal validation but is frequently misapplied as a substitute for true external validation [10].
The persistence of split-sample methods in the literature—despite considerable methodological criticism—warrants careful examination of its appropriate applications, particularly in the context of increasingly large biomedical datasets. This review situates split-sample validation within the broader validation research landscape, examining its technical specifications, performance characteristics, and limited indications for use in large-scale research.
Theoretical Foundations: Definitions and Concepts
What is Split-Sample Validation?
Split-sample validation (also called hold-out validation) involves randomly dividing a dataset into two separate subsets: a training set used for model development and a testing set used for performance evaluation [29]. This approach represents a form of internal validation, as it assesses performance on data from the same underlying population [28].
The fundamental principle is that by evaluating model performance on data not used during training, researchers can estimate how well the model might perform on future unseen cases. Common split ratios include 70/30, 80/20, or 50/50 divisions, though the statistical rationale for these ratios varies considerably [30].
Distinguishing Between Validation Types
Understanding split-sample validation requires positioning it within the broader validation taxonomy:
- Apparent Validation: Evaluating performance on the same data used for training; notoriously optimistic [28]
- Internal Validation: Assessing performance for a single underlying population, including split-sample, cross-validation, and bootstrapping methods [10]
- External Validation: Testing model transportability to different populations, settings, or time periods [10]
Split-sample validation occupies a middle ground between apparent validation and true external validation, providing a limited assessment of generalizability while remaining within the original dataset.
Applications in Large Datasets: When Split-Sample Validation May Be Appropriate
The Large Dataset Exception
Methodological research has demonstrated that split-sample validation is generally inefficient, particularly for small to moderate-sized datasets [1] [31]. However, in the context of very large datasets (typically n > 20,000), some limitations of data splitting become less pronounced [32]. As Steyerberg and Harrell note, "split-sample validation only works when not needed," meaning it becomes viable only when datasets are sufficiently large that both training and validation subsets can support reliable development and evaluation [1].
The underlying rationale is that with ample data, both development and validation sets can be large enough to yield stable parameter estimates and performance statistics. For example, with 100,000 instances, both an 80% training set (n=80,000) and a 20% validation set (n=20,000) provide substantial samples for modeling and evaluation [30].
Scenarios Favoring Split-Sample Approaches in Large-Scale Research
Computational Efficiency: For complex models requiring extensive training time, a single train-validation split is computationally more efficient than resampling methods like bootstrapping or repeated cross-validation [33].
Methodological Comparisons: When comparing multiple modeling approaches, a fixed validation set provides a consistent benchmark unaffected by resampling variability [34].
Preliminary Model Screening: In early development phases with abundant data, split-sample methods can rapidly eliminate poorly performing models before more rigorous validation [29].
Educational Contexts: The conceptual simplicity of split-sample validation makes it useful for teaching fundamental validation concepts before introducing more complex methods [10].
Table 1: Comparative Performance of Validation Methods Across Dataset Sizes
| Method | Small Datasets (n < 500) | Medium Datasets (n = 500-20,000) | Large Datasets (n > 20,000) |
|---|---|---|---|
| Split-Sample | High variance, pessimistic bias | Moderate variance, often pessimistic | Lower variance, minimal bias |
| Cross-Validation | Moderate variance, some optimism | Lower variance, slight optimism | Low variance, minimal optimism |
| Bootstrap | Lower variance, slight optimism | Lowest variance, minimal optimism | Stable, minimal bias |
| Recommended | Bootstrap or repeated cross-validation | Bootstrap | All methods potentially adequate |
Limitations and Methodological Concerns
Fundamental Statistical Limitations
Despite its intuitive appeal, split-sample validation suffers from several statistical limitations that persist even in large datasets:
Inefficient Data Usage: By reserving a portion of data exclusively for validation, the model is developed on less than the full dataset, potentially resulting in a suboptimal model [1] [31].
Evaluation Variance: Unless the validation set is very large, performance estimates will have high variance, making precise assessment difficult [33] [34].
Single Validation: A single train-validation split provides only one estimate of performance, whereas resampling methods generate multiple estimates and better characterize variability [31].
Process vs. Model Validation: When feature selection or other adaptive modeling procedures are used, split-sample validation evaluates only one realization of the modeling process, not the process itself [31].
The Instability of Single Splits
Research has consistently demonstrated that different random splits of the same dataset can yield substantially different validation results, particularly when sample sizes are modest [31] [33]. This instability reflects the inherent variability of single data partitions and underscores the limitation of split-sample approaches for reliable performance estimation.
As demonstrated in a comprehensive comparative study, the disparity between validation set performance and true generalization performance decreases with larger sample sizes, but significant gaps persist across all data splitting methods with small datasets [34].
Table 2: Comparative Study of Data Splitting Methods (Adapted from [34])
| Splitting Method | Bias in Performance Estimate | Variance of Estimate | Stability Across Samples | Recommended Minimum n |
|---|---|---|---|---|
| Split-Sample (70/30) | High (pessimistic) | High | Low | 20,000 |
| 10-Fold Cross-Validation | Moderate | Moderate | Moderate | 500 |
| Bootstrap | Low | Low | High | 100 |
| Stratified Split-Sample | Moderate | Moderate | Moderate | 5,000 |
| Repeated Cross-Validation | Low | Low | High | 1,000 |
Experimental Protocols and Implementation
Protocol for Split-Sample Validation in Large Datasets
For researchers implementing split-sample validation in large-scale studies, the following protocol provides a methodological framework:
Sample Size Assessment: Confirm dataset size sufficient for splitting (minimum 20,000 cases, preferably more) [31] [32].
Stratified Randomization: Implement stratified sampling to preserve distribution of key categorical variables (e.g., outcome classes, important predictors) across splits [35].
Ratio Selection: Choose split ratio based on modeling complexity and computational requirements; common ratios include:
- 80:20 for standard applications
- 90:10 when model complexity demands more training data
- 50:50 when validation precision is paramount [30]
Single Model Development: Train model on designated training partition without reference to validation data.
Performance Assessment: Evaluate model on validation partition using pre-specified metrics (discrimination, calibration, clinical utility).
Results Documentation: Report complete methodology including split ratio, stratification approach, and any potential limitations.
The Scientist's Toolkit: Essential Methodological Reagents
Table 3: Essential Methodological Components for Robust Validation
| Component | Function | Implementation Considerations |
|---|---|---|
| Stratified Sampling | Preserves distribution of important variables across splits | Particularly crucial for imbalanced datasets or rare outcomes |
| Performance Metrics | Quantifies model discrimination, calibration, and clinical utility | Should include C-statistic, calibration plots, and decision-curve analysis [28] |
| Sample Size Calculation | Determines adequate validation set size | Minimum 100-200 events for validation samples; precision-based approaches preferred [32] |
| Statistical Software | Implements complex sampling and validation procedures | R, Python, or specialized packages with robust sampling capabilities |
| Documentation Framework | Ensures complete methodological reporting | TRIPOD guidelines recommend detailed description of validation approach [10] |
Alternative Validation Methodologies
Superior Approaches for Most Research Settings
For the majority of research scenarios, particularly with small to moderate-sized datasets, alternative validation methods offer superior performance:
Bootstrap Validation: Involves sampling with replacement to create multiple training sets, with validation on out-of-sample cases. Demonstrates low bias and high stability, making it the preferred approach for most applications [1] [32].
Cross-Validation: Particularly k-fold cross-validation, which partitions data into k subsets, using each in turn as validation data. More efficient than split-sample for model development and performance estimation [10] [28].
Internal-External Cross-Validation: A hybrid approach that cycles through natural data partitions (e.g., different clinical sites, time periods), providing insights into both internal and external validity [1].
Decision Framework: Selecting Appropriate Validation Methods
The choice of validation strategy should be guided by dataset characteristics, research objectives, and practical constraints:
- Small datasets (n < 1,000): Bootstrap methods strongly preferred
- Moderate datasets (n = 1,000-20,000): Cross-validation or bootstrapping
- Very large datasets (n > 20,000): Split-sample may be adequate, but bootstrapping still preferred for efficiency
- Assessing generalizability: True external validation required regardless of sample size [10]
Within the broader context of internal versus external validation research, split-sample validation represents a method with limited but specific applications. Its appropriate use is restricted to very large datasets where both training and validation subsets can be sufficiently large to support stable development and evaluation. Even in these scenarios, resampling methods like bootstrapping generally provide more efficient data usage and more stable performance estimates.
For researchers and drug development professionals, understanding the limitations of split-sample validation is essential for methodological rigor. While its conceptual simplicity maintains appeal, more sophisticated validation approaches typically offer superior statistical properties for model development and evaluation. The ongoing challenge in validation research remains balancing methodological sophistication with practical implementation across diverse research contexts and dataset characteristics.
Within the broader thesis of prediction model research, the journey from model development to clinical utility hinges on a critical distinction: internal validation assesses model performance on data held out from the original development dataset, while external validation evaluates whether a model's performance generalizes to entirely new patient populations, settings, or time periods [36]. Internal validation techniques, such as bootstrapping or cross-validation, are essential first steps for mitigating over-optimism. However, they are insufficient for establishing a model's real-world applicability, as they cannot fully account for spectrum, geographic, or temporal biases [4] [36].
This guide focuses on two pivotal pillars of external validation—temporal and geographical generalizability. Temporal validation tests a model's performance on subsequent patients from the same institution(s) over time, probing its resilience to evolving clinical practices [37]. Geographic validation assesses its transportability to new hospitals or regions, testing its robustness to variations in patient demographics, clinician behavior, and healthcare systems [36] [37]. For researchers and drug development professionals, rigorously establishing these forms of generalizability is not merely an academic exercise; it is a fundamental prerequisite for regulatory acceptance, clinical adoption, and ultimately, improving patient outcomes with reliable, data-driven tools.
Core Methodological Frameworks
Defining Temporal and Geographic Validation
A clear operational understanding of these validation types is the foundation of a robust framework.
Temporal Validation involves applying the developed model, with its original structure and coefficients, to a cohort of patients treated at the same institution(s) as the development cohort but during a later, distinct time period [37]. For instance, a model developed on data from 2017-2020 would be tested on data from 2020-2022 from the same health system [37]. This approach evaluates the model's stability against natural temporal shifts, such as changes in treatment guidelines, surgical techniques, or ancillary care.
Geographic (Spatial) Validation involves testing the model on a patient population from one or more institutions that were not involved in the model's development and are located in a different geographic area [36] [37]. This is a stronger test of generalizability, as it assesses performance across potential differences in ethnic backgrounds, regional environmental factors, local clinical protocols, and healthcare delivery models.
Table 1: Key Characteristics of External Validation Types
| Validation Type | Core Question | Population Characteristics | Key Challenge Assessed |
|---|---|---|---|
| Temporal | Does the model remain accurate over time at our site? | Same institution(s), different time period | Evolution of clinical practice and technology [37] |
| Geographic | Does the model work at a new, unrelated site? | Different institution(s), different location | Variations in patient case-mix and local standards of care [36] [37] |
Experimental Protocol for External Validation
Implementing a rigorous external validation study requires a structured, step-by-step protocol. The following workflow outlines the critical stages, from planning to interpretation.
Phase 1: Define Validation Scope and Secure Data Clearly specify the type of validation (temporal, geographic, or both) and confirm that the external dataset meets the original model's inclusion and exclusion criteria [37]. Establish a data extraction and harmonization plan, using shared code (e.g., SQL) where possible to ensure variable definitions are consistent across sites [37].
Phase 2: Acquire and Prepare the External Dataset Extract the necessary predictor variables and outcome data from the new cohort. Critically, the model's original coefficients must be applied to this new data; no retraining is allowed [37]. Handle missing data according to a pre-specified plan, which may include exclusion or multiple imputation for variables with low missingness [38].
Phase 3: Apply the Original Model Using the locked-down algorithm and coefficients, calculate the predicted probabilities of the outcome for every patient in the new validation cohort [37].
Phase 4: Calculate Performance Metrics Comprehensively evaluate the model's performance using a suite of metrics that assess different aspects of validity [38] [37]:
- Discrimination: The ability to distinguish between those who do and do not experience the outcome. Measured by the C-index (or AUC) [13] [37].
- Calibration: The agreement between predicted probabilities and observed outcomes. Assessed with calibration plots, intercept, and slope [38] [37]. A slope of 1 and intercept of 0 indicate perfect calibration.
- Overall Accuracy: The mean squared difference between predicted and actual outcomes. Measured by the Brier score (lower is better) [37].
Phase 5: Analyze and Interpret Results Interpret the metrics in tandem. A model may have good discrimination but poor calibration, which could be corrected before clinical use. Compare the performance in the external cohort to its performance in the internal validation to quantify any degradation [36] [37].
Quantitative Performance Benchmarks and Analysis
Translating model outputs into actionable insights requires a standardized quantitative assessment. The following table synthesizes performance metrics from recent, real-world validation studies across medical specialties.
Table 2: External Validation Performance Metrics from Recent Studies
| Clinical Context (Model) | Validation Type | Sample Size (n) | Outcome Rate | C-Index / AUC | Calibration Assessment |
|---|---|---|---|---|---|
| Cervical Cancer OS Prediction [13] | Geographic | 318 | Not Specified | 0.872 | 3-, 5-, 10-yr AUC: 0.892, 0.896, 0.903 |
| Reintubation after Cardiac Surgery [37] | Temporal | 1,642 | 4.8% | 0.77 | Brier Score: 0.044 |
| Reintubation after Cardiac Surgery [37] | Geographic | 2,489 | 1.6% | 0.71 | Brier Score: 0.015 |
| Early-Stage Lung Cancer Recurrence [2] | Geographic | 252 | 6.3% | Not Specified | Hazard Ratio for DFS: 3.34 (Stage I) |
| Acute Leukemia Complications [38] | Geographic | 861 | 27% (Est.) | 0.801 | Calibration slope: 0.97, intercept: -0.03 |
Advanced Applications and Case Studies
Integrated Framework for Multi-Center Data
When data from multiple centers across different time periods are available, a meta-analytic approach can provide a powerful and nuanced assessment of a model's geographic and temporal transportability [36]. This method involves treating each hospital as a distinct validation cohort.
The process involves using a "leave-one-hospital-out" approach, where the model is developed on all but one hospital and then validated on the left-out hospital. This is repeated for every hospital in the dataset. The hospital-specific performance estimates (e.g., C-statistics, calibration slopes) are then pooled using random-effects meta-analysis [36]. This provides an overall estimate of performance and, crucially, quantifies the between-hospital heterogeneity via I² statistics and prediction intervals. A wide prediction interval for the C-statistic indicates that model performance is highly variable across different geographic locations and may not be reliably transportable [36].
Case Study: AI for Lung Cancer Recurrence
A machine learning model using preoperative CT radiomics and clinical data to predict recurrence in early-stage lung cancer underwent rigorous external validation. While the model demonstrated strong performance in internal validation, its true test was on an external cohort of 252 patients from a different medical center [2].
The validation confirmed the model's geographic generalizability, showing it outperformed conventional TNM staging in stratifying high- and low-risk patients, with a Hazard Ratio for disease-free survival of 3.34 in the external cohort versus 1.98 for tumor-size-based staging [2]. Furthermore, to build clinical trust and provide biological plausibility, the investigators validated the model's risk scores against established pathologic risk factors. They found significantly higher AI-derived risk scores in tumors with poor differentiation, lymphovascular invasion, and pleural invasion, bridging the gap between the AI's "black box" and known cancer biology [2].
The Scientist's Toolkit: Essential Reagents & Materials
Successful execution of external validation studies relies on a foundation of specific methodological and computational tools.
Table 3: Key Reagents and Solutions for Validation Research
| Tool / Resource | Category | Function in Validation | Exemplar Use Case |
|---|---|---|---|
| R / Python Software | Computational Platform | Statistical analysis, model application, and metric calculation. | R with rms, pROC, caret packages used for validation of a clinical prediction model [37]. |
| SQL Code | Data Protocol | Ensures consistent and homogeneous data extraction across different institutions. | Shared SQL queries used to extract EHR data from Epic systems at three academic medical centers [37]. |
| TRIPOD-AI / PROBAST-AI | Methodological Guideline | Provides a structured checklist for reporting and minimizing bias in prediction model studies. | Used to guide the evaluation of a machine learning model for acute leukemia complications [38]. |
| Cloud-Based LIMS | Data Infrastructure | Enables secure, real-time data sharing and collaboration across global sites for federated analysis. | Facilitates multi-center validation studies while maintaining data privacy and security [39]. |
| SHAP (SHapley Additive exPlanations) | Interpretability Tool | Explains the output of complex machine learning models, increasing clinician trust and interpretability. | Used to provide interpretable insights into the top predictors of complications in an acute leukemia model [38]. |
Predicting rare events represents one of the most formidable challenges in computational epidemiology and public health informatics. Suicide risk prediction exemplifies this challenge, requiring sophisticated methodological approaches to address extreme class imbalance and ensure model generalizability. This technical guide examines validation methodologies within the context of suicide risk modeling, framing the discussion within the broader research thesis contrasting internal validation with external validation practices. The fundamental challenge in this domain stems from the low incidence rate of suicide, even among high-risk populations, which creates substantial methodological hurdles for model development and validation [40]. Despite these challenges, the growing number of prediction models for self-harm and suicide underscores the field's recognition of their potential role in clinical decision-making across all stages of patient care [41].
The validation paradigm for rare-event prediction models must address multiple dimensions of performance assessment. Discrimination (a model's ability to distinguish between cases and non-cases) and calibration (the accuracy of absolute risk estimates) represent distinct aspects of predictive performance that require rigorous evaluation across different populations and settings [41]. This case study explores the current state of validation practices in suicide risk prediction, identifies persistent methodological gaps, and provides detailed protocols for comprehensive model validation that bridges the internal-external validation divide.
Current Landscape of Suicide Risk Prediction Models
Model Types and Methodological Approaches
Suicide risk prediction models employ diverse methodological approaches, ranging from traditional statistical models to advanced machine learning techniques. The field has witnessed substantial growth in both model complexity and application scope, with recent systematic reviews identifying 91 articles describing the development of 167 distinct models alongside 29 external validations [41]. These models predict various outcomes across the suicide risk spectrum, including non-fatal self-harm (76 models), suicide death (51 models), and composite outcomes (40 models) that combine fatal and non-fatal events [41].
Machine learning approaches have demonstrated particular promise in adolescent populations, where ensemble methods like random forest and extreme gradient boosting have shown superior performance across multiple outcome types [40]. The predictive performance across different suicide-related behaviors varies substantially, with meta-analyses indicating the highest accuracy for suicide attempt prediction (combined AUC 0.84) compared to non-suicidal self-injury (combined AUC 0.79) or suicidal ideation (combined AUC 0.77) [40]. This performance pattern highlights the differential predictability across the spectrum of suicide-related behaviors and underscores the need for outcome-specific validation approaches.
Quantitative Performance Assessment
Table 1: Reported Performance Metrics of Suicide Prediction Models
| Model Characteristic | Development Studies | External Validation Studies |
|---|---|---|
| Discrimination (C-index range) | 0.61 - 0.97 (median 0.82) | 0.60 - 0.86 (median 0.81) |
| Calibration assessment rate | 9% (15/167 models) | 31% (9/29 validations) |
| External validation rate | 8% (14/167 models) | - |
| Model presentation clarity | 17% (28/167 models) | - |
Source: Adapted from systematic review data [41]
The performance metrics in Table 1 reveal several critical patterns. First, the narrow range of C-indices in external validation studies (0.60-0.86) compared to development studies (0.61-0.97) suggests optimism bias in internally-reported performance [41]. Second, the inadequate assessment of calibration in most studies (only 9% in development) represents a significant methodological shortcoming, as clinical utility depends on accurate absolute risk estimates, not just ranking ability. Third, the low rate of external validation (8%) highlights a critical translational gap between model development and real-world implementation.
Methodological Challenges in Rare-Event Prediction
Statistical and Computational Constraints
Rare event prediction introduces unique methodological challenges that conventional predictive modeling approaches often inadequately address. The extreme class imbalance characteristic of suicide outcomes (typically <5% prevalence) fundamentally impacts model training, performance assessment, and clinical applicability [40]. From a statistical perspective, low event rates dramatically reduce the effective sample size for model development, increasing vulnerability to overfitting and requiring specialized techniques for reliable estimation.
Computational sampling methods developed for reliability engineering offer promising analogies for addressing these challenges. Techniques like Subset Adaptive Importance Sampling (SAIS) iteratively refine proposal distributions using weighted samples from previous stages to efficiently explore complex, high-dimensional failure regions [42]. Similarly, normalizing Flow enhanced Rare Event Sampler (FlowRES) leverages physics-informed machine learning to generate high-quality non-local Monte Carlo proposals without requiring prior data or predefined collective variables [43]. These advanced sampling methodologies maintain efficiency even as events become increasingly rare, addressing a fundamental limitation of conventional approaches.
Methodological Quality and Risk of Bias
Current suicide prediction models exhibit substantial methodological limitations that compromise their validity and potential clinical utility. Systematic assessment using the Prediction model Risk Of Bias ASsessment Tool (PROBAST) indicates that all model development studies and nearly all external validations (96%) were at high risk of bias [41]. The predominant sources of bias include:
- Inappropriate evaluation of predictive performance (92% of studies)
- Insufficient sample sizes (77% of studies)
- Inappropriate handling of missing data (66% of studies)
- Inadequate accounting for overfitting and optimism (63% of development studies)
These methodological shortcomings represent avoidable sources of research waste and underscore the need for enhanced methodological rigor in rare-event prediction research.
Validation Methodologies: Protocols and Implementation
Internal Validation Techniques
Internal validation provides the foundational assessment of model performance using data available during model development. The following protocols represent minimum standards for internal validation of rare-event prediction models:
1. K-Fold Cross-Validation with Stratification
- Partition dataset into K folds (typically K=5 or K=10) while preserving outcome distribution in each fold
- Train model on K-1 folds, validate on the held-out fold
- Repeat process K times with different validation folds
- Aggregate performance metrics across all iterations
- For rare events, employ stratified sampling to ensure adequate event representation in each fold
2. Bootstrap Resampling and Optimism Correction
- Generate multiple bootstrap samples (typically 100-200) by random sampling with replacement
- Fit model to each bootstrap sample and calculate performance metrics
- Evaluate performance on original dataset
- Estimate optimism as average difference between bootstrap and original performance
- Apply optimism correction to original performance estimates
3. Repeated Hold-Out Validation
- Randomly split data into development and validation sets (typically 70:30 or 80:20)
- Repeat process multiple times (typically 50-100 iterations) with different random splits
- Report performance distribution across all iterations
- Particularly valuable for assessing stability of rare-event predictions
Table 2: Internal Validation Techniques for Rare-Event Prediction
| Technique | Key Implementation Considerations | Strengths | Limitations |
|---|---|---|---|
| Stratified K-Fold Cross-Validation | Ensure minimum event count per fold; balance computational efficiency with variance reduction | Maximizes data usage; provides variance estimates | May underestimate performance drop in external validation |
| Bootstrap Optimism Correction | Use 200+ bootstrap samples; apply .632 correction for extreme imbalance | Directly estimates optimism; works well with small samples | Computationally intensive; may overcorrect with severe overfitting |
| Repeated Hold-Out Validation | Maintain class proportion in splits; sufficient repetitions for stable estimates | Mimics external validation process; computationally efficient | Higher variance than bootstrap; depends on split ratio |
External Validation Frameworks
External validation represents the critical step in assessing model transportability and real-world performance. The following protocol outlines a comprehensive approach for external validation of suicide risk prediction models:
Protocol: Stepwise External Validation Framework
Step 1: Validation Cohort Specification
- Define inclusion/exclusion criteria mirroring intended use population
- Ensure adequate sample size to detect clinically relevant performance differences
- For rare events, calculate minimum sample size using Riley's criteria (minimum of 100 events and 100 non-events)
- Document key cohort characteristics: demographic composition, clinical features, setting, temporal factors
Step 2: Model Implementation and Harmonization
- Obtain complete model specification (predictors, functional form, coefficients)
- Harmonize predictor definitions between development and validation cohorts
- Address missing data using prespecified methods (complete-case analysis considered inadequate)
- Implement appropriate model adjustments if needed (intercept update, predictor recalibration)
Step 3: Performance Assessment
- Calculate discrimination metrics (C-statistic, ROC analysis) with confidence intervals
- Assess calibration using calibration plots, calibration-in-the-large, and calibration slope
- Evaluate clinical utility via decision curve analysis and clinical impact curves
- Conduct subgroup analyses to assess performance heterogeneity
Step 4: Comparison with Existing Standards
- Benchmark performance against established models in same population
- Compare with simple clinical heuristics or default strategies
- Assess incremental value beyond established predictors
The systematic review by PMC identified only two models (OxMIS and Simon) that demonstrated adequate discrimination and calibration performance in external validation, highlighting the critical need for more rigorous external validation practices [41].
Advanced Sampling Techniques for Rare Events
The following experimental protocol adapts advanced sampling methodologies from reliability engineering to suicide risk prediction:
Protocol: Subset Adaptive Importance Sampling (SAIS) for Rare Events
Theoretical Foundation SAIS combines subset simulation with adaptive importance sampling, iteratively refining proposal distributions using weighted samples from previous stages to efficiently explore complex failure regions [42]. This approach addresses key limitations of conventional methods that often converge to single local failure modes in multi-failure region problems.
Implementation Steps
- Initialization: Define limit state function S(x) representing the rare event threshold
- Subset Generation: Create nested sequence of intermediate failure regions F₁ ⊃ F₂ ⊃ ... ⊃ F_m = F
- Adaptive Proposal Update: At each subset level k, update proposal distributions using weighted samples from previous stages
- Gradual Covariance Shrinkage: Implement dimension-adapted covariance estimation to maintain exploration in high-dimensional spaces
- Recycling Estimator: Reuse all past samples to improve failure probability estimates with minimal additional computational cost
Computational Advantages
- Maintains sampling efficiency as events become increasingly rare
- Naturally balances exploration and exploitation in failure space
- Reduces weight degeneracy even with relatively small sample sizes
- Particularly valuable for capturing multiple failure modes in complex systems
Diagram 1: SAIS Algorithm Workflow - Subset Adaptive Importance Sampling process for rare event estimation
Performance Assessment and Metrics Interpretation
Comprehensive Metrics for Rare Events
Evaluating rare-event prediction models requires a multifaceted approach beyond conventional classification metrics. The following assessment framework addresses the unique characteristics of low-prevalence outcomes:
Discrimination Assessment
- C-statistic (AUC): Standard measure of ranking ability with threshold-invariant interpretation
- Sensitivity at Fixed Specificity: Particularly relevant for clinical applications with capacity constraints
- Precision-Recall Curves: More informative than ROC curves for imbalanced data
- Average Precision: Summary measure of precision-recall performance
Calibration Assessment
- Calibration Plots: Visual assessment of agreement between predicted and observed risks
- Calibration Slope: Ideal value of 1 indicates appropriate strength of predictor effects
- Calibration-in-the-large: Intercept assessment indicating systematic over/under-prediction
- Brier Score: Combined measure of discrimination and calibration
Clinical Utility Assessment
- Decision Curve Analysis: Net benefit across different probability thresholds
- Clinical Impact Curves: Visualization of true and false positives at population level
- Cost-Benefit Analysis: Quantitative assessment of tradeoffs incorporating clinical consequences
Performance Interpretation in Context
Interpreting model performance requires careful consideration of the clinical context and baseline risk. The reported C-indices for suicide prediction models (median 0.82 in development, 0.81 in validation) [41] must be evaluated against the practical requirements for clinical implementation. For context, a systematic review of machine learning models for adolescent suicide attempts reported sensitivity of 0.80 and specificity of 0.96 for the best-performing models [40], though these metrics are highly dependent on the chosen classification threshold.
The substantial heterogeneity in performance across different populations and settings underscores the necessity of local performance assessment before implementation. Performance metrics should always be reported with confidence intervals to communicate estimation uncertainty, particularly given the limited sample sizes typical in rare-event prediction.
Implementation Framework and Research Reagents
Research Reagent Solutions
Table 3: Essential Methodological Reagents for Rare-Event Prediction Research
| Reagent Category | Specific Tools | Function and Application |
|---|---|---|
| Statistical Software Platforms | R (predtools, riskRegression), Python (scikit-survival, imbalanced-learn) | Implementation of specialized algorithms for rare-event analysis and validation |
| Bias Assessment Tools | PROBAST (Prediction model Risk Of Bias ASsessment Tool) | Standardized assessment of methodological quality in prediction model studies |
| Sampling Methodologies | Subset Adaptive Importance Sampling (SAIS), FlowRES | Advanced techniques for efficient exploration of rare event spaces |
| Validation Frameworks | TRIPOD (Transparent Reporting of multivariable prediction models), CHARMS (CHecklist for critical Appraisal and data extraction for systematic Reviews of prediction Modelling Studies) | Reporting guidelines and methodological standards for prediction model research |
| Performance Assessment Packages | R (pROC, PRROC, givitiR), Python (yellowbrick, scikit-plot) | Comprehensive evaluation of discrimination, calibration, and clinical utility |
Integrated Validation Workflow
Diagram 2: Validation Workflow - Comprehensive validation pathway from development to implementation
This technical guide has examined the critical role of comprehensive validation in rare-event prediction models, using suicide risk prediction as a case study. The fundamental tension between internal and external validation paradigms reflects broader challenges in translational predictive modeling. While internal validation provides essential preliminary performance assessment, external validation remains the definitive test of model transportability and real-world utility.
The evidence indicates substantial methodological shortcomings in current practices, with only 8% of developed models undergoing external validation and widespread risk of bias in both development and validation studies [41]. Addressing these limitations requires concerted effort across multiple domains: enhanced methodological rigor in model development, complete and transparent reporting, prioritization of external validation, and development of specialized techniques for rare-event Scenarios.
Future research should focus on several critical pathways: (1) developing standardized frameworks for model updating and localization across diverse settings, (2) advancing sampling methodologies adapted from reliability engineering and statistical physics, (3) establishing minimum reporting standards for rare-event prediction studies, and (4) implementing model impact assessment within prospective clinical studies. Only through such comprehensive approaches can suicide risk prediction models fulfill their potential to inform clinical decision-making and ultimately contribute to suicide prevention efforts.
In the rigorous landscape of clinical research, validation represents the critical process of confirming that a predictive model, diagnostic tool, or intervention performs as intended. This process exists on a spectrum of evidence quality, ranging from initial internal checks to the most robust external assessments. Prospective evaluation sits at the pinnacle of this hierarchy, providing the most compelling evidence for real-world clinical utility. Unlike retrospective analyses that examine historical data, prospective evaluation involves applying a model or intervention to new participants in a real-time, planned experiment and measuring outcomes as they occur [44] [2]. This methodology is indispensable for confirming that promising early results will translate into genuine clinical benefits, thereby bridging the gap between theoretical development and practical application.
The journey from initial concept to clinically adopted tool typically traverses two main phases: internal and external validation. Internal validation assesses how well a model performs on the same dataset from which it was built, using techniques like cross-validation to estimate performance. While useful for initial model tuning, it provides no guarantee of performance on new populations. External validation, by contrast, tests the model on completely independent data collected from different sites, populations, or time periods [13] [2]. Prospective evaluation represents the most rigorous form of external validation, as it not only uses independent data but does so in a forward-looking manner that mirrors actual clinical use. This distinction is crucial for drug development professionals and researchers who must make high-stakes decisions about which technologies to advance into clinical practice.
Methodological Framework for Prospective Evaluation
Core Principles and Study Designs
The fundamental principle of prospective evaluation is its forward-looking nature; it tests a predefined hypothesis on new participants according to a pre-specified analysis plan [44]. This design minimizes several biases inherent in retrospective studies, such as data dredging and overfitting. The core components of a robust prospective evaluation include:
- Pre-registered Protocol: A detailed study protocol specifying objectives, endpoints, statistical analysis plan, and sample size calculation should be finalized before participant enrollment begins. The SPIRIT 2025 statement provides a comprehensive 34-item checklist for designing robust trial protocols that ensure completeness and transparency [45].
- Blinded Outcome Assessment: Whenever possible, researchers assessing outcomes should be blinded to the model's predictions or group assignments to prevent measurement bias.
- Standardized Procedures: All data collection and intervention procedures must follow standardized operating procedures to ensure consistency across sites and time.
- Predefined Success Criteria: The thresholds for deeming the evaluation successful must be established before data collection begins, not after results are known.
For prospective evaluation of artificial intelligence tools in healthcare, the requirement for rigor is particularly high. As noted in discussions of AI in drug development, AI-powered solutions "promising clinical benefit must meet the same evidence standards as therapeutic interventions they aim to enhance or replace" [46]. This often means that randomized controlled trials (RCTs) represent the ideal design for prospective evaluation of impactful AI systems. Adaptive trial designs that allow for continuous model updates while preserving statistical rigor offer a viable approach for evaluating rapidly evolving technologies [46].
Quantitative Frameworks for Evaluation
Prospective evaluations should employ robust statistical frameworks to quantify model performance. Key metrics include:
- Discriminative Performance: Measured using the concordance index (C-index) for time-to-event data, or area under the receiver operating characteristic curve (AUC) for binary outcomes.
- Calibration: Assessment of how well predicted probabilities match observed event rates, often visualized using calibration plots.
- Clinical Utility: Evaluation of how the model impacts decision-making and patient outcomes, which can be assessed using decision curve analysis.
Table 1: Key Statistical Measures for Prospective Validation
| Metric | Interpretation | Ideal Value | Application Example |
|---|---|---|---|
| C-index | Concordance between predictions and outcomes | >0.7 (acceptable); >0.8 (good) | Survival model validation [13] [2] |
| Mean Absolute Error (MAE) | Average absolute difference between predicted and observed values | Closer to 0 is better | Workload prediction models [44] |
| Hazard Ratio (HR) | Ratio of hazard rates between groups | Statistical significance (p<0.05) with CI excluding 1.0 | Risk stratification models [2] |
Case Studies in Prospective Clinical Validation
Validating a Workload Prediction Model in Clinical Trials
A recent prospective observational study conducted over 12 months at a Historically Black College and University medical school exemplifies rigorous prospective evaluation [44]. The study aimed to validate an adapted Ontario Protocol Assessment Level (OPAL) score for predicting research coordinator workload across seven actively enrolling interventional trials.
The experimental protocol required seven coordinators to prospectively log hours worked on each trial using a standardized digital time-tracking system. Data were reconciled weekly to ensure completeness and accuracy. Estimated workload hours were derived using a published adapted OPAL reference table and compared against actual logged hours.
Key quantitative results demonstrated no statistically significant difference between estimated and actual hours, with an average difference of 24.1 hours (p=0.761) [44]. However, the mean absolute error was 167.0 hours, equivalent to approximately one month of full-time work, highlighting that while the model was unbiased on average, individual trial predictions could vary substantially.
Table 2: Prospective Validation of OPAL Workload Prediction Model
| Trial Number | Adapted OPAL Score | Trial Phase | Sponsor Type | Estimated Hours | Actual Hours | Difference | |
|---|---|---|---|---|---|---|---|
| 1 | 7.5 | 3 | Industry | 370.2 | 538 | 167.8 | |
| 2 | 6.5 | 3 | Industry | 370.2 | 492 | 121.8 | |
| 3 | 7.0 | 2/3 | Industry | 293.0 | 438 | 145.0 | |
| 4 | 9.5 | 3 | Industry | 679.2 | 310 | -369.2 | |
| 5 | 6.5 | 3 | Federal | Behavioral | 215.8 | 330 | 114.2 |
| 6 | 6.5 | 3 | Industry | Drug | 215.8 | 336 | 120.2 |
| 7 | 7.0 | 2 | Federal | Drug | 293.0 | 162 | -131.0 |
Subgroup analysis revealed that industry-sponsored trials required more coordinator time (average 422.8 hours) than federally funded trials (average 246.0 hours), a difference approaching statistical significance (p=0.095) [44]. This finding underscores how prospective evaluation can identify factors influencing real-world performance that might not be apparent from retrospective analysis.
External Validation of an AI Model for Lung Cancer Recurrence
A compelling example of external prospective validation in oncology comes from a study presented at the European Society for Medical Oncology Congress 2025 [2]. The research involved external validation of a machine learning-based survival model that incorporated preoperative CT images and clinical data to predict recurrence risk after surgery in patients with early-stage lung cancer.
The methodological protocol involved analyzing CT scans and clinical data from 1,267 patients with clinical stage I-IIIA lung cancer who underwent surgical resection. The model was trained on 1,015 patients from the U.S. National Lung Screening Trial, with internal validation on 725 patients and external validation on 252 patients from the North Estonia Medical Centre Foundation [2]. This multi-source design strengthened the generalizability of the findings.
Key performance results demonstrated the model's superiority over conventional staging systems. For stratifying patients with stage I lung cancer into high- and low-risk groups, the model achieved hazard ratios of 1.71 (internal) and 3.34 (external) compared to 1.22 and 1.98 for conventional tumor size-based staging [2]. The model also showed significant correlations with established pathologic risk factors, including tumor differentiation, lymphovascular invasion, and pleural invasion (p<0.0001 for all).
An invited expert commentary highlighted the importance of the study's "very good" methodology, including "development, internal validation, and external validation—what we wanted to see," while noting the potential for further enhancement through integration with circulating tumor DNA analysis [2]. This case illustrates how prospective external validation provides the most credible evidence for clinical adoption of AI technologies.
Experimental Protocols for Prospective Validation
General Workflow for Prospective Model Validation
The following diagram illustrates the standardized workflow for conducting prospective validation of clinical prediction models:
Relationship Between Validation Types
The pathway from model development to clinical implementation involves multiple validation stages, as illustrated below:
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents and Materials for Prospective Validation Studies
| Item Category | Specific Examples | Function in Prospective Evaluation |
|---|---|---|
| Data Collection Tools | Electronic data capture (EDC) systems, REDCap, Electronic Case Report Forms (eCRFs) | Standardized collection of clinical, demographic, and outcome data across sites [44] |
| Biomarker Assays | Immunohistochemistry kits, PCR reagents, ELISA assays, genomic sequencing panels | Objective measurement of molecular endpoints and validation of predictive biomarkers [2] |
| Imaging Acquisition | CT scanners, MRI machines, standardized imaging protocols | Acquisition of reproducible radiographic data for image-based models [2] |
| Statistical Software | R, Python, SAS, SPSS | Implementation of pre-specified statistical analysis plans and performance metrics [13] |
| Sample Collection Kits | Blood collection tubes, tissue preservation solutions, DNA/RNA stabilization reagents | Standardized biospecimen acquisition for correlative studies [44] |
| Protocol Templates | SPIRIT 2025 checklist, ICH Good Clinical Practice guidelines | Ensuring comprehensive study design and regulatory compliance [45] |
Prospective evaluation represents the definitive standard for establishing the clinical utility of predictive models, interventions, and technologies. Through its forward-looking design and application in real-world clinical settings, it provides evidence of the highest quality for guiding implementation decisions. The case studies presented demonstrate that while internal validation provides necessary preliminary evidence, and external validation offers greater generalizability, only prospective evaluation can truly confirm that a tool will perform as expected in actual clinical practice.
For researchers and drug development professionals, embracing prospective evaluation requires a commitment to methodological rigor, transparent reporting, and adherence to standardized protocols like the SPIRIT 2025 statement [45]. This approach is particularly crucial for emerging technologies like AI in healthcare, where the validation gap between technical development and clinical implementation remains substantial [46]. By systematically implementing prospective validation strategies, the research community can accelerate the translation of promising innovations into tools that genuinely improve patient care and outcomes.
The integration of artificial intelligence (AI) and machine learning (ML) into medical devices and drug development represents a transformative shift in healthcare, capable of deriving critical insights from vast datasets generated during patient care [47]. Unlike traditional software, AI/ML technologies possess the unique ability to learn from real-world use and experience, potentially improving their performance over time [47]. This very adaptability, however, introduces novel regulatory challenges that existing frameworks were not originally designed to address.
Global regulatory bodies, including the U.S. Food and Drug Administration (FDA), have responded with evolving guidance to ensure safety and efficacy while fostering innovation. The FDA's traditional paradigm of medical device regulation was not designed for adaptive AI and ML technologies, necessitating new approaches [47]. In January 2025, the FDA released a draft guidance titled "Artificial Intelligence-Enabled Device Software Functions: Lifecycle Management and Marketing Submission Recommendations," which provides a comprehensive roadmap for manufacturers navigating the complexities of AI-enabled medical device development and submission [48]. This guidance advocates for a Total Product Life Cycle (TPLC) approach to risk management, considering risks not just during design and development but throughout deployment and real-world use [48].
A critical aspect of these regulatory frameworks is the emphasis on robust validation strategies. The FDA's guidance clarifies the important distinction in terminology between the AI community and regulatory standards. For instance, in AI development, "validation" often refers to data curation or model tuning during training, whereas the regulatory definition of validation refers to "confirming – through objective evidence – that the final device consistently fulfills its specified intended use" [48]. This semantic precision is essential for compliance and underscores the need for rigorous, evidence-based evaluation processes that demonstrate real-world performance and safety.
The Critical Distinction: Internal vs. External Validation
Within regulatory and scientific contexts, validation is not a monolithic process. It is categorized into internal and external validation, each serving distinct purposes in establishing an AI model's reliability and generalizability. This distinction forms the core of a robust evaluation strategy and is fundamental to meeting regulatory standards for AI-enabled technologies.
Internal validation refers to the process of evaluating a model's performance using data that was part of its development cycle, typically through techniques such as cross-validation on the training dataset [49]. While useful for model selection and tuning during development, internal validation provides insufficient evidence of real-world performance for regulatory submissions because it does not adequately assess how the model will perform on entirely new data from different sources.
External validation (also known as independent validation) is the evaluation of model performance using data collected from a separate source that was not used in the training or development process [8] [50]. This process is critical for assessing the model's generalizability—its ability to maintain performance across different patient populations, clinical settings, imaging equipment, and operational environments. A systematic scoping review of AI in pathology highlighted that a lack of robust external validation is a primary factor limiting clinical adoption, with only approximately 10% of developed models undergoing external validation [50].
The performance gap between internal and external validation can be significant. The following table summarizes quantitative findings from external validation studies across medical domains, illustrating this critical performance drop.
Table 1: Performance Comparison Between Internal and External Validation in Medical AI Studies
| Medical Domain | AI Model Task | Internal Validation Performance (AUROC) | External Validation Performance (AUROC) | Performance Gap | Source of External Data |
|---|---|---|---|---|---|
| Non-Cardiac Surgery | Postoperative Acute Kidney Injury Prediction | 0.868 | 0.757 | -0.111 | VitalDB Open Dataset [8] |
| Lung Cancer Pathology | Tumor Subtyping (Adeno. vs. Squamous) | Range: 0.85 - 0.999 (Various AUCs) | Range: 0.746 - 0.999 (Various AUCs) | Variable, often significant | Multiple Independent Medical Centers [50] |
| Lung Cancer Pathology | Classification of Malignant vs. Non-Malignant Tissue | High Performance (Specific metrics not aggregated) | Notable Performance Drop Reported | Consistent decrease | Multiple Independent Medical Centers [50] |
This empirically observed discrepancy underscores why regulators demand external validation. It provides a more realistic assessment of an AI model's safety and effectiveness in clinical practice, ensuring it does not fail when confronted with the inherent diversity and unpredictability of real-world healthcare environments.
Regulatory Requirements for AI Validation
Navigating the regulatory landscape for AI-enabled technologies requires a proactive approach to validation, aligned with specific guidelines and principles. The FDA's 2025 draft guidance and other international frameworks establish clear expectations for the evidence needed to support marketing submissions.
Foundational Principles and Pre-Submission Requirements
A cornerstone of the regulatory approach is the Total Product Life Cycle (TPLC) framework [48]. This means that risk management must extend beyond pre-market development to include post-market surveillance and proactive updates. Key areas of focus identified by the FDA include:
- Transparency: Regulated AI systems must provide critical information about their function in an understandable and accessible manner to users, mitigating the "black box" problem and building trust [48].
- Bias Control: Manufacturers must address bias throughout the life cycle, from data collection to post-market monitoring. This involves ensuring that development and test data reflect the intended use population and proactively identifying disparities across demographic groups [48].
- Managing Data Drift: Strategies for detecting and mitigating performance degradation due to shifts in input data over time are essential. The FDA recommends implementing performance monitoring plans and utilizing Predetermined Change Control Plans (PCCP), which allow for certain pre-approved software updates without requiring a new submission [48] [47].
For the marketing submission itself, manufacturers must provide comprehensive documentation, including a detailed device description, user interface and labeling, a thorough risk assessment per standards like ISO 14971, and a robust data management plan [48].
Technical and Data Management Requirements
Regulatory submissions for AI-enabled devices must include exhaustive documentation of the model's development and performance [48]:
- Data Management: Detailed documentation on data collection, processing, annotation, and storage is required. A key requirement is demonstrating independence between training and validation datasets. The data must be diverse and representative to support generalizable performance, with controls against data leakage [48].
- Model Development and Validation: Submissions must detail model architecture, input/output features, training processes, and performance metrics. Performance validation must use independent datasets, include subgroup analyses to check for bias, and assess repeatability and reproducibility. The FDA also encourages "human-AI team" performance evaluation, such as reader studies for diagnostic tools [48].
- Cybersecurity: Given unique threats like data poisoning and model inversion, robust cybersecurity risk assessments and controls tailored to AI components are mandatory [48].
The "nested model" for AI design and validation provides a structured protocol to ensure compliance, advocating for a multidisciplinary team—including AI experts, medical professionals, and legal counsel—to address issues at each layer from regulations to prediction [51].
Experimental Protocols for AI Model Validation
A systematic, protocol-driven approach is essential for conducting validation that meets regulatory scrutiny. The following sections detail methodologies for both internal and external validation.
Internal Validation Experimental Protocol
Internal validation techniques are primarily employed during the model development phase to guide feature selection and model architecture decisions.
Step-by-Step Methodology:
- Data Splitting: Split the available development dataset into training and testing sets. A classic 80/20 split is common, but k-fold cross-validation is often preferred for complex models or smaller datasets [49].
- Stratified Sampling: When splitting data, use stratified sampling to maintain the distribution of important classes (e.g., disease prevalence) in both the training and test sets. This prevents skewed performance estimates [49].
- K-Fold Cross-Validation: Partition the training data into 'k' equal-sized folds (e.g., k=5 or k=10). Iteratively train the model on k-1 folds and validate on the remaining fold. Repeat this process until each fold has been used once as the validation set. The final performance metric is the average across all k iterations [49].
- Hyperparameter Tuning: Use the cross-validation process to optimize model hyperparameters, selecting the values that yield the best average performance on the validation folds.
- Final Evaluation on Hold-Out Test Set: After model selection and tuning, perform a final performance assessment on the held-out test set that was not used in any part of the training or validation process. This provides a less biased estimate of model performance than the cross-validation score alone.
Key Considerations:
- Data Leakage: Rigorously check for information bleeding between training and validation sets, as this can lead to overly optimistic performance estimates and model failure in production [49].
- Statistical Significance: For imbalanced datasets, ensure the validation set is large enough to trust the conclusions about minority classes, potentially using power analysis [49].
External Validation Experimental Protocol
External validation is the definitive test of a model's generalizability and is a regulatory necessity.
Step-by-Step Methodology:
- Acquisition of External Dataset: Secure one or more completely independent datasets for validation. These datasets should be collected from different institutions, geographic locations, or patient populations than the development data. Utilizing publicly available open datasets (e.g., VitalDB) is a viable and practical strategy [8].
- Preprocessing Alignment: Apply the same preprocessing steps (e.g., normalization, image scaling, feature engineering) to the external dataset that were applied to the training data. It is critical that no statistics from the external dataset (e.g., mean, standard deviation) are used in this preprocessing to maintain independence.
- Blinded Performance Evaluation: Run the fully trained and locked model on the external dataset. The model must not be retrained or fine-tuned on any part of this external data.
- Comprehensive Performance Analysis: Calculate all relevant performance metrics (e.g., AUROC, Precision, Recall, F1-Score) on the external set. Crucially, conduct subgroup analyses to evaluate performance across different demographic groups (age, sex, race), clinical settings, and equipment types to identify potential biases and performance disparities [48] [50].
- Comparison to Internal Performance: Formally compare the performance metrics from the external validation to those from the internal validation. A statistically significant drop in performance, as measured by tests like the DeLong test for AUROC, indicates a lack of generalizability [8].
Key Considerations:
- Technical Diversity: The external dataset should reflect real-world variability, including images from different scanner models, staining protocols, and containing artifacts. Some studies simulate this diversity through data augmentation, while others explicitly collect multi-center data [50].
- Representativeness: The external validation population must be clinically relevant to the model's intended use [50].
The workflow and performance relationship between internal and external validation is summarized in the following diagram:
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of AI validation protocols requires a suite of methodological and computational tools. The following table details key "research reagents" and their functions in the validation process.
Table 2: Essential Research Reagents and Solutions for AI Validation
| Tool Category | Specific Tool/Technique | Primary Function in Validation | Key Considerations for Use |
|---|---|---|---|
| Data Management | Stratified Sampling | Ensures training and test sets maintain distribution of critical variables (e.g., disease prevalence). | Prevents biased performance estimates in imbalanced datasets. |
| K-Fold Cross-Validation | Maximizes data usage for robust internal performance estimation during model development. | Preferred for small datasets; provides mean and variance of performance. | |
| Performance Metrics | AUROC (Area Under the ROC Curve) | Measures model's ability to discriminate between classes across all classification thresholds. | Robust to class imbalance; does not reflect real-world class prevalence. |
| AUPRC (Area Under the Precision-Recall Curve) | Assesses performance on imbalanced datasets where the positive class is the focus. | More informative than AUROC when one class is rare. | |
| Precision, Recall, F1-Score | Provides granular view of classification performance, trade-offs between false positives/negatives. | Essential for evaluating models where error types have different costs. | |
| Bias & Explainability | SHAP (SHapley Additive exPlanations) | Interprets model predictions by quantifying the contribution of each feature. | Critical for identifying feature-driven biases and building trust. |
| Subgroup Analysis | Evaluates model performance across different demographic or clinical patient subgroups. | Mandatory for detecting performance disparities and ensuring fairness. | |
| Statistical Validation | DeLong Test | Statistically compares the difference between two AUROC curves. | Used to confirm if performance drop in external validation is significant. |
| Confidence Intervals | Quantifies the uncertainty around performance metrics (e.g., mean AUROC ± 95% CI). | Provides a range for expected real-world performance. | |
| Computational Frameworks | Python/R with scikit-learn, TensorFlow/PyTorch | Provides libraries for implementing data splitting, model training, and metric calculation. | Enables automation and reproducibility of the validation pipeline. |
| Specialized Software | Galileo LLM Studio, XAI Question Bank | Platforms for automated drift detection, performance dashboards, and structured explainability. | Helps tackle challenges like limited labeled data and black-box model interpretation [49] [51]. |
The regulatory pathway for AI-enabled technologies is firmly grounded in the principle of demonstrated safety and effectiveness throughout the total product life cycle. While internal validation remains a necessary step in model development, it is the rigorous, independent external validation that provides the definitive evidence required by regulators and demanded by clinical practice. The consistent observation of a performance gap between internal and external evaluations, as documented in systematic reviews and primary studies, underscores the non-negotiable nature of this process. Successfully navigating this landscape requires a multidisciplinary approach, integrating robust experimental protocols, comprehensive documentation, and a commitment to continuous monitoring and improvement. By adhering to these structured validation requirements, researchers and drug development professionals can ensure their AI-enabled technologies are not only innovative but also reliable, equitable, and ready for integration into the healthcare ecosystem.
Overcoming Challenges: Optimizing Validation in Complex Research Environments
Addressing Small Sample Sizes and Rare Events in Validation
The accurate validation of predictive models is a cornerstone of robust scientific research, particularly in fields like healthcare and drug development where outcomes can have significant consequences. This process is framed by two complementary paradigms: internal validation, which assesses a model's performance on data derived from the same source population, and external validation, which evaluates its generalizability to entirely independent populations or settings. However, a significant challenge arises when research focuses on rare events—defined as outcomes that occur infrequently within a specific population, geographic area, or time frame. Examples include certain types of cancer, early phases of emerging infectious diseases, or rare adverse drug reactions. Predicting these events is paramount for the early identification of high-risk individuals and facilitating targeted interventions, but the accompanying small sample sizes and imbalanced datasets introduce substantial methodological hurdles for both internal and external validation processes. These challenges can compromise model accuracy, introduce biases that favor non-event predictions, and ultimately limit the clinical utility and reliability of research findings [52].
The core of the problem lies in the fundamental tension between data scarcity and the statistical power required for trustworthy validation. During internal validation, limited data can lead to model overfitting and optimistic performance estimates, while for external validation, it raises serious questions about the model's stability and transportability. This whitepaper provides an in-depth technical guide to advanced strategies and methodologies designed to address these specific challenges, ensuring that validation research for rare events remains scientifically rigorous and clinically meaningful within the broader framework of internal versus external validation research.
Core Challenges in Rare Event and Small Sample Research
Research involving rare events is fraught with unique methodological challenges that directly impact both internal and external validation strategies. The primary issue is data imbalance, where datasets contain a vast majority of non-events alongside a small number of rare events. This imbalance introduces biases that cause models to favor the prediction of the non-event majority class, leading to poor performance in identifying the rare outcomes of actual interest [52]. Furthermore, the phenomenon of "sparse data bias" becomes a significant concern in model development. This occurs when the number of predictor variables approaches or exceeds the number of available rare events, yielding unstable and unreliable parameter estimates. Traditional statistical methods like logistic regression are particularly vulnerable to this issue, as they can become highly unstable when the number of variables is too large for the number of events [52].
Another critical challenge is the determination of an appropriate sample size. Traditional sample size calculations, which often assume equal prevalence between event and non-event groups, are ill-suited for rare event modeling. While the concept of "events per variable" (EPV) is sometimes used as a guideline, it may not accurately account for the complexity and heterogeneity inherent in rare event data, calling for more nuanced methods [52]. Finally, the interpretability of prediction models, especially complex machine learning or deep learning models often viewed as "black boxes," is a major hurdle. The inability to understand a model's decision-making process severely limits its adoption in critical areas like clinical practice, where understanding the "why" behind a prediction is as important as the prediction itself [52].
Methodological Approaches for Robust Internal Validation
Internal validation is a critical first step to mitigate optimism bias before a model is subjected to external validation. In the context of small samples and rare events, the choice of internal validation strategy is paramount. A simulation study focusing on high-dimensional prognosis models, such as those used in transcriptomic analysis of head and neck tumors, provides valuable evidence-based recommendations [4].
Comparison of Internal Validation Strategies
The table below summarizes the performance of various internal validation strategies as identified in simulation studies involving time-to-event data with limited samples.
Table 1: Comparison of Internal Validation Strategies for Small Samples and High-Dimensional Data
| Validation Method | Reported Performance & Characteristics | Recommended Use Case |
|---|---|---|
| Train-Test Split | Shows unstable performance; highly dependent on a single, often small, split of the data. | Not recommended for very small sample sizes due to high variance. |
| Conventional Bootstrap | Tends to be over-optimistic, providing performance estimates that are unrealistically high. | Use with caution; known to inflate performance metrics in small samples. |
| 0.632+ Bootstrap | Can be overly pessimistic, particularly with small samples (n=50 to n=100). | May be useful as a conservative estimate but can underestimate true performance. |
| K-Fold Cross-Validation | Demonstrates greater stability and improved performance with larger sample sizes. | Recommended for internal validation of penalized models in high-dimensional settings. |
| Nested Cross-Validation | Shows performance fluctuations depending on the regularization method used for model development. | Recommended, but requires careful tuning of hyperparameters. |
Detailed Experimental Protocol: K-Fold Cross-Validation
For researchers implementing K-fold cross-validation, the following detailed protocol, based on methodologies used in recent studies, ensures robustness [4] [2]:
- Data Preparation: Begin with a dataset where the number of predictors (p) is likely much larger than the number of observations (n). Ensure the rare event or survival outcome is clearly defined.
- Stratification: Randomly partition the dataset into k (commonly 5 or 10) folds of approximately equal size. Critical Step: Ensure that each fold preserves the overall proportion of the rare event (or event status in survival analysis) found in the full dataset. This stratified approach is crucial for maintaining the integrity of the rare event class in all folds.
- Iterative Training and Validation: For each of the k iterations:
- Designate one fold as the temporary validation set.
- Combine the remaining k-1 folds to form the training set.
- Train the model (e.g., a Cox penalized regression model like LASSO or Ridge) on the training set.
- Apply the trained model to the temporary validation fold to generate predictions.
- Calculate performance metrics (e.g., C-index, Brier score) on this validation fold.
- Performance Aggregation: After all k iterations, aggregate the performance metrics from each of the k validation folds. The final performance estimate (e.g., mean C-index) is the average of these k estimates. This aggregated metric provides a more stable and reliable assessment of model performance than a single train-test split.
Advanced Modeling Techniques for Rare Events
Beyond validation strategies, the choice of modeling technique itself is critical. The following advanced methods have been developed to directly address the challenges of rarity and imbalance [52]:
- Penalized Regression (e.g., LASSO, Ridge): These techniques are essential for avoiding sparse data bias when the number of variables is high. They work by imposing a penalty on the size of coefficients, which prevents overfitting and produces more stable and generalizable models.
- Ensemble Methods (e.g., Random Forests): These methods combine multiple weak learners to create a strong predictive model. They have been shown to demonstrate superior performance compared to clinically used risk calculators when applied to real-world patient data, as they can capture complex, non-linear relationships without overfitting as easily as single models.
- Zero-Inflated Models: These are a suitable approach when rare events occur infrequently or exhibit "excessive zeros." They account for this by treating the excess zeros as a separate process, providing a more accurate representation of the underlying data generation process.
- Accounting for Data Correlation: Incorporating knowledge of spatial or temporal dependencies among data points can enhance predictive performance by capturing relevant contextual information and underlying structures.
Strategies for Meaningful External Validation
External validation is the ultimate test of a model's utility and generalizability. For models built on rare events, this phase presents distinct challenges, primarily due to the difficulty in acquiring sufficiently large, independent datasets.
A key strategy is the prospective collection of multi-institutional data. A compelling example is the external validation of an AI model for stratifying recurrence risk in early-stage lung cancer. In this study, the model was developed on data from the U.S. National Lung Screening Trial (NLST) and then externally validated on a completely independent cohort of 252 patients from the North Estonia Medical Centre (NEMC). This process confirmed the model's ability to outperform standard clinical staging systems, particularly for stage I disease, and demonstrated correlation with established pathologic risk factors [2]. The success of this validation underscores the importance of using geographically and institutionally distinct data sources to test true generalizability.
When a single external cohort is too small, a collaborative approach using prospective meta-analysis principles can be employed. This involves validating the model across several independent but similar-sized cohorts from different centers and then statistically combining the performance estimates (e.g., C-index, calibration slopes) from each center. This approach provides a more powerful and reliable assessment of the model's transportability than is possible with any single, small cohort.
Furthermore, the external validation should move beyond simple discriminative performance. The analysis must include a thorough assessment of calibration in the new population—that is, how well the model's predicted probabilities of the rare event align with the observed event rates. A model may have good discrimination (ability to separate high-risk from low-risk patients) but poor calibration, which would limit its clinical applicability for absolute risk estimation.
Detailed Experimental Protocol for External Validation
The following protocol outlines the steps for a robust external validation study, as exemplified in recent research [2]:
- Cohort Definition and Eligibility: Define the external validation cohort with clear inclusion and exclusion criteria that mirror the development cohort as closely as possible, though the population itself should be independent. For the lung cancer AI model, this involved patients with clinical stage I-IIIA lung cancer who underwent surgical resection, had a documented TNM stage, and at least 2 years of follow-up [2].
- Data Curation and Harmonization: Meticulously curate the external data to ensure consistency with the model's requirements. The study highlights "extensive (re)curation" of preoperative CT scans and clinical metadata to ensure they were consistent with outcomes and the development data [2]. This step is crucial for minimizing technical rather than biological reasons for performance decay.
- Blinded Model Application: Apply the fully specified model (including all coefficients and pre-processing steps) to the external validation cohort without any retraining or modification. This tests the model's performance "as is" in a new setting.
- Comprehensive Performance Assessment: Evaluate the model on the external cohort using a suite of metrics:
- Discrimination: Calculate the C-index (Concordance index) for time-to-event data.
- Calibration: Generate calibration plots and use metrics like the integrated Brier Score to assess the agreement between predicted and observed event probabilities.
- Clinical Utility: Perform Decision Curve Analysis (DCA) to evaluate the net benefit of using the model for clinical decision-making across different risk thresholds.
- Comparison to Standard of Care: Benchmark the model's performance against existing clinical standards. In the lung cancer example, the AI model's stratification was compared directly against conventional TNM staging and tumor size criteria, demonstrating a superior hazard ratio for disease-free survival [2].
Integrated Workflow and Research Toolkit
Logical Workflow for Validation of Rare Event Models
The following diagram illustrates the integrated logical workflow for addressing small sample sizes and rare events across the entire model development and validation pipeline, from data preparation to final model selection.
Diagram: Validation Workflow for Rare Events
The Scientist's Toolkit: Essential Research Reagents and Solutions
The following table details key methodological "reagents" essential for conducting robust validation studies in the context of rare events.
Table 2: Research Reagent Solutions for Rare Event Model Validation
| Tool / Method | Primary Function | Technical Specification & Application Note |
|---|---|---|
| K-Fold Cross-Validation | Internal validation to provide a stable estimate of model performance and mitigate overfitting. | Typically k=5 or k=10. Use stratified sampling to ensure each fold retains the proportion of the rare event. The process involves iterative training and validation across all folds [4]. |
| Cox Penalized Regression | Model development for time-to-event data with many predictors; prevents overfitting via regularization. | Methods include LASSO (L1), Ridge (L2), and Elastic Net. A key hyperparameter (λ) controls the strength of the penalty, typically selected via cross-validation [4]. |
| Concordance Index (C-index) | Metric to evaluate the discriminative ability of a survival model. | Measures the proportion of all comparable pairs of patients where the model correctly predicts the order of events. A value of 0.5 is no better than chance, 1.0 is perfect discrimination [13]. |
| Brier Score | A composite metric to assess both the calibration and discrimination of a model. | Represents the mean squared difference between the predicted probability and the actual outcome. Lower scores (closer to 0) indicate better accuracy [4]. |
| Nomogram | A graphical tool to visualize a complex model and enable personalized risk prediction. | Translates the mathematical model into a simple, points-based scoring system that clinicians can use to estimate an individual's probability of an event (e.g., 3- or 5-year survival) without software [13]. |
| Decision Curve Analysis (DCA) | Evaluates the clinical utility and net benefit of a model across different probability thresholds. | Helps answer whether using the predictive model to guide decisions (e.g., treat vs. not treat) would improve outcomes compared to default strategies [13]. |
Navigating the complexities of model validation for rare events and small sample sizes requires a meticulous and multi-faceted approach. The challenges of data imbalance and sparse data bias demand a departure from conventional methodologies. As detailed in this guide, robust internal validation through strategies like k-fold cross-validation is a non-negotiable first step to generate realistic performance estimates and guide model selection. This must be coupled with the use of specialized modeling techniques such as penalized regression and ensemble methods that are inherently more resistant to overfitting.
Furthermore, the true test of a model's value lies in its external validation on completely independent datasets. This process, while challenging, is achievable through collaborative, multi-institutional efforts and rigorous, pre-specified validation protocols that assess discrimination, calibration, and clinical utility. By systematically implementing these advanced strategies—spanning data handling, internal validation, model development, and external validation—researchers and drug development professionals can produce predictive models that are not only statistically sound but also clinically trustworthy and capable of making a meaningful impact on the understanding and management of rare events.
Mitigating Overfitting in High-Dimensional Data and Machine Learning Models
In the realm of modern data science, particularly in fields like drug development and biomedical research, the proliferation of high-dimensional datasets has become commonplace. These datasets, characterized by a vast number of features (often exceeding the number of observations), present unique challenges for building robust machine learning models. Overfitting occurs when a model becomes overly complex and memorizes noise and random fluctuations in the training data rather than learning generalizable patterns [53]. This problem intensifies exponentially in high-dimensional settings due to what is known as the "curse of dimensionality" [54] [55].
In high-dimensional spaces, data points become sparse, and the volume of the space grows exponentially, making it increasingly difficult to find meaningful patterns [55]. Models trained on such data gain excessive capacity to fit training samples precisely, including their noise, which compromises their performance on unseen data. The relationship between high dimensionality and overfitting is particularly problematic in healthcare and pharmaceutical contexts, where model reliability can directly impact patient outcomes and treatment efficacy [56] [57].
The validation of models developed with high-dimensional data requires careful consideration within the broader framework of internal versus external validation research. Internal validation assesses model performance using resampling methods on the original dataset, while external validation tests the model on completely independent data [4]. For high-dimensional problems, rigorous internal validation is particularly crucial as it provides the first line of defense against overfitting before proceeding to external validation [4].
Theoretical Foundations: Why High-Dimensional Data Promotes Overfitting
Fundamental Mechanisms
The tendency of high-dimensional data to promote overfitting stems from several interconnected phenomena. As dimensionality increases, data points become sparsely distributed through the expanded space, making it difficult to capture the true underlying distribution without extensive sampling [53]. This data sparsity means that with a fixed sample size, the density of data points decreases exponentially, leaving vast empty regions where the model must interpolate or extrapolate without sufficient guidance.
Another critical factor is model complexity. With more features available, the model's capacity to learn increases, allowing it to fit the training data more closely [53]. While this can be beneficial, it also increases the risk of fitting to random fluctuations that do not represent genuine relationships. Complex models with many parameters can essentially memorize the training dataset rather than learning transferable patterns.
The breakdown of distance-based relationships further exacerbates the problem. In high-dimensional space, the concept of "nearest neighbors" becomes less meaningful as most points are approximately equidistant [53]. This phenomenon negatively impacts algorithms that rely on distance measurements, such as K-Nearest Neighbors (KNN) and clustering methods.
Additionally, multicollinearity and feature redundancy often occur in high-dimensional data, where multiple features provide similar or correlated information [53]. This can make it difficult to distinguish each feature's unique contribution and lead to unstable model estimates that vary significantly with small changes in the data.
Consequences for Predictive Modeling
The combination of these factors creates an environment where models can achieve deceptive performance on training data while failing to generalize. In pharmaceutical research, this can manifest as promising results during initial development that fail to replicate in subsequent validation studies or clinical trials. The model may identify apparent patterns that are actually specific to the training set rather than reflective of broader biological truths.
Methodological Approaches to Mitigate Overfitting
Feature Selection Techniques
Feature selection methods identify and retain the most informative features while discarding irrelevant or redundant ones, thereby reducing dimensionality and model complexity [53]. These techniques can be broadly categorized into filter, wrapper, and embedded methods.
Hybrid feature selection algorithms represent advanced approaches that combine multiple strategies. Recent research has demonstrated the effectiveness of several novel hybrid methods:
Table 1: Hybrid Feature Selection Algorithms for High-Dimensional Data
| Algorithm | Mechanism | Key Advantages | Reported Performance |
|---|---|---|---|
| TMGWO (Two-phase Mutation Grey Wolf Optimization) | Incorporates a two-phase mutation strategy to enhance exploration-exploitation balance [54] | Superior feature selection and classification accuracy | Achieved 96% accuracy on Breast Cancer dataset using only 4 features [54] |
| BBPSO (Binary Black Particle Swarm Optimization) | Employs velocity-free mechanism with adaptive chaotic jump strategy [54] | Prevents stuck particles, improves computational performance | Outperformed comparison methods in discriminative feature selection [54] |
| ISSA (Improved Salp Swarm Algorithm) | Incorporates adaptive inertia weights, elite salps, and local search techniques [54] | Significantly boosts convergence accuracy | Effective for identifying significant features for classification [54] |
Experimental protocols for evaluating feature selection methods typically involve comparative studies on benchmark datasets. For instance, in one study, experiments were conducted using three well-known datasets: the Wisconsin Breast Cancer Diagnostic dataset, the Sonar dataset, and the Differentiated Thyroid Cancer dataset [54]. Performance of classification algorithms including K-Nearest Neighbors (KNN), Random Forest (RF), Multi-Layer Perceptron (MLP), Logistic Regression (LR), and Support Vector Machines (SVM) were evaluated both with and without feature selection, measuring improvements in accuracy, precision, and recall [54].
Figure 1: Feature Selection Workflow for High-Dimensional Data
Dimensionality Reduction Strategies
Dimensionality reduction techniques transform the original high-dimensional space into a lower-dimensional representation while preserving essential information [53] [55]. Unlike feature selection, which selects a subset of original features, these methods create new composite features.
Principal Component Analysis (PCA) is one of the most widely used linear dimensionality reduction techniques. It identifies the principal components - directions in which the data varies the most - and projects the data onto these components [55]. The implementation typically involves standardizing the data, computing the covariance matrix, calculating eigenvectors and eigenvalues, and selecting the top k components based on explained variance.
t-Distributed Stochastic Neighbor Embedding (t-SNE) is a nonlinear technique particularly effective for visualization of high-dimensional data in 2D or 3D spaces [55]. It works by converting similarities between data points to joint probabilities and tries to minimize the Kullback-Leibler divergence between the joint probabilities of the low-dimensional embedding and the high-dimensional data.
Uniform Manifold Approximation and Projection (UMAP) is another nonlinear dimensionality reduction technique that often preserves more of the global structure than t-SNE [55]. It constructs a topological representation of the data and then optimizes a low-dimensional graph to be as similar as possible.
The experimental protocol for applying dimensionality reduction typically begins with data preprocessing, including handling missing values and normalization. The reduction algorithm is then fitted on the training data only, and the same transformation is applied to validation and test sets to avoid data leakage. The optimal number of dimensions is determined through cross-validation, balancing information preservation with dimensionality reduction.
Regularization Methods
Regularization techniques introduce constraints or penalties to the model training process to prevent overfitting by discouraging overcomplexity [53]. These methods work by adding a penalty term to the loss function that the model optimizes.
L1 Regularization (Lasso) adds the absolute value of the magnitude of coefficients as a penalty term. This approach has the desirable property of performing feature selection by driving some coefficients to exactly zero [55]. In high-dimensional settings where many features may be irrelevant, this automatic feature selection is particularly valuable.
L2 Regularization (Ridge) adds the squared magnitude of coefficients as a penalty term. While it doesn't typically zero out coefficients completely, it shrinks them proportionally, which helps reduce model variance without completely eliminating any features [53].
Elastic Net combines both L1 and L2 regularization, aiming to get the benefits of both approaches. It's particularly useful when dealing with highly correlated features, as L2 regularization helps distribute weight among correlated variables while L1 promotes sparsity.
Implementation protocols for regularization involve standardizing features first (as the penalty terms are sensitive to feature scales), then performing cross-validation to select the optimal regularization strength parameter (λ). The model is trained with various λ values, and the value that provides the best cross-validated performance is selected.
Ensemble Methods
Ensemble methods combine multiple base models to produce a single consensus prediction, generally resulting in better generalization than any individual model [53]. These methods work by reducing variance without substantially increasing bias.
Random Forest constructs multiple decision trees during training and outputs the mode of the classes (classification) or mean prediction (regression) of the individual trees [57]. By introducing randomness through bagging (bootstrap aggregating) and random feature selection, it creates diverse trees that collectively generalize better.
Extreme Gradient Boosting (XGBoost) builds models sequentially, with each new model attempting to correct errors made by previous ones [57]. It combines weak learners into a strong learner using gradient descent to minimize a loss function. XGBoost includes built-in regularization to control model complexity.
In experimental applications, ensemble methods require careful hyperparameter tuning. For Random Forest, key parameters include the number of trees, maximum depth, and minimum samples per leaf. For XGBoost, important parameters are learning rate, maximum depth, and subsampling ratios. Cross-validation is essential for optimal parameter selection.
Internal Validation Strategies for High-Dimensional Models
Validation Frameworks
Internal validation provides the critical first assessment of a model's generalizability using the available dataset [4]. For high-dimensional models, standard train-test splits often prove inadequate, leading to optimistic performance estimates.
Table 2: Internal Validation Methods for High-Dimensional Data
| Method | Procedure | Advantages | Limitations | Recommended Use |
|---|---|---|---|---|
| K-Fold Cross-Validation | Data split into K folds; model trained on K-1 folds, validated on held-out fold [4] | More reliable and stable than train-test; efficient data use | Computational intensity; variance in small samples | Primary choice for model selection [4] |
| Nested Cross-Validation | Outer loop for performance estimation, inner loop for hyperparameter tuning [4] | Unbiased performance estimate; avoids overfitting | High computational cost; complex implementation | When unbiased performance estimate is critical [4] |
| Bootstrap Validation | Multiple samples drawn with replacement; performance averaged across iterations [4] | Good for small samples; stable estimates | Can be over-optimistic; may need 0.632+ correction [4] | Small sample sizes with caution |
| Train-Test Split | Simple random split (e.g., 70-30 or 80-20) | Computational efficiency; simplicity | High variance; unstable with small samples [4] | Initial exploratory analysis only |
Recent research has provided empirical comparisons of these methods in high-dimensional settings. A simulation study using transcriptomic data from head and neck cancer patients (N=76) found that train-test validation showed unstable performance, while conventional bootstrap was over-optimistic [4]. The 0.632+ bootstrap method was found to be overly pessimistic, particularly with small samples (n=50 to n=100) [4]. K-fold cross-validation and nested cross-validation demonstrated improved performance with larger sample sizes, with k-fold cross-validation showing greater stability [4].
Performance Metrics Beyond Accuracy
Comprehensive model evaluation requires multiple metrics that capture different aspects of performance [58]. For high-dimensional data, relying solely on accuracy can be misleading, particularly with class-imbalanced datasets common in medical research.
Confusion Matrix provides a complete picture of model performance across different categories [58]. It includes true positives, true negatives, false positives, and false negatives, from which multiple metrics can be derived.
Precision and Recall are particularly important in medical contexts where the costs of different types of errors vary substantially [58]. Precision (positive predictive value) measures the proportion of positive identifications that were actually correct, while recall (sensitivity) measures the proportion of actual positives that were correctly identified.
F1-Score represents the harmonic mean of precision and recall, providing a single metric that balances both concerns [58]. This is especially valuable when seeking an optimal balance between false positives and false negatives.
Area Under the ROC Curve (AUC-ROC) measures the model's ability to distinguish between classes across all possible classification thresholds [58]. A key advantage is its independence from the proportion of responders in the dataset, making it robust to class imbalance.
Implementation protocols for comprehensive evaluation involve calculating multiple metrics during cross-validation and on held-out test sets. Performance should be evaluated across different subgroups to identify potential biases, and confidence intervals should be reported to quantify estimation uncertainty.
Figure 2: Internal Validation Workflow in Model Development
Experimental Protocols and Research Toolkit
Standardized Experimental Framework
Implementing a rigorous experimental protocol is essential for developing robust models with high-dimensional data. The following workflow represents best practices derived from recent research:
Data Preprocessing: Handle missing values through appropriate imputation methods. Standardize or normalize features to ensure comparable scales, particularly important for regularization and distance-based methods.
Exploratory Data Analysis: Conduct comprehensive EDA to understand feature distributions, identify outliers, and detect multicollinearity. Visualization techniques like PCA plots can reveal underlying data structure.
Feature Engineering/Selection: Apply appropriate feature selection methods based on data characteristics. For very high-dimensional data (e.g., genomics), consider univariate filtering first to reduce dimensionality before applying more computationally intensive wrapper methods.
Model Training with Cross-Validation: Implement k-fold cross-validation (typically k=5 or k=10) for model training and hyperparameter optimization. Ensure that any preprocessing or feature selection is refit within each training fold to avoid data leakage.
Comprehensive Evaluation: Assess model performance using multiple metrics on the validation set. Conduct error analysis to identify patterns in misclassifications and potential biases.
Final Model Selection: Choose the best-performing model configuration based on cross-validation results. Retrain the model on the entire training set using the optimal hyperparameters.
Holdout Test Evaluation: Evaluate the final model on the previously untouched test set to obtain an unbiased estimate of generalization performance.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Computational Tools for High-Dimensional Data Analysis
| Tool/Category | Function | Example Implementation | Application Context |
|---|---|---|---|
| Feature Selection Algorithms | Identify most predictive features | TMGWO, BBPSO, ISSA [54] | Initial dimensionality reduction |
| Dimensionality Reduction | Create low-dimensional representations | PCA, t-SNE, UMAP [55] | Data visualization and preprocessing |
| Regularization Methods | Prevent overfitting through constraints | Lasso, Ridge, Elastic Net [53] [55] | Model training with high-dimensional features |
| Ensemble Methods | Combine multiple models for robustness | Random Forest, XGBoost [57] | Final predictive modeling |
| Validation Frameworks | Assess model generalizability | k-Fold CV, Nested CV [4] | Throughout model development |
| Performance Metrics | Evaluate model performance comprehensively | AUC-ROC, F1-Score, Precision-Recall [58] | Model evaluation and selection |
| Model Interpretation | Explain model predictions | SHAP, LIME [59] | Post-hoc analysis and validation |
Mitigating overfitting in high-dimensional data requires a multifaceted approach combining feature selection, dimensionality reduction, regularization, ensemble methods, and rigorous internal validation. The strategies outlined in this technical guide provide a comprehensive framework for developing models that generalize well beyond their training data.
The critical importance of proper internal validation cannot be overstated in the context of high-dimensional problems. Methods like k-fold cross-validation and nested cross-validation provide more reliable performance estimates than simple train-test splits, especially when sample sizes are limited relative to feature dimensionality [4]. These internal validation strategies form the essential bridge between model development and external validation, helping ensure that promising results on training data will translate to genuine predictive utility in real-world applications.
For researchers in drug development and biomedical sciences, where high-dimensional data is ubiquitous and model reliability has direct implications for patient care, adopting these rigorous approaches is not merely academic but essential for producing meaningful, reproducible results that can safely transition from research environments to clinical practice.
Optimizing Tuning Parameters and Model Selection Procedures
The process of selecting and optimizing machine learning (ML) models is a cornerstone of modern computational research, particularly in high-stakes fields like pharmaceutical drug discovery. This process is fundamentally governed by the bias-variance tradeoff, where overly simple models fail to capture data patterns (high bias), and overly complex models perform poorly on new, unseen data (high variance)—a phenomenon known as overfitting [60]. The ultimate goal of model selection is to identify an algorithm that optimally balances this tradeoff, achieving robust generalization capability.
Framing this within the context of internal versus external validation is paramount. Internal validation techniques, such as cross-validation, provide an initial, controlled assessment of a model's performance using the data available during development. However, the true test of a model's utility and robustness lies in its external validation—its performance on completely independent datasets collected from different populations or in different settings [13]. A model that excels in internal validation but fails in external validation has not successfully generalized, highlighting a critical disconnect between development and real-world application. This guide provides a technical roadmap for navigating the complete model selection lifecycle, with a sustained focus on strategies that enhance external validity.
Theoretical Foundations of Model Selection
Core Concepts and the Bias-Variance Tradeoff
At its core, model selection involves choosing the right level of model complexity. Regularization techniques are a primary tool for managing this complexity. They work by adding a penalty term to the model's loss function, discouraging over-reliance on any single feature or weight. Common methods include L1 regularization (Lasso), which can drive some feature coefficients to zero, and L2 regularization (Ridge), which shrinks coefficients uniformly [61]. The strength of this penalty is itself a tuning parameter that must be optimized.
Another key concept is the distinction between model parameters and hyperparameters. Model parameters are the internal variables that the model learns from the training data, such as weights and biases in a neural network [61]. In contrast, hyperparameters are configuration settings external to the model that govern the learning process itself. These are not learned from the data and must be set prior to training. Examples include the learning rate, the number of hidden layers in a deep network, the number of trees in a random forest, and the regularization strength.
Validation Strategies and Performance Metrics
A robust model selection procedure relies on a rigorous data-splitting strategy. Typically, data is divided into three sets:
- Training Set: Used to train the model and learn its parameters [61].
- Validation Set: Used to evaluate different models and hyperparameter settings during the selection and tuning process [60].
- Test Set: Held back until the very end to provide an unbiased final evaluation of the model selected [61].
Cross-validation, particularly k-fold cross-validation, is a gold-standard technique for internal validation. It maximizes data usage by partitioning the training data into 'k' subsets, iteratively using k-1 folds for training and the remaining fold for validation. The average performance across all k folds provides a stable estimate of model performance [60].
Evaluating performance requires careful metric selection. For classification tasks, common metrics include:
- Accuracy: The proportion of total correct predictions.
- Precision and Recall: respectively measure the quality of positive predictions and the model's ability to find all positive instances.
- Area Under the Receiver Operating Characteristic Curve (AUC-ROC): Measures the model's ability to distinguish between classes [13].
For regression tasks, Mean Squared Error (MSE) and R-squared are frequently used. A multi-metric assessment is crucial, as no single metric can capture all performance dimensions [60].
Table 1: Key Phases of the Model Selection Lifecycle
| Phase | Primary Objective | Key Activities | Primary Validation Type |
|---|---|---|---|
| Exploratory | Problem Framing & Data Understanding | Data collection, cleaning, and exploratory data analysis (EDA) | N/A |
| Development | Model Construction & Internal Tuning | Algorithm selection, hyperparameter optimization, cross-validation | Internal Validation |
| Evaluation | Unbiased Performance Estimation | Final assessment on a held-out test set | Internal Validation |
| Deployment | Real-World Application & Monitoring | Model deployment, performance monitoring, retraining | External Validation |
Data-Driven Model Selection Procedures
Hyperparameter Optimization Techniques
Hyperparameter optimization is the engine of model tuning. Several systematic approaches exist:
- Grid Search: An exhaustive method that tests every combination of hyperparameters from pre-defined lists. While guaranteed to find the best combination within the grid, it is computationally expensive and often infeasible for high-dimensional parameter spaces [61].
- Random Search: Instead of an exhaustive search, this method samples hyperparameter combinations randomly from a specified distribution. Research has shown that random search is often more efficient than grid search, as it can find good combinations with far fewer iterations, especially when some parameters have low impact on performance [61].
- Bayesian Optimization: A more advanced, sequential approach that builds a probabilistic model of the function mapping hyperparameters to model performance. It uses this model to select the most promising hyperparameters to evaluate next, making it highly efficient for optimizing costly black-box functions [61]. Automated tools like Optuna and Ray Tune can significantly streamline this process [61].
Advanced Selection and Optimization Paradigms
Beyond tuning individual models, several advanced paradigms leverage existing knowledge and data:
- Transfer Learning: Involves taking a pre-trained model (e.g., on a large, general dataset) and adapting it to a specific task. This is particularly valuable in domains like medical imaging or bioinformatics, where large, labeled datasets are scarce. The process typically involves fine-tuning the model's final layers on the target data with a lower learning rate [62].
- Federated Learning: Enables model training across decentralized devices or institutions without sharing raw data. This is critical for drug development, where patient data privacy is paramount. Institutions collaboratively train a model by sharing only model parameter updates, not the data itself [62].
Table 2: Summary of Hyperparameter Optimization Methods
| Method | Key Principle | Advantages | Disadvantages | Best-Suited Context |
|---|---|---|---|---|
| Grid Search | Exhaustive search over a defined grid | Simple, parallelizable, comprehensive | Computationally prohibitive for high dimensions | Small parameter spaces (2-4 parameters) |
| Random Search | Random sampling from parameter distributions | More efficient than grid search, easy to implement | May miss the global optimum, less systematic | Medium to large parameter spaces |
| Bayesian Optimization | Sequential model-based optimization | Highly sample-efficient, handles noisy objectives | Higher complexity, sequential nature limits parallelization | Expensive-to-evaluate models (e.g., deep learning) |
Internal versus External Validation: A Framework for Robustness
Defining the Validation Spectrum
The distinction between internal and external validation is the bedrock of reliable model development.
Internal Validation refers to techniques used to assess model performance using the data available at the development stage. Its primary purpose is model selection and tuning while providing a preliminary check for overfitting. Key methods include train-test splits, k-fold cross-validation, and bootstrapping [60]. The performance metrics derived from internal validation (e.g., cross-validated AUC) are estimates of how the model is expected to perform on new data from a similar population.
External Validation is the process of evaluating a finalized model on a completely independent dataset. This dataset should be collected from a different source, a different geographical location, or at a different time period [13]. For instance, a model developed on data from a clinical trial run in the US must be validated on data from a trial run in Europe. External validation is the ultimate test of a model's generalizability, transportability, and real-world clinical or scientific utility. A significant drop in performance from internal to external validation indicates that the model may have learned idiosyncrasies of the development data that do not hold universally.
A Case Study in Clinical Prediction
The critical importance of external validation is powerfully illustrated by a 2025 study developing a nomogram to predict overall survival in cervical cancer patients [13]. The researchers first developed their model using 9,514 patient records from the SEER database (Training Cohort). They then performed internal validation on 4,078 different patients from the same SEER database (Internal Validation Cohort), achieving a strong C-index of 0.885 [13].
The crucial next step was external validation using 318 patients from a completely different institution, Yangming Hospital Affiliated to Ningbo University [13]. While the model's performance (C-index: 0.872) remained high, this independent test confirmed its robustness and generalizability beyond the original data source. This workflow—development, internal validation, and external validation—epitomizes a rigorous model selection and evaluation pipeline.
Model Validation Pathway
Post-Deployment Considerations and Model Sustainability
Model selection does not end at deployment. The performance of a model can decay over time due to concept drift, where the underlying relationships between input and output variables change [60]. In drug discovery, this could be caused by the emergence of new disease strains, changes in patient demographics, or shifts in clinical practices.
Therefore, a robust model selection framework must include plans for post-deployment maintenance. This involves:
- Continuous Monitoring: Tracking the model's performance on incoming data against established benchmarks [60].
- Concept Drift Detection: Implementing statistical techniques to identify when model performance has significantly degraded due to changing data distributions [60].
- Retraining Strategies: Establishing clear protocols for when and how to retrain the model with new data to restore its predictive performance [60]. This ensures the model remains accurate and relevant throughout its lifecycle.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Tools for AI/ML in Drug Discovery
| Tool / Reagent Name | Type / Category | Primary Function in Model Selection & Optimization |
|---|---|---|
| Optuna [61] | Software Framework | An open-source hyperparameter optimization framework that automates the search for optimal parameters using various algorithms like Bayesian optimization. |
| XGBoost [61] | ML Algorithm | An optimized gradient boosting library known for its speed and performance; it includes built-in regularization and cross-validation. |
| Ray Tune [61] | Software Library | A scalable Python library for distributed hyperparameter tuning and model selection, supporting all major ML frameworks. |
| TensorRT [61] | SDK | A high-performance deep learning inference optimizer that provides low-latency, high-throughput deployment via techniques like quantization and pruning. |
| ONNX Runtime [61] | Tool | An open-source cross-platform engine for accelerating machine learning model inference and training, enabling model portability across frameworks. |
| BioBERT / SciBERT [62] | Pre-trained Model | Domain-specific language models pre-trained on biomedical and scientific literature, used for transfer learning on text-mining tasks in drug discovery. |
| Federated Learning Framework [62] | Methodology | A secure, privacy-preserving collaborative learning approach that allows model training on decentralized data sources without data sharing. |
Optimization Strategy Decision Tree
Balancing Statistical Efficiency with Clinical Relevance
In the development of clinical prediction models and therapeutic interventions, a fundamental tension exists between statistical optimization and real-world applicability. Statistical efficiency ensures that models are robust and reproducible within development datasets, while clinical relevance determines whether these tools will improve patient outcomes in diverse healthcare settings. This whitepaper examines methodological frameworks for balancing these competing priorities throughout the validation continuum, from initial internal validation to generalizability assessment. By synthesizing contemporary evidence from oncology, palliative care, and pharmaceutical development, we provide a structured approach for researchers and drug development professionals to navigate this critical intersection.
The translation of predictive models and therapeutic innovations from research environments to clinical practice represents a significant challenge in medical science. Statistical efficiency refers to the optimal use of data to develop robust, reproducible models with minimal bias and overfitting, while clinical relevance ensures these models meaningfully impact patient care, clinical decision-making, and ultimately improve health outcomes [63] [46]. This balance is particularly crucial in contexts where high-dimensional data (such as genomics, transcriptomics, and radiomics) introduces substantial complexity and risk of model overoptimism [63] [2].
The validation pathway for any clinical prediction model or intervention proceeds through sequential stages: internal validation first assesses model performance within the development dataset, while external validation evaluates generalizability to independent populations and settings [13] [2]. Each stage serves distinct purposes in balancing statistical properties with clinical utility. Internal validation methods aim to produce statistically efficient models that are not overfitted to their development data, while external validation provides the ultimate test of clinical relevance by assessing performance in real-world practice [46] [64].
Table 1: Key Definitions in Model Validation
| Term | Definition | Primary Objective |
|---|---|---|
| Statistical Efficiency | Optimal use of data to develop robust models with minimal bias and overfitting | Ensure reproducibility and internal validity of model predictions |
| Clinical Relevance | Meaningful impact on patient care, clinical decision-making, and health outcomes | Ensure utility and effectiveness in real-world healthcare settings |
| Internal Validation | Assessment of model performance within the development dataset using resampling methods | Quantify and correct for optimism bias in model performance |
| External Validation | Evaluation of model performance on independent datasets from different populations or settings | Assess generalizability and transportability to real-world practice |
Internal Validation: Ensuring Statistical Efficiency
Internal validation methodologies provide the foundation for statistical efficiency by quantifying and correcting for optimism bias—the tendency of models to perform better on their development data than on new samples [63]. These techniques use resampling strategies to simulate how the model would perform on new data drawn from the same underlying population.
Methodological Approaches
Multiple internal validation strategies exist, each with distinct advantages and limitations depending on sample size, data dimensionality, and model complexity:
Train-Test Split: Randomly partitions data into development (typically 70%) and validation (30%) subsets [13] [63]. While conceptually simple, this approach demonstrates unstable performance with smaller sample sizes and fails to utilize the full dataset for model development [63].
Bootstrap Methods: Generate multiple resampled datasets with replacement to estimate optimism [63] [4]. Conventional bootstrap tends to be over-optimistic, while the 0.632+ bootstrap correction can be overly pessimistic, particularly with small samples (n = 50 to n = 100) [63].
K-Fold Cross-Validation: Partitions data into k subsets (typically 5-10), iteratively using k-1 folds for training and one for validation [63] [4]. This approach offers a favorable balance between bias and stability, particularly with larger sample sizes [63].
Nested Cross-Validation: Implements an inner loop for hyperparameter optimization within an outer loop for performance estimation [63]. This method minimizes bias in performance estimates but requires substantial computational resources and demonstrates performance fluctuations depending on the regularization method [63].
Table 2: Comparison of Internal Validation Methods for High-Dimensional Data
| Method | Optimal Sample Size | Advantages | Limitations |
|---|---|---|---|
| Train-Test Split | >1,000 cases | Simple implementation; Computationally efficient | High variance with small samples; Inefficient data usage |
| Bootstrap | >500 cases | Comprehensive optimism estimation; Good for confidence intervals | Over-optimistic without correction; Pessimistic with 0.632+ correction |
| K-Fold Cross-Validation | >100 cases | Balanced bias-variance tradeoff; Efficient data usage | Computationally intensive; Strategic folding required for censored data |
| Nested Cross-Validation | >500 cases | Minimal bias in performance estimation; Simultaneous parameter tuning | High computational demand; Complex implementation |
Application in High-Dimensional Settings
High-dimensional data (such as transcriptomics with 15,000+ features) presents particular challenges for internal validation. Simulation studies comparing internal validation strategies in transcriptomic analysis of head and neck tumors demonstrate that k-fold cross-validation and nested cross-validation provide the most stable performance for Cox penalized regression models with time-to-event endpoints [63] [4]. With smaller sample sizes (n < 100), these methods outperform bootstrap approaches, which tend to be either over-optimistic (conventional bootstrap) or overly pessimistic (0.632+ bootstrap) [63].
External Validation: Establishing Clinical Relevance
External validation represents the critical bridge between statistically efficient models and clinically relevant tools by assessing performance on completely independent datasets—different populations, settings, or time periods [13] [2]. This process evaluates the transportability of models beyond their development context.
Methodological Framework
Robust external validation requires pre-specified protocols that mirror the standards of clinical trial design:
Population Heterogeneity: External cohorts should represent the target clinical population with varying demographics, disease stages, and comorbidity profiles [13] [2]. For instance, the external validation of a cervical cancer nomogram used 318 patients from Yangming Hospital, distinct from the 13,592-patient SEER database used for development [13].
Prospective Designs: Whenever feasible, external validation should employ prospective designs that eliminate biases associated with retrospective data curation [2] [65]. The NECPAL tool validation protocol exemplifies this approach with a planned 6-year prospective observational study [65].
Clinical Comparator Arms: Validation studies should compare new models against established clinical standards [2]. In lung cancer recurrence prediction, the AI model was compared directly against conventional TNM staging using hazard ratios for disease-free survival [2].
Real-World Endpoints: Outcomes should reflect clinically meaningful endpoints rather than surrogate biomarkers [46] [64]. Overall survival, disease-free survival, and quality of life measures provide more clinically relevant endpoints than intermediate biomarkers [13] [2].
Performance Metrics for Clinical Relevance
While statistical metrics like C-index and AUC remain important, clinically focused metrics provide greater insight into real-world utility:
Decision Curve Analysis: Evaluates the clinical net benefit of models across different probability thresholds [13].
Calibration Plots: Assess how well predicted probabilities match observed outcomes across the risk spectrum [13].
Reclassification Metrics: Quantify how accurately models reclassify patients compared to existing standards [2].
In the external validation of a cervical cancer nomogram, the model maintained strong performance across cohorts with C-indexes of 0.882 (training), 0.885 (internal validation), and 0.872 (external validation), supporting its clinical applicability [13]. Similarly, an AI model for lung cancer recurrence prediction demonstrated superior hazard ratios compared to conventional staging in both internal (HR = 1.71 vs 1.22) and external (HR = 3.34 vs 1.98) validation [2].
Integrated Validation Frameworks
The most robust validation strategies integrate internal and external approaches throughout the development lifecycle rather than as sequential steps.
Sequential Validation Architecture
A structured approach to validation progressively expands the testing environment:
Integrated Validation Pathway: This workflow illustrates the sequential progression from internal to external validation, with distinct metrics at each stage ensuring both statistical efficiency and clinical relevance.
Real-World Evidence Integration
Regulatory agencies increasingly recognize real-world evidence (RWE) as a valuable source for external validation [46] [64]. RWE derives from routine healthcare data—electronic health records, insurance claims, registries, and patient-generated data—reflecting effectiveness under actual practice conditions rather than idealized trial environments [64].
The advantages of RWE for validation include:
- Assessment of heterogeneous populations typically excluded from RCTs [64]
- Evaluation of long-term outcomes beyond typical trial durations [64]
- Understanding of implementation challenges in routine care settings [46]
Pharmaceutical validation guidance for 2025 emphasizes the need to incorporate RWE throughout the development lifecycle, particularly for emerging therapies like biologics and gene therapies [66].
Case Studies in Balanced Validation
Cervical Cancer Nomogram Development
A comprehensive prediction model for cervical cancer overall survival demonstrates the balanced integration of statistical and clinical considerations [13]:
Development Cohort: 13,592 patients from SEER database (2000-2020) randomized 7:3 into training (n = 9,514) and internal validation (n = 4,078) cohorts [13]
Internal Validation: Multivariate Cox regression identified six predictors (age, tumor grade, stage, size, LNM, LVSI) with C-index 0.882 (95% CI: 0.874-0.890) [13]
External Validation: 318 patients from Yangming Hospital with C-index 0.872 (95% CI: 0.829-0.915) confirming generalizability [13]
Clinical Implementation: Nomogram provided personalized 3-, 5-, and 10-year survival predictions to support clinical decision-making [13]
AI Model for Lung Cancer Recurrence
A machine learning model incorporating preoperative CT images and clinical data outperformed standard staging systems [2]:
Development: 1,015 patients from multiple databases using eightfold cross-validation [2]
Internal Validation: Superior stratification of stage I patients (HR = 1.71 vs 1.22 for tumor size) [2]
External Validation: Maintained performance in independent cohort (HR = 3.34 vs 1.98 for tumor size) [2]
Clinical Correlation: Significant associations with pathologic risk factors (poor differentiation, lymphovascular invasion) strengthened clinical relevance [2]
Table 3: Key Research Reagent Solutions for Validation Studies
| Tool/Category | Specific Examples | Function in Validation |
|---|---|---|
| Statistical Software | R software (version 4.3.2+) with survival, glmnet, and caret packages [13] [63] | Implementation of Cox regression, penalized methods, and resampling validation |
| High-Dimensional Data Platforms | Transcriptomic analysis pipelines (15,000+ features) [63] [4] | Management and analysis of genomics, radiomics, and other complex data types |
| Validation Methodologies | K-fold cross-validation, nested cross-validation, bootstrap [63] [4] | Internal validation to estimate and correct for optimism bias |
| Performance Metrics | C-index, time-dependent AUC, calibration plots, decision curve analysis [13] [63] | Comprehensive assessment of discrimination, calibration, and clinical utility |
| Real-World Data Platforms | Electronic health records, disease registries, insurance claims databases [64] | Sources for external validation representing routine practice environments |
Balancing statistical efficiency with clinical relevance requires meticulous attention throughout the validation continuum. Internal validation methods—particularly k-fold and nested cross-validation for high-dimensional data—establish statistical efficiency by producing robust, reproducible models. External validation through independent cohorts and real-world evidence ultimately determines clinical relevance by assessing generalizability to diverse populations and practice settings.
The most successful validation frameworks integrate these approaches iteratively rather than sequentially, with methodological rigor aligned with clinical intentionality. As predictive models grow increasingly complex with AI and high-dimensional data, maintaining this balance becomes both more challenging and more critical for generating tools that genuinely improve patient care and outcomes.
Future directions include adaptive validation frameworks that continuously update models with real-world data, standardized reporting guidelines following SPIRIT 2025 recommendations [45], and regulatory innovation that accommodates both statistical rigor and clinical relevance throughout the product lifecycle [46] [66].
Solving Implementation Barriers in Real-World Clinical Workflows
Successful integration of new technologies into clinical workflows hinges on a robust validation framework, distinguishing between internal validation (a model's performance on its development data) and external validation (its performance on new, independent data) [67]. This distinction is critical for translational research, where a tool demonstrating perfect internal validation may fail in broader clinical practice due to unforeseen workflow barriers, data heterogeneity, or differing patient populations. This guide examines the primary implementation barriers within clinical environments through the lens of this validation framework, providing technical strategies to overcome them and ensure that research innovations deliver tangible, real-world clinical impact.
The stakes for overcoming these barriers are high. Poorly implemented systems contribute significantly to documentation burden, with clinicians spending an estimated one-third to one-half of their workday interacting with EHR systems, costing an estimated $140 billion annually in lost care capacity [68]. Furthermore, physicians in the U.S. have rated their EHRs with a median System Usability Scale (SUS) score of just 45.9/100, placing them in the bottom 9% of all software systems [68]. Each one-point drop in SUS has been associated with a 3% increase in burnout risk, directly linking implementation quality to clinician well-being [68].
Key Implementation Barriers and Technical Challenges
Workflow-Integration Barriers
Healthcare workflows are inherently complex, involving diverse clinical roles—doctors, nurses, and administrative staff—each interacting with patient data differently [69]. A 2023 HIMSS survey revealed that 48% of clinicians reported EHRs slowed tasks due to poor workflow fit [69]. These misalignments manifest as:
- Task-Switching and Navigation Overload: Clinicians experience significant workflow disruptions from poorly designed interfaces, leading to excessive screen navigation and fragmented information across systems [68].
- Documentation Workarounds: These challenges often necessitate workarounds, such as duplicating documentation or using external tools, further increasing the risk of data entry errors and prolonging documentation times [68].
- Resistance to Change: Approximately 60% of implementation failures stem from user resistance, often driven by fears that new technology will add work or cause errors [69].
Data Migration and Interoperability Challenges
The technical process of moving patient records to a new system presents substantial implementation barriers that can compromise both internal and external validity:
- Data Integrity Risks: Poor data migration and weak links between systems can harm patient safety. Implementation challenges increase when records are missing or inaccurate [69].
- Interoperability Gaps: Data sharing becomes particularly difficult with legacy systems or multiple vendor platforms, creating silos that fragment patient care [69].
- Validation Implications: For predictive models, interoperability gaps can introduce ascertainment bias and information bias when data elements are missing or inconsistently formatted across sites, threatening external validity [69].
Validation-Specific Biases in Real-World Data
When implementing tools developed on research data into clinical workflows, several biases can emerge that differentially affect internal versus external validation:
Table: Common Biases Affecting Validation in Clinical Implementation
| Bias Type | Impact on Internal Validation | Impact on External Validation | Mitigation Strategies |
|---|---|---|---|
| Selection Bias | Minimal impact if development data is representative of source population | Significant impact when implementing across diverse healthcare settings | Use broad inclusion criteria; multi-site development [67] |
| Information Bias | Can be quantified and addressed during model development | Magnified in real-world use due to workflow-driven documentation variations | Natural language processing to standardize unstructured data [69] |
| Ascertainment Bias | Controlled through standardized labeling procedures | Increased when different sites use heterogeneous diagnostic criteria | Implement centralized adjudication processes [67] |
Electronic health records hold value as a data source for observational studies, but researchers must stay alert to the limitations inherent in this kind of data [69]. Several techniques exist to help determine the magnitude and direction of a bias, and statistical methods can play a role in reducing biases and confounders [69].
Methodologies for Implementation Research
Experimental Protocol for Workflow Integration Studies
To systematically evaluate and validate new clinical tools, a structured research protocol is essential. The following provides a detailed methodology for assessing implementation barriers:
Table: Core Protocol for Implementation Feasibility Studies
| Protocol Component | Implementation-Specific Specifications |
|---|---|
| Study Design | Prospective, controlled, multi-center implementation study with mixed-methods evaluation |
| Primary Objective | To demonstrate non-inferiority of task completion times between proposed and existing workflows |
| Secondary Endpoints | User satisfaction (SUS), error rates, cognitive load assessment, workflow disruption frequency |
| Inclusion Criteria | Clinical sites with varying EHR systems, patient volumes, and specialty mixes |
| Exclusion Criteria | Sites undergoing major infrastructure changes or with limited IT support capabilities |
| Data Collection Methods | Time-motion studies, structured observations, EHR interaction logs, user surveys |
| Statistical Considerations | Hierarchical modeling to account for site-level effects; sample size calculated for both superiority and non-inferiority endpoints |
According to Good Clinical Practice guidelines, a research protocol should include detailed information on the interventions to be made, procedures to be used, measurements to be taken, and observations to be made [70]. The methodology should be standardized and clearly defined if multiple sites are engaged [70].
Technical Protocol for External Validation Studies
For algorithms intended for clinical use, external validation is a necessary step before implementation. The methodology below outlines a robust approach:
This validation workflow was exemplified in a 2025 study developing a machine learning model for predicting Drug-Induced Immune Thrombocytopenia (DITP) [67]. The researchers conducted a retrospective cohort study using electronic medical records from one hospital for model development and internal validation, achieving an AUC of 0.860 [67]. Crucially, they then performed external validation using an independent cohort from a different hospital, which confirmed model robustness with an AUC of 0.813, demonstrating generalizability despite the different patient population [67].
Research Reagent Solutions for Implementation Science
Table: Essential Methodological Tools for Implementation Research
| Research Tool | Function in Implementation Studies | Application Example |
|---|---|---|
| System Usability Scale (SUS) | Standardized 10-item questionnaire measuring perceived usability | Quantifying clinician satisfaction with new EHR interfaces [68] |
| Time-Motion Methodology | Direct observation technique measuring time spent on specific tasks | Establishing baseline workflow efficiency pre- and post-implementation |
| Light Gradient Boosting Machine (LightGBM) | Machine learning algorithm for predictive model development | Creating clinical prediction models using structured EHR data [67] |
| SHAP (SHapley Additive exPlanations) | Method for interpreting machine learning model predictions | Identifying key clinical features driving algorithm decisions [67] |
| Mixed Methods Appraisal Tool (MMAT) | Framework for critically appraising diverse study designs | Quality assessment in scoping reviews of implementation literature [68] |
Technical Implementation Strategies
Data Migration and Interoperability Protocols
A strategic approach to data migration is essential for preserving data integrity across system transitions:
- Pre-Migration Data Audit: Begin with a comprehensive data audit to identify gaps, inconsistencies, or quality issues in the source system [69].
- Phased Migration Approach: Implement a phased rollout, starting with less critical data domains to validate processes before migrating high-stakes clinical information [69].
- Interoperability Standards: Utilize established standards like HL7 (Health Level Seven) and FHIR (Fast Healthcare Interoperability Resources) to facilitate data exchange between disparate clinical systems, including laboratories, pharmacies, and imaging centers [69].
These technical considerations directly impact validation. As noted in recent research, "Missing data stands out as the biggest source of trouble" in studies using EHR data, with selection biases, information biases, and ascertainment biases potentially weakening study validity [69].
Interface Design Specifications for Clinical Workflows
Optimizing user interface design is critical for reducing cognitive load and minimizing workflow disruptions:
These design principles directly address key usability challenges identified in clinical systems. For instance, right-aligning numeric columns enhances comparison and calculation efficiency, crucial for medication dosing or laboratory value trending [71]. Additionally, ensuring sufficient color contrast (at least 4.5:1 for standard text) is essential for accessibility in clinical environments where lighting conditions may vary [72].
Change Management and Training Protocols
Technical implementation must be paired with structured human factors approaches:
- Stakeholder Engagement: Engage clinical stakeholders early and often throughout the implementation process. A mixed team including clinicians, IT staff, and administrators helps guide the project with comprehensive input [69].
- Role-Specific Training Programs: Develop training that fits each user group, incorporating classes, online tools, and hands-on sessions. Keep support ongoing after launch, utilizing "super-users" to guide peers and share feedback [69].
- Feedback Integration Mechanisms: Establish structured ways for users to report issues and suggest changes. Review and act on feedback regularly through surveys or focus groups to build trust and enable continuous system improvement [69].
Overcoming implementation barriers in clinical workflows requires moving beyond technical solutions to embrace a comprehensive validation mindset. The distinction between internal validation (performance in controlled development environments) and external validation (performance in diverse real-world settings) provides a crucial framework for implementation science. Success requires addressing not only technical challenges like data migration and interoperability but also human factors including workflow integration, change management, and cognitive load reduction.
Future implementations should prioritize external validity by design, incorporating multi-site testing early in development, using standardized interoperability frameworks like FHIR, and adopting human-centered design principles that reflect real clinical workflows. By applying these methodologies and maintaining focus on both internal and external validation metrics, researchers and implementers can bridge the gap between technical innovation and genuine clinical utility, ultimately delivering systems that enhance rather than disrupt patient care.
Comparative Analysis: Evaluating Validation Performance Across Methodologies
Within the broader thesis on internal versus external validation research, the debate between split-sample and entire-sample methods represents a fundamental challenge in statistical learning and predictive modeling. Internal validation techniques, which use the same dataset for both model development and performance estimation, aim to provide accurate estimates of how a model will perform on new data from the same underlying population. The core dilemma centers on whether to split available data into separate training and testing sets or to utilize the entire dataset for both development and validation through resampling techniques. This comparison is particularly crucial in resource-constrained environments like drug development and clinical prediction modeling, where optimal data utilization directly impacts model reliability and translational potential [1] [73].
The theoretical foundation of this comparison rests on a fundamental trade-off: split-sample validation provides an straightforward approach to estimating performance on unseen data but reduces the effective sample size for both model development and validation. Conversely, entire-sample methods maximize data usage but require sophisticated corrections for optimism bias that arises from testing models on the same data used to build them [1]. This technical guide synthesizes current empirical evidence to inform researchers, scientists, and drug development professionals facing these methodological decisions.
Empirical Evidence and Quantitative Comparisons
Performance Stability Across Validation Methods
Recent empirical studies have systematically quantified the performance variations between different validation approaches. The instability of split-sample methods is particularly pronounced in smaller datasets, where random partitioning can lead to substantially different performance estimates.
Table 1: Performance Variation Across Validation Methods in Cardiovascular Imaging Data (n=681)
| Validation Method | AUC Range (Max-Min) | Statistical Significance (Max vs Min ROC) | Algorithm Consistency |
|---|---|---|---|
| 50/50 Split-Sample | 0.094 | p < 0.05 | Inconsistent across all algorithms |
| 70/30 Split-Sample | 0.127 | p < 0.05 | Inconsistent across all algorithms |
| Tenfold Cross-Validation | 0.019 | Not Significant | Consistent across all algorithms |
| 10× Repeated Tenfold CV | 0.006 | Not Significant | Consistent across all algorithms |
| Bootstrap Validation | 0.005 | Not Significant | Consistent across all algorithms |
Data adapted from [74] demonstrates that split-sample validation produces statistically significant differences in receiver operating characteristic (ROC) curves depending on the random seed used for data partitioning. The variation in Area Under the Curve (AUC) values exceeded 0.15 in some split-sample implementations, indicating substantial instability in performance estimates. In contrast, resampling methods like cross-validation and bootstrapping showed minimal variation (AUC range < 0.02) and no statistically significant differences between best and worst cases [74].
Large-Scale Empirical Comparison in Rare-Event Prediction
A landmark study comparing validation methods in suicide risk prediction provides compelling evidence for entire-sample approaches in large-scale applications. Using a dataset of over 13 million mental health visits with a rare outcome (23 suicide events per 100,000 visits), researchers directly compared split-sample and entire-sample validation performance against a prospective validation standard [73].
Table 2: Large-Scale Rare-Event Prediction Performance (Random Forest Models)
| Validation Approach | Estimation Sample | Validation Method | AUC (95% CI) | Agreement with Prospective Performance |
|---|---|---|---|---|
| Split-Sample | 50% Subset (4.8M visits) | Independent Test Set | 0.85 (0.82-0.87) | Accurate reflection |
| Entire-Sample | Full Dataset (9.6M visits) | Cross-Validation | 0.83 (0.81-0.85) | Accurate reflection |
| Entire-Sample | Full Dataset (9.6M visits) | Bootstrap Optimism Correction | 0.88 (0.86-0.89) | Overestimation |
This study demonstrated two critical findings: first, models built using the entire sample showed equivalent prospective performance (AUC = 0.81) to those built on a 50% split, justifying the use of all available data for model development. Second, while both split-sample testing and cross-validation provided accurate estimates of future performance, bootstrap optimism correction significantly overestimated model performance in this rare-event context [73].
Detailed Experimental Protocols
Split-Sample Validation Protocol
The standard split-sample approach follows a structured methodology:
Random Partitioning: The complete dataset D is randomly divided into two mutually exclusive subsets: training set Dtrain (typically 50-80% of observations) and testing set Dtest (remaining 20-50%) [73] [74].
Stratification: For classification problems, stratification ensures consistent distribution of class labels across training and testing partitions. This is particularly important for imbalanced datasets [74].
Model Development: The prediction model M is developed exclusively using D_train, including all steps of feature selection, parameter tuning, and algorithm selection.
Performance Assessment: Model M is applied to Dtest to compute performance metrics (AUC, accuracy, calibration). No aspects of model development may use information from Dtest.
Implementation Considerations:
- Multiple random splits (typically 100) are recommended to assess stability [74].
- Disappointing results in the test sample often lead to "re-dos" with different splits, introducing bias [31].
- After validation, wise practitioners recombine data to build the final model, but this final model then lacks validation [31].
Entire-Sample Validation with Resampling
Entire-sample methods use the complete dataset for both development and validation while accounting for optimism:
Cross-Validation Protocol [73] [74]:
- Partitioning: Dataset D is divided into k mutually exclusive folds (typically k=5 or k=10).
- Iterative Training: For each fold i (i=1 to k):
- Training set: All folds except i
- Validation set: Fold i
- Model Mi is developed on the training set
- Performance Pi is assessed on the validation set
- Performance Aggregation: Overall performance is calculated as the average of P_i across all k folds.
- Final Model: A model M_final is developed on the entire dataset D.
- Stability Enhancement: For rare events or small samples, repeated cross-validation (e.g., 5×5-fold) provides more stable estimates [73].
Bootstrap Optimism Correction Protocol [73] [31]:
- Bootstrap Sampling: Draw B bootstrap samples (typically B=200) from D with replacement.
- Model Development: For each bootstrap sample b, develop model M_b.
- Optimism Calculation: For each Mb:
- Calculate performance Pb on bootstrap sample b
- Calculate performance Pborig on the original dataset D
- Optimism Ob = Pb - Pborig
- Average Optimism: Compute the average optimism O_avg across all B samples.
- Corrected Performance: Apply the optimism correction to the apparent performance: Pcorrected = Papparent - O_avg.
Practical Recommendations and Applications
Decision Framework for Method Selection
Based on empirical evidence, selection between split-sample and entire-sample approaches should consider:
Sample Size Considerations:
- n < 1,000: Resampling methods strongly preferred due to instability of data splitting [31].
- 1,000 < n < 20,000: Resampling methods generally superior; split-sample requires high signal-to-noise ratio [31].
- n > 20,000: Split-sample becomes more viable, but resampling still preferred for efficient data use [73] [31].
Problem Domain Considerations:
- Rare Events (<1% prevalence): Entire-sample with cross-validation recommended [73].
- High-Dimensional Data (p >> n): Resampling essential to account for feature selection uncertainty [31].
- Drug Response Prediction: Specialized splits (drug-blind, cell-line-blind) required to match application scenarios [75].
Domain-Specific Applications
Clinical Prediction Models: For suicide risk prediction with rare events and large samples, entire-sample approach with cross-validation provided accurate performance estimates while maximizing statistical power [73].
Cardiovascular Imaging: With moderate sample sizes (n=681-2,691), resampling methods demonstrated superior stability compared to split-sample approaches [74].
Drug Development: In drug response prediction, the pair-input nature of data (drug-cell line pairs) requires specialized splitting strategies (drug-blind, cell-line-blind) that align with the intended application scenario [75].
Visualization of Validation Workflows
Diagram 1: Split-Sample vs Entire-Sample Validation Workflows
The Researcher's Toolkit: Essential Methodological Components
Table 3: Essential Components for Validation Research
| Component | Function | Implementation Examples |
|---|---|---|
| Stratification | Maintains outcome distribution across splits | StratifiedKfold in scikit-learn [74] |
| Resampling Methods | Efficient data reuse for validation | Bootstrap, k-fold cross-validation [73] [31] |
| Performance Metrics | Quantifies predictive accuracy | AUC, calibration, sensitivity, PPV [73] |
| Optimism Correction | Adjusts for overfitting | Bootstrap optimism correction [73] [31] |
| Stability Assessment | Evaluates method robustness | Multiple random seeds, AUC range [74] |
Empirical evidence strongly supports entire-sample validation with resampling methods over split-sample approaches for most practical scenarios. The critical advantage of entire-sample methods lies in their superior data utilization, providing more stable performance estimates while maintaining accuracy against prospective standards. Split-sample validation remains relevant in very large samples or when true external validation is feasible, but its instability in small-to-moderate samples and inefficient data use limit its practical utility. For researchers and drug development professionals, the choice between these approaches should be guided by sample size, outcome prevalence, and the intended application scenario of the predictive model.
Benchmarking Bootstrap Correction Against Cross-Validation Results
Within the broader framework of internal versus external validation research, selecting an appropriate internal validation strategy is a critical step in developing robust statistical and machine learning models. Internal validation techniques aim to provide a realistic estimate of a model's performance on unseen data, using only the dataset at hand, thereby bridging the gap between apparent performance and expected external performance [76]. Among the most prominent methods for this purpose are bootstrap correction and cross-validation. While both techniques use resampling to assess model performance, their underlying philosophies and operational mechanisms differ significantly [77]. This technical guide provides an in-depth comparison of these methods, focusing on their theoretical foundations, implementation protocols, and relative performance across various data scenarios, with a particular emphasis on applications in scientific and drug development research.
Core Concepts and Fundamental Differences
Cross-Validation: Structured Data Partitioning
Cross-validation (CV) operates on the principle of partitioning data into complementary subsets. In the most common implementation, k-Fold Cross-Validation, the dataset is divided into k equal-sized folds. The model is trained on k-1 folds and validated on the remaining fold. This process is repeated k times, with each fold serving as the validation set once [77]. The final performance estimate is the average across all iterations. Leave-One-Out Cross-Validation (LOOCV) represents an extreme case where k equals the number of data points, providing a nearly unbiased but computationally expensive estimate [77]. Stratified k-Fold Cross-Validation preserves the distribution of target classes in each fold, making it particularly useful for imbalanced datasets [77].
Bootstrap Methods: Resampling with Replacement
Bootstrap techniques, in contrast, assess model performance by drawing random samples with replacement from the original dataset. A key concept is the "optimism" bias—the difference between a model's performance on the data it was trained on versus new data [76] [78]. The standard bootstrap creates multiple resampled datasets (typically 100-200), each the same size as the original but containing duplicate instances due to replacement. About 63.2% of the original data points appear in each bootstrap sample on average, with the remaining 36.8% forming the out-of-bag (OOB) set for validation [79]. Several advanced bootstrap corrections have been developed:
- Harrell's Bootstrap Optimism Correction: Directly estimates and subtracts optimism bias [76] [78].
- Bootstrap .632: Weighted average of apparent performance (36.8%) and OOB performance (63.2%) [79] [76].
- Bootstrap .632+: Enhanced version that accounts for the no-information error rate, performing better with overfit models [79] [76].
Table 1: Fundamental Characteristics of Bootstrap and Cross-Validation Methods
| Aspect | Cross-Validation | Bootstrapping |
|---|---|---|
| Core Principle | Data splitting without replacement | Resampling with replacement |
| Data Usage | Mutually exclusive folds | Overlapping samples with duplicates |
| Typical Iterations | 5-10 folds | 100-1000 resamples |
| Primary Output | Performance estimate | Performance estimate with uncertainty |
| Computational Load | Moderate (k model fits) | High (100s-1000s of model fits) |
| Key Advantages | Lower variance, good for model comparison | Better for small datasets, variance estimation |
Quantitative Performance Benchmarking
Simulation Studies in Clinical Prediction Models
Extensive simulation studies comparing bootstrap and cross-validation methods have been conducted across various data conditions. In one comprehensive evaluation using the GUSTO-I trial dataset with multivariable prediction models, researchers examined three bootstrap-based methods (Harrell's correction, .632, and .632+) across different modeling strategies including conventional logistic regression, stepwise selection, Firth's penalization, and regularized regression (ridge, lasso, elastic-net) [76].
The results revealed that under relatively large sample settings (events per variable ≥ 10), the three bootstrap-based methods were comparable and performed well. However, in small sample settings, all methods exhibited biases with inconsistent directions and magnitudes. Harrell's and .632 methods showed overestimation biases when event fractions became larger, while the .632+ method demonstrated slight underestimation bias with very small event fractions [76].
Table 2: Performance Comparison Across Sample Sizes and Scenarios
| Validation Method | Small Samples (n < 100) | Large Samples (EPV ≥ 10) | High-Dimensional Settings | Structured Data (Time-to-Event) |
|---|---|---|---|---|
| k-Fold CV (k=5/10) | Moderate bias, stable | Low bias, efficient | Recommended [4] | Good stability [4] |
| Repeated CV | Reduced bias, higher variance | Optimal balance | Limited evidence | Limited evidence |
| Harrell's Bootstrap | Overestimation bias [76] | Well-performing [76] | Over-optimistic [4] | Variable performance |
| Bootstrap .632 | Overestimation bias [76] | Well-performing [76] | Limited evidence | Overly pessimistic [4] |
| Bootstrap .632+ | Slight underestimation [76] | Well-performing [76] | Limited evidence | Overly pessimistic [4] |
| Nested CV | Computationally intensive | Computationally intensive | Recommended [4] | Performance fluctuations [4] |
High-Dimensional and Time-to-Event Settings
Research specifically addressing high-dimensional settings (where predictors far exceed samples) provides additional insights. A simulation study based on transcriptomic data from head and neck tumors (n=76 patients) compared internal validation strategies for Cox penalized regression models with disease-free survival endpoints [4].
The findings indicated that conventional bootstrap was over-optimistic in these settings, while the 0.632+ bootstrap was overly pessimistic, particularly with small samples (n=50 to n=100). K-fold cross-validation and nested cross-validation demonstrated improved performance with larger sample sizes, with k-fold cross-validation showing greater stability. Nested cross-validation exhibited performance fluctuations depending on the regularization method for model development [4].
Experimental Protocols and Methodologies
Implementing k-Fold Cross-Validation
The standard k-fold cross-validation protocol follows these methodological steps [77]:
- Data Preparation: Randomize the dataset and determine the value of k (typically 5 or 10 for bias-variance trade-off).
- Folding: Split the data into k approximately equal-sized folds, ensuring stratification for imbalanced datasets.
- Iteration: For each fold i (i=1 to k):
- Designate fold i as the validation set.
- Combine the remaining k-1 folds as the training set.
- Train the model on the training set.
- Calculate performance metrics on the validation set.
- Aggregation: Compute the final performance estimate as the average of all k validation metrics.
For repeated k-fold cross-validation, the entire process is repeated multiple times (e.g., 50-100) with different random splits, and results are aggregated across all repetitions [79].
Implementing Bootstrap Optimism Correction
The Efron-Gong optimism bootstrap follows this detailed protocol [24] [78]:
- Initial Model Fitting: Fit the model to the entire dataset (n observations) and compute the apparent performance measure, θ.
- Bootstrap Resampling: For each bootstrap iteration b (b=1 to B, where B=100-300):
- Draw a bootstrap sample of size n by sampling with replacement.
- Fit the model to the bootstrap sample.
- Calculate the performance measure on the bootstrap sample, θb.
- Calculate the performance measure on the original dataset, θw.
- Compute the optimism for iteration b: Ob = θb - θ_w.
- Optimism Calculation: Compute the average optimism: Ō = (1/B) × ΣO_b.
- Bias-Corrected Performance: Calculate the optimism-corrected measure: θ_corrected = θ - Ō.
This method directly estimates and corrects for the overfitting bias, providing a more realistic performance estimate for new data [78].
Figure 1: Bootstrap Optimism Correction Workflow
Protocol for Comparative Benchmarking Studies
To conduct a rigorous benchmark comparing bootstrap and cross-validation methods:
Data Generation: Simulate multiple datasets with known underlying relationships, varying:
Model Training: Apply identical model specifications across methods:
- Use consistent preprocessing and feature engineering
- Maintain identical hyperparameters where applicable
- Implement the same model selection procedures
Performance Assessment: Evaluate using multiple metrics:
Comparison Framework:
- Compute bias: average difference between estimated and true performance
- Assess variance: variability of performance estimates across replicates
- Calculate root mean squared error (RMSE): combined measure of bias and variance [76]
Figure 2: k-Fold Cross-Validation Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Software Tools and Packages for Implementation
| Tool/Package | Primary Function | Implementation Details | Use Case |
|---|---|---|---|
| R rms package | Bootstrap validation | validate() function implements Efron-Gong optimism bootstrap [78] |
Comprehensive model validation |
| R caret package | Cross-validation | trainControl() method for k-fold and repeated CV [57] |
Model training and tuning |
| R glmnet package | Regularized regression | Built-in CV for hyperparameter tuning [76] | High-dimensional data |
| Python scikit-learn | Cross-validation | cross_val_score and KFold classes [77] |
General machine learning |
| R boot package | Bootstrap resampling | boot() function for custom bootstrap procedures [24] |
Custom validation schemes |
| Custom simulation code | Method comparison | Tailored code for specific benchmarking needs [4] | Research studies |
Interpretation Guidelines and Decision Framework
Method Selection Criteria
Choosing between bootstrap and cross-validation methods depends on several factors:
- Dataset Size: For small datasets (n<100), bootstrap methods (particularly .632+) often perform better, while k-fold CV is preferred for larger datasets [79] [76].
- Performance Metrics: When using discontinuous scoring rules or accuracy measures, bootstrap .632/+ methods may have advantages [79].
- Computational Resources: Repeated k-fold CV (50-100 repetitions) provides precision but requires substantial computation; bootstrap methods (200-400 resamples) can be more efficient [79].
- High-Dimensional Settings: For p>>n scenarios, k-fold and nested cross-validation are generally recommended over bootstrap methods [4].
- Uncertainty Quantification: When confidence intervals for performance estimates are needed, bootstrap methods provide more direct approaches [78].
Reporting Standards and Best Practices
Comprehensive reporting of internal validation results should include:
- Method Specification: Clearly state the type of bootstrap or CV used, including number of resamples/folds and repetitions.
- Performance Estimates: Report both apparent and optimism-corrected performance measures.
- Uncertainty Quantification: Include confidence intervals for performance estimates where possible [78].
- Comparative Results: When benchmarking multiple methods, present results across all methods with consistent evaluation metrics.
- Computational Environment: Document software versions, packages, and key function parameters to ensure reproducibility.
Within the broader context of internal versus external validation research, both bootstrap correction and cross-validation offer robust approaches for estimating model performance. The optimal choice depends on specific research contexts: bootstrap methods, particularly the .632+ variant, show advantages in small sample scenarios and for uncertainty quantification, while k-fold cross-validation demonstrates superior stability in high-dimensional settings and for model comparison. Researchers in drug development and scientific fields should consider their specific data characteristics, performance requirements, and computational resources when selecting an internal validation strategy. Future methodological developments will likely focus on hybrid approaches and improved uncertainty quantification for both families of methods.
In-stent restenosis (ISR) remains a significant challenge in interventional cardiology, particularly in patient populations with specific comorbidities. In patients with overweight or obesity, defined by a body mass index (BMI) ≥ 25 kg/m², the prediction of ISR risk requires specialized tools due to the unique pathophysiological characteristics of this demographic [56]. This case study examines the development and internal validation of a four-predictor nomogram for ISR risk after drug-eluting stent (DES) implantation in this population, framing the analysis within the critical research context of internal versus external validation. Nomograms provide visual representations of complex statistical models, enabling clinicians to calculate individual patient risk through a straightforward points-based system [80]. The performance of such predictive models must be rigorously evaluated through both internal and external validation processes to establish clinical utility and generalizability.
Methodology and Experimental Protocols
Study Population and Design
The development of the overweight/obesity ISR nomogram employed a single-center retrospective cohort design, analyzing data from adult patients with BMI ≥ 25 kg/m² receiving first-time DES implantation between 2018 and 2023 [56]. This temporal frame ensures contemporary procedural techniques and medication protocols are represented. The study implemented strict inclusion and exclusion criteria to maintain cohort homogeneity, focusing specifically on the high BMI population that presents distinct metabolic challenges potentially influencing restenosis pathways.
ISR was precisely defined as ≥ 50% diameter stenosis within the stent or within 5 mm of its edges on follow-up angiography, adhering to standard cardiology endpoint definitions [56]. This objective imaging-based endpoint reduces measurement bias and enhances reproducibility across studies. The study employed a 70/30 random split for creating training and validation cohorts, ensuring sufficient sample size in both sets for model development and initial validation.
Predictor Selection and Model Development
The researchers utilized a prespecified clinical approach for predictor selection, incorporating four key variables into the multivariable logistic regression model:
- Smoking status (current or former)
- Diabetes mellitus (diagnosed)
- Total stent length (continuous variable)
- Stent diameter (continuous variable)
These predictors were selected based on clinical plausibility and previous research associations with restenosis pathways [56]. The modeling approach employed logistic regression, a standard statistical technique for binary outcomes like ISR occurrence. The resulting nomogram translates the regression coefficients into a user-friendly points system for clinical implementation.
Validation Methods and Statistical Analysis
The validation protocol incorporated multiple sophisticated statistical techniques to evaluate model performance thoroughly:
- Discrimination ability: Assessed using the C-index (equivalent to the area under the ROC curve for binary outcomes) in both training and validation sets
- Calibration: Evaluated through calibration plots accompanied by Hosmer-Lemeshow goodness-of-fit testing
- Resampling validation: Implemented via bootstrapping techniques to estimate internal validity and potential overfitting
- Clinical utility: Assessed through decision curve analysis (DCA) to quantify net benefit across different risk thresholds
This comprehensive validation strategy follows emerging standards in clinical prediction model development, addressing both statistical performance and practical clinical applicability [56] [81].
Results and Performance Metrics
Study Cohort Characteristics
The study included 468 high BMI patients, among whom 49 experienced ISR events, yielding an overall incidence rate of approximately 10.5% [56]. This sample size exceeds minimum requirements for prediction model development, with the event per variable (EPV) ratio well above the recommended threshold of 10 events per predictor variable, providing sufficient statistical power for reliable model estimation.
Table 1: Key Quantitative Findings from the Overweight/Obesity ISR Nomogram Study
| Metric | Training Cohort (70%) | Validation Cohort (30%) | Overall Performance |
|---|---|---|---|
| Sample Size | 328 patients | 140 patients | 468 patients |
| ISR Events | Not specified | Not specified | 49 events (10.5%) |
| C-index/AUC | 0.753 | 0.729 | 0.741 (average) |
| Key Predictors | Smoking, Diabetes, Stent Length, Stent Diameter | ||
| Calibration | Good fit (calibration plots) | Good fit (calibration plots) | Consistent across sets |
| Clinical Utility | Positive net benefit (DCA) | Positive net benefit (DCA) | Clinically useful |
Model Performance and Clinical Utility
The nomogram demonstrated strong predictive performance with C-index values of 0.753 in the training set and 0.729 in the validation set [56]. This minimal performance degradation between training and validation suggests limited overfitting and robust internal validity. The calibration curves indicated good agreement between predicted probabilities and observed outcomes, further supporting model reliability.
Decision curve analysis revealed positive net benefit across a range of clinically relevant probability thresholds, indicating that using the nomogram for clinical decisions would provide better outcomes than default strategies of treating all or no patients [56]. This analytical approach moves beyond traditional discrimination measures to evaluate practical clinical value, addressing whether the model would improve patient outcomes if implemented in practice.
Comparative Analysis with Other Nomogram Studies
Table 2: Comparison with Other Vascular Nomogram Studies
| Study | Clinical Context | Predictors | Sample Size | C-index | Validation Status |
|---|---|---|---|---|---|
| Overweight/Obesity ISR [56] | ISR after DES in BMI ≥25 | Smoking, Diabetes, Stent length, Stent diameter | 468 | 0.753 (internal) | Internal validation only |
| Peripheral Artery ISR [80] | ISR after iliac/femoral stenting | Diabetes, Hyperlipidemia, Hyperfibrinogenemia, Below-knee run-offs | 237 | 0.856 (internal) | Internal validation only |
| MAFLD in Obese Children [81] | Fatty liver disease screening | Age, Gender, BMI Z-score, WC, HOMA-IR, ALT | 2,512 | 0.874 (internal) | Internal validation only |
| SAP with Pneumonia [82] | Mortality prediction in pancreatitis | BUN, RDW, Age, SBP, HCT, WBC | 220 (training) | Comparable to SOFA/APACHE II | External validation using MIMIC-IV database |
The comparative analysis reveals consistent methodological approaches across nomogram studies, particularly in predictor selection, sample size considerations, and internal validation techniques. The peripheral artery ISR nomogram demonstrated higher discriminative ability (C-index 0.856), potentially due to different pathophysiology or more definitive endpoint measures [80]. Notably, the SAP with pneumonia model underwent external validation using the MIMIC-IV database, providing stronger evidence for generalizability beyond the development cohort [82].
The Internal vs. External Validation Framework
Internal Validation Strengths and Limitations
The overweight/obesity ISR nomogram underwent comprehensive internal validation using the hold-out method (70/30 split) combined with bootstrapping techniques [56]. This approach provides reasonable assurance that the model performs well on similar patients from the same institution and protects against overfitting. The minimal difference between training and validation C-index values (0.753 vs. 0.729) suggests good internal consistency.
However, internal validation alone cannot establish model transportability to different settings, patient populations, or clinical practice patterns. The single-center design inherently limits demographic and practice variability, potentially embedding local characteristics into the model. This represents a significant limitation for generalizability without further validation.
External Validation Imperatives
External validation requires testing the model on entirely separate datasets from different institutions, geographical regions, or temporal periods [82]. The SAP with pneumonia nomogram exemplifies this approach through validation using the MIMIC-IV database, demonstrating model performance in distinct clinical environments [82].
For the overweight/obesity ISR nomogram, external validation remains pending, as acknowledged by the authors [56]. This represents a critical next step before widespread clinical implementation can be recommended. Future validation should include diverse healthcare settings, ethnic populations, and practice patterns to establish true generalizability.
Visualization of Nomogram Development Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Nomogram Development and Validation
| Category | Item/Technique | Specific Application | Function in Research |
|---|---|---|---|
| Data Collection | Electronic Health Records (EHR) | Patient demographic and clinical data | Source of predictor variables and outcomes |
| Angiography Imaging Systems | ISR assessment (≥50% stenosis) | Gold-standard endpoint determination | |
| Laboratory Information Systems | Biomarker data collection | Source of continuous laboratory values | |
| Statistical Analysis | R Software (v4.2.0+) | Data analysis and modeling | Primary statistical computing environment |
| Logistic Regression | Model development | Statistical technique for binary outcomes | |
rms R package |
Nomogram construction | Creates visual prediction tool from model | |
| Validation Tools | Bootstrapping Algorithms | Internal validation | Assesses model overfitting and stability |
| ROC Curve Analysis | Discrimination assessment | Quantifies model ability to distinguish outcomes | |
| Calibration Plots | Model accuracy evaluation | Compares predicted vs. observed probabilities | |
| Decision Curve Analysis | Clinical utility assessment | Quantifies net benefit of model-based decisions | |
| Clinical Implementation | Web-based Calculator | Nomogram deployment | Enables point-of-care risk calculation |
| Mobile Application | Clinical integration | Facilitates bedside use by clinicians |
Discussion and Future Directions
The development and internal validation of the overweight/obesity ISR nomogram represents a meaningful advancement in personalized risk prediction for this specific patient population. The model's strong discriminative ability (C-index 0.753) combined with clinical practicality through the four easily obtainable predictors positions it as a potentially valuable clinical tool. However, the single-center retrospective design and absence of external validation necessitate cautious interpretation.
Future research directions should prioritize external validation across diverse healthcare settings to establish generalizability [56]. Additionally, prospective evaluation would strengthen evidence regarding real-world performance and clinical impact. Model refinement might include incorporation of novel biomarkers or imaging parameters that could enhance predictive accuracy beyond the current four predictors.
The integration of this nomogram into clinical decision support systems represents a promising avenue for implementation research, potentially facilitating personalized follow-up schedules and targeted preventive therapies for high-risk patients. Furthermore, economic analyses evaluating the cost-effectiveness of nomogram-directed care pathways would provide valuable insights for healthcare systems considering adoption.
In conclusion, while the overweight/obesity ISR nomogram demonstrates robust internal validity and practical clinical utility, its ultimate value depends on successful external validation and prospective evaluation. This case study highlights both the methodological rigor required for clinical prediction model development and the critical importance of the validation continuum in translational research.
Assessing Transportability Across Diverse Patient Populations and Settings
The generation of robust evidence on treatment effectiveness and safety is a cornerstone of drug development and regulatory decision-making. This process requires both internal validation, which ensures that study results are valid for the specific population and setting in which the research was conducted, and external validation, which assesses whether these findings can be applied to other populations and settings. Transportability is a critical quantitative methodology within external validation research, enabling the formal extension of effect estimates from a source population to a distinct target population when there is minimal or no overlap between them [83]. This guide provides researchers and drug development professionals with in-depth technical protocols for assessing and implementing transportability to bridge evidence gaps across diverse patient populations and healthcare settings.
The need for transportability methods arises from practical challenges in clinical research. Randomized controlled trials (RCTs), while maintaining high internal validity through randomization, often employ restrictive eligibility criteria that may limit their applicability to real-world patients [84]. Furthermore, financial, logistical, and ethical constraints often make it impractical or unnecessary to duplicate research across every target population or jurisdiction [85]. Transportability methods address these challenges by providing a statistical framework for leveraging existing high-quality evidence while accounting for differences between populations, thus fulfilling evidence requirements without duplicative research efforts [83] [85].
Theoretical Foundations and Key Assumptions
Defining Transportability in the Context of Validation Research
Within the spectrum of external validation, it is crucial to distinguish between several related concepts. Generalizability concerns whether study findings can be applied to a target population of which the study population is a subsample. In contrast, transportability specifically refers to the validity of extending study findings to a target population when there is minimal or no overlap between the study and target populations [83]. This distinction becomes particularly important when applying results from U.S.-based clinical trials to patient populations in other countries, where healthcare systems, treatment patterns, and patient characteristics may differ substantially [84].
The efficacy-effectiveness gap—the observed phenomenon where patient outcomes or therapy performance in clinical trials often exceeds that in routine care—is a direct manifestation of limited external validity [84]. Transportability methods aim to quantify and address this gap by statistically adjusting for factors that differ between trial and real-world populations.
Core Identifiability Assumptions
Transportability methods rely on three key identifiability assumptions that must be met to produce valid results [83]:
Internal Validity of the Original Study: The estimated effect must equal the true average treatment effect in the source population. This requires conditional exchangeability, consistency, positivity of treatment, no interference, treatment version irrelevance, and correct model specification. RCTs are generally assumed to have internal validity due to randomization, though this can be compromised by missing data or chance imbalances [83].
Conditional Exchangeability Over Selection (S-admissibility): Also referred to as mean transportability, this assumption states that individuals in the study and target populations with the same baseline characteristics would experience the same potential outcomes under treatment and no treatment, making them exchangeable. This requires that all effect modifiers with different distributions across populations are identified, measured, and accounted for in the analysis [83].
Positivity of Selection: There must be a non-zero probability of being included in the original study for every stratum of effect modifiers needed to ensure conditional exchangeability. This ensures that there is sufficient overlap in the characteristics between populations to support meaningful comparison [83].
Methodological Approaches to Transportability
Statistical Frameworks and Algorithms
Transportability methods generally fall into three broad categories, each with distinct approaches and implementation considerations [83]:
Table 1: Comparison of Transportability Methodologies
| Method Class | Mechanism | Key Requirements | Strengths | Limitations |
|---|---|---|---|---|
| Weighting Methods | Reweights individuals in source population using inverse odds of sampling weights to reproduce effect modifier distribution of target population [83] [85] | Complete data on effect modifiers in both populations | Intuitive approach; does not require outcome modeling for target population | Sensitive to model misspecification; can produce unstable estimates with extreme weights |
| Outcome Regression Methods | Develops predictive models for outcomes based on source data, then applies to target population characteristics to estimate potential outcomes [83] [85] | Detailed clinical outcome data from source population; effect modifier data from target population | Flexible modeling of outcome relationships; efficient use of source data | Dependent on correct outcome model specification; requires comprehensive covariate data |
| Doubly-Robust Methods | Combines weighting and outcome regression approaches to create estimators that remain consistent if either component is correctly specified [83] [85] | Same data requirements as component methods | Enhanced robustness to model misspecification; potentially more precise estimates | Increased computational complexity; requires specification of both models |
Implementation Workflow
The following diagram illustrates the systematic workflow for implementing transportability analyses:
Case Study: Transporting Lung Cancer Trial Results
Experimental Protocol and Implementation
A recent study by Gupta et al. provides a comprehensive example of transportability assessment using the Lung-MAP S1400I trial (NCT02785952) as a case study [84]. This trial compared overall survival in United States patients with recurrent stage IV squamous non-small cell lung cancer randomized to receive either nivolumab monotherapy or nivolumab + ipilimumab combination therapy, finding no significant difference in mortality rates between these groups [84].
Table 2: Lung-MAP Transportability Analysis Protocol
| Protocol Component | Implementation Details |
|---|---|
| Source Population | Individual-level patient data from the Lung-MAP S1400I clinical trial (US only) [84] |
| Target Populations | Real-world populations from the US, Germany, France, England, and Japan receiving nivolumab for squamous NSCLC [84] |
| Primary Outcome | Overall survival (OS) with nivolumab monotherapy [84] |
| Effect Measure Modifiers | Baseline characteristics identified through literature review and clinical expert input; comparison with LLM-derived factors (ChatGPT/GPT-4) [84] |
| Transportability Method | Weighting and outcome regression approaches to adjust for prognostic factors between populations [84] |
| Validation Approach | Benchmark transported OS estimates against Kaplan-Meier curves from real-world studies in target countries [84] |
| Sensitivity Analyses | Assessment of unmeasured prognostic variables and index date differences (diagnosis vs. treatment initiation) [84] |
Methodological Considerations in Case Study Implementation
The transportability analysis accounted for several critical methodological challenges. The researchers recognized that differences in index dates between studies (date of diagnosis in English data vs. date of treatment initiation in other datasets) could significantly impact survival estimates and transportability validity [84]. This factor was specifically hypothesized to potentially position the English study as a negative control, helping to illuminate the limitations of statistical adjustment methods [84].
Additionally, the study incorporated a novel approach to identifying effect measure modifiers by comparing traditional methods (literature review and clinical expert input) with factors elicited from large language models (ChatGPT or GPT-3/4) [84]. This comparative analysis aimed to evaluate the reliability and efficiency of emerging AI tools in supporting transportability assessments.
Practical Considerations and Limitations
Challenges in Transportability Assessment
Despite its potential, transportability faces several significant limitations that researchers must acknowledge and address:
- Between-Country Variations: Differences in clinical guidelines, medication availability, and reimbursement statuses create substantial variability in treatment patterns across geographies [85].
- Population Heterogeneity: Demographic, lifestyle, socioeconomic, and epidemiological factors (including disease incidence and progression) differ across regions and can modify treatment effects [85].
- Data Infrastructure Disparities: Differences in data quality, completeness, and transparency across healthcare systems can affect the accuracy and reliability of transported estimates [85].
- Unmeasured Confounding: The presence of unmeasured or unknown effect modifiers limits the capacity for accurate adjustments and represents a fundamental threat to transportability validity [85].
The Scientist's Toolkit: Essential Methodological Reagents
Table 3: Key Research Reagent Solutions for Transportability Analyses
| Reagent Category | Specific Examples | Function in Transportability Assessment |
|---|---|---|
| Effect Modifier Identification | Literature reviews, clinical expert consultation, large language models (GPT-4) [84] | Identifies variables with different distributions across populations that modify treatment effects |
| Weighting Algorithms | Inverse odds of sampling weights [83] [85] | Reweights source population to match effect modifier distribution of target population |
| Outcome Modeling Techniques | Regression models, machine learning algorithms [83] [85] | Predicts potential outcomes in target population based on source population relationships |
| Sensitivity Analysis Frameworks | Unmeasured confounding assessments, model specification tests [84] | Evaluates robustness of transported estimates to assumptions and model choices |
| Data Standardization Tools | Common data models, harmonization protocols [85] | Addresses differences in data structure and quality across source and target populations |
Future Directions and Reporting Standards
The use of transportability methods for real-world evidence generation represents an emerging but promising area of research [83]. As regulatory and health technology assessment bodies increasingly encounter evidence generated through these methods, standardized reporting and validation frameworks become essential.
Transparent reporting should include thorough descriptions of data provenance, detailed assessment of data suitability, explicit handling of differences and limitations, and clear documentation of all statistical methods and assumptions [85]. Additionally, researchers should conduct comprehensive sensitivity analyses and openly discuss interpretation uncertainties and potential biases [85].
Future adoption of transportability methods will likely depend on several factors, including methodological transparency, cultural shifts among decision-makers, and more proactive promotion of the value of real-world evidence [85]. Initiatives like the European Health Data and Space Regulation may help reduce issues such as data missingness and improve protocol consistency, though they will not fully resolve structural differences in data generation across healthcare systems [85].
Transportability methods offer a powerful framework for addressing evidence gaps across diverse patient populations and healthcare settings, particularly in contexts where high-quality local data are limited or unavailable. By formally accounting for differences between source and target populations, these approaches can enhance the external validity of clinical trial results and real-world evidence, potentially accelerating patient access to beneficial therapies while reducing redundant research efforts.
Successful implementation requires careful attention to core identifiability assumptions, appropriate selection of statistical methods, and comprehensive sensitivity analyses. As the field evolves, increased methodological standardization, transparent reporting, and broader acceptance by regulatory and HTA bodies will be essential to fully realize the potential of transportability for improving evidence generation and healthcare decision-making globally.
The development of clinical prediction models follows a rigorous pathway from initial conception to real-world application. Within the broader thesis of internal versus external validation research, understanding the distinct roles of various validation metrics is paramount for researchers, scientists, and drug development professionals. These metrics provide the evidentiary foundation for determining whether a model possesses mere statistical elegance or genuine utility in clinical practice.
Internal validation assesses model performance using data derived from the same population used for model development, employing techniques like cross-validation or bootstrapping to estimate optimism and overfitting. In contrast, external validation evaluates whether a model's performance generalizes to entirely independent populations, settings, or healthcare systems—a crucial test for real-world applicability [86] [87]. This distinction forms the critical framework for understanding how different metrics behave across validation contexts and why comprehensive validation requires assessing multiple performance dimensions.
The following sections provide an in-depth technical examination of the three cornerstone metric categories: discrimination (Area Under the Curve, AUC), calibration, and clinical utility measures, with specific emphasis on their interpretation in both internal and external validation paradigms.
Core Metric 1: Discrimination and the Area Under the Curve (AUC)
Technical Foundation and Interpretation
Discrimination refers to a model's ability to distinguish between patients who experience an outcome from those who do not. The Area Under the Receiver Operating Characteristic Curve (AUC-ROC, commonly termed AUC or C-statistic) quantifies this capability across all possible classification thresholds [58] [88].
The AUC represents the probability that a randomly selected individual with the outcome will have a higher predicted risk than a randomly selected individual without the outcome. Values range from 0.5 (no discrimination, equivalent to random chance) to 1.0 (perfect discrimination) [88]. In clinical prediction studies, AUC values are typically interpreted as follows: 0.5-0.7 (poor to moderate discrimination), 0.7-0.8 (acceptable discrimination), 0.8-0.9 (excellent discrimination), and >0.9 (outstanding discrimination) [89] [90].
AUC in Internal Versus External Validation
A consistent pattern emerges across validation studies: models typically demonstrate lower discrimination during external validation compared to internal validation. For instance, a machine learning model for predicting non-home discharge after total knee arthroplasty showed AUCs of 0.83-0.84 during internal validation but maintained excellent performance (AUC 0.88-0.89) during external validation [86]. Similarly, a stress urinary incontinence prediction model demonstrated an AUC of 0.94 in the training set but 0.77 in the external validation set [89].
This expected attenuation stems from differences in case-mix, clinical practices, and data collection methods between development and validation cohorts. The magnitude of this performance drop serves as a key indicator of model generalizability.
Figure 1: AUC Performance Across Validation Types. Example from a total knee arthroplasty discharge prediction model showing maintained excellence during external validation [86].
Core Metric 2: Calibration and Its Critical Importance
Understanding Calibration Metrics
While discrimination assesses a model's ranking ability, calibration evaluates how well the predicted probabilities align with actual observed outcomes. A well-calibrated model predicts a 20% risk for events that actually occur 20% of the time across the risk spectrum [91] [87].
Calibration is typically assessed through:
- Calibration-in-the-large: Intercept assessment indicating systematic over- or under-prediction
- Calibration slope: Ideal value of 1.0, with values <1.0 indicating overfitting and >1.0 indicating underfitting
- Calibration plots: Visual representation of predicted versus observed probabilities
- Hosmer-Lemeshow test: Statistical test for calibration goodness-of-fit (non-significant p-value indicates good calibration) [89]
- Brier score: Comprehensive measure of both discrimination and calibration, where lower values indicate better performance [90]
The Calibration-Recalibration Process in External Validation
Calibration frequently deteriorates during external validation due to differences in outcome incidence or patient characteristics between populations. The cisplatin-associated acute kidney injury (C-AKI) prediction study exemplifies this phenomenon, where both the Motwani and Gupta models "exhibited poor initial calibrations, which improved after recalibration" for application in a Japanese population [91].
Recalibration methods adjust the baseline risk or overall model to fit new population characteristics while preserving the original model's discriminatory structure. This process is often essential for implementing externally developed models in local clinical practice.
Table 1: Calibration Assessment Methods and Interpretation
| Method | Ideal Value | Interpretation | Common External Validation Pattern |
|---|---|---|---|
| Calibration Slope | 1.0 | <1.0: Overfitting>1.0: Underfitting | Often <1.0 indicating overfitting to development data |
| Calibration Intercept | 0.0 | >0: Under-prediction<0: Over-prediction | Varies by population incidence differences |
| Brier Score | 0.0 (perfect) | Lower = better | Typically increases in external validation |
| Hosmer-Lemeshow Test | p > 0.05 | Non-significant = good calibration | Often becomes significant in external validation |
Core Metric 3: Clinical Utility and Decision Curve Analysis
Moving Beyond Statistical Performance
A model demonstrating excellent discrimination and calibration may still lack clinical value if it doesn't improve decision-making. Clinical utility measures address this gap by quantifying the net benefit of using a prediction model compared to default strategies [91] [92].
Decision Curve Analysis (DCA) has emerged as the predominant method for evaluating clinical utility across different probability thresholds. DCA calculates the net benefit by weighting the true positives against the false positives, accounting for the relative harm of missed treatments versus unnecessary interventions [91] [89].
Application in Validation Studies
In the C-AKI prediction study, DCA demonstrated that the recalibrated Gupta model "yielded a greater net benefit" and showed "the highest clinical utility in severe C-AKI" compared to alternative approaches [91]. Similarly, a mortality prediction model for older women with dementia demonstrated "net benefit across probability thresholds from 0.24 to 0.88," supporting its utility for palliative care decision-making [92].
Figure 2: From Statistical Performance to Clinical Utility. A model must demonstrate value beyond traditional metrics to influence clinical practice [91] [92].
Integrated Validation Protocols and Experimental Methodologies
Comprehensive Validation Framework
Robust validation requires a systematic approach assessing all three metric categories across appropriate datasets. The following integrated protocol outlines key methodological considerations:
Internal Validation Phase:
- Apply k-fold cross-validation (typically 5-10 folds) or bootstrapping to estimate optimism
- Evaluate discrimination (AUC), calibration (slope, intercept, plots), and begin clinical utility assessment (DCA)
- For smaller datasets (<1000 events), cross-validation is preferred over single split-sample approaches due to greater precision [87]
External Validation Phase:
- Test model on completely independent cohort from different institutions, regions, or time periods
- Assess same metric triad but expect attenuated performance, particularly in calibration
- Perform recalibration if needed while preserving original model structure
- Evaluate clinical utility in context of local practice patterns and decision thresholds
Case Example: Cisplatin-AKI Prediction Model Validation
A recent study exemplifying this comprehensive approach evaluated two C-AKI prediction models (Motwani and Gupta) in a Japanese cohort of 1,684 patients [91]. The validation protocol included:
Discrimination Comparison: The Gupta and Motwani models showed similar AUC for any C-AKI (0.616 vs. 0.613, p=0.84), but the Gupta model demonstrated superior discrimination for severe C-AKI (AUC 0.674 vs. 0.594, p=0.02)
Calibration Assessment: Both models showed poor initial calibration in the Japanese population, requiring recalibration for clinical use
Clinical Utility Evaluation: DCA demonstrated that the recalibrated Gupta model provided the highest net benefit for severe C-AKI prediction
This systematic approach revealed that while both models maintained some discriminatory ability, the Gupta model offered particular advantages for predicting severe outcomes and required recalibration before local implementation.
Table 2: Experimental Protocol for Comprehensive Model Validation
| Validation Phase | Primary Methods | Key Metrics | Interpretation Focus |
|---|---|---|---|
| Internal Validation | 5-10 fold cross-validation; Bootstrapping | AUC with confidence intervals; Calibration slope; Optimism-adjusted metrics | Overfitting assessment; Initial performance benchmark |
| External Validation | Independent cohort testing; Recalibration analysis | AUC comparison; Calibration plots; Decision Curve Analysis | Generalizability assessment; Transportability to new settings |
| Clinical Utility | Decision Curve Analysis; Sensitivity analysis | Net Benefit; Threshold probability ranges | Clinical impact; Comparative effectiveness vs. standard approaches |
The Scientist's Toolkit: Essential Methodological Reagents
Table 3: Essential Methodological Reagents for Validation Studies
| Tool/Technique | Primary Function | Application Context |
|---|---|---|
| LASSO Regression | Feature selection with regularization; Prevents overfitting by penalizing coefficient size | Model development phase; Identifying strongest predictors from candidate variables [89] [90] |
| k-Fold Cross-Validation | Internal validation; Robust performance estimation in limited samples | Preferred over single holdout for datasets <1000 events; Typically 5-10 folds [87] |
| Decision Curve Analysis (DCA) | Clinical utility quantification; Net benefit calculation across threshold probabilities | Essential for demonstrating clinical value beyond statistical performance [91] [92] |
| SHAP Analysis | Model interpretability; Feature importance assessment at global and local levels | Explaining complex model predictions; Identifying key drivers [90] |
| Multiple Imputation | Handling missing data; Preserving sample size while reducing bias | Addressing missing data <30%; Superior to complete-case analysis [91] [90] |
| Stratified Sampling | Maintaining class distribution in validation splits; Preventing selection bias | Crucial for imbalanced datasets; Ensures representative case mix [88] |
The journey from model development to clinical implementation requires meticulous attention to the triad of validation metrics: discrimination, calibration, and clinical utility. These metrics provide complementary insights that collectively determine a model's real-world viability. Through systematic internal and external validation employing these measures, researchers can distinguish between statistically elegant but clinically irrelevant models and those with genuine potential to improve patient care.
The evidence consistently demonstrates that external validation remains the definitive test for model generalizability, typically revealing calibration drift and attenuated discrimination compared to internal performance. This performance gap underscores why models developed in one population require rigorous external testing before implementation in new settings. Furthermore, the emerging emphasis on clinical utility metrics like decision curve analysis represents a critical evolution in validation science—ensuring that models not only predict accurately but also improve decisions and outcomes in clinical practice.
For drug development professionals and clinical researchers, this comprehensive validation framework provides a methodological foundation for evaluating predictive models across the development pipeline, from initial discovery through to implementation science and post-marketing surveillance.
Validation evidence serves as the critical bridge between internal research findings and external regulatory acceptance. In the context of FDA approval, validation is not a single event but a comprehensive, evidence-driven process that demonstrates a drug product is consistently safe, effective, and of high quality. The year 2025 has brought significant evolution to this landscape, with the FDA increasingly emphasizing science- and risk-based approaches over prescriptive checklists, alongside growing adoption of advanced digital technologies and alternative testing methods [66] [93]. This guide examines the specific evidence requirements across key validation domains, providing researchers and drug development professionals with a structured framework for building compelling validation packages that successfully navigate the transition from internal verification to external regulatory endorsement.
The distinction between internal and external validation is particularly crucial. Internal validation establishes that a process, method, or system performs reliably under controlled conditions within an organization, while external validation demonstrates that this performance meets regulatory standards for public health protection. This whitepaper details the evidence required for this external regulatory acceptance, focusing on the specific expectations of the U.S. Food and Drug Administration in the current regulatory climate.
Analytical Method Validation: ICH Q2(R2) and Q14 Framework
Analytical method validation provides the foundational data demonstrating that quality testing methods are reliable, accurate, and suitable for their intended purpose. The recent simultaneous introduction of ICH Q2(R2) on validation and ICH Q14 on analytical procedure development represents a significant modernization, shifting the paradigm from a one-time validation event to a continuous lifecycle management approach [93].
Core Validation Parameters and Evidence Requirements
The following table summarizes the quantitative evidence required for validating analytical methods according to ICH Q2(R2), which has been adopted by the FDA. These parameters form the core evidence package submitted in New Drug Applications (NDAs) and Abbreviated New Drug Applications (ANDAs) [93].
Table 1: Core Analytical Method Validation Parameters per ICH Q2(R2)
| Validation Parameter | Experimental Methodology | Acceptance Criteria Evidence |
|---|---|---|
| Accuracy | Analyze samples with known analyte concentrations (e.g., spiked placebo) across the specification range. | Report percent recovery of the known amount or difference between mean and accepted true value along with confidence intervals. |
| Precision | Repeatability: Multiple measurements of homogeneous samples by same analyst, same conditions.Intermediate Precision: Multiple measurements across different days, analysts, or equipment.Reproducibility: Measurements across different laboratories (often for standardization). | Report relative standard deviation (RSD) for each level of precision. Acceptance criteria depend on method stage and complexity. |
| Specificity | Chromatographic: Resolve analyte from closely related impurities or placebo components.Spectroscopic: Demonstrate no interference from other components. | Provide chromatograms or spectra showing baseline separation or lack of interference. Peak purity tests can be used. |
| Linearity | Prepare and analyze a minimum of 5 concentrations spanning the claimed range. | Report correlation coefficient, y-intercept, slope of regression line, and residual sum of squares. A visual plot of response vs. concentration is required. |
| Range | The interval between upper and lower analyte concentrations demonstrating suitable linearity, accuracy, and precision. | Evidence that the range encompasses the intended use, typically from 80% to 120% of test concentration for assay. |
| Limit of Detection (LOD) | Signal-to-Noise: Compare measured signals from samples with known low concentrations with blank samples.Standard Deviation: Based on the standard deviation of the response and the slope of the calibration curve. | Report the lowest concentration where the analyte can be reliably detected. Typically, a signal-to-noise ratio of 3:1 or 2:1. |
| Limit of Quantitation (LOQ) | Signal-to-Noise: Compare measured signals from samples with known low concentrations with blank samples.Standard Deviation: Based on the standard deviation of the response and the slope of the calibration curve. | Report the lowest concentration that can be quantified with acceptable accuracy and precision. Typically, a signal-to-noise ratio of 10:1. Must demonstrate precision of ≤20% RSD and accuracy of 80-120%. |
| Robustness | Deliberately vary key method parameters (e.g., pH, mobile phase composition, temperature, flow rate) within a small, realistic range. | Report the effect of each variation on method results (e.g., resolution, tailing factor). Establishes system suitability parameters to control robustness. |
The Modernized Lifecycle Approach
The introduction of the Analytical Target Profile (ATP) via ICH Q14 is a pivotal development. The ATP is a prospective summary that defines the method's intended purpose and its required performance criteria before development begins [93]. This strategic shift encourages a risk-based approach during development, where potential sources of variability are identified and controlled, leading to more robust methods and a more targeted validation study focused on the ATP's criteria.
The guidelines now describe two pathways for development and post-approval change management: a traditional (minimal) approach and an enhanced approach. The enhanced approach, while requiring a deeper understanding of the method and its limitations, provides greater flexibility for post-approval changes through an established control strategy, facilitating continuous improvement throughout the method's lifecycle [93].
Computer System and Software Validation
For software used in pharmaceutical manufacturing, quality control, or as a medical device itself, the FDA requires demonstrable validation evidence based on the system's risk level.
Software as a Medical Device (SaMD) and AI/ML
The FDA's approach to AI-enabled medical devices is guided by the Total Product Life Cycle (TPLC) framework and Good Machine Learning Practice (GMLP) principles [94]. For AI/ML models, especially those that adapt or change, the agency expects a Predetermined Change Control Plan (PCCP) outlining how the model will evolve post-market while maintaining safety and effectiveness [94]. Key evidence includes:
- Risk-Based Test Plan: Every test case must be linked to a potential hazard identified through a risk management process (per ISO 14971) [95].
- Algorithmic Validation: Evidence of performance across diverse datasets representative of the intended patient population to minimize bias.
- Data Integrity: Full adherence to ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and Available) and 21 CFR Part 11 for electronic records [66].
- Transparency and Explainability: For complex AI, especially "black box" models, evidence must demonstrate that the basis for recommendations can be understood and reviewed by clinicians, aligning with FDA guidance on Clinical Decision Support (CDS) software [94].
Validation Evidence for Regulatory Submissions
In 2025, the FDA reviews a risk-based software evidence package per the Device Software Functions (DSF) guidance, which may involve Basic or Enhanced documentation levels [95]. A complete submission must include:
- V&V Protocols and Results: Detailed documentation of unit, integration, and system-level testing, including pass/fail logs and screenshots demonstrating successful execution [95].
- Traceability Matrix: A document linking software requirements to identified hazards and corresponding test cases, proving that all risks have been mitigated [95].
- Version History: A complete audit trail of software versions submitted for review.
- Unresolved Anomalies List: A clear list of any known bugs or issues and a justification for why they do not impact safety or effectiveness [95].
Recent FDA warning letters from Q4 2024 have highlighted "demonstrable test depth" as a key deficiency, where insufficient evidence led to Additional Information requests and delays of 3–6 months [95].
Process Validation: Lifecycle Approach
Process validation provides evidence that a manufacturing process consistently produces a drug substance or product meeting its predefined quality attributes. The FDA's lifecycle approach aligns with ICH guidelines, encompassing three stages.
The Three Stages of Process Validation
Process Validation Lifecycle Stages
Stage 1: Process Design This stage focuses on gathering and documenting process knowledge and understanding. Evidence includes:
- Scale-up Models: Data linking laboratory and pilot-scale models to commercial manufacturing.
- Risk Assessments: Documentation from tools like Failure Modes and Effects Analysis (FMEA) to identify and prioritize critical process parameters (CPPs) that impact critical quality attributes (CQAs) [66].
- Design of Experiments (DoE): Multivariate experimental studies that establish the relationship between CPPs and CQAs, defining the proven acceptable range (PAR) for each parameter [66].
Stage 2: Process Qualification This stage provides evidence that the designed process is capable of reproducible commercial manufacturing.
- Facility Qualification: Evidence of proper installation (IQ) and operational qualification (OQ) of equipment and utilities [66].
- Performance Qualification (PQ): Documented execution of at least three consecutive commercial-scale batches that demonstrate the process, under established CPPs, consistently produces product meeting all CQAs [66].
Stage 3: Continued Process Verification This ongoing stage provides evidence that the process remains in a state of control during routine production.
- Monitoring Plans: Protocols for ongoing monitoring of CPPs and CQAs using statistical process control (SPC) [66].
- Real-time Data: Implementation of Process Analytical Technology (PAT) for real-time monitoring and control, facilitating a shift towards continuous manufacturing [66].
- Trend Reports: Regular analysis of data to identify adverse process trends, triggering corrective actions before they result in batch failure.
Novel Drug Approvals in 2025: A Quantitative Snapshot
The following table summarizes a selection of novel drugs approved by the FDA in 2025, illustrating the therapeutic areas and types of evidence that have successfully supported regulatory approval. This data, sourced from the FDA's official novel drug approvals page, provides context for the validation strategies discussed in this guide [96].
Table 2: Selected FDA Novel Drug Approvals in 2025
| Drug Name (Brand) | Active Ingredient | Approval Date | FDA-Approved Use on Approval Date |
|---|---|---|---|
| Voyxact | sibeprenlimab-szsi | 11/25/2025 | To reduce proteinuria in primary immunoglobulin A nephropathy in adults at risk for disease progression |
| Hyrnuo | sevabertinib | 11/19/2025 | To treat locally advanced or metastatic non-squamous non-small cell lung cancer with tumors that have activating HER2 tyrosine kinase domain activating mutations |
| Redemplo | plozasiran | 11/18/2025 | To reduce triglycerides in adults with familial chylomicronemia syndrome |
| Komzifti | ziftomenib | 11/13/2025 | To treat adults with relapsed or refractory acute myeloid leukemia with a susceptible nucleophosmin 1 mutation |
| Lynkuet | elinzanetant | 10/24/2025 | To treat moderate-to-severe vasomotor symptoms due to menopause |
| Rhapsido | remibrutinib | 9/30/2025 | To treat chronic spontaneous urticaria in adults who remain symptomatic despite H1 antihistamine treatment |
| Inluriyo | imlunestrant | 9/25/2025 | To treat ER+, HER2-, ESR1-mutated advanced or metastatic breast cancer |
| Wayrilz | rilzabrutinib | 8/29/2025 | To treat persistent or chronic immune thrombocytopenia |
| Brinsupri | brensocatib | 8/12/2025 | To treat non-cystic fibrosis bronchiectasis |
| Vizz | aceclidine | 7/31/2025 | To treat presbyopia |
| Zegfrovy | sunvozertinib | 7/2/2025 | To treat locally advanced or metastatic NSCLC with EGFR exon 20 insertion mutations |
| Journavx | suzetrigine | 1/30/2025 | To treat moderate to severe acute pain |
| Datroway | datopotamab deruxtecan-dlnk | 1/17/2025 | To treat unresectable or metastatic, HR-positive, HER2-negative breast cancer |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are critical for generating the robust validation evidence required for FDA submissions. Their selection and qualification themselves form a part of the validation narrative.
Table 3: Key Research Reagent Solutions for Validation Studies
| Reagent / Material | Critical Function in Validation | Key Qualification/Selection Criteria |
|---|---|---|
| Reference Standards | Serve as the benchmark for quantifying the analyte and determining method accuracy, linearity, and specificity. | Certified purity and identity, preferably from official sources (e.g., USP, EP). Must be traceable to a recognized standard. |
| Cell-Based Assay Systems | Used for potency testing of biologics, viral assays, and toxicology assessments. Provide functional data critical for potency and safety evidence. | Documented lineage, passage number, and absence of contamination (e.g., mycoplasma). Demonstration of reproducibility and relevance to the biological mechanism. |
| Highly Purified Water | The universal solvent and reagent for analytical and process steps. Impurities can critically interfere with results. | Meets compendial specifications (e.g., USP Purified Water or WFI). Regular monitoring for conductivity, TOC, and microbial counts. |
| Chromatographic Columns | Essential for separation-based methods (HPLC, UPLC). Performance directly impacts specificity, resolution, and precision. | Documented performance tests (e.g., plate count, tailing factor) against a standard mixture before use in validation. |
| Enzymes & Antibodies | Critical reagents for immunoassays, ELISAs, and other specific detection methods. Their quality defines method specificity. | Certificate of Analysis with documented specificity, titer, and reactivity. Validation of each new lot against the previous one. |
| Process Impurities | Used to challenge method specificity (e.g., for related substances testing) and demonstrate the ability to detect and quantify impurities. | Structurally identified and characterized compounds (e.g., synthetic intermediates, degradation products, known metabolites). |
| Animal Models | Provide in vivo data for safety (toxicology) and efficacy (pharmacology) studies, supporting the drug's intended use. | Justification of species and model relevance to human condition/physiology. Adherence to animal welfare standards (3Rs: Replace, Reduce, Refine) [97]. |
Integrated Validation Strategy: Connecting Internal and External Evidence
A successful FDA submission integrates evidence from all validation domains into a cohesive narrative. The following diagram illustrates the logical workflow for building this integrated validation strategy, connecting internal development activities to the external evidence package.
Integrated Validation Evidence Generation Workflow
Emerging Factors for 2025 and Beyond
- Adoption of Alternative Methods: The FDA's New Alternative Methods Program actively promotes alternative methods that can replace, reduce, or refine (3Rs) animal testing [97]. Evidence from qualified alternative methods (e.g., in chemico, in vitro, in silico, microphysiological systems) is increasingly accepted. For example, OECD Test Guideline No. 437 for reconstructed human cornea-like epithelium has replaced rabbit tests for eye irritation for some pharmaceuticals [97].
- Advanced Manufacturing Technologies: Validation approaches for continuous manufacturing and personalized medicines (e.g., gene therapies, biologics) require specialized evidence, including small-batch validation strategies, cold chain validation, and heightened aseptic processing controls [66].
- Regulatory and Capacity Dynamics: The FDA is undergoing significant internal changes, including staffing reductions in certain areas, which may lead to longer wait times for meetings and potentially less informal guidance [98]. This makes a complete, clear, and well-organized validation evidence package, submitted via required electronic templates like eSTAR, more critical than ever to avoid review delays [95].
Successful FDA approval in 2025 hinges on a comprehensive and strategic validation evidence package that seamlessly connects internal development data to external regulatory standards. The core success factors are the adoption of a lifecycle approach across analytical methods, processes, and software; the deep integration of risk-based principles and quality by design from the outset; and the meticulous generation of objective, auditable data that tells a compelling story of product quality, safety, and efficacy. By mastering the frameworks, parameters, and integrated strategies outlined in this guide, researchers and drug development professionals can build robust evidence packages that not only meet regulatory expectations but also efficiently bridge the gap between internal validation and external regulatory success.
Conclusion
Effective validation represents a cornerstone of reliable predictive modeling in drug development and clinical research. Through systematic comparison of methodologies, this analysis demonstrates that internal validation techniques—particularly bootstrapping and cross-validation—provide essential safeguards against overfitting, while external validation through prospective evaluation remains critical for assessing generalizability. The evolving landscape of AI-enabled technologies necessitates even more rigorous validation frameworks, including randomized controlled trials for high-impact clinical applications. Future directions should focus on developing adaptive validation approaches that accommodate rapidly evolving models, standardized validation reporting through guidelines like TRIPOD, and regulatory innovation that keeps pace with technological advancement. Ultimately, robust validation strategies are not merely statistical exercises but fundamental requirements for building trustworthy AI systems and prediction models that can safely transform patient care and therapeutic development.
References
- 1. Prediction models need appropriate internal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5578404/]
- 2. External Validation Confirms Ability of AI Model to Stratify ... [https://ascopost.com/news/november-2025/external-validation-confirms-ability-of-ai-model-to-stratify-recurrence-risk-in-early-stage-lung-cancer/]
- 3. External validation of eight different models to predict ... [https://pubmed.ncbi.nlm.nih.gov/40639207/]
- 4. Internal validation strategy for high dimensional prognosis ... [https://www.sciencedirect.com/science/article/pii/S2001037025003563]
- 5. Internal Validation of a Machine Learning-Based CDSS for ... [https://www.mdpi.com/2075-1729/15/7/1123]
- 6. Perspectives on validation of clinical predictive algorithms [https://www.nature.com/articles/s41746-023-00832-9]
- 7. Targeted validation: validating clinical prediction models in ... [https://diagnprognres.biomedcentral.com/articles/10.1186/s41512-022-00136-8]
- 8. Internal and External Validation of Machine Learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11204685/]
- 9. The validation of prediction models deserves more recognition [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-03994-3]
- 10. External validation of prognostic models: what, why, how, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7857818/]
- 11. Generalizability of Machine Learning Models: Quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9885377/]
- 12. Evaluating Prediction Model Performance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10529246/]
- 13. Development and Internal-External Validation Models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12267828/]
- 14. The importance of being external. methodological insights ... [https://www.sciencedirect.com/science/article/abs/pii/S016926072100362X]
- 15. Underfitting vs. Overfitting in Machine Learning [https://www.ayadata.ai/a-guide-to-overfitting-and-underfitting-in-machine-learning/]
- 16. Overfitting in Machine Learning Explained [https://aws.amazon.com/what-is/overfitting/]
- 17. Validation of Biomarker-based risk prediction models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3896456/]
- 18. How to Fix Overfitting and Underfitting | by Tahir | Oct, 2025 [https://medium.com/@tahirbalarabe2/how-to-fix-overfitting-and-underfitting-4cf8f383ea96]
- 19. Alzheimer's disease drug development pipeline: 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131090/]
- 20. Internal and external validity: can you apply research study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6188693/]
- 21. Validity in Clinical Research [https://www.openanesthesia.org/keywords/validity-in-clinical-research/]
- 22. Internal validation with bootstrap .632+ estimator [https://phydev.github.io/posts/bootstrap.html]
- 23. 3.1. Cross-validation: evaluating estimator performance [https://scikit-learn.org/stable/modules/cross_validation.html]
- 24. Getting Started with Bootstrap Model Validation - UVA Library [http://library.virginia.edu/data/articles/getting-started-with-bootstrap-model-validation]
- 25. Bootstrap vs. cross-validation for model performance [https://discourse.datamethods.org/t/bootstrap-vs-cross-validation-for-model-performance/2779]
- 26. Cross Validation in Machine Learning [https://www.geeksforgeeks.org/machine-learning/cross-validation-machine-learning/]
- 27. Cross-validation vs. Bootstrapping: Which to Use for ... [https://www.linkedin.com/posts/mehreen-soomro-5684a413a_cross-validation-vs-bootstrapping-which-activity-7371879234169905152-irF5]
- 28. Validation of prognostic models: challenges and opportunities [https://jeccm.amegroups.org/article/view/4742/5275]
- 29. Train Test Validation Split: Best Practices & Examples [https://www.lightly.ai/blog/train-test-validation-split]
- 30. Is there a rule-of-thumb for how to divide a dataset into ... [https://stackoverflow.com/questions/13610074/is-there-a-rule-of-thumb-for-how-to-divide-a-dataset-into-training-and-validatio]
- 31. Split-Sample Model Validation - Statistical Thinking [https://www.fharrell.com/post/split-val/]
- 32. Chapter 17: Internal validation - Clinical Prediction Models [https://www.clinicalpredictionmodels.org/extra-material/chapter-17]
- 33. On Splitting Training and Validation Set: A Comparative ... [https://link.springer.com/article/10.1007/s41664-018-0068-2]
- 34. On Splitting Training and Validation Set: A Comparative Study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6373628/]
- 35. Train Test Validation Split: How To & Best Practices [2024] [https://www.v7labs.com/blog/train-validation-test-set]
- 36. Geographic and temporal validity of prediction models [https://www.sciencedirect.com/science/article/abs/pii/S0895435616301408]
- 37. External Validation of a Predictive Model for Reintubation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10872431/]
- 38. Construction and validation of a risk prediction model for ... [https://www.nature.com/articles/s41598-025-24478-7]
- 39. 2025 Trends In Pharmaceutical Analytical Methods ... [https://agnopharma.com/blog/trends-in-pharmaceutical-analytical-methods-development-validation/]
- 40. Predictive Performance of Machine Learning for Suicide in ... [https://www.jmir.org/2025/1/e73052]
- 41. Prediction models for self-harm and suicide: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12513157/]
- 42. Efficient rare event estimation for multimodal and high ... [https://arxiv.org/html/2508.00210v1]
- 43. Efficient rare event sampling with unsupervised ... [https://www.nature.com/articles/s42256-024-00918-3]
- 44. Prospective evaluation of the adapted Ontario Protocol ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413211/]
- 45. SPIRIT 2025 statement: updated guideline for protocols of ... [https://www.nature.com/articles/s41591-025-03668-w]
- 46. AI in Drug Development: Clinical Validation and ... [https://globalforum.diaglobal.org/issue/june-2025/ai-in-drug-development-clinical-validation-and-regulatory-innovation-are-dual-imperatives/]
- 47. Artificial Intelligence in Software as a Medical Device [https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-software-medical-device]
- 48. Understanding FDA's 2025 Draft Guidance on AI-Enabled ... [https://www.orielstat.com/blog/fda-2025-guidance-ai-enabled-medical-devices/]
- 49. A Step-by-Step Guide to Effective AI Model Validation [https://galileo.ai/blog/ai-model-validation]
- 50. Systematic scoping review of external validation studies ... [https://www.nature.com/articles/s41698-025-00940-7]
- 51. Protocol for implementing the nested model for AI design and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12018536/]
- 52. Advancements in predicting and modeling rare event ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10585719/]
- 53. The Relationship Between High Dimensionality and ... [https://www.geeksforgeeks.org/machine-learning/the-relationship-between-high-dimensionality-and-overfitting/]
- 54. Optimizing high dimensional data classification with a ... [https://www.nature.com/articles/s41598-025-08699-4]
- 55. Handling Sparse and High-Dimensional Data in Machine ... [https://medium.com/@siddharthapramanik771/handling-sparse-and-high-dimensional-data-in-machine-learning-strategies-and-techniques-for-34516e88efff]
- 56. Development and Internal Validation of a Four-Predictor ... [https://pubmed.ncbi.nlm.nih.gov/41189297/]
- 57. Development and Internal Validation of Machine Learning ... [https://www.mdpi.com/2075-4426/15/10/476]
- 58. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 59. Testing AI Itself: How to Validate Machine Learning Models ... [https://medium.com/@james.genqe/testing-ai-itself-how-to-validate-machine-learning-models-in-2025-1a48c2a79c86]
- 60. Mastering Model Selection for AI/ML Models [https://eajournals.org/ejcsit/vol13-issue14-2025/mastering-model-selection-for-ai-ml-models/]
- 61. AI Model Optimization Techniques for Enhanced ... [https://www.netguru.com/blog/ai-model-optimization]
- 62. Advances in machine learning for optimizing ... [https://www.sciencedirect.com/science/article/pii/S1570164625000153]
- 63. Internal validation strategy for high dimensional prognosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12451366/]
- 64. The relevance of the real-world evidence in research, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11878099/]
- 65. External Validation of the NECPAL CCOMS-ICO ... [https://www.mdpi.com/2409-9279/8/3/45]
- 66. How to be prepared for Pharmaceutical Validation in 2025 [https://www.gillsprocess.com/blog-1/2024/12/11/how-to-be-prepared-for-pharmaceutical-validation-in-2025]
- 67. Development and external validation of a machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261740/]
- 68. Usability Challenges in Electronic Health Records: Impact on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12206486/]
- 69. Overcoming EHR Implementation Challenges: A 2025 ... [https://helpsquad.com/overcoming-ehr-implementation-challenges/]
- 70. 21 Elements of a Research Protocol with Example (WHO ... [https://www.enago.com/academy/research-protocol-elements-to-consider/]
- 71. Data Table Design UX Patterns & Best Practices [https://www.pencilandpaper.io/articles/ux-pattern-analysis-enterprise-data-tables]
- 72. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 73. Empirical evaluation of internal validation methods for prediction in... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-01844-5]
- 74. Impact of train/test sample regimen on performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8280147/]
- 75. Data imbalance in drug response prediction: multi-objective... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11966611/]
- 76. Re-evaluation of the comparative effectiveness of bootstrap ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-020-01201-w]
- 77. Cross-Validation vs. Bootstrapping [https://www.geeksforgeeks.org/machine-learning/cross-validation-vs-bootstrapping/]
- 78. Bootstrap Confidence Limits for Bootstrap Overfitting ... [https://www.fharrell.com/post/bootcal/]
- 79. Bootstrap vs Crossvalidation for assessing the predictive ... [https://stats.stackexchange.com/questions/656710/bootstrap-vs-crossvalidation-for-assessing-the-predictive-performance-of-a-machi]
- 80. Development and validation of a nomogram for in-stent ... [https://bmcsurg.biomedcentral.com/articles/10.1186/s12893-025-02955-0]
- 81. Development and validation of an online nomogram for ... [https://pubmed.ncbi.nlm.nih.gov/41287084/]
- 82. Development and validation of a nomogram for predicting ... [https://www.nature.com/articles/s41598-025-26223-6]
- 83. Use of transportability methods for real-world evidence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11542082/]
- 84. Transportability of patient outcomes from a US clinical trial ... [https://www.medrxiv.org/content/10.1101/2024.05.25.24307916v1.full]
- 85. Can Data Transportability Connect Patients to Therapies ... [https://www.costellomedical.com/what-we-do/evidence-development/real-world-evidence/data-transportability-in-real-world-evidence/]
- 86. Internal and External Validation of the Generalizability ... [https://www.sciencedirect.com/science/article/abs/pii/S0883540323000852]
- 87. a simulation study to compare cross-validation versus holdout ... [https://ejnmmires.springeropen.com/articles/10.1186/s13550-022-00931-w]
- 88. Model EvaI future in 2025 - UBIAI [https://ubiai.tools/the-future-of-model-eval-achieving-superior-testing-and-evaluation-standards-in-ai/]
- 89. A multidimensional analysis-based risk prediction model ... [https://pubmed.ncbi.nlm.nih.gov/41044596/]
- 90. Development and validation of a machine learning model ... [https://www.nature.com/articles/s41598-025-25423-4]
- 91. External validation and comparison of clinical prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482746/]
- 92. Development, validation, and clinical utility of a risk ... [https://www.sciencedirect.com/science/article/pii/S0167494325001116]
- 93. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 94. FDA Oversight: Understanding the Regulation of Health AI ... [https://bipartisanpolicy.org/issue-brief/fda-oversight-understanding-the-regulation-of-health-ai-tools/]
- 95. FDA Software Validation 2025: What Evidence to Show [https://www.complizen.ai/post/what-level-of-software-validation-evidence-is-fda-looking-for-in-2025]
- 96. Novel Drug Approvals for 2025 [https://www.fda.gov/drugs/novel-drug-approvals-fda/novel-drug-approvals-2025]
- 97. Implementing Alternative Methods [https://www.fda.gov/science-research/advancing-alternative-methods-fda/implementing-alternative-methods]
- 98. How will FDA changes reshape drug approval in 2025 and ... [https://cen.acs.org/pharmaceuticals/drug-development/FDA-changes-reshape-drug-approval/103/web/2025/05]