Statistical Validation Techniques for Predictive Models: A Comprehensive Guide for Biomedical Research
This article provides a comprehensive framework for the statistical validation of predictive models in biomedical and clinical research.
Statistical Validation Techniques for Predictive Models: A Comprehensive Guide for Biomedical Research
Abstract
This article provides a comprehensive framework for the statistical validation of predictive models in biomedical and clinical research. Tailored for researchers, scientists, and drug development professionals, it covers the foundational principles of model evaluation, key methodological approaches for assessing performance, advanced techniques for troubleshooting and optimization, and rigorous strategies for external validation and model comparison. By synthesizing current best practices and emerging methodologies, this guide aims to equip practitioners with the knowledge to build reliable, clinically applicable predictive models that can withstand the complexities of real-world data and support critical decision-making in healthcare.
Core Principles and the Critical Importance of Model Validation
In the field of predictive modeling, particularly within medical and pharmaceutical research, model validation is the critical process of evaluating a model's performance to ensure its predictions are accurate, reliable, and trustworthy for supporting clinical decisions [1] [2]. Validation provides essential safeguards against the risks of deploying models that may fail when applied to new patient populations or in different clinical settings. Without rigorous validation, prediction models may appear effective in the development data but prove misleading or harmful in real-world applications [3].
The core distinction in validation approaches lies between internal and external validation. Internal validation assesses model performance on data from the same source population as the development data, primarily addressing overfitting—where a model learns patterns specific to the development data that do not generalize. External validation evaluates performance on data collected from different populations, locations, or time periods, assessing the model's transportability and generalizability beyond its original development context [1]. Both forms of validation are essential components of a comprehensive validation strategy, with external validation being particularly crucial for verifying that a model can safely support decisions in diverse clinical environments [3] [1].
Internal Validation: Concepts and Methodologies
Core Principle and Purpose
Internal validation aims to estimate how well a predictive model would perform when applied to new samples from the same underlying population as the development data [2]. It focuses on quantifying and correcting for overfitting, which occurs when a model learns random noise or idiosyncratic patterns in the development dataset rather than true underlying relationships. This over-optimism, known as optimism bias, means the model's performance in the development data will be better than its performance in new data from the same population [3]. Internal validation techniques provide corrected estimates of model performance to address this bias.
Key Methodological Approaches
Table 1: Common Internal Validation Techniques
| Technique | Description | Key Advantages | Common Use Cases |
|---|---|---|---|
| Holdout Validation | Dataset randomly split into training and testing sets [4] [5] | Simple to implement; computationally efficient | Large datasets with ample samples |
| K-Fold Cross-Validation | Data divided into k subsets; each subset serves once as validation while others train [4] [5] | More robust performance estimate; uses data efficiently | Medium-sized datasets; model comparison |
| Bootstrap Validation | Multiple random samples with replacement from original data; model evaluated on unsampled cases [3] | Provides optimism-corrected estimates; does not require large holdout samples | Small to medium datasets; optimal for clinical models [3] |
| Leave-One-Out Cross-Validation | Special case of k-fold where k equals number of observations [5] | Minimizes bias; uses nearly all data for training | Small datasets where every observation counts |
Application in Medical Research
In clinical prediction model development, internal validation is considered a mandatory step. Research indicates that models developed from small datasets are particularly vulnerable to overfitting, making internal validation essential [3]. For example, in a study developing a nomogram to predict overall survival in cervical cancer patients, the researchers randomly split their 13,592 patient records from the SEER database into a training cohort (n=9,514) and an internal validation cohort (n=4,078) using a 70:30 ratio [6]. This internal validation approach allowed them to obtain optimism-corrected performance estimates, with the model achieving a concordance index (C-index) of 0.885 in the internal validation cohort, similar to the training performance [6].
External Validation: Concepts and Methodologies
Core Principle and Purpose
External validation tests whether a predictive model developed in one setting performs adequately in different populations, locations, or time periods [1]. Where internal validation addresses reproducibility, external validation focuses on transportability—the model's ability to maintain performance when applied to new environments with potentially different patient characteristics, measurement procedures, or clinical practices [1]. A model succeeding only in internal validation but failing in external validation may be clinically dangerous if implemented broadly.
Key Methodological Approaches
Table 2: Types of External Validation
| Validation Type | Description | Strengths | Limitations |
|---|---|---|---|
| Geographic Validation | Validation on data from different locations or centers [1] | Tests cross-center applicability; identifies geographic variations | May reflect different healthcare systems rather than model flaws |
| Temporal Validation | Validation on data from the same location but different time period [3] | Assesses temporal stability; detects model decay over time | Does not test spatial generalizability |
| Domain Validation | Validation on data with different inclusion criteria or patient populations [1] | Tests robustness to population shifts; broadest generalizability test | Most challenging to pass; may require model recalibration |
Critical Challenges in External Validation
Three fundamental reasons explain why models often perform worse during external validation [1]:
Patient populations vary: Differences in demographics, risk factors, disease severity, and healthcare systems between development and validation settings affect model performance. These variations can impact both discrimination (separation between risk groups) and calibration (accuracy of absolute risk estimates) [1].
Measurement procedures vary: Equipment from different manufacturers, subjective assessments, clinical practice patterns, and measurement timing can create heterogeneity that diminishes model performance [1].
Populations and measurements change over time: Natural temporal shifts in patient characteristics, disease management, and measurement technologies can degrade model performance, a phenomenon known as "model drift" [1].
Application in Medical Research
The cervical cancer prediction study exemplifies rigorous external validation, where researchers tested their nomogram on 318 patients from Yangming Hospital Affiliated to Ningbo University—a completely different institution from the SEER database used for development [6]. The model maintained strong performance with a C-index of 0.872, demonstrating successful geographic transportability [6]. Similarly, in HIV research, a study developing a random survival forest model to predict survival following antiretroviral therapy initiation conducted external validation using data from a different city [7]. While the model showed excellent internal performance (C-index: 0.896), external validation revealed a substantial decrease (C-index: 0.756), highlighting how model performance can vary across settings and the critical importance of external testing [7].
Comparative Analysis: Performance Across Validation Contexts
Quantitative Performance Comparisons
Table 3: Performance Comparison Across Validation Types in Medical Studies
| Study & Condition | Model Type | Internal Performance (C-index/AUC) | External Performance (C-index/AUC) | Performance Gap |
|---|---|---|---|---|
| Cervical Cancer Survival [6] | Cox Nomogram | C-index: 0.885 (95% CI: 0.873-0.897) | C-index: 0.872 (95% CI: 0.829-0.915) | -0.013 |
| HIV Survival Post-HAART [7] | Random Survival Forest | C-index: 0.896 (95% CI: 0.885-0.906) | C-index: 0.756 (95% CI: 0.730-0.782) | -0.140 |
| HIV Treatment Interruption Prediction [8] | Various ML Models | Mean AUC: 0.668 (SD=0.066) | Rarely performed [8] | Not assessed |
Interpretation of Performance Discrepancies
The performance differences between internal and external validation reveal important characteristics about model robustness and generalizability. The cervical cancer nomogram demonstrated remarkable consistency between internal and external validation, suggesting the identified prognostic factors (age, tumor grade, stage, size, lymph node metastasis, and lymph vascular space invasion) maintain consistent relationships across healthcare settings [6]. In contrast, the substantial performance drop in the HIV survival model during external validation indicates higher sensitivity to differences between development and validation settings, potentially due to variations in patient populations, measurement procedures, or clinical practices [7].
Systematic reviews highlight that performance degradation during external validation is common. One analysis of 104 cardiovascular prediction models found median C-statistics decreased from 0.76 in development data to 0.64 at external validation [1]. This underscores why external validation is indispensable for determining a model's true clinical utility.
Experimental Protocols for Comprehensive Validation
Recommended Validation Workflow
A comprehensive validation strategy should incorporate both internal and external validation components [3]:
Internal validation using bootstrapping: For the development dataset, use bootstrap resampling (with 1000 or more replicates) to obtain optimism-corrected performance estimates [3]. This approach is preferred over simple data splitting, particularly for small to medium-sized datasets, as it uses the full dataset for development while providing robust overfitting corrections.
Internal-external cross-validation: When multiple centers or studies are available, use a leave-one-center-out approach where the model is developed on all but one center and validated on the left-out center, repeating for all centers [3]. This provides preliminary evidence of transportability while using all available data.
External validation in fully independent data: Seek validation in completely independent datasets from different locations, preferably collected at different times and representing the intended use populations [1].
Critical Performance Metrics
Both internal and external validation should assess multiple performance dimensions:
- Discrimination: Ability to separate high-risk and low-risk patients, measured by C-index (survival models) or AUC (classification models) [6] [7]
- Calibration: Agreement between predicted and observed event rates, assessed via calibration plots or tests [6] [1]
- Clinical utility: Net benefit of using the model for clinical decisions, evaluated through decision curve analysis [6]
Essential Research Reagents and Tools
Table 4: Researcher's Toolkit for Predictive Model Validation
| Tool Category | Specific Solutions | Function in Validation | Examples from Literature |
|---|---|---|---|
| Statistical Software | R software with specific packages | Implementation of validation techniques and performance metrics | R version 4.3.2 used for cervical cancer nomogram development [6] |
| Validation Techniques | Bootstrap resampling, k-fold cross-validation | Internal validation and optimism correction | Bootstrapping with 1000 replicates recommended for internal validation [3] |
| Performance Metrics | C-index, AUC, calibration plots, Brier score | Quantifying discrimination, calibration, overall performance | C-index reported in cervical cancer (0.872-0.885) and HIV (0.756-0.896) studies [6] [7] |
| Data Splitting Methods | Random sampling, stratified sampling, temporal splitting | Creating training/validation splits | 70:30 random split used in cervical cancer study [6] |
| Reporting Guidelines | TRIPOD (Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis) | Ensuring comprehensive reporting of validation results | TRIPOD guidelines followed in HIV prediction study [7] |
Internal and external validation serve complementary but distinct roles in establishing the credibility of predictive models. Internal validation, through techniques such as bootstrapping and cross-validation, provides essential safeguards against overfitting and generates optimism-corrected performance estimates [3]. External validation, including geographic, temporal, and fully independent validation, tests the model's transportability to new settings and populations [1]. The empirical evidence consistently demonstrates that models frequently exhibit degraded performance during external validation, underscoring why both validation types are indispensable in the model development lifecycle [6] [7] [1].
For researchers and drug development professionals, a comprehensive validation strategy should progress from rigorous internal validation to multiple external validations across diverse settings. This systematic approach ensures that predictive models deployed in clinical practice are both statistically sound and clinically useful across the varied contexts in which they will be applied.
The statistical validation of predictive models is a cornerstone of reliable research, particularly in fields like drug development and healthcare, where model predictions can directly impact clinical decisions and patient outcomes. A model's utility is not determined solely by its algorithmic sophistication but by its rigorously demonstrated performance on new, unseen data. This evaluation process moves beyond simple metrics to provide a holistic view of how a model will behave in real-world settings.
The TRIPOD (Transparent Reporting of a multivariable prediction model for Individual Prognosis) checklist was developed to improve the reliability and value of clinical predictive model reporting, promoting transparency and methodological rigor [9]. Independent validation is crucial because a model's performance on its development data is often overly optimistic due to overfitting, where the model learns not only the underlying data patterns but also the noise specific to that sample [9] [10]. This guide objectively compares the three pillars of model assessment—Discrimination, Calibration, and Overall Accuracy—providing researchers with the experimental protocols and data needed for robust statistical validation.
Defining the Key Performance Aspects
Discrimination
- Definition: Discrimination is a model's ability to separate distinct outcome classes. For instance, it quantifies how well a model distinguishes between patients who will experience an event (e.g., disease progression) from those who will not [9].
- Core Concept: A model with high discrimination assigns a higher predicted risk or probability to subjects who have the event compared to those who do not.
Calibration
- Definition: Calibration reflects the agreement between predicted probabilities and the actual observed event rates. It assesses the reliability of a model's probability estimates [9] [11].
- Core Concept: A perfectly calibrated model would mean that among 100 patients each assigned a risk of 20%, the event would occur for exactly 20 of them. Poor calibration has been identified as the 'Achilles heel' of predictive models, as it directly reduces a model's clinical utility and net benefit [9].
- Definition: Overall Accuracy is a general measure of a model's correctness. For classification models, it is typically defined as the proportion of total correct predictions (both positive and negative) among all predictions made [12] [10].
- Core Concept: While intuitive, accuracy can be a misleading metric, especially for imbalanced datasets where one outcome class is much more frequent than the other.
Quantitative Comparison of Performance Metrics
The following tables summarize the key metrics, their interpretation, and comparative data for evaluating discrimination, calibration, and accuracy.
Table 1: Core Evaluation Metrics for Discrimination, Calibration, and Accuracy
| Performance Aspect | Key Metric(s) | Interpretation & Calculation | Ideal Value |
|---|---|---|---|
| Discrimination | Area Under the ROC Curve (AUC-ROC) [9] [12] | Proportion of randomly selected patient pairs (one with, one without the event) where the model assigns a higher risk to the patient with the event. Ranges from 0.5 (no discrimination) to 1.0 (perfect discrimination). | 0.8 - 0.9 (Excellent), >0.9 (Outstanding) |
| Kolmogorov-Smirnov (K-S) Statistic [12] | Measures the degree of separation between the positive and negative distributions. Higher values indicate better separation. | 0 (No separation) to 100 (Perfect separation) | |
| Calibration | Calibration Slope [9] [11] | Slope of the linear predictor in a validation model. A slope of 1 indicates perfect calibration, <1 suggests overfitting, and >1 suggests underfitting. | ~1.0 |
| Calibration-in-the-Large [9] | Compares the overall observed event rate to the average predicted risk. Assesses whether the model systematically over- or under-predicts. | ~0.0 | |
| Hosmer-Lemeshow Test [11] | A goodness-of-fit test comparing predicted and observed events across risk groups. A low chi-square statistic and p-value >0.05 suggest good calibration. | p > 0.05 | |
| Brier Score [9] | The mean squared difference between the predicted probabilities and the actual outcomes (0 or 1). A proper scoring rule that combines discrimination and calibration. | 0 (Perfect) to 0.25 (Worthless) | |
| Overall Accuracy | Accuracy [12] [10] | (True Positives + True Negatives) / Total Predictions. The overall proportion of correct predictions. | Higher is better, but context-dependent. |
| F1 Score [12] | Harmonic mean of Precision and Recall. Provides a single score that balances the two concerns. Useful for imbalanced datasets. | 0 to 1, higher is better. |
Table 2: Example Performance Comparison of Cardiovascular Risk Prediction Models
This table summarizes data from a systematic review comparing the performance of laboratory-based and non-laboratory-based models on external validation cohorts [11].
| Model Type | Median C-Statistic (IQR) | C-Statistic Difference (vs. Lab-based) | Calibration Performance |
|---|---|---|---|
| Laboratory-Based | 0.74 (0.72 - 0.77) | (Reference) | Similar to non-lab models, but non-calibrated equations often overestimated risk. |
| Non-Laboratory-Based | 0.74 (0.70 - 0.76) | Median Absolute Difference: 0.01 (Very Small) | Similar to lab models, but non-calibrated equations often overestimated risk. |
Table 3: The Researcher's Toolkit for Model Validation
| Tool / Reagent | Function in Validation |
|---|---|
| Statistical Software (R, Python) | Provides libraries (e.g., scikit-learn, rms, pROC) for calculating all key metrics and performing resampling. |
| Resampling Methods (Bootstrap, Cross-Validation) | Core techniques for internal validation to estimate model optimism and correct for overfitting [9]. |
| Validation Dataset | An independent, unseen dataset held out from the model development process, essential for external validation [9]. |
| Fairness Metrics (e.g., Equalized Odds, Demographic Parity) | Tools to evaluate potential disparities in model performance across sensitive subgroups like sex, race, or ethnicity [13]. |
Experimental Protocols for Performance Assessment
Protocol for Internal Validation using Resampling
Aim: To estimate the optimism in model performance metrics due to overfitting using only the development dataset [9].
- Bootstrap Resampling: Repeatedly draw many samples (e.g., 1000) with replacement from the original development dataset. Each sample should be the same size as the original dataset.
- Model Development & Testing: For each bootstrap sample:
- Develop the model using the same entire procedure (variable selection, parameter tuning) on the bootstrap sample.
- Calculate the apparent performance (e.g., AUC, Brier score) of this model on the same bootstrap sample.
- Calculate the test performance of this model on the original dataset (or the data points not in the bootstrap sample, known as the out-of-bag sample).
- Optimism Calculation: For each bootstrap iteration, compute the optimism as the difference between the apparent performance and the test performance.
- Performance Correction: Calculate the average optimism across all iterations. Subtract this average optimism from the apparent performance of the model developed on the original full dataset to obtain an optimism-corrected performance estimate.
Protocol for External Validation
Aim: To quantify the model's performance and generalizability in a fully independent participant sample from a different location or time period [9] [11].
- Dataset Acquisition: Obtain a dataset that was not used in any part of the model development process. The population can be from a different clinical site, geographic region, or time period.
- Apply Model: Apply the exact, finalized model (including the same coefficients and intercept) to the new data to generate predictions for each individual.
- Measure Performance: Calculate all relevant performance metrics—including discrimination (AUC), calibration (calibration slope, intercept, and plot), and overall accuracy—directly on this new dataset.
- Analyze Calibration: Create a calibration plot:
- Stratify the validation cohort into groups (e.g., deciles) based on their predicted risk.
- For each group, plot the mean predicted risk against the observed event rate (with confidence intervals).
- Fit a logistic regression of the observed outcome on the log-odds of the predicted probability to estimate the calibration intercept and slope.
Relationships and Workflows in Model Validation
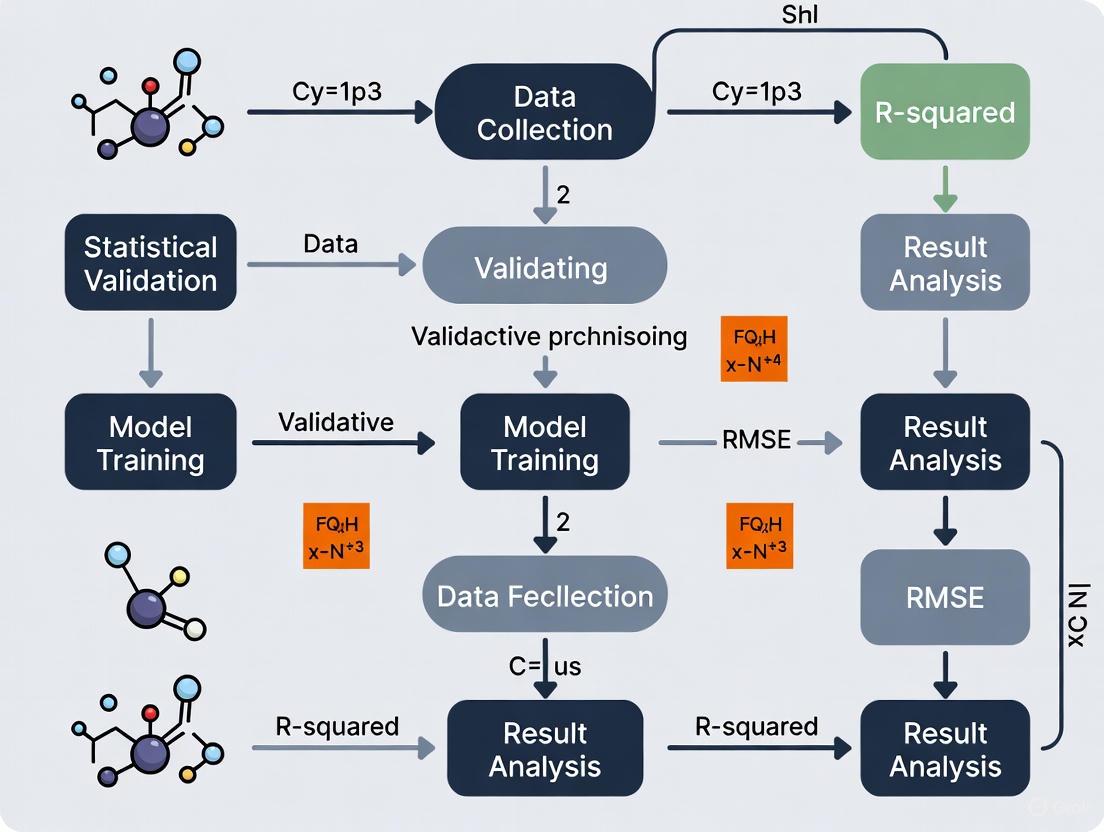
The following diagram illustrates the logical sequence and key decision points in the model validation process, highlighting the roles of discrimination, calibration, and accuracy.
Model Validation Workflow
Critical Considerations for Researchers
The Interplay of Metrics and Potential Pitfalls
- The Limitation of Discrimination: A model can have high discrimination (AUC) but poor calibration, leading to systematically biased risk estimates that are clinically harmful [9]. Furthermore, recent research highlights that a model can retain high discrimination after implementation and still harm patients if it creates "harmful self-fulfilling prophecies"—where the model's predictions directly influence decisions that make the prediction come true, without improving outcomes [14].
- The Insensitivity of C-Statistics: When comparing models, a difference in the c-statistic (AUC) of less than 0.025 is generally considered "very small" [11]. As shown in Table 2, laboratory and non-laboratory-based models can show nearly identical discrimination, demonstrating that this metric is insensitive to the inclusion of additional predictors. The clinical value of new predictors may be better assessed by their hazard ratios and impact on reclassification metrics [11].
- The Bias-Variance Trade-off: Both overfitting and underfitting are critical pitfalls. Overfitting occurs when a model is too complex and learns noise from the training data, leading to poor performance on new data. Underfitting occurs when a model is too simple to capture the underlying trends in the data [10]. Techniques like cross-validation and regularization are essential to find the right balance.
The Critical Role of Fairness and Reporting
- Algorithmic Fairness: As predictive models are integrated into clinical care, it is vital to evaluate their performance across sensitive demographic subgroups (e.g., sex, race, ethnicity). Fairness metrics, such as Equalized Odds and Demographic Parity, are tools to detect disparities [13]. However, a 2025 review found that the use of these metrics in clinical risk prediction literature remains rare, and training data are often racially and ethnically homogeneous, risking the perpetuation of health inequities [13].
- Robust External Validation: The common practice of using a simple train-test split for validation can fail for spatial or temporal data because it violates the assumption that data points are independent and identically distributed [15]. For such data, validation techniques that account for geographic or temporal correlation are necessary for reliable performance estimates [15].
In predictive model research, particularly for binary outcomes in fields like clinical development and epidemiology, statistical validation is paramount for assessing model reliability and accuracy. Three core metrics form the foundation for evaluating probabilistic prediction models: the Brier Score, the C-statistic, and various calibration measures. The Brier Score provides an overall measure of prediction accuracy, the C-statistic (or concordance index) evaluates the model's ranking ability, and calibration measures assess the agreement between predicted probabilities and observed outcomes. Together, these metrics offer complementary insights into model performance, with the Brier Score uniquely incorporating aspects of both discrimination and calibration [16]. Understanding their distinct properties, interpretations, and interrelationships enables researchers to perform comprehensive model validation and select the most appropriate models for specific applications, ultimately supporting robust decision-making in drug development and clinical research.
Metric Definitions and Core Concepts
Brier Score
The Brier Score (BS) is a strictly proper scoring rule that measures the accuracy of probabilistic predictions for binary or categorical outcomes. It represents the mean squared difference between the predicted probabilities and the actual outcomes, serving as an overall measure of prediction error [17] [18] [19].
Formula: For a set of N predictions, the Brier Score is calculated as:
( BS = \frac{1}{N} \sum{t=1}^{N} (ft - o_t)^2 )
where ( ft ) is the forecast probability (between 0 and 1) and ( ot ) is the actual outcome (0 or 1) [17] [18].
Interpretation: The score ranges from 0 to 1, where 0 represents perfect accuracy and 1 indicates perfect inaccuracy [17] [19].
Extension: For multi-category outcomes with R classes, the Brier Score extends to:
( BS = \frac{1}{N} \sum{t=1}^{N} \sum{i=1}^{R} (f{ti} - o{ti})^2 )
where the probabilities across all classes for each event must sum to 1 [18] [19].
C-Statistic (Concordance Statistic)
The C-statistic (C), also known as the concordance index or C-index, measures the discriminative ability of a model—its capacity to separate those who experience an event from those who do not [20] [21] [22].
Definition: The C-statistic represents the probability that a randomly selected subject who experienced the event has a higher predicted risk than a randomly selected subject who did not experience the event [20] [22]. It is equivalent to the area under the Receiver Operating Characteristic (ROC) curve (AUC) [20] [22].
Interpretation: Values range from 0 to 1, where:
- 0.5 indicates no discrimination better than chance
- 0.7-0.8 suggests acceptable discrimination
- 0.8-0.9 indicates excellent discrimination
- 1.0 represents perfect discrimination [22]
Limitation: The C-statistic is often conservative and can be insensitive to meaningful improvements in model performance, particularly when new biomarkers are added to already robust models [21].
Calibration Measures
Calibration refers to the agreement between predicted probabilities and observed event rates. A well-calibrated model that predicts a 70% chance of an event should see that event occur approximately 70% of the time across many such predictions [23] [24].
Confidence Calibration: A model is considered confidence-calibrated if for all confidence levels c, the model is correct c proportion of the time:
( \mathbb{P}(Y = \text{arg max}(\hat{p}(X)) | \text{max}(\hat{p}(X)) = c) = c \ \forall c \in [0, 1] ) [23]
Expected Calibration Error (ECE): A widely used measure that bins predictions and calculates the weighted average of the difference between accuracy and confidence across bins:
( ECE = \sum{m=1}^{M} \frac{|Bm|}{n} |\text{acc}(Bm) - \text{conf}(Bm)| )
where ( B_m ) is the m-th bin, acc is the average accuracy, and conf is the average confidence in that bin [23].
Multi-class and Class-wise Calibration: Extends the concept beyond binary outcomes to multiple classes, requiring alignment between predicted probability vectors and actual class distributions [23].
Comparative Analysis of Metrics
Table 1: Core Characteristics of Validation Metrics
| Metric | Primary Function | Measurement Range | Optimal Value | Key Strengths |
|---|---|---|---|---|
| Brier Score | Overall prediction accuracy | 0 to 1 | 0 | Strictly proper scoring rule; incorporates both discrimination and calibration |
| C-statistic | Discrimination ability | 0 to 1 | 1 | Intuitive interpretation; equivalent to AUC; widely understood |
| Calibration Measures | Agreement between predicted and observed probabilities | Varies by measure | 0 (for ECE) | Direct assessment of probability reliability; crucial for clinical decision-making |
Table 2: Metric Limitations and Complementary Uses
| Metric | Key Limitations | Best Paired With | Clinical Utility |
|---|---|---|---|
| Brier Score | Does not directly incorporate clinical costs; insufficient for clinical utility alone [16] | Calibration measures | Provides overall accuracy assessment but lacks cost-sensitive evaluation |
| C-statistic | Conservative; insensitive to model improvements; ignores calibration [21] | Brier Score, calibration plots | Assesses ranking ability but not magnitude of risk differences |
| Calibration Measures | ECE sensitive to binning strategy; does not measure discrimination [23] | Brier Score, C-statistic | Critical for probability interpretation in treatment decisions |
Methodologies for Metric Calculation
Brier Score Calculation Protocol
The Brier Score can be decomposed into three additive components, providing deeper insight into the sources of prediction error [18]:
Experimental Protocol:
- Data Preparation: Collect N prediction-outcome pairs (f, o) where f is the predicted probability (0-1) and o is the actual outcome (0 or 1)
- Direct Calculation: Compute ( BS = \frac{1}{N} \sum{t=1}^{N} (ft - o_t)^2 )
- Reference Calculation: For comparison, compute the reference Brier Score using climatology: ( BS{ref} = \frac{1}{N} \sum{t=1}^{N} (\bar{o} - o_t)^2 ) where ( \bar{o} ) is the overall event rate
- Brier Skill Score Calculation: Determine relative improvement: ( BSS = 1 - \frac{BS}{BS_{ref}} ) [18] [19]
Interpretation: The Brier Skill Score ranges from -∞ to 1, where positive values indicate improvement over the reference forecast, 0 indicates no improvement, and negative values indicate worse performance [17] [19].
C-Statistic Derivation Methodology
Analytical Derivation under Binormality [20]:
- Assumption: Continuous explanatory variable follows normal distribution in both affected (Y=1) and unaffected (Y=0) populations
- Calculation: With means μA and μU and variances σA² and σU² in affected and unaffected groups:
- General case: ( C = \Phi(\frac{\muA - \muU}{\sqrt{\sigmaA^2 + \sigmaU^2}}) = \Phi(\frac{d}{\sqrt{2}}) ) where d is Cohen's effect size
- Equal variances: ( C = \Phi(\frac{\sigma\beta}{\sqrt{2}}) ) where β is the log-odds ratio
- Empirical Estimation: Using all possible pairs of subjects where one experienced the event and one did not, calculate the proportion where the subject with the event had higher predicted risk [20]
Calibration Assessment Protocol
Expected Calibration Error (ECE) Calculation [23]:
- Binning: Partition predictions into M bins (typically 10) of equal interval (0-0.1, 0.1-0.2, ..., 0.9-1.0)
- Bin Statistics: For each bin Bm, calculate:
- Accuracy: ( acc(Bm) = \frac{1}{|Bm|} \sum{i \in Bm} \mathbb{1}(\hat{y}i = yi) )
- Confidence: ( conf(Bm) = \frac{1}{|Bm|} \sum{i \in Bm} \hat{p}(x_i) )
- ECE Computation: ( ECE = \sum{m=1}^{M} \frac{|Bm|}{n} |acc(Bm) - conf(Bm)| )
Reliability Diagrams: Visual representation of calibration by plotting expected accuracy (confidence) against observed accuracy (true frequency) for each bin [24].
Advanced Concepts and Recent Developments
Brier Score Decomposition
The Brier Score can be decomposed to provide deeper insights into model performance [18]:
Three-component decomposition: ( BS = REL - RES + UNC ) where REL is reliability (calibration), RES is resolution, and UNC is uncertainty
Two-component decomposition: ( BS = CAL + REF ) where CAL is calibration and REF is refinement
The uncertainty component measures inherent outcome variability, resolution measures how much forecasts differ from the average outcome, and reliability measures how close forecasts are to the actual probabilities [18].
Weighted Brier Score for Clinical Utility
Traditional Brier Score is limited in assessing clinical utility as it weights all prediction errors equally regardless of clinical consequences [16]. The weighted Brier score incorporates clinical utility by aligning with decision-theoretic frameworks:
- Framework: Considers different costs for false positives and false negatives in clinical decisions
- Implementation: Uses cost-weighted misclassification loss functions that balance trade-offs between false positives and false negatives
- Advantage: Provides a single measure incorporating calibration, discrimination, and clinical utility [16]
Relationship Between Metrics
The C-statistic primarily measures discrimination, calibration measures assess probability agreement, while the Brier Score incorporates both aspects. Under the assumption of binormality (explanatory variable normally distributed in both outcome groups), the C-statistic follows a standard normal cumulative distribution with dependence on the product of the standard deviation and the log-odds ratio [20]. This relationship highlights that discriminative ability depends on both the effect size and population heterogeneity.
Visual Guide to Metric Relationships
Figure 1: Relationship between predictive model validation metrics and their composite contributions to clinical utility assessment
Figure 2: Brier Score calculation workflow and decomposition process
Research Reagent Solutions
Table 3: Essential Tools for Predictive Model Validation
| Tool Category | Specific Solutions | Research Application | Implementation Example |
|---|---|---|---|
| Statistical Software | R, Python with scikit-learn | Metric calculation and model validation | sklearn.metrics.brier_score_loss, roc_auc_score |
| Calibration Visualization | Reliability diagrams, Calibration curves | Visual assessment of probability calibration | Plotting expected vs. observed probabilities by bin |
| Model Validation Frameworks | ROC analysis, Decision curve analysis | Comprehensive model performance assessment | Calculating net benefit across probability thresholds |
| Clinical Utility Assessment | Weighted Brier score, Net benefit functions | Incorporating clinical consequences into evaluation | Applying cost-weighted loss functions for clinical decisions |
The Brier Score, C-statistic, and calibration measures provide distinct but complementary insights into predictive model performance. The Brier Score offers an overall measure of prediction accuracy that incorporates both discrimination and calibration, the C-statistic specifically evaluates ranking ability, and calibration measures assess the reliability of probability estimates. For comprehensive model validation, researchers should consider all three metrics rather than relying on a single measure. Recent developments, such as weighted Brier scores that incorporate clinical utility, represent promising advances for aligning statistical evaluation with clinical decision-making. By understanding the strengths, limitations, and appropriate application contexts for each metric, researchers in drug development and clinical research can make more informed decisions about model selection and implementation.
The Role of Validation in Clinical Decision-Making and Regulatory Science
Validation serves as the foundational bridge between innovative predictive models and their reliable application in clinical and regulatory settings. In both clinical decision-making and regulatory science, validation transforms theoretical algorithms into trusted tools for patient care and drug development. As defined by regulatory bodies, validation provides "objective evidence that a process consistently produces a result meeting predetermined specifications," ensuring that predictive models perform as intended in real-world scenarios [25]. The European Medicines Agency (EMA) emphasizes that active innovation in regulatory science is required to keep pace with accelerating technological advances, underscoring validation's role in protecting human and animal health [26].
The year 2025 represents a pivotal moment for validation practices, with nearly 60% of U.S. hospitals projected to adopt AI-assisted predictive tools in routine clinical care, a significant increase from approximately 35% in 2022 [27]. This rapid adoption necessitates robust validation frameworks to ensure these technologies deliver accurate, reliable, and equitable healthcare outcomes. Validation provides the critical evidence base that allows healthcare professionals, patients, and regulatory authorities to trust predictive models guiding medical decisions [28] [29].
Core Principles of Predictive Model Validation
The Validation Lifecycle
The validation of clinical prediction models follows a structured pathway from development through implementation. This lifecycle approach ensures models remain accurate and relevant throughout their operational use. According to foundational texts in clinical prediction models, a "practical checklist" guides development of valid prediction models, encompassing preliminary considerations, handling missing values, predictor coding, selection of main effects and interactions, and model parameter estimation with shrinkage methods [29].
The core principles of clinical prediction model validation include both internal and external validation techniques. Internal validation assesses model performance using the original development dataset, typically through methods like bootstrapping or cross-validation, which provide optimism-adjusted performance measures. External validation evaluates whether a model developed in one setting performs adequately in different populations or healthcare settings, testing its transportability and generalizability [28]. This distinction is crucial for determining whether a model requires updating or complete recalibration when deployed in new environments.
Performance Metrics and Evaluation
Comprehensive model evaluation extends beyond simple discrimination metrics to include calibration and clinical utility. Standard validation metrics include:
- Discrimination: The model's ability to distinguish between different outcome classes, typically measured by the Area Under the Receiver Operating Characteristic curve (AUC-ROC) or C-statistic [30].
- Calibration: The agreement between predicted probabilities and observed outcomes, often visualized using calibration plots [28] [29].
- Clinical Utility: The net benefit of using a model for clinical decision-making across various probability thresholds, evaluated through decision curve analysis [29].
Table 1: Key Performance Metrics for Predictive Model Validation
| Metric Category | Specific Measures | Interpretation | Optimal Values |
|---|---|---|---|
| Discrimination | AUC-ROC, C-statistic | Ability to distinguish between outcome classes | >0.7 (acceptable), >0.8 (good), >0.9 (excellent) |
| Calibration | Calibration slope, intercept | Agreement between predictions and observed outcomes | Slope close to 1, intercept close to 0 |
| Overall Performance | Brier score, R² | Accuracy of probabilistic predictions | Lower Brier score indicates better accuracy |
| Clinical Utility | Decision Curve Analysis | Net benefit across decision thresholds | Positive net benefit versus default strategies |
Regulatory Validation Frameworks to 2025
Evolving Regulatory Expectations
Regulatory science is undergoing significant transformation to address emerging challenges in medicine development and evaluation. The EMA's Regulatory Science to 2025 strategy reflects stakeholder priorities for enhancing evidence generation throughout a medicine's lifecycle [26]. This strategy acknowledges that regulators must innovate both science and processes themselves rather than maintaining "business as usual" approaches [26].
Key regulatory trends impacting validation include increased emphasis on computer system validation (CSV), process validation aligned with lifecycle management, and data integrity in validation processes [25]. The integration of real-world evidence and digital health technologies into regulatory decision-making requires novel validation approaches that maintain scientific rigor while accommodating new data types. Regulatory agencies are particularly focused on risk-based validation approaches that prioritize resources based on the potential impact on product quality and patient safety [25].
Validation in Pharmaceutical Contexts
Pharmaceutical validation extends beyond predictive models to encompass manufacturing processes, analytical methods, and cleaning procedures. Preparation for pharmaceutical validation in 2025 involves anticipating regulatory trends and adopting advanced technologies while enhancing traditional validation practices [25]. The transition from traditional validation methods to continuous process validation (CPV) represents a significant shift, using real-time data to monitor and validate manufacturing processes throughout their lifecycle [25].
Table 2: Pharmaceutical Validation Framework Components for 2025
| Validation Domain | Key Requirements | Emerging Technologies | Regulatory Standards |
|---|---|---|---|
| Computer System Validation | Data integrity, security, electronic records | Blockchain for traceability, paperless validation systems | 21 CFR Part 11, ALCOA+ principles |
| Process Validation | Lifecycle approach, real-time monitoring | Process Analytical Technology, IoT sensors | FDA Process Validation Guidance (2011) |
| Cleaning Validation | Scientifically justified limits, contamination control | Modern analytical methods, automation | EMA Guidelines on setting health-based exposure limits |
| Analytical Method Validation | Accuracy, precision, specificity | Advanced spectroscopy, chromatography | ICH Q2(R2) Guideline |
Experimental Protocols for Model Validation
Future-Guided Learning for Time-Series Forecasting
Recent advances in validation methodologies include sophisticated approaches like Future-Guided Learning for enhancing time-series forecasting. This protocol employs a dynamic feedback mechanism inspired by predictive coding theory, using two models: a detection model that analyzes future data to identify critical events, and a forecasting model that predicts these events based on current data [30].
Experimental Protocol:
- Model Architecture: Implement two separate models - a "teacher" detection model with access to short-term future data and a "student" forecasting model using only current and historical data.
- Training Procedure: When discrepancies occur between forecasting and detection models, apply significant parameter updates to the forecasting model to minimize prediction surprise.
- Evaluation Metrics: Quantify performance using AUC-ROC for event prediction tasks and Mean Squared Error for regression forecasting.
- Validation: Apply rigorous internal validation through cross-validation and external validation on completely separate datasets [30].
This approach demonstrated a 44.8% increase in AUC-ROC for seizure prediction using EEG data and a 23.4% reduction in MSE for forecasting in nonlinear dynamical systems [30]. The method showcases how innovative validation frameworks can substantially enhance model performance while maintaining methodological rigor.
Machine Learning Classifier Validation
A comprehensive study on machine learning classifiers for construction quality and schedule prediction provides a transferable protocol for clinical and regulatory applications. The research utilized nine ML classifiers including MLP, SVM, KNN, LDA, LR, DT, RF, AdaBoost, and Gradient Boosting, systematically comparing their performance on standardized inspection data [31].
Experimental Workflow:
- Data Preprocessing: Address missing values, normalize features, and handle class imbalance through appropriate sampling techniques.
- Hyperparameter Optimization: Systematically tune model parameters using grid search or Bayesian optimization with cross-validation.
- Model Training: Implement appropriate regularization techniques to prevent overfitting and ensure generalizability.
- Performance Evaluation: Assess models using multiple metrics including accuracy, precision, recall, F1-score, and AUC-ROC.
- Feature Importance Analysis: Identify which input features most significantly impact model predictions to enhance interpretability [31].
This structured validation protocol highlights the importance of comparing multiple algorithms rather than relying on a single modeling approach, particularly for high-stakes applications in regulatory science and clinical decision-making.
Comparative Performance of Validation Techniques
Quantitative Validation Metrics
Different validation approaches yield substantially different performance outcomes, as demonstrated by comparative studies across domains. In clinical settings, biomarker-based predictive models have shown significant improvements in early disease identification, with some applications achieving up to 48% improvement in early detection rates [27]. The integration of multi-omics data with advanced analytical methods has improved early Alzheimer's disease diagnosis specificity by 32%, providing a crucial intervention window [32].
Table 3: Comparative Performance of Predictive Modeling Techniques
| Model Category | Best Application Context | Performance Strengths | Validation Considerations |
|---|---|---|---|
| Traditional Statistical Models | Small datasets, strong prior knowledge | High interpretability, clinical acceptance | Prone to bias with correlated predictors |
| Machine Learning Classifiers | High-dimensional data, complex interactions | Handles non-linear relationships, robust to multicollinearity | Requires large samples, hyperparameter tuning critical |
| Deep Learning Models | Image, temporal, and multimodal data | Superior accuracy for complex patterns | "Black box" limitations, extensive computational needs |
| Time-Series Forecasting | Longitudinal data, dynamic systems | Captures temporal dependencies, trend analysis | Sensitive to non-stationary data, requires specialized validation |
Addressing Validation Challenges
Even with robust protocols, significant challenges persist in predictive model validation. Biomarker-based models face particular hurdles including data heterogeneity, inconsistent standardization protocols, limited generalizability across populations, high implementation costs, and substantial barriers in clinical translation [32]. These challenges necessitate integrated frameworks prioritizing multi-modal data fusion, standardized governance protocols, and interpretability enhancement [32].
In regulatory contexts, validation must also address ethical considerations such as algorithmic bias mitigation. If historical data reflects societal biases or inequalities, predictive analytics could perpetuate these issues in decision-making processes [27]. Organizations must prioritize fairness in their algorithms by implementing measures to identify and mitigate bias during model development and validation [27].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing robust validation frameworks requires specific methodological tools and approaches. The following table details key "research reagent solutions" essential for predictive model validation in clinical and regulatory contexts.
Table 4: Essential Research Reagent Solutions for Predictive Model Validation
| Tool Category | Specific Solutions | Function in Validation | Application Context |
|---|---|---|---|
| Statistical Software | R, Python, SAS, IBM SPSS Modeler | Model development, performance metrics, visualization | General predictive modeling, comprehensive analysis |
| Time-Series Analysis | Prophet, ARIMA models | Specialized forecasting, seasonality handling | Longitudinal data, dynamic system prediction |
| Machine Learning Platforms | Scikit-learn, TensorFlow, PyTorch | Algorithm implementation, hyperparameter tuning | High-dimensional data, complex pattern recognition |
| Data Standards | CDISC, OMOP Common Data Model | Data harmonization, interoperability | Multi-site studies, regulatory submissions |
| Validation Frameworks | CARP, TRIPOD, PROBAST | Methodological guidance, reporting standards | Study design, protocol development, manuscript preparation |
| Visualization Tools | Tableau, ggplot2, matplotlib | Performance communication, exploratory analysis | Result interpretation, stakeholder engagement |
Visualization of Validation Workflows
Clinical Prediction Model Development Pathway
Regulatory Validation Decision Framework
Validation represents both a scientific discipline and a strategic imperative in clinical decision-making and regulatory science. As predictive technologies continue to evolve, validation frameworks must similarly advance to ensure these tools deliver safe, effective, and equitable outcomes. The EMA's Regulatory Science to 2025 initiative highlights the critical importance of stakeholder engagement and collaborative approaches to validation in an era of rapid innovation [26].
Future directions in validation science include expanded application to rare diseases, incorporation of dynamic health indicators, strengthened integrative multi-omics approaches, conduct of longitudinal cohort studies, and leveraging edge computing solutions for low-resource settings [32]. Additionally, the growing emphasis on real-world evidence and continuous monitoring of deployed models will require more adaptive validation frameworks that can accommodate iterative learning systems while maintaining rigorous oversight.
For researchers, scientists, and drug development professionals, mastering validation principles and practices is no longer optional but essential for translating predictive models into clinically useful tools and regulatory-approved solutions. By adhering to robust validation standards while innovating new approaches, the scientific community can harness the full potential of predictive technologies to advance patient care and public health.
Key Validation Metrics and Performance Assessment Techniques
The performance of prediction models is critically assessed using a variety of methods and metrics to ensure their reliability and appropriateness for real-world applications [33]. In evidence-based medicine, well-validated risk scoring systems play an indispensable role in selecting prevention and treatment strategies by predicting the occurrence of clinical events [34]. Traditional measures for evaluating models with binary and survival outcomes include the Brier score for overall model performance, the concordance statistic (C-statistic) for discriminative ability, and goodness-of-fit statistics for calibration [33]. These metrics provide complementary insights into different aspects of model performance, with discrimination measuring how well models separate those with and without outcomes, and calibration assessing the accuracy of the absolute risk estimates [35].
Despite the emergence of newer measures, reporting discrimination and calibration remains fundamental for any prediction model [33]. This guide provides a comprehensive comparison of these three traditional performance measures, offering researchers, scientists, and drug development professionals with the foundational knowledge needed for robust statistical validation of predictive models in medical research.
The table below summarizes the key characteristics, interpretations, and optimal values for the Brier score, C-statistic, and calibration slope.
Table 1: Comparison of Traditional Performance Measures for Predictive Models
| Metric | Primary Function | Interpretation | Optimal Value | Strengths | Limitations |
|---|---|---|---|---|---|
| Brier Score | Overall performance measurement [33] | Mean squared difference between predicted probabilities and actual outcomes [36] | 0 (perfect) [36] | Strictly proper scoring rule; evaluates both discrimination and calibration [37] | Difficult to interpret without context; value range depends on incidence [37] |
| C-statistic (AUC) | Discrimination assessment [33] | Probability that a random patient with event has higher risk score than one without event [34] | 1 (perfect discrimination) | Intuitive interpretation; handles censored data [38] [34] | Does not measure prediction accuracy [38]; insensitive to calibration [35] |
| Calibration Slope | Calibration evaluation [35] | Spread of estimated risks; slope of linear predictor [33] | 1 (perfect calibration) | Identifies overfitting (slope <1) or underfitting (slope >1) [35] | Does not fully capture calibration; requires sufficient sample size [35] |
Detailed Methodologies and Protocols
Brier Score: Protocol for Implementation and Interpretation
Calculation Methodology
The Brier score represents a quadratic scoring rule calculated as the mean squared difference between predicted probabilities and actual outcomes [33]. For binary outcomes, the mathematical formulation is:
BS(p,y) = 1/n × Σ(pi - yi)² [37]
where:
- n = total number of predictions
- pi = predicted probability of event for case i
- yi = actual outcome (1 if event occurred, 0 otherwise) [37]
The Brier score ranges from 0 to 1, where 0 represents perfect accuracy and 1 indicates the worst possible performance [36]. However, the maximum value for a non-informative model depends on the outcome incidence; for a 50% incidence, the maximum is 0.25, while for a 10% incidence, it is approximately 0.09 [33].
Interpretation Guidelines
When interpreting Brier scores, researchers should avoid common misconceptions. A Brier score of 0 is theoretically perfect but practically improbable, as it requires extreme predictions (0% or 100%) that exactly match outcomes [37]. Lower Brier scores generally indicate better performance, but comparisons should only be made within the same population and context, as the score depends on the underlying outcome distribution [37]. Importantly, a low Brier score does not necessarily indicate good calibration, as these measure different aspects of model performance [37].
C-statistic: Protocol for Implementation and Interpretation
Calculation Methodology
The C-statistic measures discrimination—the ability to distinguish between patients who experience an event earlier versus those who experience it later or not at all [38]. For survival outcomes, the calculation involves comparing pairs of patients:
C = Pr(g(Z₁) > g(Z₂) ∣ T₂ > T₁) [34]
where:
- g(Z) = risk score derived from the model
- T = event time
- The subscript indicates two independent patients [34]
In practice, the C-statistic is computed as the proportion of concordant pairs among all usable pairs [38] [34]. A pair is concordant if the patient with the shorter observed event time has a higher risk score. Modifications exist to handle censored observations, such as Harrell's C-statistic and Uno's C-statistic, with the latter being less dependent on the study-specific censoring distribution [38] [34].
Interpretation Guidelines
The C-statistic ranges from 0.5 (no discriminative ability) to 1.0 (perfect discrimination) [34]. However, it's crucial to recognize that the C-statistic quantifies only the model's ability to rank patients according to risk, not the accuracy of the predicted risk values themselves [38]. Two models with identical C-statistics can have substantially different prediction accuracy, particularly if one uses transformed predictors [38].
Calibration Slope: Protocol for Implementation and Interpretation
Calculation Methodology
The calibration slope evaluates the spread of estimated risks and is an essential aspect of both internal and external validation [33]. It is obtained by fitting a logistic regression model to the outcome using the linear predictor of the original model as the only covariate:
logit(pᵢ) = α + β × LPᵢ
where:
- pᵢ = predicted probability for patient i
- LPᵢ = linear predictor from the original model
- β = calibration slope [35]
The linear predictor LPᵢ is typically the sum of the product of regression coefficients and predictor values from the original model.
Interpretation Guidelines
The target value for the calibration slope is 1 [35]. A slope less than 1 indicates that predictions are too extreme (overfitting), meaning high risks are overestimated and low risks are underestimated [35]. Conversely, a slope greater than 1 suggests that risk estimates are too moderate (underfitting) [35]. It's important to note that the calibration slope alone does not fully capture model calibration, as it primarily measures the spread of risk estimates rather than their absolute accuracy [39].
Relationships Between Performance Measures
The diagram below illustrates the conceptual relationships between the three performance measures and what they assess in a predictive model.
Figure 1: Interrelationships between traditional performance measures in predictive model validation
Experimental Applications and Case Studies
Cardiovascular Risk Prediction Study
In a recent study predicting cardiovascular composite outcomes in high-risk patients with type 2 diabetes, three Cox models were evaluated using traditional performance measures [38]. The model with 21 variables demonstrated a C-statistic of 0.76, while a simplified model containing only log NT-proBNP achieved a C-statistic of 0.72 [38]. This minimal difference in discrimination, despite dramatic differences in model complexity, highlights how the C-statistic alone may not fully capture clinical utility.
Esophageal Cancer Risk Model Comparison
A comparison of standard and penalized logistic regression models for predicting pathologic nodal disease in esophageal cancer patients revealed remarkably consistent performance across measures [40]. The standard regression and four penalized regression models had nearly identical Brier scores (0.138-0.141), C-statistics (0.775-0.788), and calibration slopes (0.965-1.05) [40]. This case demonstrates that when datasets are large and outcomes relatively frequent, different modeling approaches may yield similar predictive performance as measured by traditional metrics.
Cardiovascular Model Calibration Comparison
An external validation study of QRISK2-2011 and NICE Framingham models in 2 million UK patients demonstrated the critical importance of calibration [35]. Although both models had similar C-statistics (0.771 vs. 0.776), the Framingham model significantly overestimated risk [35]. At the 20% risk threshold for intervention, QRISK2-2011 identified 110 per 1000 men as high-risk, while Framingham identified nearly twice as many (206 per 1000) due to miscalibration [35]. This case illustrates how poor calibration can lead to substantial overtreatment even when discrimination appears adequate.
Research Reagent Solutions
Table 2: Essential Analytical Tools for Predictive Model Validation
| Tool | Function | Implementation Examples |
|---|---|---|
| Statistical Software | Calculation of performance metrics | R: rms, survival packages; Python: scikit-learn |
| Calibration Curves | Visual assessment of risk accuracy | Plotting observed vs. predicted probabilities by risk decile [35] |
| Kaplan-Meier Estimator | Handling censored data in C-statistic | Nonparametric survival curve estimation for risk stratification [34] |
| Penalized Regression | Preventing overfitting | Ridge, Lasso, Elastic Net for improved calibration [40] |
| Validation Cohorts | External performance assessment | Split-sample, bootstrap, or external dataset validation [33] |
The Brier score, C-statistic, and calibration slope provide complementary insights into different aspects of predictive model performance. The Brier score offers an overall measure of prediction accuracy, the C-statistic quantifies the model's ability to discriminate between outcomes, and the calibration slope assesses the appropriateness of the absolute risk estimates. Researchers should report all three measures to provide a comprehensive assessment of model performance, with particular attention to calibration when models inform clinical decisions [33] [35]. No single metric captures all aspects of model performance, and the choice of emphasis should align with the intended application of the predictive model.
In the field of predictive model research, traditional performance metrics such as sensitivity, specificity, and the Area Under the Receiver Operating Characteristic Curve (AUC) offer limited insight because they measure diagnostic accuracy without accounting for clinical consequences or patient preferences [41] [42]. Decision Curve Analysis (DCA) has emerged as a decision-analytic method that evaluates the clinical utility of prediction models and diagnostic tests by quantifying the net benefit across a range of clinically reasonable threshold probabilities [43] [44]. First introduced by Vickers and Elkin in 2006, DCA addresses a critical gap in model evaluation by integrating the relative value that patients and clinicians place on different outcomes (e.g., true positives vs. false positives) into the assessment framework [42] [45]. This approach allows researchers and drug development professionals to determine whether a model, despite having good statistical accuracy, is truly useful for guiding clinical decisions and improving patient outcomes.
The core principle of DCA is to compare the net benefit of using a prediction model against two default strategies: intervening on all patients or intervening on no patients [42] [43]. "Intervention" is defined broadly and can include administering a drug, performing a surgery, conducting a diagnostic workup, or providing lifestyle advice [42]. By using net benefit as a standardized measure that combines model performance with clinical consequences, DCA provides a more pragmatic and patient-centered framework for model validation than traditional statistical metrics alone.
Core Principles and Quantification of Net Benefit
The Concept of Threshold Probability
A foundational element of DCA is the threshold probability, denoted as ( p_t ) [41]. This represents the minimum probability of a disease or event at which a patient or clinician would decide to intervene. This threshold inherently reflects a personal valuation of the relative harms of unnecessary intervention (a false positive) versus missing a disease (a false negative) [42].
For example, in a prostate cancer biopsy scenario, a patient who is highly cancer-averse (perhaps due to family history) might opt for a biopsy even at a low predicted risk (e.g., 5%). This patient has a low threshold probability. Conversely, a patient who is more averse to the potential side effects of a biopsy might only proceed if the predicted risk is high (e.g., 30%), indicating a high threshold probability [42]. The DCA framework acknowledges that no single threshold fits all patients, and therefore evaluates model performance across a range of reasonable threshold probabilities [41].
Calculating Net Benefit
The net benefit is the key quantitative output of a DCA, providing a single metric that balances the benefits of true positives against the harms of false positives, weighted by the threshold probability [41]. The standard formula for net benefit for the treated is:
[ \text{net benefit}{\text{treated}} = \frac{\text{TP}}{n} - \frac{\text{FP}}{n} \times \left(\frac{pt}{1 - p_t}\right) ]
Where:
- TP = Number of True Positives
- FP = Number of False Positives
- n = Total number of subjects
- ( p_t ) = Threshold probability [41]
This calculation can be adapted to focus on untreated patients or an overall net benefit, but the ranking of models typically remains consistent across these variations [41]. The net benefit is calculated for each strategy (the model, "treat all," and "treat none") across the entire range of threshold probabilities. A model is considered clinically useful at a specific threshold if its net benefit surpasses that of the "treat all" and "treat none" strategies for that value of ( p_t ) [41] [43].
DCA Versus Traditional Performance Metrics
The following table summarizes the critical distinctions between DCA and traditional metrics for evaluating predictive models.
Table 1: Comparison of DCA with Traditional Model Evaluation Metrics
| Feature | Decision Curve Analysis (DCA) | Traditional Metrics (AUC, Sensitivity/Specificity) |
|---|---|---|
| Primary Focus | Clinical utility and decision-making consequences [41] [43] | Diagnostic accuracy and statistical discrimination [41] |
| Incorporation of Preferences | Explicitly integrates patient/clinician preferences via threshold probability (( p_t )) [41] [42] | Does not incorporate preferences or clinical consequences of decisions [42] |
| Result Interpretation | Identifies if and for whom (i.e., at what preferences) a model is useful [42] [43] | Indicates how well a model separates classes, but not if it improves decisions [41] |
| Reference Strategies | Directly compares against "treat all" and "treat none" default strategies [43] [44] | No comparison to simple default clinical strategies |
| Handling of Probability Thresholds | Evaluates all possible thresholds simultaneously [41] | A single, often arbitrary, threshold must be chosen for sensitivity/specificity [42] |
A key advantage of DCA is its ability to reveal that a model with a high AUC may not always offer superior clinical utility. A study comparing the Pediatric Appendicitis Score (PAS), leukocyte count, and serum sodium for suspected appendicitis found that while both PAS and leukocyte count had acceptable AUCs, their decision curves showed substantially different net benefit profiles [46]. This demonstrates that higher discrimination does not automatically translate to superior clinical value, a critical insight that traditional metrics fail to provide.
Experimental Protocols for Implementing DCA
Data Requirements and Model Preparation
To perform a DCA, you need a dataset with observed binary outcomes (e.g., disease present/absent) and the predicted probabilities from the model(s) you wish to evaluate [43]. These probabilities can come from a model developed on the same dataset (requiring internal validation to correct for overfitting) or from an externally published model applied to your validation cohort [41] [43].
Key Consideration: A common pitfall is evaluating a model on the same data used to build it without correcting for overfitting. This can lead to overly optimistic net benefit estimates. Bootstrap validation or cross-validation should be used to correct for this optimism [41].
Step-by-Step DCA Protocol
- Define the Clinical Decision: Clearly state the intervention (e.g., "biopsy," "prescribe drug") and the target outcome (e.g., "high-grade cancer," "disease recurrence") [42].
- Calculate Predicted Probabilities: For each patient in the validation dataset, obtain the predicted probability of the outcome from the model(s) under evaluation [43].
- Specify the Threshold Probability Range: Define a sequence of threshold probabilities (( p_t )) from just above 0% to just below 100%. The range can be restricted to clinically plausible values (e.g., 5% to 35%) for a clearer visualization [43].
- Compute Net Benefit for Each Strategy:
- For the Prediction Model: At each ( pt ), classify patients as "test positive" if their predicted probability ≥ ( pt ). Calculate net benefit using the formula in Section 2.2 [41].
- For "Treat All": This strategy has a net benefit of ( \pi - (1 - \pi)\frac{pt}{1 - pt} ), where ( \pi ) is the outcome prevalence [41].
- For "Treat None": This strategy always has a net benefit of 0 [41].
- Visualize the Results: Plot net benefit (y-axis) against threshold probability (x-axis) for all strategies [41] [43].
- Statistical Comparison (Optional): For a formal comparison between two models, use bootstrap methods to calculate confidence intervals and p-values for the difference in net benefit across the range of ( p_t ) [41].
The Scientist's Toolkit for DCA
Table 2: Essential "Research Reagents" for Implementing Decision Curve Analysis
| Tool / Resource | Function / Purpose | Example Platforms / Packages |
|---|---|---|
| Statistical Software | Provides the computational environment to perform data management, model fitting, and DCA calculations. | R, Stata, SAS, Python [44] |
| DCA Software Package | Dedicated functions that automate the calculation of net benefit and plotting of decision curves. | R: dcurves [43], rmda; Stata: dca [44] |
| Validation Dataset | A dataset with observed outcomes and model-predicted probabilities, used to evaluate the model's clinical utility. | Internally validated cohort or external validation dataset [43] |
| Bootstrap Routine | A resampling method used to correct for model overfitting and to calculate confidence intervals for net benefit. | Available in standard statistical software (e.g., R's boot package) [41] |
| Plotting System | A graphics library used to create the decision curve plot, ideally with smooth curves and confidence intervals. | R's ggplot2 system [41] |
Interpretation of Decision Curves and Case Study
How to Read a Decision Curve
Interpreting a decision curve involves a few simple steps [42]:
- Identify the Highest Line: At any given threshold probability on the x-axis, the strategy with the highest net benefit (the top line on the y-axis) is the preferred clinical strategy.
- Determine the Useful Range: A prediction model is clinically useful across the range of ( p_t ) where its net benefit is higher than both the "treat all" and "treat none" lines.
- Understand the Extremes: The "treat all" strategy typically has a high net benefit at very low thresholds (where missing a disease is considered far worse than an unnecessary intervention). The "treat none" strategy is only preferred at very high thresholds.
Case Study: Prostate Cancer Biopsy
A pivotal application of DCA is in evaluating models for predicting high-grade prostate cancer to guide biopsy decisions. In a study comparing two models—the Prostate Cancer Prevention Trial (PCPT) risk calculator and a new model incorporating free PSA—traditional analysis showed both had reasonable AUCs (0.735 and 0.774, respectively). However, the PCPT model was miscalibrated [45].
The decision curve analysis revealed critical insights:
- The free PSA model (green line) demonstrated superior net benefit across a wide range of threshold probabilities compared to the default strategies [45].
- The PCPT model (orange line), despite its acceptable AUC, had lower net benefit than the "biopsy all" strategy for much of the range, indicating that using this model would lead to worse clinical outcomes than the current practice of biopsying everyone [45].
Table 3: Net Benefit Comparison in Prostate Cancer Biopsy Case Study (Selected Thresholds)
| Threshold Probability | Free PSA Model | PCPT Model | Biopsy All | Biopsy None |
|---|---|---|---|---|
| 5% | 0.110 | 0.085 | 0.092 | 0.000 |
| 10% | 0.075 | 0.050 | 0.042 | 0.000 |
| 15% | 0.055 | 0.030 | 0.018 | 0.000 |
| 20% | 0.040 | 0.018 | 0.005 | 0.000 |
Note: Net benefit values are illustrative approximations based on the case study description [45].
This case demonstrates DCA's power to identify a model that is not just statistically significant but clinically harmful, a conclusion that would be missed by relying on AUC alone.
Decision Curve Analysis represents a paradigm shift in the statistical validation of predictive models. By moving beyond pure accuracy metrics to a framework that incorporates clinical consequences and patient preferences, DCA provides a pragmatic and powerful tool for researchers and drug development professionals. It directly answers the critical question: "Will using this model improve patient decisions and outcomes?"
The experimental protocols and case studies outlined in this guide provide a foundation for implementing DCA in practice. As the demand for clinically actionable predictive models grows, DCA is poised to play an increasingly vital role in translating statistical predictions into tangible clinical benefits.
In predictive modeling research, particularly within medical and drug development contexts, the statistical validation of survival models is paramount. Survival analysis, or time-to-event analysis, deals with predicting the time until a critical event occurs, such as patient death, disease relapse, or recovery. A fundamental challenge in this domain is the presence of censored data, where the event of interest has not been observed for some subjects during the study period, meaning we only know that their true survival time exceeds their last observed time [47]. This characteristic necessitates specialized performance metrics that can handle such incomplete information. The research community has historically relied heavily on the Concordance Index (C-index) for evaluating survival models. However, a narrow focus on this single metric is increasingly recognized as insufficient, as it measures only a model's discriminative ability—how well it ranks patients by risk—and ignores other critical aspects like the accuracy of predicted probabilities and survival times [47]. A comprehensive evaluation strategy should integrate multiple metrics, primarily the C-index and the Integrated Brier Score (IBS), to provide a holistic view of model performance, assessing not just discrimination but also calibration and overall prediction error [33].
Core Metrics: Theoretical Foundations
The Concordance Index (C-index)
The Concordance Index, also known as the C-statistic, is a rank-based measure that evaluates a survival model's ability to correctly order patients by their relative risk. Intuitively, it calculates the proportion of all comparable pairs of patients in which the model's predictions and the observed outcomes agree. Formally, two patients are comparable if the one with the shorter observed time experienced the event (i.e., was not censored at that time). A comparable pair is concordant if the patient who died first had a higher predicted risk score; otherwise, it is discordant [48] [49].
The C-index is estimated using the following equation, where ( N ) is the number of comparable pairs: [ \text{C-index} = \frac{\text{Number of Concordant Pairs}}{N} ]
A C-index of 1.0 represents perfect discrimination, 0.5 indicates a model no better than random chance, and values below 0.5 suggest worse-than-random performance. While Harrell's C-index is widely used, it can be overly optimistic with high levels of censoring. Alternative estimators, such as the Inverse Probability of Censoring Weighting (IPCW) C-index, have been developed to provide a less biased estimate in such scenarios [48].
The Integrated Brier Score (IBS)
The Brier Score (BS) is a strict proper scoring rule that measures the accuracy of probabilistic predictions. For survival models, which predict a probability of survival over time, the BS is calculated at a specific time point ( t ) as the mean squared difference between the observed survival status (1 if alive, 0 if dead) and the predicted survival probability at ( t ) [18]. For a model that predicts a survival probability ( S(t | xi) ) for patient ( i ), the Brier Score at time ( t ) is: [ BS(t) = \frac{1}{N} \sum{i=1}^N \left( I(ti > t) - S(t | xi) \right)^2 ] where ( I(ti > t) ) is the indicator function that is 1 if the patient's observed time ( ti ) exceeds ( t ), and 0 otherwise.
The BS can be decomposed into three components: uncertainty (the inherent noise in the data), resolution (the model's ability to provide distinct predictions for different outcomes), and reliability (the calibration, or how closely the predicted probabilities match the actual outcomes) [18]. The Integrated Brier Score (IBS) provides a single summary measure of model performance over a defined time range of interest ( [0, t{max}] ) by integrating the BS over that period [48]: [ IBS = \frac{1}{t{max}} \int0^{t{max}} BS(t) \, dt ]
The IBS ranges from 0 to 1, with lower values indicating better overall performance. An IBS of 0 represents a perfect model, while a value of 0.25 or higher might indicate a non-informative model for a scenario with a 50% event rate [18] [33].
Comparative Performance of Survival Models
Quantitative Comparison Across Studies
Different survival models exhibit varying strengths and weaknesses, which are captured by the C-index and IBS. The following table synthesizes performance data from recent studies on cancer survival prediction, allowing for a direct, objective comparison of popular modeling approaches.
Table 1: Comparative Performance of Survival Models Across Various Studies
| Study & Disease Context | Model | C-index | Integrated Brier Score (IBS) | Key Predictors Identified |
|---|---|---|---|---|
| HR-positive/HER2-negative Breast Cancer [50] | DeepSurv | 0.70 (DFS), 0.68 (OS) | 0.22 (DFS), 0.17 (OS) | Nodal status, ER/PR expression, tumor size, Ki-67, pCR |
| Best ML Model (e.g., RSF) | 0.64 (DFS), 0.68 (OS) | Not Reported | ||
| Esophageal Cancer [51] | NMTLR | >0.81 (AUC for 1/3/5-year OS) | <0.175 | M stage, N stage, age, grade, bone/liver/lung metastases, radiotherapy |
| Random Survival Forest (RSF) | Similar high AUC | <0.175 | ||
| Invasive Lobular Carcinoma (Breast) [52] | Random Survival Forest | 0.72 | 0.08 | Age, tumor grade, AJCC stage, marital status, radiation therapy |
| Cox Proportional Hazards | ~0.814 | 0.08 | ||
| Deep Learning (RBM) | Accuracy: 0.97 | Not Reported |
Interpretation of Comparative Data
The data in Table 1 reveals several key insights for researchers. First, no single model dominates across all contexts. In the breast cancer study [50], the deep learning model DeepSurv marginally outperformed traditional machine learning (ML) models in discrimination for disease-free survival (DFS), but this came at the cost of lower interpretability and higher computational demands. This highlights a common trade-off: deep learning may offer slight performance gains, but simpler models can perform equally well, especially in smaller datasets [50].
Second, models like Random Survival Forest (RSF) and Neural Multi-Task Logistic Regression (NMTLR) consistently demonstrate strong performance, achieving high C-indices and low IBS values [51] [52]. The RSF's performance is particularly notable as it achieves a balance between model fit and complexity, as indicated by its low Akaike and Bayesian Information Criterion values [52]. Finally, the identified key predictors across studies—such as cancer stage, nodal involvement, age, and specific metastases—align with clinical knowledge, providing a sanity check on the models' logic and supporting their potential validity for clinical application [50] [51].
Experimental Protocols for Metric Evaluation
General Workflow for Survival Model Validation
The following diagram outlines a standardized workflow for training and evaluating a survival model, which serves as the foundation for obtaining the C-index and IBS values discussed in this guide.
Diagram 1: Survival Model Validation Workflow
Protocol for Calculating the Concordance Index
The C-index is typically calculated on a held-out test or validation set to ensure an unbiased estimate of model performance.
- Model Output: For each subject ( i ) in the test set, obtain a risk score ( r_i ) from the model. This can be a linear predictor from a Cox model, the negative of the predicted mean/median survival time, or another model-specific risk score.
- Identify Comparable Pairs: Form all possible pairs of subjects ( (i, j) ) in the test set. A pair is comparable if the observed time of the shorter-term subject is an event (not censored), i.e., ( tj > ti ) and ( \delta_i = 1 ).
- Assess Concordance: For each comparable pair, check if the subject with the higher risk score had the shorter event time. The pair is concordant if ( ri > rj ) and ( ti < tj ).
- Calculate the Statistic: The C-index is the fraction of concordant pairs among all comparable pairs.
- Implementation: Most statistical software packages (e.g., the
scikit-survivallibrary in Python) provide efficient functions for this calculation, such asconcordance_index_censoredfor Harrell's estimator andconcordance_index_ipcwfor the IPCW-adjusted estimator, which is recommended with high censoring [48].
Protocol for Calculating the Integrated Brier Score
The IBS evaluates the accuracy of a model's predicted survival probabilities over time.
- Model Output: The model must provide an Individual Survival Distribution (ISD), i.e., a predicted survival function ( S_i(t) ) for each subject ( i ) in the test set, which gives the probability that the subject survives beyond time ( t ) [47].
- Calculate Brier Score at Time Points: Select a sequence of time points ( t1, t2, ..., tk ) within the interval ( [0, t{max}] ), where ( t_{max} ) is the maximum time of interest. For each time point ( t ):
- The Brier Score ( BS(t) ) is computed as: [ BS(t) = \frac{1}{n} \sum{i=1}^n wi(t) \cdot (I(ti > t) - Si(t))^2 ]
- Here, ( I(ti > t) ) is the true status at time ( t ) (1 if alive, 0 if dead), and ( wi(t) ) is a weight that accounts for censoring, typically based on inverse probability of censoring weights (IPCW). This ensures that censored subjects are appropriately handled in the calculation [48].
- Integrate Over Time: The IBS is computed by integrating (averaging) the Brier scores across all time points: [ IBS = \frac{1}{t{max}} \int0^{t{max}} BS(t) \, dt ] In practice, this is often approximated numerically (e.g., using the trapezoidal rule) from the calculated values at ( t1, t2, ..., tk ).
- Implementation: The
integrated_brier_scorefunction inscikit-survivalautomates this process, requiring the true survival data, the predicted survival functions, and the time points for evaluation [48].
A Framework for Comprehensive Model Evaluation
Relying solely on the C-index provides an incomplete picture of a model's utility. A robust evaluation should be multi-faceted, as illustrated in the following framework.
Diagram 2: Framework for Comprehensive Model Evaluation
- Discrimination: This aspect, measured by the C-index and time-dependent Area Under the ROC Curve (AUC), assesses how well a model separates patients who experience the event early from those who experience it later or not at all. It is a measure of ranking [48] [33].
- Calibration: This evaluates the agreement between predicted probabilities and observed outcomes. For example, among 100 patients given a 1-year survival probability of 70%, 70 should indeed be alive at one year. Calibration can be visualized with a calibration plot and tested with goodness-of-fit statistics [33] [36]. The Brier score is also influenced by calibration.
- Overall Accuracy: The Integrated Brier Score is a key metric here, as it summarizes the model's error across all prediction times, incorporating both discrimination and calibration [48] [33].
- Clinical Usefulness: This moves beyond pure statistics to evaluate whether using the model for clinical decision-making would improve patient outcomes more than alternative strategies. Decision Curve Analysis is a prominent method for this, calculating the "net benefit" of model-based decisions across a range of risk thresholds [33].
The Scientist's Toolkit: Essential Research Reagents
To implement the experimental protocols and metrics described in this guide, researchers require both software tools and a principled methodological approach. The following table details these essential "research reagents."
Table 2: Essential Reagents for Survival Model Evaluation
| Tool / Concept | Type | Primary Function | Key Considerations |
|---|---|---|---|
scikit-survival (sksurv) |
Software Library | Provides a comprehensive suite for survival analysis in Python, including model implementations and key metrics like C-index and IBS. | The de facto standard in Python; includes concordance_index_ipcw and integrated_brier_score [48]. |
randomForestSRC |
Software Library | Implements Random Survival Forests in R. | A powerful and well-established package for ensemble survival modeling [51]. |
| Inverse Probability of Censoring Weighting (IPCW) | Statistical Method | A technique to correct for bias introduced by censored data by weighting observations. | Used in more robust versions of the C-index and Brier score, especially under high censoring [48]. |
| Individual Survival Distribution (ISD) | Model Output | A model that outputs a full probability distribution over survival time for each patient. | Required for calculating time-dependent metrics like the Brier score and predicting median survival time [47]. |
| Censoring Assumption | Methodological Principle | The assumed mechanism behind the censoring of data (e.g., random, informative). | The validity of most evaluation metrics, including C-index and IBS, often relies on the assumption of non-informative (random) censoring [47]. |
The rigorous validation of survival models is a cornerstone of reliable predictive research in healthcare and drug development. As this guide demonstrates, an over-reliance on the Concordance Index alone is a critical limitation in current practice. The C-index, while useful for assessing a model's ranking ability, reveals nothing about the accuracy of its predicted probabilities or survival times. A robust evaluation must be multi-dimensional, integrating the C-index with the Integrated Brier Score and other metrics like calibration plots. The IBS is particularly valuable as it provides a holistic measure of model performance that synthesizes both discrimination and calibration into a single, interpretable value. By adopting this comprehensive framework and the detailed experimental protocols provided, researchers and clinicians can better discern the true clinical utility of a survival model, ensuring that predictive tools are not only statistically sound but also fit for purpose in guiding critical decision-making.
Conceptual Foundation and Calculation
Net Reclassification Improvement (NRI) and Integrated Discrimination Improvement (IDI) are statistical metrics developed to quantify the improvement in predictive performance when new predictors are added to an existing risk prediction model. They address a key limitation of the traditional Area Under the ROC Curve (AUC), which often shows only small changes even when new markers provide clinically meaningful information [53] [54].
The NRI specifically measures how well a new model reclassifies subjects appropriately compared to an old model, with a focus on movement across clinically relevant risk categories [53]. It separates this reclassification for events (cases) and non-events (controls), then combines them into a single metric.
- Calculation of Categorical NRI: NRI = [P(up|case) - P(down|case)] + [P(down|control) - P(up|control)] Where "up" indicates movement to a higher risk category and "down" to a lower risk category with the new model [54].
The IDI provides a related but distinct measure that captures the average improvement in predicted probabilities without requiring predefined risk categories.
- Calculation of IDI: IDI = (p̄new,events - p̄old,events) - (p̄new,non-events - p̄old,non-events) Where p̄new,events and p̄old,events are the average predicted probabilities for events with the new and old models, respectively [55].
Table 1: Conceptual Comparison Between NRI and IDI
| Aspect | Net Reclassification Improvement (NRI) | Integrated Discrimination Improvement (IDI) |
|---|---|---|
| Primary Focus | Movement across risk categories | Average change in predicted probabilities |
| Requires Risk Categories | Yes (for categorical version) | No |
| Core Components | Reclassification of events and non-events | Difference in average sensitivity and (1-specificity) |
| Interpretation | Proportion of improved reclassification | Integrated difference in discrimination slopes |
Statistical Properties and Methodological Considerations
Key Statistical Formulations
The continuous NRI, which doesn't require predefined risk categories, is defined in population terms as:
ρ(θ₀; θ₀; π₀) = 2{Pr(β₀ᵀX + γ₀ᵀZ ≥ β₀ᵀX | Y=1) - Pr(β₀ᵀX + γ₀ᵀZ ≥ β₀ᵀX | Y=0)} [56]
The estimator for this population NRI is:
Rₙ(θ̂; θ̂₀; π̂) = [nȳ(1-ȳ)]⁻¹ Σᵢ[(yᵢ - ȳ) × I(β̂ᵀxᵢ + γ̂ᵀzᵢ - β̂₀ᵀxᵢ > 0) - ½] [56]
For the IDI, the standard estimator is:
IDÎ = (p̂̄new,₁ - p̂̄old,₁) - (p̂̄new,₀ - p̂̄old,₀) [55]
Where p̂̄new,₁ and p̂̄old,₁ are the average predicted probabilities for events with the new and old models, and p̂̄new,₀ and p̂̄old,₀ are the corresponding averages for non-events [55].
Critical Methodological Concerns
Several significant statistical concerns have been identified regarding NRI and IDI:
High False Positive Rates for NRI: Simulation studies demonstrate that the NRI statistic calculated on a large test dataset using risk models derived from a training set is likely to be positive even when the new marker has no predictive information [57]. One study found that with an AUC of 0.7 for the baseline model, the NRI was positive in 29.4% of simulations when the new marker was uninformative [57].
Invalid Inference for IDI: The standard z-test proposed for IDI is not valid because the null distribution of the test statistic is not standard normal, even in large samples [58]. Published methods of estimating the standard error of an IDI estimate tend to underestimate the error [58].
Susceptibility to Simpson's Paradox for IDI: The IDI can be affected by Simpson's Paradox, where the overall metric contradicts the conclusions when stratified by a key covariate [55]. This occurs because the IDI averages risks across events and non-events, which can mask stratum-specific effects.
Table 2: Statistical Concerns and Evidence
| Concern | Evidence | Implications for Research |
|---|---|---|
| NRI false positive rate | Positive NRI observed in 29.4-69.0% of simulations with uninformative markers [57] | NRI significance tests may be misleading |
| IDI inference problems | Standard error estimates tend to be too small [58] | z-test for IDI should not be relied upon |
| Lack of propriety | NRI is not a proper scoring function [56] | May reward incorrect model specification |
| Calibration dependence | Both metrics depend on calibration [55] | Poor calibration can lead to misleading values |
Experimental Applications and Protocols
Typical Experimental Workflow
The application of NRI and IDI in predictive model research typically follows a structured workflow that integrates these metrics within a comprehensive validation framework.
Case Study: Pulmonary Hypertension Risk Assessment
A study developing prediction models for pulmonary hypertension in high-altitude populations demonstrates the practical application of NRI and IDI [59]. Researchers developed two nomograms based on clinical and electrocardiographic factors:
- NomogramI: Included gender, Tibetan ethnicity, age, incomplete right bundle branch block (IRBBB), atrial fibrillation (AF), sinus tachycardia (ST), and T wave changes (TC)
- NomogramII: Included Tibetan ethnicity, age, right axis deviation (RAD), high voltage in the right ventricle (HVRV), IRBBB, AF, pulmonary P waves, ST, and TC
The study utilized a dataset of 6,603 subjects, randomly divided into derivation (70%) and validation (30%) sets. After model development using LASSO regression and multivariate logistic regression, the researchers compared the models using both NRI and IDI [59].
Table 3: Performance Comparison in Pulmonary Hypertension Study
| Model | AUC (Derivation) | AUC (Validation) | IDI | NRI |
|---|---|---|---|---|
| NomogramI | 0.716 | 0.718 | Reference | Reference |
| NomogramII | 0.844 | 0.801 | Significant improvement | Significant improvement |
The IDI and NRI indices confirmed that NomogramII outperformed NomogramI, leading the researchers to select NomogramII as their final model [59].
Case Study: Biomarker Evaluation
In toxicological sciences, the Predictive Safety Testing Consortium (PSTC) has used NRI and IDI to evaluate novel biomarkers for drug-induced injuries [60]. One study assessed four blood biomarkers of drug-induced skeletal muscle injury:
- Skeletal troponin I (sTnI)
- Myosin light chain 3 (Myl3)
- Creatine kinase M Isoform (Ckm)
- Fatty acid binding protein 3 (Fabp3)
The experimental protocol involved:
- Developing logistic regression models with standard biomarkers alone
- Expanding models by adding novel biomarkers
- Calculating NRI components (fraction improved positive findings and fraction improved negative findings)
- Computing IDI values
- Comparing these to likelihood-based tests [60]
The results showed consistent improvement with all novel biomarkers, though the PSTC now recommends likelihood-based methods for significance testing due to concerns about NRI/IDI false positive rates [60].
Recommended Research Practices
Statistical Testing Recommendations
Based on identified methodological concerns, researchers should adopt modified practices when using NRI and IDI:
Use Likelihood-Based Tests for Significance: When parametric models are employed, likelihood-based methods such as the likelihood ratio test should be used for significance testing rather than tests based on NRI or IDI [60]. The likelihood ratio test provides a valid test procedure while NRI and IDI tests may have inflated false positive rates [60].
Report Multiple Performance Measures: NRI and IDI should be reported alongside traditional measures such as AUC, Brier score, and calibration metrics to provide a comprehensive assessment of model performance [57].
Interpret Magnitude Alongside Statistical Significance: The interpretation of NRI and IDI should consider both statistical significance and magnitude of effect, as these measures can be statistically significant even with minimal clinical importance [61].
Researchers have several computational resources available for implementing NRI and IDI analyses:
R Packages for NRI/IDI Calculation:
Modified NRI Statistics: Recent methodological work has proposed a modified NRI (mNRI) to address the lack of propriety and high false positive rates of the standard NRI [56]. The mNRI replaces the constant model score residual with the base model score residual, creating a proper change score that satisfies the adaptation of proper scoring principle to change measures [56].
Reporting Guidelines
When reporting NRI and IDI results, researchers should include:
- Clear specification of whether categorical or continuous versions are used
- For categorical NRI, justification of the chosen risk categories
- Both components of NRI (event and non-event reclassification) separately
- Comparison with traditional performance measures
- Results of likelihood-based tests in addition to NRI/IDI values
- Discussion of clinical relevance in addition to statistical significance
Table 4: Essential Resources for Reclassification Analysis
| Resource | Type | Function | Implementation |
|---|---|---|---|
| R Statistical Software | Software platform | Primary environment for statistical analysis | Comprehensive R Archive Network (CRAN) |
| PredictABEL Package | R package | Assessment of risk prediction models | Available through CRAN |
| survIDINRI Package | R package | IDI and NRI for censored survival data | Available through CRAN |
| nricens Package | R package | NRI calculation for time-to-event and binary data | Available through CRAN |
| Likelihood Ratio Test | Statistical method | Valid significance testing for nested models | Standard in statistical packages |
| Simulation Studies | Methodological approach | Evaluating statistical properties of metrics | Custom programming required |
Residual Analysis and Influence Diagnostics for Model Refinement
Statistical validation forms the cornerstone of reliable predictive modeling in scientific research and drug development. Without rigorous diagnostic procedures, even sophisticated models can produce misleading results, potentially compromising research integrity and decision-making. Residual analysis and influence diagnostics serve as critical model refinement techniques, allowing researchers to quantify the agreement between models and data while identifying observations that disproportionately impact results. These methodologies are particularly vital in high-stakes fields like clinical pharmacology and healthcare research, where model predictions inform diagnostic and treatment decisions. This guide provides a comprehensive comparison of diagnostic tools, complete with experimental protocols and data presentation frameworks essential for robust model validation.
Core Concepts and Definitions
Residuals in Statistical Modeling
Residuals represent the discrepancies between observed values and model predictions, serving as the foundation for diagnostic procedures. For a continuous dependent variable Y, the residual ri for the i-th observation is calculated as ri = yi - ŷi, where yi is the observed value and ŷi is the corresponding model prediction [62]. These differences contain valuable information about model performance and potential assumption violations.
Several residual types facilitate different diagnostic purposes:
- Standardized residuals: Raw residuals scaled by their estimated standard deviation, facilitating comparison across observations [62]
- Pearson residuals: Standardized distances between observed and expected responses, particularly useful for generalized linear models [63]
- Deviance residuals: Based on contributions to the overall model deviance, often preferred for likelihood-based model comparisons [63]
- Randomized quantile residuals (RQRs): Transformed residuals that follow approximately standard normal distributions when models are correctly specified, especially valuable for discrete data [63]
Influence Diagnostics
Influence diagnostics identify observations that exert disproportionate effects on model parameters and predictions. Key concepts include:
- Outliers: Observations with response values unusual given their covariate patterns [64]
- Leverage: Measures how extreme an observation's predictor values are relative to others in the dataset [62] [65]
- Influence: The combined effect of being an outlier with high leverage, quantified by how much parameter estimates change when the observation is removed [64]
Comparative Analysis of Diagnostic Tools
Residual Types and Their Applications
Table 1: Comparison of Residual Types for Model Diagnostics
| Residual Type | Definition | Optimal Use Cases | Strengths | Limitations |
|---|---|---|---|---|
| Raw residuals | ri = yi - ŷi | Initial model checking, continuous outcomes | Simple interpretation, direct measure of error | Scale-dependent, difficult to compare across models |
| Standardized residuals | ri/√Var(ri) | Identifying unusual observations, outlier detection | Scale-invariant, facilitates outlier identification | Requires accurate variance estimation |
| Pearson residuals | Standardized distance between observed and expected values | Generalized linear models, count data | Familiar interpretation, widely supported | Non-normal for discrete data, parallel curves in plots |
| Deviance residuals | Signed √(contribution to deviance) | Model comparison, hierarchical models | Likelihood-based, comparable across nested models | Computation more complex |
| Randomized quantile residuals (RQRs) | Inverted CDF with randomization | Count regression, zero-inflated models | Approximately normal under correct specification, powerful for count data | Requires randomization, less familiar to practitioners |
Influence Measures and Detection Methods
Table 2: Influence Diagnostics and Their Interpretation
| Diagnostic Measure | Calculation | Purpose | Critical Threshold | Interpretation |
|---|---|---|---|---|
| Leverage (hat values) | Diagonal elements of hat matrix H = X(X^TX)^-1X^T | Identifies extreme predictor values | > 2p/n | High leverage points may unduly influence fits |
| Studentized residuals | ri/(s√(1 - hii)) | Flags outliers accounting for leverage | |ri*| > 2 or 3 | Unusual response given predictor values |
| Cook's distance | Combines residual size and leverage: (ri²/(p × s²)) × (hii/(1 - hii)²) | Measures overall influence on coefficients | > 4/(n - p - 1) | Identifies observations that change parameter estimates |
| DFFITS | Standardized change in predicted values | Assesses influence on predictions | > 2√(p/n) | Measures effect on fitted values |
| DFBETAS | Standardized change in each coefficient | Identifies influence on specific parameters | > 2/√n | Pinpoints which parameters are affected |
Experimental Protocols for Model Diagnostics
Comprehensive Residual Analysis Workflow
Figure 1: Comprehensive workflow for systematic residual analysis in predictive model validation.
Protocol 1: Systematic Residual Analysis
Calculate multiple residual types: Compute raw, standardized, and specialized residuals (Pearson, deviance, or RQRs) appropriate for your model family [62] [63]
Create diagnostic plots:
- Residuals vs. fitted values: Check for non-linearity, heteroscedasticity (non-constant variance), and outliers [62] [66]
- Residuals vs. predictor variables: Identify missing non-linear effects or interaction terms [64]
- Normal Q-Q plot: Assess normality assumption by comparing residual quantiles to theoretical normal quantiles [66] [65]
- Scale-location plot: Plot √\|standardized residuals\| against fitted values to visualize trends in variance [62]
Interpret patterns and test assumptions:
- Random scatter in residuals vs. fitted indicates well-specified model [66]
- Funnel-shaped patterns suggest heteroscedasticity, requiring variance-stabilizing transformations or weighted regression [62] [65]
- Systematic curved patterns indicate non-linearity, potentially addressed by adding polynomial terms or splines [64]
- Formally test homoscedasticity using Breusch-Pagan or White's tests [65]
Implement remedial measures:
- Apply variable transformations (log, square root) to address non-linearity or heteroscedasticity [65]
- Consider alternative model families (generalized linear models, robust regression) for severe assumption violations [65]
- For time series data, address autocorrelation using lagged terms or differencing [65]
Influence Diagnostic Protocol
Figure 2: Methodical approach for identifying and addressing influential observations in regression models.
Protocol 2: Comprehensive Influence Analysis
Compute influence statistics:
Visualize influence patterns:
Identify influential observations:
Address influential cases:
Performance Comparison in Different Scenarios
Diagnostic Power Across Model Types
Table 3: Comparative Performance of Residual Types for Different Data Scenarios
| Data Type | Residual Method | Non-linearity Detection | Over-dispersion Detection | Zero-inflation Detection | Outlier Identification |
|---|---|---|---|---|---|
| Continuous normal | Pearson residuals | High power | High power | N/A | High power |
| Count data (Poisson) | Pearson residuals | Moderate power | Low power | Low power | Moderate power |
| Count data (Poisson) | Deviance residuals | Moderate power | Low power | Low power | Moderate power |
| Count data (Poisson) | Randomized quantile residuals | High power | High power | High power | High power |
| Zero-inflated counts | Randomized quantile residuals | High power | High power | High power | High power |
| Binary outcomes | Pearson residuals | Moderate power | N/A | N/A | Moderate power |
Case Study: Healthcare Utilization Modeling
A recent methodological comparison examined residual diagnosis tools for count data in healthcare utilization research [63]. The study modeled repeated emergency department visits using:
- Models tested: Poisson, negative binomial, and zero-inflated Poisson regression
- Diagnostic comparison: Pearson residuals, deviance residuals, and randomized quantile residuals (RQRs)
- Performance metrics: Type I error rates and statistical power for detecting misspecification
Key findings:
- RQRs demonstrated approximately standard normal distribution under correct model specification
- RQRs showed superior statistical power for detecting non-linearity (92% vs. 65% for Pearson residuals)
- RQRs effectively identified over-dispersion (88% detection rate) and zero-inflation (85% detection rate)
- Traditional Pearson and deviance residuals exhibited low power (typically <50%) for identifying these misspecifications
- RQRs maintained appropriate type I error rates (≈5%) when models were correctly specified
Table 4: Key Software Implementations and Diagnostic Tools
| Tool/Software | Primary Function | Key Diagnostic Features | Implementation Example |
|---|---|---|---|
| R car package | Regression diagnostics | Influence plots, residual plots, variance inflation factors | influencePlot(model, id.n=3) |
| R stat package | Base statistics | Hat values, Cook's distance, Pearson residuals | cooks.distance(model) |
| Python statsmodels | Statistical modeling | Q-Q plots, residual plots, influence measures | statsmodels.graphics.influence_plot() |
| MoDeVa platform | Model validation | Automated residual analysis, performance comparison | TestSuite.diagnose_residual_analysis() |
| Custom R functions | Randomized quantile residuals | RQR calculation for count models | statmod::qresiduals(model) |
Residual analysis and influence diagnostics provide indispensable methodologies for refining predictive models across scientific disciplines. The comparative evidence presented demonstrates that diagnostic tool selection should align with data characteristics and model family, with randomized quantile residuals offering particular advantages for count data applications. For healthcare researchers and drug development professionals, these diagnostic procedures form a critical component of model validation, ensuring that predictive algorithms perform reliably before deployment in clinical decision-making. By implementing the systematic protocols and comparison frameworks outlined in this guide, researchers can enhance model robustness and ultimately improve the quality of scientific inferences drawn from predictive modeling efforts.
Addressing Common Challenges and Enhancing Model Robustness
In the field of machine learning and statistical modeling, overfitting represents a fundamental challenge that compromises the real-world utility of predictive systems. Overfitting occurs when a model learns the training data too well, capturing not only the underlying signal but also the noise and random fluctuations specific to that dataset [68]. This results in a model that demonstrates excellent performance on its training data but fails to generalize effectively to new, unseen data [69]. The opposite problem, underfitting, arises when a model is too simple to capture the underlying pattern in the data, performing poorly on both training and validation datasets [68]. For researchers in fields like drug development and biomedical science, where model predictions can inform critical decisions, effectively mitigating overfitting is not merely a technical exercise but a fundamental requirement for producing valid, reliable research.
The core of the overfitting problem lies in navigating the bias-variance tradeoff. Complex models with high capacity often achieve low bias (and excellent training performance) at the cost of high variance (poor generalization), while overly simple models may exhibit high bias but low variance [68]. Cross-validation and regularization techniques represent two complementary approaches to managing this tradeoff. Cross-validation provides a robust framework for estimating how well a model will generalize to unseen data, while regularization techniques actively constrain model complexity during the training process itself [70]. When used in concert, they form a powerful toolkit for developing models whose performance extends beyond the training dataset to deliver genuine predictive insight in scientific applications.
Theoretical Foundations: Cross-Validation and Regularization
Cross-Validation: Assessing Generalization Performance
Cross-validation is a resampling technique used to evaluate how well a machine learning model will perform on unseen data while simultaneously helping to prevent overfitting [71]. The core principle involves splitting the dataset into several parts, training the model on some subsets, and testing it on the remaining subsets in a rotating fashion. This process is repeated multiple times with different partitions, and the results are averaged to produce a final performance estimate that more reliably reflects true generalization capability [71].
Several cross-validation methodologies have been developed, each with distinct characteristics suited to different data scenarios:
K-Fold Cross-Validation: The dataset is randomly partitioned into k equal-sized folds. The model is trained k times, each time using k-1 folds for training and the remaining fold for testing. This process ensures each data point is used exactly once for validation [71]. The value of k is typically set to 10, as lower values move toward simple validation, while higher values approach the Leave-One-Out method [71].
Stratified Cross-Validation: A variation of k-fold that ensures each fold has the same class distribution as the full dataset. This is particularly valuable for imbalanced datasets where some classes are underrepresented, as it maintains proportional representation of all classes in each split [71].
Leave-One-Out Cross-Validation (LOOCV): An extreme form of k-fold where k equals the number of data points. The model is trained on all data except one point, which is used for testing, and this process is repeated for every data point. While LOOCV utilizes maximum data for training and produces low-bias estimates, it can be computationally expensive for large datasets and may yield high variance if individual points are outliers [71].
Holdout Validation: The simplest approach, where data is split once into training and testing sets, typically with 50-80% of data for training and the remainder for testing. While computationally efficient, this method can produce unreliable estimates if the single split is not representative of the overall data distribution [71].
Regularization: Constraining Model Complexity
Regularization encompasses a family of techniques that actively prevent overfitting by adding constraints to the model learning process. These methods work by penalizing model complexity, typically by adding a penalty term to the loss function that discourages the model from developing excessively complex patterns that may represent noise rather than true signal [68] [72].
The general form of a regularized regression problem can be expressed as minimizing the combination of a loss function and a penalty term: min_β{L(β) + λP(β)}, where L(β) is the loss function (e.g., negative log-likelihood), P(β) is the penalty function, and λ is the tuning parameter controlling the strength of regularization [72].
Several powerful regularization techniques have been developed for different modeling contexts:
L1 Regularization (LASSO): Adds a penalty equal to the absolute value of the magnitude of coefficients (
P(β) = ||β||₁ = Σ|β_j|) [72]. This approach tends to produce sparse models by driving some coefficients exactly to zero, effectively performing variable selection [69] [72]. LASSO is particularly valuable in high-dimensional settings where the number of predictors (p) exceeds the number of observations (n), though it tends to select at most n variables and can be biased for large coefficients [72].L2 Regularization (Ridge): Adds a penalty equal to the square of the magnitude of coefficients [69]. This technique discourages large coefficients but rarely reduces them exactly to zero, retaining all variables but with diminished influence [68]. L2 regularization is particularly effective for handling multicollinearity among predictors [72].
Elastic Net: Combines both L1 and L2 penalties, attempting to leverage the benefits of both approaches. This hybrid method is particularly useful when dealing with highly correlated predictors, where pure LASSO might arbitrarily select only one from a group of correlated variables [72].
Advanced Non-Convex Penalties: Methods like Smoothly Clipped Absolute Deviation (SCAD) and Minimax Concave Penalty (MCP) were developed to overcome the bias limitations of LASSO for large coefficients while maintaining its variable selection properties [72]. These non-convex penalties possess the "oracle property" (asymptotically performing as well as if the true model were known) but require more sophisticated optimization approaches and tuning of additional parameters [72].
Neural Network Regularization: For deep learning architectures, specialized techniques include Dropout, which randomly deactivates neurons during training to prevent over-reliance on any single neuron [68] [73], and Early Stopping, which halts training when performance on a validation set stops improving [68].
Table 1: Comparison of Regularization Techniques
| Technique | Penalty Type | Key Characteristics | Best Use Cases |
|---|---|---|---|
| L1 (LASSO) | Absolute value (Σ|β_j|) |
Produces sparse models; performs variable selection | High-dimensional data; feature selection |
| L2 (Ridge) | Squared value (Σβ_j²) |
Shrinks coefficients evenly; handles multicollinearity | Correlated predictors; when all features are relevant |
| SCAD | Non-convex | Reduces bias for large coefficients; oracle properties | When unbiased coefficient estimation is crucial |
| MCP | Non-convex | Similar to SCAD with different mathematical properties | Balancing variable selection and estimation accuracy |
| Dropout | Structural | Randomly disables neurons during training | Neural networks; preventing co-adaptation of features |
Comparative Analysis: Experimental Evidence and Performance
Performance in Medical Prediction Models
Substantial empirical evidence demonstrates the effectiveness of regularization techniques in biomedical research applications. In a study developing machine learning models to predict blastocyst yield in IVF cycles, regularization and feature selection played crucial roles in optimizing model performance [74]. Researchers employed recursive feature elimination (RFE) to identify optimal feature subsets, finding that models maintained stable performance with 8 to 21 features but showed sharp performance declines when features were reduced to 6 or fewer [74].
The study compared three machine learning models—Support Vector Machines (SVM), LightGBM, and XGBoost—alongside traditional linear regression. The regularized machine learning models demonstrated significantly superior performance (R²: 0.673-0.676, MAE: 0.793-0.809) compared to linear regression (R²: 0.587, MAE: 0.943) [74]. Among these, LightGBM emerged as the optimal model, achieving comparable performance to other approaches while utilizing fewer features (8 versus 10-11 for SVM and XGBoost), thereby reducing overfitting risk while enhancing clinical interpretability [74].
In depression risk prediction research, LASSO regression has proven valuable for feature selection in high-dimensional data. A study focused on predicting depression risk in physically inactive adults used LASSO to identify seven significant predictors from a broader set of potential variables [75]. The resulting model demonstrated robust performance (AUC = 0.769) and maintained stable generalizability across multiple validation sets, highlighting how regularization can yield clinically applicable models with enhanced interpretability [75].
Table 2: Performance Comparison of Regularized Models in Biomedical Research
| Study/Application | Algorithms Compared | Key Performance Metrics | Optimal Model |
|---|---|---|---|
| Blastocyst Yield Prediction [74] | SVM, LightGBM, XGBoost, Linear Regression | R²: 0.673-0.676 vs 0.587; MAE: 0.793-0.809 vs 0.943 | LightGBM (fewer features, less overfitting risk) |
| Depression Risk Prediction [75] | LASSO + Logistic Regression | AUC: 0.769; Stable across validation sets | Regularized logistic regression |
| Image Classification [73] | CNN, ResNet-18 | Validation accuracy: 68.74% (CNN) vs 82.37% (ResNet-18) | ResNet-18 with regularization |
Image Classification and Deep Learning Applications
In image classification tasks, the combination of architectural innovations and regularization techniques has demonstrated significant impacts on generalization performance. A comparative deep learning analysis examined regularization techniques on both baseline CNNs and ResNet-18 architectures using the Imagenette dataset [73]. The results showed that ResNet-18 achieved superior validation accuracy (82.37%) compared to the baseline CNN (68.74%), and that regularization consistently reduced overfitting and improved generalization across all experimental scenarios [73].
The study further revealed that transfer learning—a approach where models pre-trained on large datasets are fine-tuned for specific tasks—provided additional benefits when combined with regularization. Fine-tuned models converged faster and attained higher accuracy than those trained from scratch, demonstrating the complementary relationship between architectural choices, transfer learning, and regularization strategies [73]. These findings underscore that in complex domains like medical imaging, successful mitigation of overfitting often requires combining multiple approaches rather than relying on a single technique.
Complementary Roles in Model Development
Cross-validation and regularization serve distinct but complementary roles in the model development process [70]. Regularization actively constrains model complexity during training, while cross-validation provides a framework for assessing generalization performance and tuning hyperparameters [70]. This relationship is particularly evident in the process of selecting the optimal regularization parameter (λ).
As one respondent on Stack Exchange clarified, "Cross validation and regularization serve different tasks. Cross validation is about choosing the 'best' model, where 'best' is defined in terms of test set performance. Regularization is about simplifying the model. They could, but do not have to, result in similar solutions. Moreover, to check if the regularized model works better than unregularized you would still need cross validation" [70].
This interplay is especially important in high-dimensional settings where the number of predictors exceeds the number of observations (p > n). In such cases, comparing all possible feature combinations would be computationally prohibitive (requiring examination of 2^p possible models), but regularization techniques like LASSO can efficiently perform variable selection in a single step [70]. Cross-validation then provides the mechanism for determining the appropriate strength of the regularization penalty.
Implementation Protocols: Methodological Approaches
Experimental Workflow for Regularization and Cross-Validation
The following diagram illustrates the integrated experimental workflow combining cross-validation and regularization for developing robust predictive models:
K-Fold Cross-Validation Process
The k-fold cross-validation mechanism, central to reliable model evaluation, operates through the following systematic procedure:
Python Implementation Code
For practical implementation, the following code demonstrates how to integrate cross-validation with regularized models using Python and scikit-learn:
Table 3: Research Reagent Solutions for Model Validation Studies
| Tool/Resource | Function/Purpose | Example Applications |
|---|---|---|
| LASSO Regression | Variable selection & regularization via L1 penalty | Identifying key biomarkers from high-dimensional data [72] [75] |
| SCAD/MCP Regularization | Non-convex penalties reducing estimation bias | When unbiased coefficient estimation is critical [72] |
| K-Fold Cross-Validation | Robust performance estimation via data partitioning | Model evaluation with limited sample sizes [71] |
| Stratified Cross-Validation | Maintains class distribution in imbalanced datasets | Medical diagnostics with rare disease outcomes [71] |
| Dropout Regularization | Random neuron deactivation in neural networks | Deep learning architectures for image analysis [68] [73] |
| Early Stopping | Halts training when validation performance plateaus | Preventing overfitting in iterative learning algorithms [68] |
| Recursive Feature Elimination | Iteratively removes least important features | Identifying optimal feature subsets [74] |
Cross-validation and regularization are not competing approaches but complementary pillars in the construction of generalizable predictive models. Cross-validation provides the essential framework for evaluating model performance and tuning hyperparameters, while regularization actively constrains model complexity during training to prevent overfitting [70]. The experimental evidence across diverse domains—from medical diagnostics to image classification—consistently demonstrates that their integrated application yields models with superior generalization capabilities [74] [73] [75].
For researchers in drug development and biomedical science, where predictive accuracy directly impacts scientific validity and clinical decisions, the strategic implementation of these techniques is paramount. The optimal approach typically involves using cross-validation to guide the selection of appropriate regularization strength and other hyperparameters, creating a systematic workflow that balances model complexity with predictive performance [71] [70]. As machine learning applications continue to expand in scientific research, mastering these fundamental validation and regularization strategies remains essential for producing models that deliver genuine insight rather than merely memorizing training data.
In the development of predictive models for critical applications such as drug development and medical diagnosis, class imbalance presents a fundamental challenge that can severely compromise model utility. Imbalanced datasets, where one class significantly outnumbers others, are prevalent in real-world scenarios from financial distress prediction to disease detection [76] [77]. When machine learning algorithms are trained on such data, they often develop a prediction bias toward the majority class, resulting in poor performance for the minority class that is frequently of greater interest and clinical importance [77] [78].
The statistical validation of models developed from imbalanced data requires specialized approaches, as traditional performance metrics like overall accuracy can be profoundly misleading [78] [79]. For instance, a model that simply classifies all cases as the majority class can achieve high accuracy while being clinically useless for identifying the critical minority cases [79]. This challenge has spurred the development of two principal technical approaches: data-level resampling techniques that adjust training set composition, and algorithm-level methods including cost-sensitive learning that modifies how models account for errors during training [80] [81].
Within a rigorous statistical validation framework, researchers must carefully evaluate how these imbalance-handling techniques affect not only discrimination but also calibration - the accuracy of predicted probabilities - which is crucial for informed clinical decision-making [9] [78]. This guide provides an objective comparison of these methods based on recent experimental evidence, with particular emphasis on their performance within validation paradigms relevant to pharmaceutical research and development.
Resampling Techniques: Methodological Approaches and Experimental Evidence
Resampling techniques address class imbalance by adjusting the composition of the training dataset through various strategic approaches. These methods are broadly categorized into oversampling, undersampling, and hybrid techniques, each with distinct mechanisms and implementation considerations.
Oversampling Techniques
Oversampling methods augment the minority class by generating additional instances, with approaches ranging from simple duplication to sophisticated synthetic generation:
SMOTE (Synthetic Minority Oversampling Technique): Generates synthetic minority class instances by interpolating between existing minority instances and their nearest neighbors [76]. While effective in many scenarios, it can introduce noise when minority class instances are sparsely distributed [76].
Borderline-SMOTE: A refinement that focuses specifically on generating samples near the class boundary rather than throughout the entire minority class, operating on the premise that boundary samples are most critical for classification [76].
ADASYN (Adaptive Synthetic Sampling): Extends SMOTE by adaptively focusing on minority class instances that are harder to learn, increasing the sampling rate for instances near decision boundaries or frequently misclassified [76].
Undersampling Techniques
Undersampling methods balance datasets by reducing majority class instances:
Random Undersampling (RUS): Randomly removes instances from the majority class until balance is achieved [76]. While computationally efficient and fast, it carries the risk of discarding potentially important information from the majority class [76] [79].
Tomek Links: Identifies and removes majority class instances that form "Tomek Links" - pairs of instances from different classes where each is the nearest neighbor of the other - effectively cleaning the decision boundary [76].
Hybrid Techniques
Hybrid methods combine both oversampling and undersampling approaches:
SMOTE-Tomek: Applies SMOTE for oversampling followed by Tomek Links for cleaning the resulting dataset by removing noisy majority samples near minority instances [76].
SMOTE-ENN: Integrates SMOTE with Edited Nearest Neighbors (ENN) to delete misclassified majority samples post-oversampling, further refining decision boundaries [76].
Bagging-SMOTE: An ensemble-based resampling approach that maintains robust performance with minimal impact on original class distribution, though with higher computational requirements [76].
Experimental Performance Comparison
Recent comparative studies provide quantitative evidence of how these resampling techniques perform across various metrics relevant to imbalanced classification. The table below summarizes results from a comprehensive evaluation of resampling techniques for financial distress prediction using XGBoost, which is methodologically analogous to medical prediction tasks.
Table 1: Performance Comparison of Resampling Techniques with XGBoost Classifier [76]
| Resampling Technique | AUC | F1-Score | Recall | Precision | MCC | Computational Efficiency |
|---|---|---|---|---|---|---|
| No Resampling (Baseline) | 0.92 | 0.65 | 0.68 | 0.63 | 0.62 | Reference |
| SMOTE | 0.95 | 0.73 | 0.75 | 0.71 | 0.70 | Medium |
| Borderline-SMOTE | 0.94 | 0.72 | 0.78 | 0.67 | 0.68 | Medium |
| ADASYN | 0.94 | 0.71 | 0.76 | 0.67 | 0.67 | Medium |
| Random Undersampling (RUS) | 0.89 | 0.61 | 0.85 | 0.46 | 0.58 | High |
| Tomek Links | 0.93 | 0.68 | 0.71 | 0.66 | 0.65 | Medium |
| SMOTE-Tomek | 0.95 | 0.72 | 0.79 | 0.66 | 0.69 | Medium-Low |
| SMOTE-ENN | 0.94 | 0.71 | 0.77 | 0.66 | 0.68 | Low |
| Bagging-SMOTE | 0.96 | 0.72 | 0.74 | 0.70 | 0.68 | Low |
A separate study examining logistic regression models for ovarian cancer diagnosis revealed important considerations about resampling effects on probability calibration, with critical implications for clinical utility:
Table 2: Effect of Resampling on Model Calibration (Ovarian Cancer Diagnosis) [78]
| Method | AUROC | Calibration Intercept | Calibration Slope | Sensitivity | Specificity |
|---|---|---|---|---|---|
| No Correction | 0.841 | 0.02 (good) | 0.98 (good) | 0.65 | 0.85 |
| Random Oversampling | 0.840 | -0.78 (overestimation) | 0.95 (slight overfitting) | 0.76 | 0.77 |
| Random Undersampling | 0.837 | -0.81 (overestimation) | 0.94 (slight overfitting) | 0.78 | 0.75 |
| SMOTE | 0.839 | -0.75 (overestimation) | 0.96 (slight overfitting) | 0.77 | 0.76 |
The experimental data indicates that while resampling techniques generally improve sensitivity for minority class detection, they often compromise calibration by leading to systematically overestimated probabilities [78]. This calibration distortion represents a significant limitation for clinical applications where accurate probability estimates directly inform treatment decisions.
Cost-Sensitive Learning: Algorithm-Level Approaches
Cost-sensitive learning addresses class imbalance at the algorithmic level by assigning different misclassification costs during model training, explicitly making errors on the minority class more "expensive" than errors on the majority class [80] [81]. This approach preserves the original data distribution while embedding awareness of the asymmetric consequences of different error types directly into the learning process.
Fundamental Principles
The foundation of cost-sensitive learning lies in modifying the loss function to incorporate a cost matrix that reflects real-world clinical or business implications:
Table 3: Cost Matrix Structure for Clinical Prediction Models
| Predicted: Negative | Predicted: Positive | |
|---|---|---|
| Actual: Negative | C(0,0) = 0 (True Negative) | C(0,1) = Cost of False Positive |
| Actual: Positive | C(1,0) = Cost of False Negative | C(1,1) = 0 (True Positive) |
In this framework, C(1,0) (false negative cost) typically substantially exceeds C(0,1) (false positive cost) in clinical contexts, such as failing to identify patients with a serious condition versus unnecessary further testing [81]. This cost asymmetry is formally incorporated into the model's optimization objective function.
Implementation Approaches
Cost-sensitive learning can be implemented through several technical strategies:
Direct Cost-Sensitive Methods: Modify the learning algorithm itself to minimize misclassification costs during training, such as cost-sensitive splitting criteria in decision trees or cost-weighted loss functions in gradient boosting [80].
Meta-Cost Frameworks: Wrapper approaches that make standard algorithms cost-sensitive through relabeling or weighting instances based on their misclassification costs [81].
Cost-Sensitive Ensembles: Methods like RUSBoost that combine data sampling with cost-sensitive boosting algorithms [76].
Experimental Evidence
Recent studies demonstrate the effectiveness of cost-sensitive approaches for imbalanced classification. A study on business failure prediction using data from the Iranian capital market found that cost-sensitive implementations of powerful gradient boosting algorithms like CatBoost achieved high sensitivity while maintaining reasonable overall performance [81]. Specifically, cost-sensitive CatBoost achieved a sensitivity of 0.909 for identifying failing businesses, significantly outperforming standard implementations without explicit cost sensitivity [81].
Another study developing cost-sensitive variants of logistic regression, decision trees, and extreme gradient boosting for medical diagnosis found that these approaches "yield superior performance compared to the standard algorithms" while avoiding the distributional distortion introduced by resampling techniques [80]. The preservation of the original data distribution provides a significant advantage for maintaining the representativeness of validation samples.
Integrated Methodological Workflow
The comprehensive approach to handling imbalanced datasets within a rigorous validation framework involves multiple interconnected methodological stages, from initial problem formulation through final model validation:
Diagram 1: Methodological Workflow for handling imbalanced datasets
This workflow emphasizes the critical importance of proper validation techniques at each stage, particularly the assessment of both discrimination and calibration performance metrics. The selection between resampling and cost-sensitive approaches depends on multiple factors including dataset characteristics, computational constraints, and the specific clinical requirements for probability accuracy versus classification performance.
The Researcher's Toolkit: Essential Methodological Components
Implementing effective solutions for imbalanced data requires both conceptual understanding and practical tools. The following table summarizes key methodological components and their functions in addressing class imbalance challenges:
Table 4: Essential Methodological Components for Imbalanced Data Research
| Component | Function | Implementation Examples |
|---|---|---|
| Resampling Algorithms | Adjust training set composition to balance class distribution | SMOTE, Borderline-SMOTE, ADASYN, Random Undersampling, Tomek Links [76] |
| Cost-Sensitive Frameworks | Incorporate differential misclassification costs directly into learning algorithms | Cost-sensitive logistic regression, Cost-sensitive XGBoost, RUSBoost [80] [81] |
| Ensemble Methods | Combine multiple models to improve robustness on minority class | Balanced Random Forests, EasyEnsemble, Bagging-SMOTE [76] [82] |
| Performance Metrics | Evaluate model performance beyond accuracy | F1-score, AUC-PR, Matthews Correlation Coefficient (MCC), Balanced Accuracy [76] [9] |
| Calibration Assessment Tools | Validate accuracy of predicted probabilities | Calibration curves, Brier score, Expected Calibration Error [9] [78] |
| Validation Techniques | Ensure reliable performance estimation | Repeated cross-validation, bootstrap validation, external validation [9] |
| Threshold Optimization | Find optimal classification thresholds for clinical utility | Decision curve analysis, cost-benefit analysis [78] |
Comparative Analysis and Decision Framework
The choice between resampling and cost-sensitive approaches involves trade-offs across multiple dimensions, with the optimal selection dependent on specific research context and requirements:
Diagram 2: Decision Framework for selecting imbalance handling techniques
Key Comparative Insights
Experimental evidence reveals several critical patterns in the performance of different approaches:
Resampling advantages: Techniques like SMOTE and Bagging-SMOTE consistently demonstrate strong performance across multiple metrics, with Bagging-SMOTE achieving AUC of 0.96 in financial distress prediction [76]. These methods are particularly valuable when using weaker classifiers or when probability outputs are not required [82].
Cost-sensitive strengths: Cost-sensitive learning preserves the original data distribution and avoids the calibration problems common with resampling methods, while achieving competitive sensitivity (e.g., 0.909 with cost-sensitive CatBoost) [81]. This makes it particularly suitable for clinical applications where probability accuracy matters.
Threshold optimization alternative: Simple threshold adjustment often achieves similar classification performance to resampling without distorting probability calibration [82] [78]. For strong classifiers like XGBoost and CatBoost, threshold optimization may render resampling unnecessary [82].
Computational considerations: Random undersampling offers superior computational efficiency for large datasets [76] [79], while complex hybrid methods like SMOTE-ENN and Bagging-SMOTE have significantly higher computational demands [76].
Within the rigorous framework of statistical validation for predictive models, both resampling and cost-sensitive learning offer viable approaches to addressing class imbalance, with the optimal choice dependent on specific research constraints and objectives. Resampling techniques, particularly sophisticated methods like Bagging-SMOTE and SMOTE-Tomek, provide powerful solutions for improving minority class identification, but often at the cost of probability calibration [76] [78]. Cost-sensitive learning preserves calibration and original data distribution while directly incorporating clinical cost asymmetries, making it particularly valuable for medical applications [80] [81].
Future research directions include developing more advanced density-based resampling approaches that better account for feature importance and instance distribution [77], creating more computationally efficient hybrid algorithms suitable for large-scale biomedical data [79], and establishing standardized validation frameworks specifically designed for imbalanced learning scenarios in clinical contexts [9] [78]. For drug development professionals and researchers, the current evidence supports a preference for cost-sensitive approaches when accurate probability estimation is required, with reserving resampling techniques for scenarios focused primarily on classification performance with weaker learners or when probability outputs are not utilized.
The most robust approach to model validation with imbalanced data involves implementing multiple complementary strategies - potentially including both resampling and cost-sensitive techniques - within a comprehensive internal validation framework using resampling methods like bootstrapping or repeated cross-validation, followed by external validation in fully independent datasets [9]. This multi-faceted validation strategy ensures that performance estimates reflect true generalizability rather than methodological artifacts of the imbalance handling techniques themselves.
Identifying and Managing Influential Outliers and High-Leverage Points
Conceptual Definitions and Distinctions
In predictive regression modeling, not all unusual observations are created equal. Accurate diagnosis hinges on understanding the precise definitions and interrelationships between outliers, high-leverage points, and influential points [83] [84].
- Outliers: An outlier is an observation whose response (y-value) does not follow the general trend of the rest of the data, resulting in a large residual [83] [85]. It is identified by its extreme value in the dependent variable.
- High-Leverage Points: A high-leverage point has an extreme or unusual combination of predictor (x-) values compared to the other data points [83] [86]. In multiple regression, this can mean a value that is particularly high or low for one or more predictors, or an unusual combination of predictor values [83]. These points have the potential to exert a strong pull on the regression line.
- Influential Points: A point is influential if its inclusion or exclusion from the model causes substantial changes to the regression analysis [83] [86]. This can include significant shifts in the predicted responses, the estimated slope coefficients, the intercept, or the hypothesis test results [83] [87]. Influence is the ultimate effect on the model.
The key distinction is that a high-leverage point is not necessarily an outlier, and an outlier does not always have high leverage [83] [88]. However, an observation that is both an outlier and a high-leverage point is very likely to be influential [83] [85].
Impact on Regression Model Estimates
The presence of these unusual observations can skew insights, dilute statistical power, and mislead decision-making, which is particularly critical in fields like drug development [89].
Table 1: Comparative Impact of Unusual Observations on Regression Models
| Observation Type | Impact on Slope (β1) | Impact on R-squared (R²) | Impact on Standard Error |
|---|---|---|---|
| Outlier (Y-extreme) | Minimal to Moderate Change | Decreases Slightly | Increases [83] |
| High-Leverage Point (X-extreme) | Minimal Change if on trend [83] | Can Inflate Strength [86] | Largely Unaffected [83] |
| Influential Point | Significant Change [83] | Substantial Change [83] | Can Increase Dramatically [83] |
The most dramatic effects occur when a single point is both an outlier and has high leverage. Its removal can significantly alter the regression slope and reduce the standard error, thereby changing the practical and statistical conclusions drawn from the model [83] [90]. For example, in a biocomputational analysis, a single outlier can disproportionately skew regression coefficients, leading to over- or under-estimation of effects [89].
Experimental Protocols for Detection and Diagnosis
A robust diagnostic workflow is essential for statistical validation. The following protocol provides a step-by-step methodology for identifying and assessing unusual observations.
Diagram 1: Statistical Diagnostic Workflow for Unusual Observations
Protocol 1: Diagnostic Calculations and Workflow
This protocol outlines the core computational steps for detecting unusual observations, leveraging standard outputs from most statistical software [86] [90].
- Model Fitting: Begin by fitting the proposed regression model to the entire dataset.
- Residual Calculation: Calculate the studentized residuals for each observation. Unlike raw residuals, studentized residuals are divided by an estimate of their standard deviation, making them more effective for comparing across observations and detecting outliers [90].
- Leverage Calculation: Compute the leverage values (diagonal elements of the hat matrix, often denoted as hᵢ₊). Leverage measures the potential influence of an observation based solely on its position in the predictor space [86] [87].
- Influence Calculation: Calculate Cook's Distance (often denoted as Dᵢ) for each observation. This metric measures the combined effect of an observation's leverage and its residual, quantifying its overall influence on the model's coefficient estimates [86] [90].
- Iterative Diagnosis: If influential points are identified and handled (e.g., removed or corrected), the model must be re-fit and the diagnostic process repeated to ensure no new issues have been introduced and that the model is stable.
Protocol 2: Establishing Diagnostic Thresholds
Formal identification requires comparing calculated metrics against established statistical thresholds.
Table 2: Statistical Thresholds for Identifying Unusual Observations
| Metric | Calculation | Diagnostic Threshold | Interpretation |
|---|---|---|---|
| Studentized Residual | Residual / (External Std. Error) | Absolute Value > 2 or 3 [90] | Flags potential outliers. |
| Leverage (hᵢ) | Diagonal of Hat Matrix | > 2p/n (where p=# of parameters, n=sample size) [86] | Flags high-leverage points. |
| Cook's Distance (D) | Function of leverage and residual | > 1.0 or "sticks out" from others [90] | Flags influential points. |
- Outlier Flag: An observation with an absolute studentized residual greater than 2 or 3 is considered a potential outlier, as it is unusually far from the regression line relative to other points [90].
- Leverage Flag: The mean leverage value is p/n. A common rule of thumb is that observations with leverage values greater than 2p/n are considered to have high leverage [86].
- Influence Flag: Cook's Distance values above 1.0 are generally considered influential. However, any observation with a Cook's D that is substantially larger than the others in the dataset warrants investigation [90].
Comparison of Statistical Software and Tools
Different software environments offer varied implementations of these diagnostic tests. The following comparison focuses on the practical application within research contexts.
"The Scientist's Toolkit": Essential Diagnostic Reagents
Table 3: Key Software Tools and Diagnostic Functions for Researchers
| Software / Package | Key Functions for Detection | Primary Application Context |
|---|---|---|
| R Statistical Language | olsrr::ols_plot_cooksd_bar(), car::outlierTest(), influence.measures() |
Comprehensive statistical analysis and method development [91]. |
| Python (statsmodels) | get_influence().hat_matrix_diag, cooks_distance, outlier_test() |
Integration with machine learning pipelines and general-purpose data science [87]. |
| JMP | Automatic plots for Studentized Residuals, Leverage, and Cook's D in fit model platform [90] | Interactive GUI-based analysis for rapid prototyping and visualization. |
| Minitab | Regression diagnostics output within regression analysis menu [86] | Industrial statistics and quality control with straightforward menu navigation. |
Analytical Workflow Comparison
While the underlying statistics are consistent, the workflow differs significantly between programming-based and GUI-based tools.
- Programming-Based (R/Python): Offer the highest degree of flexibility and reproducibility. Researchers can script the entire diagnostic workflow, creating custom plots and automated reports. This is essential for large-scale biocomputational analyses, such as screening thousands of compounds in drug discovery [91]. The
statsmodelslibrary in Python, for instance, provides direct access to hat matrix diagonals and Cook's Distance, allowing for integration into larger machine-learning pipelines [87]. - GUI-Based (JMP/Minitab): Provide excellent accessibility for iterative, exploratory analysis. They automatically generate a suite of diagnostic plots (e.g., Residual by Predicted, Leverage plots) alongside numerical outputs, making it easier for researchers to visually identify and understand unusual observations without writing code [86] [90]. JMP's interactive linking of plots and data tables is particularly useful for investigating the source of an influential point.
Management Strategies for Influential Data Points
Once identified, the approach to handling influential points must be scientifically rigorous and documented.
- Investigation and Verification: The first step is never automatic deletion. Investigate the influential point for potential data entry errors, measurement issues, or sampling anomalies [87]. In drug development, this could involve checking lab instrumentation logs or sample contamination records [89].
- Robust Statistical Techniques: Consider using statistical methods that are less sensitive to extreme values. These can include:
- Winsorization: Replacing extreme values with less extreme but still plausible values from the dataset [87].
- Data Transformation: Applying logarithms or other transformations to make the data distribution more symmetrical and reduce the impact of extremes [87].
- Robust Regression: Employing regression methods designed to down-weight the influence of outliers, such as M-estimation or Least Trimmed Squares [90].
- Reporting and Sensitivity Analysis: A transparent approach is to report the results of the model both with and without the influential observations [83]. This sensitivity analysis demonstrates the robustness (or lack thereof) of the findings and allows other researchers to assess the impact of these points for themselves. A trend that does not survive the removal of high-leverage outlier data points may be spurious [89].
- Domain Knowledge Integration: The final decision should be guided by subject-matter expertise. If an influential point is a biologically implausible artifact, removal may be justified. If it represents a valid, albeit rare, biological phenomenon, it may be critical to retain and model appropriately [89].
Predictive models are crucial tools in clinical decision-making and drug development, yet their performance is not static. Over time, changes in underlying clinical populations, evolving medical practices, and shifts in data generation processes can lead to model decay and performance deterioration [92] [93]. This phenomenon poses significant challenges for researchers and drug development professionals who rely on these models for critical decisions. Without systematic updating, even well-validated models can become unreliable, potentially compromising patient care and drug development efficiency.
The healthcare setting presents unique challenges for model maintenance, where errors have more serious repercussions, sample sizes are often smaller, and data tend to be noisier compared to other industries [93]. Within this context, three principal model updating strategies have emerged: recalibration, revision, and dynamic updating. This guide provides an objective comparison of these approaches, supported by experimental data and detailed methodologies, to inform researchers and scientists in their model maintenance practices.
Core Model Updating Strategies: Definitions and Applications
Recalibration
Recalibration adjusts a model's output without altering the underlying model structure or coefficients. It focuses on modifying the intercept and/or slope of the model to better align predictions with observed outcomes.
- Intercept Recalibration: Adjusts the baseline risk estimate to match the overall event rate in the new population.
- Slope Recalibration: Modifies the strength of association between predictors and outcome.
- Intercept and Slope Recalibration: Combines both approaches for comprehensive calibration adjustment.
Recalibration is particularly valuable when the fundamental relationships between predictors and outcomes remain stable, but their baseline levels or strengths have shifted [92].
Revision (Refitting)
Revision, also known as refitting, involves more substantial changes to the model, including modifying existing predictor coefficients, adding new predictors, or removing existing ones. This approach essentially redevelops parts of the model structure to better capture relationships in the new data [92]. Revision becomes necessary when the original model suffers from substantial miscalibration or when new important predictors become available.
Dynamic Updating
Dynamic updating represents a systematic approach to maintaining model performance over time through regular, scheduled updates. This strategy involves updating models at multiple time points as new data are accrued, employing either recalibration or revision methods based on performance metrics and statistical testing [92]. Dynamic updating frameworks can incorporate various intervals for reassessment and different amounts of historical data in each update.
Comparative Performance Analysis
Quantitative Comparison of Update Strategies
Experimental comparisons of updating strategies provide crucial insights for researchers selecting appropriate maintenance approaches. A comprehensive study comparing dynamic updating strategies for predicting 1-year post-lung transplant survival yielded the following performance data [92]:
Table 1: Performance Comparison of Update Strategies for Predicting 1-Year Post-Lung Transplant Survival
| Update Strategy | Brier Score Improvement | Discrimination (C-statistic) | Calibration Performance | Sensitivity to Update Interval | Sensitivity to Window Length |
|---|---|---|---|---|---|
| Never Update | Reference | 0.71 | Poor | N/A | N/A |
| Closed Testing Procedure | Moderate improvement | 0.74 | Variable | High | High |
| Intercept Recalibration | Significant improvement | 0.76 | Good | Low | Low |
| Intercept + Slope Recalibration | Significant improvement | 0.77 | Excellent | Low | Low |
| Model Revision (Refitting) | Significant improvement | 0.78 | Good | High | High |
Impact of Update Frequency and Data Volume
The same study investigated how update frequency and the amount of historical data used in updates affected model performance [92]:
Table 2: Impact of Update Parameters on Model Performance
| Update Parameter | Setting | Impact on Brier Score | Impact on Discrimination | Impact on Calibration |
|---|---|---|---|---|
| Update Interval | Every 1 quarter | Best performance | Best | Best |
| Every 2 quarters | Good performance | Good | Good | |
| Every 4 quarters | Moderate performance | Moderate | Moderate | |
| Every 8 quarters | Poor performance | Poor | Poor | |
| Sliding Window Length | 1 quarter new (100% new) | Good for recalibration | Variable for revision | Good for recalibration |
| 1 quarter new + 1 quarter old (50%/50%) | Good for recalibration | Good for revision | Good for recalibration | |
| 1 quarter new + 3 quarters old (25%/75%) | Good for recalibration | Better for revision | Good for recalibration | |
| 1 quarter new + 7 quarters old (12.5%/87.5%) | Good for recalibration | Best for revision | Good for recalibration |
Clinical Implementation Landscape
The current state of clinical implementation of prediction models reveals significant gaps in updating practices. A comprehensive review of 37 articles describing 56 clinically implemented prediction models found that [94]:
- Only 27% of models underwent external validation before implementation
- Just 13% of models have been updated following implementation
- 86% of publications had high risk of bias
- Implementation routes included: Hospital Information Systems (63%), web applications (32%), and patient decision aid tools (5%)
This implementation gap highlights the need for more systematic approaches to model maintenance in clinical and drug development settings.
Experimental Protocols and Methodologies
Dynamic Updating Experimental Protocol
The methodology from the lung transplant survival prediction study provides a robust template for evaluating updating strategies [92]:
Data Partitioning
- Baseline period: 2007-2009 (2,853 patients, 508 events)
- Post-baseline period: 2010-2015 (10,948 patients, 1,449 events)
- Quarterly cohorts: Mean 456.2 patients per quarter, 60.4 events per quarter
Model Updating Workflow
- Baseline model developed using 2007-2009 data
- Model tested on Q1 2010 cohort
- Model updated using Q1 2010 cohort data according to each strategy
- Updated model tested on Q2 2010 cohort
- Process repeated for subsequent quarters
Performance Metrics
- Brier Score: Measure of overall model performance
- C-statistic: Measure of discrimination
- Calibration Metrics: Hosmer-Lemeshow statistic, calibration intercepts, calibration slopes
- Statistical Testing: Wilcoxon signed rank tests for strategy comparisons
Recalibration Techniques
Intercept Recalibration
- Fit a logistic regression model with the original linear predictor as the only covariate
- Estimate only the intercept, fixing the slope at 1
- Adjusts baseline risk without changing predictor effects
Intercept and Slope Recalibration
- Fit a logistic regression model with the original linear predictor as a covariate
- Estimate both intercept and slope parameters
- Adjusts both baseline risk and strength of predictor effects
Model Revision Protocol
Closed Testing Procedure
- Test whether updating significantly improves model fit
- If significant, proceed with model revision
- If not significant, retain original model
- Uses statistical testing to guide update decisions
Complete Model Refitting
- Use new data to re-estimate all model coefficients
- Optionally add or remove predictors based on new data
- Essentially redevelops the model on more recent data
Visualizing Model Updating Workflows
Dynamic Model Updating Framework
Dynamic Updating Process Flow
This diagram illustrates the sequential process for dynamic model updating, showing how models are continuously tested, updated, and evaluated using new data quarters.
Strategy Selection Framework
Update Strategy Selection Guide
This decision framework guides researchers in selecting appropriate updating strategies based on the nature and severity of performance decay.
Table 3: Research Reagent Solutions for Model Updating Studies
| Resource Category | Specific Tools/Solutions | Function/Purpose | Key Features |
|---|---|---|---|
| Statistical Software | R Statistical Environment | Implementation of recalibration and revision methods | Comprehensive packages for predictive modeling (rms, caret, pmsamps) |
| Performance Metrics | Brier Score, C-statistic, Calibration Plots | Quantitative assessment of model performance | Measures overall performance, discrimination, and calibration |
| Data Infrastructure | Hospital Information Systems (HIS), Web Applications | Model implementation and data collection | Platforms for deploying and monitoring clinical prediction models [94] |
| Validation Frameworks | TRIPOD, PROBAST | Guidance for transparent reporting and risk of bias assessment | Ensures methodological rigor in model development and validation [94] |
| Drug Development Databases | Pharmaprojects, Trialtrove | Comprehensive drug and clinical trial data | Provides features for predicting drug approval outcomes [95] |
The comparative analysis of model updating strategies reveals several key insights for researchers and drug development professionals. Recalibration strategies provide consistent improvements with low sensitivity to update intervals and window lengths, making them particularly suitable for environments with limited data or computational resources [92]. Model revision offers potentially greater performance gains but requires more data and computational effort, with higher sensitivity to update parameters.
Dynamic updating frameworks demonstrate that more frequent updates generally yield better performance across all strategies, highlighting the importance of continuous monitoring and maintenance [92] [93]. The finding that only 13% of clinically implemented models undergo updating indicates a significant implementation gap that researchers should address [94].
For drug development applications, these updating strategies can enhance predictive modeling for drug approval outcomes, where machine learning approaches have achieved AUCs of 0.78 for phase 2 to approval predictions and 0.81 for phase 3 to approval predictions [95]. As predictive models become increasingly integrated into clinical care and drug development, establishing systematic approaches to model updating will be essential for maintaining their long-term safety, effectiveness, and scientific validity.
In predictive model research, particularly within drug development and healthcare, data quality remains a foundational challenge directly influencing model reliability and clinical applicability. The "garbage in, garbage out" principle is especially pertinent when building models from real-world data, which invariably contains missing values and high-dimensional features. Statistical validation techniques provide the framework for assessing how different methodological approaches to these data quality issues impact ultimate model performance. This guide objectively compares prevalent methods for handling missing data and performing feature selection, drawing on empirical evidence to inform researchers and scientists in selecting optimal strategies for their predictive modeling pipelines.
Comparative Analysis of Missing Data Imputation Methods
Missing data is an inevitable challenge in clinical and cohort studies that, if improperly handled, can introduce bias, reduce statistical power, and diminish predictive model accuracy. The performance of various imputation methods has been quantitatively evaluated in comparative studies, providing evidence-based guidance for researchers.
Experimental Protocol: Benchmarking Imputation Methods
A comprehensive evaluation framework was employed in a 2024 study comparing eight statistical and machine learning imputation methods using a real-world cardiovascular disease cohort dataset from Xinjiang, China. The experimental design included several key components [96]:
- Dataset: 10,164 subjects with 37 variables encompassing personal information, physical examinations, questionnaires, and laboratory results.
- Missing Data Mechanism: Assumed Missing at Random for method evaluation.
- Missing Rate: 20% missingness was introduced for controlled evaluation.
- Performance Metrics: Root Mean Square Error and Mean Absolute Error assessed imputation accuracy.
- Predictive Validation: Imputed datasets were used to construct cardiovascular disease risk prediction models using Support Vector Machines, with performance evaluated via Area Under the Curve.
This robust protocol enabled direct comparison of method efficacy across both imputation accuracy and downstream predictive performance.
Quantitative Performance Comparison of Imputation Techniques
Table 1: Performance comparison of missing data imputation methods
| Imputation Method | Mean Absolute Error (MAE) | Root Mean Square Error (RMSE) | Predictive AUC | 95% Confidence Interval |
|---|---|---|---|---|
| K-Nearest Neighbors | 0.2032 | 0.7438 | 0.730 | 0.719-0.741 |
| Random Forest | 0.3944 | 1.4866 | 0.777 | 0.769-0.785 |
| Expectation-Maximization | Not reported | Not reported | Intermediate | Not reported |
| Multiple Imputation | Not reported | Not reported | Intermediate | Not reported |
| Decision Tree | Not reported | Not reported | Intermediate | Not reported |
| Simple Imputation | Not reported | Not reported | 0.713 | Not reported |
| Regression Imputation | Not reported | Not reported | 0.699 | Not reported |
| Clustering Imputation | Not reported | Not reported | 0.651 | Not reported |
| Complete Data (Benchmark) | N/A | N/A | 0.804 | 0.796-0.812 |
The experimental results demonstrate significant performance variation among methods. Machine learning approaches, particularly K-Nearest Neighbors and Random Forest, achieved superior performance on both imputation accuracy and downstream predictive tasks. KNN excelled in direct imputation accuracy, while Random Forest produced the best predictive model performance after imputation. Simple methods like mean substitution and regression imputation consistently underperformed, highlighting the limitations of simplistic approaches for complex clinical data [96].
Simple Imputation: Replaces missing values with a quantitative or qualitative attribute of the non-missing data. For continuous variables, this typically involves mean substitution; for categorical variables, mode substitution. While computationally simple, this method often produces poor results with complex dataset relationships [96].
Regression Imputation: Develops regression equations from complete data in the dataset, using these equations to predict and replace missing values. Performance depends heavily on correct model specification and may underestimate variance [96].
Expectation-Maximization: An iterative approach that estimates missing values based on complete data, then re-estimates parameters using both observed and imputed values. The process alternates between expectation and maximization steps until convergence [96].
Multiple Imputation: Generates several complete datasets by simulating each missing value multiple times to reflect uncertainty. Analyses are performed separately on each dataset, then combined for final inference. Considered a gold standard among statistical approaches [96].
K-Nearest Neighbors: Identifies k similar samples using distance metrics, then imputes missing values based on these neighbors. Uses measures like Euclidean distance and can capture complex patterns without parametric assumptions [96].
Random Forest: Constructs multiple decision trees through bootstrap sampling and random feature selection, then aggregates predictions across trees. Particularly effective for complex interactions in data [96].
Comparative Analysis of Feature Selection Methods
Feature selection addresses the "curse of dimensionality" by identifying the most informative features while removing irrelevant or redundant variables. This critical preprocessing step improves model generalization, interpretability, and computational efficiency, especially crucial for high-dimensional biological and clinical datasets.
Experimental Protocol: Evaluating Feature Selection Algorithms
A rigorous 2023 radiomics study systematically evaluated feature selection and classification algorithm combinations across ten clinical datasets. The experimental methodology provides a robust framework for comparative assessment [97]:
- Datasets: Ten independent radiomics datasets addressing various diagnostic questions, including COVID-19 pneumonia, sarcopenia, and various lesions across imaging modalities.
- Dataset Characteristics: Varied dimensions from 97-693 patients and 105-606 radiomics features per sample.
- Algorithm Combinations: Nine feature selection methods combined with fourteen classification algorithms, resulting in 126 unique combinations.
- Evaluation Framework: Three-fold dataset splitting stratified by diagnosis, with ten-fold cross-validation for hyperparameter tuning.
- Performance Metric: Area under the receiver operating characteristic curve, penalized by the absolute difference between test and train AUC to account for overfitting.
- Statistical Analysis: Multifactor ANOVA to quantify performance variability attributable to different factors.
This comprehensive design enabled evidence-based assessment of feature selection method performance across diverse clinical contexts.
Quantitative Performance Comparison of Feature Selection Methods
Table 2: Performance comparison of feature selection algorithms
| Feature Selection Method | Category | Performance Ranking | Key Characteristics |
|---|---|---|---|
| Joint Mutual Information Maximization (JMIM) | Information theory | Best overall | Captures feature interactions, minimizes redundancy |
| Joint Mutual Information (JMI) | Information theory | Best overall | Balances relevance and redundancy |
| Minimum-Redundancy-Maximum-Relevance (MRMR) | Information theory | High | Explicitly addresses feature redundancy |
| Random Forest Permutation Importance | Tree-based | High | Robust to nonlinear relationships |
| Random Forest Variable Importance | Tree-based | Intermediate | May select correlated features |
| Spearman Correlation Coefficient | Statistical | Intermediate | Captures monotonic relationships |
| Pearson Correlation Coefficient | Statistical | Intermediate | Limited to linear associations |
| Random Selection | Benchmark | Low | Non-informative baseline |
| No Selection | Benchmark | Low | Includes all features |
The investigation revealed that information-theoretic methods (JMIM, JMI, MRMR) consistently achieved superior performance across diverse datasets and classification algorithms. The choice of feature selection algorithm explained approximately 2% of total performance variance, while the classification algorithm selection accounted for 10%, and dataset characteristics explained 17% of variance. This indicates that while feature selection contributes meaningfully to performance, its impact is moderated by dataset-specific characteristics and classifier choice [97].
Filter Methods: Select features based on statistical measures of relationship with outcome variable, independent of classifier. Include correlation coefficients and information-theoretic measures. Computationally efficient but may ignore feature dependencies [98] [97].
Wrapper Methods: Evaluate feature subsets using model performance. Typically achieve better performance but are computationally intensive and risk overfitting [98].
Embedded Methods: Integrate feature selection within model training process. Include regularization techniques like LASSO and tree-based importance measures. Balance performance and computational efficiency [98].
Information-Theoretic Approaches: Quantify the information gain between features and outcome. Methods like JMI and JMIM effectively capture complex feature interactions while minimizing redundancy, making them particularly suitable for biological data with epistatic effects [98] [97].
Integrated Workflow for Addressing Data Quality Issues
Effective data quality management requires systematic integration of missing data handling and feature selection within the predictive modeling pipeline. The following workflow visualization illustrates this coordinated approach:
Diagram 1: Integrated workflow for handling data quality issues in predictive modeling
This workflow emphasizes the sequential yet interdependent nature of addressing data quality challenges. The selection of imputation methods should be informed by missing data patterns and mechanisms, while feature selection operates on the complete dataset to enhance model generalizability.
Table 3: Essential solutions for addressing data quality challenges
| Solution Category | Specific Methods/Tools | Primary Function | Applicable Context |
|---|---|---|---|
| Missing Data Imputation | K-Nearest Neighbors (KNN) | Missing value estimation using similar instances | Complex data patterns, non-linear relationships |
| Random Forest (RF) | Robust missing value imputation using ensemble trees | High-dimensional data, complex interactions | |
| Multiple Imputation by Chained Equations (MICE) | Generates multiple imputed datasets accounting for uncertainty | MAR data, statistical inference | |
| Expectation-Maximization (EM) | Maximum likelihood estimation via iterative algorithm | Normally distributed data, parametric approach | |
| Feature Selection | Joint Mutual Information Maximization (JMIM) | Selects features with high relevance and low redundancy | Biological data with feature interactions |
| Minimum-Redundancy-Maximum-Relevance (MRMR) | Balances feature relevance and inter-correlation | High-dimensional clinical datasets | |
| Random Forest Permutation Importance | Assesses feature importance through permutation | Non-linear relationships, model-specific selection | |
| LASSO Regularization | Embedded feature selection via L1 penalty | Linear models, automatic feature selection | |
| Validation Frameworks | Repeated Cross-Validation | Robust performance estimation while mitigating overfitting | Limited sample sizes, model development |
| External Validation | Assesses model generalizability on independent datasets | Clinical implementation, transportability assessment | |
| TRIPOD Guidelines | Reporting standards for predictive model studies | Transparent research reporting, methodological rigor |
This toolkit provides researchers with essential methodological approaches for constructing robust predictive models in the presence of data quality challenges. Selection should be guided by dataset characteristics, missing data mechanisms, and research objectives.
Implications for Predictive Model Validation
The choice of methods for addressing missing data and performing feature selection significantly impacts subsequent model validation processes and performance interpretation. Several key considerations emerge from comparative analyses:
First, improper missing data handling can introduce bias that persists through model development and becomes embedded in final predictions. The demonstrated superiority of machine learning imputation methods like KNN and Random Forest suggests these approaches better preserve dataset structure and relationships, leading to more valid predictive models [96].
Second, feature selection method choice influences both model performance and biological interpretability. Information-theoretic approaches that effectively handle feature redundancy (e.g., JMIM, JMI) provide dual benefits of enhanced predictive accuracy and more parsimonious feature sets potentially more relevant to underlying biological mechanisms [98] [97].
Third, the interaction between imputation, feature selection, and classifier algorithms necessitates comprehensive validation approaches. Studies indicate classifier choice explains approximately 10% of performance variance, highlighting the importance of algorithm selection and tuning after addressing data quality issues [97].
Finally, rigorous validation must account for the entire preprocessing pipeline, not merely the final modeling step. Internal validation through resampling methods and external validation on independent datasets remain essential for quantifying model performance and generalizability, particularly given the methodological choices involved in addressing data quality challenges [9].
Addressing data quality issues through appropriate missing data handling and feature selection methodologies forms the foundation for robust, clinically applicable predictive models in drug development and healthcare research. Empirical evidence demonstrates that machine learning approaches, particularly K-Nearest Neighbors and Random Forest for missing data imputation, and information-theoretic methods like Joint Mutual Information Maximization for feature selection, consistently outperform traditional statistical techniques across diverse clinical datasets.
The interdependence of methodological choices throughout the predictive modeling pipeline necessitates integrated validation approaches that account for the cumulative impact of data quality decisions on ultimate model performance. By adopting evidence-based practices for missing data handling and feature selection, researchers can enhance model accuracy, interpretability, and translational potential, ultimately advancing the development of reliable predictive tools for precision medicine and drug discovery.
Rigorous Validation Frameworks and Model Comparison
Designing Robust External Validation Studies
In the field of predictive model research, particularly within pharmaceutical development and clinical medicine, the creation of a prognostic statistical model is only the first step. For a model to achieve widespread clinical utility, it must demonstrate reliability beyond the initial development dataset. This process, known as external validation, assesses how well a prediction model performs in new populations, different clinical settings, or across geographical boundaries. External validation represents a critical bridge between theoretical model development and practical, real-world implementation, serving as a fundamental component of the model lifecycle before consideration in clinical decision-making or regulatory approval.
The importance of external validation has intensified with the rapid expansion of artificial intelligence and machine learning applications in healthcare. Without rigorous external validation, even models exhibiting outstanding performance in development samples may fail in broader practice due to issues like overfitting, selection bias, or population-specific characteristics that limit generalizability. This guide examines the methodological framework for designing robust external validation studies, using a contemporary case study from oncology drug safety to illustrate key principles and provide practical implementation protocols.
Theoretical Framework: Core Validation Concepts
Defining External Validation
External validation quantifies the predictive performance of a model in an independent dataset that was not used in any phase of the model development process. This independence is crucial, as it tests the model's transportability—its ability to maintain accuracy when applied to new patients who may differ from the original development cohort in demographics, clinical characteristics, treatment protocols, or healthcare systems. Unlike internal validation techniques (such as bootstrapping or cross-validation) which assess model stability within the development sample, external validation evaluates model generalizability across different clinical environments and populations [9].
Essential Performance Metrics
Robust external validation requires assessment across multiple complementary performance dimensions, each capturing different aspects of predictive accuracy:
Discrimination: The ability of a model to distinguish between patients who experience the outcome versus those who do not. This is typically measured using the Area Under the Receiver Operating Characteristic Curve (AUROC), which represents the probability that a randomly selected patient with the outcome has a higher predicted risk than a randomly selected patient without the outcome. AUROC values range from 0.5 (no better than chance) to 1.0 (perfect discrimination) [9].
Calibration: The agreement between predicted probabilities and observed outcomes. A well-calibrated model predicts risks that match the actual event rates across different risk strata. Calibration can be assessed at multiple levels: calibration-in-the-large (overall average predictions versus overall event rate), weak calibration (no systematic over- or under-prediction), and moderate calibration (agreement across risk groups) [9].
Clinical Utility: The net benefit of using the model for clinical decision-making across various probability thresholds, typically evaluated using Decision Curve Analysis (DCA). This approach incorporates the relative clinical consequences of false positives and false negatives, providing a clinically relevant assessment beyond purely statistical measures [99] [9].
Case Study: External Validation of Cisplatin-Associated AKI Prediction Models
Background and Study Objectives
Cisplatin remains a cornerstone chemotherapeutic agent for various solid tumors, but its clinical utility is limited by dose-dependent nephrotoxicity. Cisplatin-associated acute kidney injury (C-AKI) occurs in 20-30% of patients and is associated with treatment interruptions, poor prognosis, prolonged hospitalization, and increased healthcare costs [99]. Two clinical prediction models have been developed to stratify C-AKI risk: the Motwani model (2018) and the Gupta model (2024). While both were derived from U.S. populations, their performance in other populations, including Japanese patients, remained unknown.
A recent study conducted external validation of these models in a Japanese cohort, addressing several key questions: (1) How well do U.S.-derived models generalize to Japanese patients? (2) Which model demonstrates superior performance for different AKI severity definitions? (3) What methodological adjustments are necessary when applying these models in new populations? [99]
Comparative Model Characteristics
Table 1: Characteristics of Cisplatin-AKI Prediction Models
| Model Characteristic | Motwani et al. Model | Gupta et al. Model |
|---|---|---|
| AKI Definition | Serum creatinine ≥0.3 mg/dL increase within 14 days | Serum creatinine ≥2.0-fold increase or renal replacement therapy within 14 days |
| Predictors Included | Age, hypertension, cisplatin dose, serum albumin | Age, hypertension, diabetes, smoking, cisplatin dose, hemoglobin, white blood cell count, serum albumin, serum magnesium |
| Population Origin | U.S. development cohort | U.S. development cohort |
| Target Population | Patients receiving cisplatin chemotherapy | Patients receiving cisplatin chemotherapy |
Experimental Protocol and Methodology
Study Design and Setting
The validation study employed a retrospective cohort design using data from patients who received cisplatin at Iwate Medical University Hospital between April 2014 and December 2023. This temporal and geographical independence from the original development cohorts provided a rigorous test of transportability [99].
Participant Eligibility Criteria
The study implemented explicit inclusion and exclusion criteria to define the validation cohort:
- Inclusion: Adult patients (≥18 years) receiving cisplatin-based chemotherapy within the study period.
- Exclusion: (1) Age <18 years at cisplatin administration; (2) Cisplatin administration outside the study period or at another institution; (3) Treatment with daily or weekly cisplatin regimens (due to different nephrotoxicity profiles); (4) Missing baseline renal function or outcome data [99].
The final cohort included 1,684 patients, demonstrating the substantial sample sizes often required for adequately powered validation studies.
Data Collection and Management
Investigators extracted comprehensive data from electronic medical records:
- Patient characteristics: Age, sex, height, weight, smoking history
- Clinical data: Comorbidities (hypertension, diabetes), concomitant medications
- Treatment information: Cisplatin administration dates and doses
- Laboratory values: Serum creatinine, albumin, complete blood count, magnesium
Baseline laboratory values were defined as the most recent measurements within 30 days preceding cisplatin initiation. The study addressed missing data using regression-based imputation, acknowledging this as a potential limitation while recognizing that complete-case analysis would substantially reduce sample size and potentially introduce selection bias [99].
Outcome Definitions
The study evaluated both models against multiple outcome definitions to enhance clinical relevance:
- C-AKI: ≥0.3 mg/dL increase in serum creatinine OR ≥1.5-fold increase from baseline within 14 days of cisplatin exposure (aligning with KDIGO criteria)
- Severe C-AKI: ≥2.0-fold increase in serum creatinine OR initiation of renal replacement therapy (KDIGO stage ≥2) [99]
Statistical Validation Protocol
The validation methodology employed a comprehensive multi-dimensional approach:
Discrimination Assessment: Calculated AUROC values for each model against both C-AKI definitions, with statistical comparison using bootstrap methods.
Calibration Evaluation: Assessed agreement between predicted probabilities and observed outcomes using calibration plots and metrics (calibration-in-the-large and calibration slope).
Recalibration Procedure: Applied logistic recalibration to adapt the original models to the Japanese population when poor calibration was detected.
Clinical Utility Quantification: Performed decision curve analysis to estimate the net benefit of each model across clinically relevant risk thresholds [99].
All statistical analyses were conducted using R version 4.3.1, with transparency enhanced by publicly sharing analysis code (Table S2 in the original publication) [99].
Experimental Results and Performance Comparison
Table 2: External Validation Performance Metrics in Japanese Cohort
| Performance Measure | Motwani et al. Model | Gupta et al. Model | Statistical Comparison |
|---|---|---|---|
| Discrimination for C-AKI (AUROC) | 0.613 | 0.616 | p = 0.84 |
| Discrimination for Severe C-AKI (AUROC) | 0.594 | 0.674 | p = 0.02 |
| Initial Calibration | Poor | Poor | - |
| Calibration After Recalibration | Improved | Improved | - |
| Net Benefit for Severe C-AKI | Moderate | Highest clinical utility | - |
The validation revealed several critical findings. First, both models demonstrated similar discriminatory ability for the standard C-AKI definition, with nearly identical AUROCs around 0.615. However, for severe C-AKI (a clinically more consequential outcome), the Gupta model showed significantly better discrimination (AUROC 0.674 vs. 0.594, p=0.02). Second, both models exhibited poor calibration in their original forms, systematically over- or under-estimating risk in the Japanese population. Third, after logistic recalibration, both models showed improved fit, with the recalibrated Gupta model demonstrating the highest clinical utility for severe C-AKI prediction in decision curve analysis [99].
Methodological Framework for Validation Studies
Conceptual Workflow for External Validation
The diagram below illustrates the systematic workflow for designing and conducting robust external validation studies, derived from methodological principles and the case study application:
Essential Methodological Considerations
Cohort Design and Selection
The validation cohort should be representative of the target population for intended model use, with clear eligibility criteria mirroring clinical practice. Temporal validation (different time period) and geographical validation (different institutions or regions) provide stronger evidence of transportability than simple split-sample approaches. For the C-AKI validation, the Japanese cohort provided geographical and potentially ethnic diversity compared to the original U.S. development samples [99].
Sample Size Requirements
While formal sample size calculations for validation studies are complex, practical guidelines suggest a minimum of 100-200 events (outcomes) and 100-200 nonevents to precisely estimate performance metrics, particularly calibration. The C-AKI study with 1,684 patients provided adequate statistical power to detect clinically meaningful differences in performance [9].
Handling Missing Data
Missing data presents a universal challenge in validation studies. Approaches include complete-case analysis (which may introduce bias), single imputation, or multiple imputation. The C-AKI study used regression-based imputation as a pragmatic approach, though multiple imputation is generally preferred when computationally feasible [99].
Outcome Ascertainment
Outcome definitions should align as closely as possible with the original development study while maintaining clinical relevance. Using multiple outcome definitions (as in the C-AKI study) enhances insights into model performance across different clinical contexts.
Table 3: Essential Methodological Resources for External Validation Studies
| Resource Category | Specific Tool/Method | Function/Purpose | Implementation Example |
|---|---|---|---|
| Statistical Software | R Statistical Environment | Comprehensive data management, analysis, and visualization | Used for all analyses in C-AKI study [99] |
| Reporting Guidelines | TRIPOD/TRIPOD-AI Statement | Structured reporting of prediction model development and validation | Ensures transparent and complete methodology reporting [9] |
| Discrimination Metrics | Area Under ROC Curve (AUROC) | Quantifies model ability to distinguish between outcome groups | Bootstrap method for comparing AUROCs between models [99] |
| Calibration Assessment | Calibration Plots and Slopes | Evaluates agreement between predicted and observed risks | Identified miscalibration in original models [99] |
| Clinical Utility Analysis | Decision Curve Analysis (DCA) | Estimates net clinical benefit across risk thresholds | Demonstrated superior utility of recalibrated Gupta model [99] |
| Model Updating Methods | Logistic Recalibration | Adjusts model intercept and/or slopes for new population | Improved model fit in Japanese cohort [99] |
Implications for Model Implementation and Clinical Practice
The C-AKI validation case study offers several crucial insights for researchers and clinicians considering implementation of prediction models:
First, direct transportability of models across populations cannot be assumed. The significant miscalibration of both original models in the Japanese cohort underscores the necessity of local validation before clinical implementation. This has particular relevance for drug development professionals working in global clinical trials or post-marketing safety surveillance, where prediction models may be applied across diverse ethnic and healthcare systems.
Second, model performance varies by outcome severity. The superior discrimination of the Gupta model for severe C-AKI (versus similar performance for any C-AKI) highlights how clinical context and outcome definitions influence model selection. For safety applications in drug development, models predicting severe outcomes may have greater clinical value despite potentially lower overall incidence.
Third, recalibration represents a pragmatic approach to model localization. Rather than developing entirely new models—a resource-intensive process—recalibrating existing models using local data can efficiently enhance performance while preserving the original predictor structure and clinical reasoning.
Finally, multi-dimensional validation is essential. Reliance on discrimination alone provides an incomplete picture; comprehensive evaluation requires complementary assessment of calibration and clinical utility to inform implementation decisions. This holistic approach ensures that models not only statistically discriminate but also provide clinically actionable risk estimates that improve decision-making.
These principles extend beyond the specific case of C-AKI prediction to the broader domain of predictive model validation in pharmaceutical research, including models for drug safety, treatment response, disease progression, and healthcare utilization. As predictive models increasingly inform critical decisions in drug development and clinical practice, robust external validation represents an indispensable component of the translational pathway from statistical innovation to clinical impact.
Benchmarking Against Established Models and Clinical Standards
For researchers and drug development professionals, the integration of artificial intelligence (AI) and predictive modeling into clinical research represents a paradigm shift with the potential to accelerate discovery and improve patient outcomes. However, this promise is contingent upon rigorous statistical validation that ensures models are not only accurate but also reliable, generalizable, and clinically relevant. The process of benchmarking against established models and clinical standards is foundational to this validation, providing an objective framework for assessing predictive performance and translational potential. This guide synthesizes current benchmarking methodologies and performance data to facilitate evidence-based evaluation of clinical predictive models, emphasizing the statistical rigor required for research applications.
Performance Benchmarking: Comparative Analysis of Leading Models
Independent, head-to-head comparisons on standardized clinical tasks are crucial for assessing the relative strengths and weaknesses of different models. The table below summarizes the performance of various large language models (LLMs) on a comprehensive examination of clinical knowledge, based on a 2025 benchmark study involving 1,965 multiple-choice questions across five medical specialties [100].
Table 1: Clinical Knowledge and Confidence Benchmarking of Select LLMs
| Model | Overall Accuracy (%) | Mean Confidence (Correct Answers) | Mean Confidence (Incorrect Answers) | Confidence Gap (Correct - Incorrect) |
|---|---|---|---|---|
| Claude 3.5 Sonnet | 74.0 | 70.5% | 67.4% | 3.1% |
| GPT-4o | 73.8 | 64.4% | 59.0% | 5.4% |
| Claude 3 Opus | 71.7 | 68.9% | 67.3% | 1.6% |
| GPT-4 | 66.0 | 84.5% | 83.3% | 1.2% |
| Llama-3-70B | 63.4 | 59.5% | 53.6% | 5.9% |
| Gemini | 59.1 | 87.2% | 85.5% | 1.7% |
| Mixtral-8x7B | 50.6 | 85.5% | 83.0% | 2.5% |
| GPT-3.5 | 49.0 | 81.6% | 82.9% | -1.3% |
| Qwen2-7B | 46.0 | 74.4% | 76.4% | -2.0% |
A critical finding from this study is the inverse correlation (r = -0.40; p=.001) between model accuracy and mean confidence for correct answers, revealing that lower-performing models often exhibit paradoxically higher confidence in their responses [100]. This miscalibration is a significant risk for clinical deployment, as it can erode user trust or lead to over-reliance on incorrect information. For research purposes, benchmarking must therefore extend beyond simple accuracy to include calibration metrics, as a model's ability to accurately quantify its own uncertainty is vital for risk-aware decision-making in drug development.
Established Experimental Protocols for Model Validation
Adhering to standardized experimental protocols is essential for producing reproducible and comparable benchmark results. The following methodologies are commonly employed in rigorous evaluations.
Clinical Knowledge and Reasoning Assessment
Objective: To evaluate a model's mastery of clinical knowledge and its ability to reason through complex, specialty-specific scenarios [100].
- Dataset: Utilize a standardized set of clinical questions, such as 1,965 multiple-choice questions derived from official licensing examinations for internal medicine, obstetrics and gynecology, psychiatry, pediatrics, and general surgery.
- Rephrasing: To enhance benchmark reliability, each original question can be rephrised multiple times using an API, modifying only the writing style while preserving all clinical details, medical terms, and answer choices.
- Physician Review: A random sample (e.g., 20%) of the rephrased questions should be reviewed by board-certified physicians to confirm clinical meaning and terminology remain unchanged.
- Model Prompting: Models are prompted with a structured query to return both an answer and a confidence score (0-100%) for each multiple-choice option in a structured JSON format.
- Statistical Analysis: Calculate overall accuracy and mean confidence scores. Analyze the correlation between accuracy and confidence, and compare confidence levels for correct versus incorrect answers using two-sample, two-tailed t-tests.
The DRAGON Benchmark for Clinical NLP
Objective: To assess the capability of Natural Language Processing (NLP) models and LLMs in automating the annotation and curation of data from clinical reports, a key task in research dataset generation [101].
- Dataset: The benchmark comprises 28,824 annotated clinical reports (e.g., radiology, pathology) from multiple centers, sequestered on a secure platform to ensure patient privacy.
- Task Diversity: It includes 28 tasks covering classification, regression, and named entity recognition (NER), such as identifying disease presence, extracting measurements, and recognizing medical terminology.
- Execution: Models are evaluated on the Grand Challenge platform, where they process the clinical reports from the test set and generate predictions for the specific tasks without direct access to the ground-truth labels.
- Metrics: Performance is measured using clinically relevant metrics including Area Under the Receiver Operating Characteristic Curve (AUROC) for binary classification, Linearly Weighted Kappa for multi-class classification, and Robust Symmetric Mean Absolute Percentage Error (RSMAPES) for regression tasks [101].
Workflow Diagram for Predictive Model Validation
The following diagram illustrates the core statistical validation workflow for clinical predictive models, integrating key concepts from internal and external validation [9] [102].
Diagram 1: Clinical Model Validation Workflow
This workflow underscores that model development is an iterative process. After initial development on a training set, internal validation techniques like bootstrapping or cross-validation are used to estimate and correct for optimism in the model's performance [9] [102]. This is a critical step for assessing how the model might perform on new data from the same underlying population. However, true generalizability is only established through external validation—evaluating the model's performance on a completely independent dataset, often from a different institution or population [9]. The final, and often overlooked, step is a prospective impact study to determine if using the model actually improves clinical processes or patient outcomes, bridging the "AI chasm" between statistical accuracy and real-world efficacy [9].
Essential Research Reagents and Computational Tools
Successful benchmarking and model validation require a suite of methodological tools and frameworks. The following table details key resources for researchers.
Table 2: Research Reagent Solutions for Model Validation
| Tool / Framework | Primary Function | Relevance to Validation |
|---|---|---|
| TRIPOD-AI Checklist | Reporting Guideline | Ensures transparent and complete reporting of predictive model studies, improving reproducibility and critical appraisal [9]. |
| Resampling Methods | Internal Validation | Techniques like k-fold cross-validation and bootstrapping estimate model optimism and performance on unseen data from the same distribution [9] [102] [10]. |
| Discrimination Metrics | Performance Evaluation | Area Under the ROC Curve (AUC) measures the model's ability to distinguish between classes (e.g., disease vs. no disease) [9]. |
| Calibration Metrics | Performance Evaluation | Calibration Plots and Brier Score assess the agreement between predicted probabilities and observed event rates, crucial for risk stratification [9]. |
| Decision Curve Analysis | Clinical Utility | Net Benefit quantifies the clinical value of a model across different decision thresholds, integrating calibration and discrimination [9]. |
| Public Benchmarks (e.g., DRAGON) | Standardized Evaluation | Provides objective, sequestered datasets and tasks for comparing NLP algorithm performance on clinically relevant information extraction [101]. |
Benchmarking against established models and clinical standards is not an academic exercise; it is a fundamental component of responsible research and development. The data and protocols outlined in this guide provide a roadmap for moving beyond isolated accuracy metrics toward a holistic understanding of a model's performance, limitations, and readiness for translational research. For drug development professionals and clinical researchers, this rigorous approach to validation is indispensable. It ensures that the predictive models integrated into the research pipeline are not only statistically sound but also clinically plausible, reliably calibrated, and ultimately capable of generating the robust evidence required to advance patient care. The future of AI in healthcare depends on this foundation of rigorous, standardized, and transparent evaluation.
Comparative Analysis of Traditional Statistical vs. Machine Learning Models
The evolution of predictive modeling has been marked by a dynamic tension between traditional statistical methods and modern machine learning (ML) algorithms. Within research domains such as drug development, where predictive accuracy can significantly impact therapeutic outcomes, selecting the appropriate modeling approach becomes paramount. Statistical models have long served as the foundation for inference in scientific research, providing interpretable relationships between variables and outcomes [103]. In contrast, machine learning offers a powerful framework for discovering complex, non-linear patterns in high-dimensional data, often at the cost of interpretability [104]. This guide provides an objective comparison of these approaches, focusing on their performance characteristics, methodological considerations, and applicability within the context of statistical validation for predictive model research. Understanding the strengths and limitations of each paradigm enables researchers to make informed decisions tailored to their specific predictive modeling goals, whether they prioritize explanatory power or predictive accuracy.
Fundamental Differences Between Statistical and Machine Learning Approaches
The distinction between statistical modeling and machine learning extends beyond their technical implementations to their foundational philosophies and primary objectives. Statistical modeling traditionally adopts a hypothesis-driven approach, beginning with a predefined model that describes the relationship between variables based on underlying theory [105]. The focus lies in understanding data-generating processes, quantifying uncertainty through confidence intervals and p-values, and testing explicit hypotheses about population parameters [103]. Statistical models often maintain relative simplicity to ensure interpretability, with parameters that frequently correspond to tangible, real-world relationships.
In contrast, machine learning embraces a data-driven philosophy, prioritizing predictive accuracy over interpretability [105]. Rather than starting with a predefined model structure, ML algorithms learn patterns directly from data, often capturing complex, non-linear relationships that might elude traditional statistical methods [104]. This approach typically involves splitting data into training and testing sets to validate model performance on unseen data, emphasizing generalization capability [103]. The machine learning workflow often employs more complex model structures, sometimes described as "black boxes" due to the difficulty in interpreting their inner workings [104].
As succinctly summarized in Nature Methods, "Statistics draws population inferences from a sample, and machine learning finds generalizable predictive patterns" [106]. This fundamental distinction in purpose profoundly influences their application across research domains, with statistical methods dominating traditional scientific inference and machine learning excelling in prediction tasks with complex, high-dimensional data.
Performance Comparison Across Domains
Quantitative Performance Metrics
Empirical comparisons across diverse research domains reveal distinct performance patterns between traditional statistical and machine learning approaches. The following table summarizes key findings from recent comparative studies:
Table 1: Performance Comparison of Statistical vs. Machine Learning Models Across Domains
| Domain | Statistical Models | Machine Learning Models | Performance Outcome | Citation |
|---|---|---|---|---|
| Building Performance | Linear Regression, Logistic Regression | Random Forest, Gradient Boosting | ML outperformed statistical methods in both classification and regression metrics | [104] |
| Finance & Stock Prediction | Linear Regression | Random Forests, Decision Trees, LSTM | Advanced ML techniques substantially outperformed traditional models on accuracy and reliability | [107] |
| Alzheimer's Progression | Cox PH, Weibull, Elastic Net Cox | Random Survival Forests, Gradient Boosting | RSF achieved superior predictive performance (C-index: 0.878) vs. Cox PH | [108] |
| World Happiness Classification | Logistic Regression | Decision Tree, SVM, Random Forest, ANN, XGBoost | Multiple algorithms (LR, DT, SVM, ANN) achieved equal highest accuracy (86.2%) | [109] |
| Clinical Prediction | Logistic Regression | Various ML algorithms | No significant performance benefit of ML over logistic regression in clinical prediction | [104] |
Domain-Specific Performance Analysis
The comparative performance between statistical and machine learning approaches varies significantly across application domains, reflecting the inherent characteristics of different data types and prediction tasks. In building performance analytics, a systematic review of 56 journal articles found that machine learning algorithms consistently outperformed traditional statistical methods in both classification and regression metrics [104]. This performance advantage is particularly pronounced in complex systems with non-linear relationships between variables, where ML's ability to capture intricate patterns without predefined structural assumptions provides substantial benefits.
In healthcare and medical research, results appear more nuanced. For predicting progression from Mild Cognitive Impairment (MCI) to Alzheimer's disease, Random Survival Forests (RSF) demonstrated statistically significant superiority (p-value < 0.001) over traditional survival models, achieving a C-index of 0.878 compared to conventional Cox proportional hazards models [108]. This suggests that for complex, multifactorial disease progression with time-to-event outcomes, ML survival methods can leverage non-linear relationships effectively. However, broader analyses of clinical prediction models have found no significant improvement when using machine learning compared to logistic regression in many clinical prediction studies [104], highlighting how well-specified statistical models remain competitive for many standard medical prediction tasks.
The financial sector has witnessed a substantial transformation through machine learning incorporation. Comparative studies of stock price prediction reveal that advanced ML techniques like LSTMs and random forests substantially outperform traditional linear regression models in both accuracy and reliability [107]. This performance advantage is particularly evident in volatile market conditions where non-linear patterns and complex temporal dependencies emerge.
For classification tasks with structured data, such as classifying countries based on happiness indices, multiple approaches including both logistic regression and machine learning algorithms like SVM and neural networks can achieve comparably high accuracy (86.2%) [109]. This suggests that for well-defined classification problems with clear feature-target relationships, the model selection decision may depend more on interpretability needs and computational constraints than raw predictive performance.
Experimental Protocols and Methodologies
Standardized Benchmarking Framework
To ensure fair comparisons between statistical and machine learning approaches, researchers have developed standardized benchmarking frameworks. The "Bahari" framework, implemented in Python with a spreadsheet interface, provides a systematic approach for comparing traditional statistical methods and machine learning algorithms on identical datasets [104]. This framework employs multiple validation methodologies to ensure robust performance assessment:
Table 2: Key Components of Experimental Validation Protocols
| Component | Statistical Approach | Machine Learning Approach | Purpose |
|---|---|---|---|
| Data Splitting | Single dataset for model fitting | Training/validation/test splits | Evaluate generalization performance |
| Model Assessment | Confidence intervals, significance tests, goodness-of-fit measures | Cross-validation, accuracy metrics, precision, recall, F1-score | Quantify model performance and uncertainty |
| Feature Handling | Manual selection based on domain knowledge | Automated feature selection, regularization | Manage model complexity and prevent overfitting |
| Validation Metrics | R-squared, p-values, AIC, BIC | C-index, Brier Score, calibration plots | Assess predictive accuracy and model calibration |
Domain-Specific Experimental Designs
In medical survival analysis for Alzheimer's progression prediction, researchers employed a comprehensive methodology using data from the Alzheimer's Disease Neuroimaging Initiative (ADNI) dataset [108]. The experimental protocol included:
- Study Population: 902 MCI individuals with at least one follow-up visit from the ADNIMERGE dataset spanning 2005-2023
- Feature Selection: Initial 61 features reduced to 14 key predictors using Lasso Cox model to eliminate variables with little explanatory power
- Data Imputation: Nonparametric missForest method using random forest predictions for handling missing data
- Model Training: Five survival approaches compared: CoxPH, Weibull, CoxEN, GBSA, and RSF
- Evaluation Metrics: Concordance index (C-index) and Integrated Brier Score (IBS) with statistical significance testing
For financial forecasting comparisons, studies typically employ historical stock price data with rigorous temporal splitting to avoid look-ahead bias [107]. The experimental workflow generally includes:
- Data Partitioning: Chronological split into training, validation, and test sets to simulate real-world forecasting conditions
- Benchmark Models: Linear regression as statistical baseline compared against multiple ML algorithms
- Evaluation Framework: Accuracy metrics tailored to financial applications, including risk-adjusted returns and directional accuracy
In building performance analytics, researchers have adopted a systematic review methodology analyzing studies that applied both approaches on the same datasets [104]. This meta-analytic approach enables:
- Cross-Study Comparison: Qualitative and quantitative synthesis of results from multiple independent studies
- Domain Generalization: Assessment of whether performance results can be generalized across different building performance applications
- Bias Mitigation: Identification of potential confounding factors and study quality assessment
Research Reagent Solutions: Essential Materials for Predictive Modeling
Implementing robust comparative analyses between statistical and machine learning approaches requires specific computational tools and methodological resources. The following table catalogues essential "research reagents" for conducting such studies:
Table 3: Essential Research Reagents for Predictive Modeling Comparisons
| Reagent Category | Specific Tools/Solutions | Function/Purpose | Examples from Literature |
|---|---|---|---|
| Computational Frameworks | Python, R, MATLAB | Implementation environment for models and analyses | Bahari framework (Python-based) [104] |
| Statistical Modeling Packages | statsmodels (Python), survival (R) | Implementation of traditional statistical models | CoxPH, Weibull regression [108] |
| Machine Learning Libraries | scikit-learn, XGBoost, TensorFlow | ML algorithm implementation | Random Forests, GBSA, ANN [108] [109] |
| Validation Methodologies | Cross-validation, bootstrap resampling | Performance assessment and uncertainty quantification | C-index, IBS for survival models [108] |
| Data Imputation Tools | missForest, MICE | Handling missing data in predictive modeling | missForest for dementia datasets [108] |
| Interpretation Frameworks | SHAP, LIME | Model interpretation and feature importance analysis | SHAP for Random Survival Forests [108] |
Visualization of Model Selection Workflow
Selecting between statistical and machine learning approaches requires careful consideration of multiple factors. The following workflow diagram outlines a systematic decision process based on research requirements and data characteristics:
Model Selection Workflow Diagram: This decision framework illustrates the key considerations when choosing between statistical and machine learning approaches, emphasizing data characteristics, interpretability needs, and domain-specific constraints.
The comparative analysis between traditional statistical methods and machine learning approaches reveals a nuanced landscape where neither approach universally dominates. Machine learning algorithms generally demonstrate superior predictive accuracy for complex, high-dimensional problems with non-linear relationships, particularly in domains like building performance, financial forecasting, and complex disease progression modeling [104] [107] [108]. Conversely, traditional statistical methods maintain advantages in interpretability, theoretical grounding, and performance with smaller datasets or when explicit inference about variable relationships is required [103] [105].
The choice between these approaches should be guided by specific research objectives, data characteristics, and interpretability requirements rather than assumed superiority of either paradigm. For drug development professionals and researchers, this evidence-based comparison provides a framework for selecting appropriate modeling techniques based on empirical performance rather than methodological trends. As predictive modeling continues to evolve, the integration of statistical rigor with machine learning flexibility represents the most promising path forward for advancing predictive validity across scientific domains.
Assessing Clinical Usefulness and Impact on Decision-Making
Clinical prediction models are computational tools that estimate the probability of a specific health condition being present (diagnostic) or of a particular health outcome occurring in the future (prognostic). By integrating multiple predictors simultaneously, these models provide individualized risk estimates that support clinical decision-making, offering superior predictive accuracy compared to simpler risk classification systems or single prognostic factors. [110]
The assessment of a model's clinical usefulness extends beyond its statistical performance to its tangible impact on healthcare processes and patient outcomes. This evaluation is framed within the broader thesis on statistical validation, which emphasizes that rigorous validation is not merely a technical necessity but the cornerstone for determining whether a model is reliable and effective enough to be integrated into real-world clinical workflows. Key considerations for clinical implementation include the model's ability to improve decision-making transparency, reduce cognitive bias, and ultimately lead to more personalized and effective patient care. [111] [110]
Comparative Analysis of Modeling Approaches
Different modeling methodologies offer distinct advantages and challenges in a clinical context. The table below summarizes the core characteristics, validation requirements, and clinical usefulness of common approaches.
Table 1: Comparison of Clinical Prediction Modeling Approaches
| Modeling Approach | Key Characteristics | Primary Clinical Use Case | Validation & Data Considerations |
|---|---|---|---|
| Traditional Regression Models (e.g., Logistic, Cox) [110] | Provides interpretable, parsimonious models with coefficients for each predictor. | Developing prognostic tools for cancer survival or diagnostic models for disease presence. | Requires careful handling of proportional hazards (Cox) and predictor linearity. Sample size must be sufficient to avoid overfitting. [110] |
| Machine Learning (ML) Models (e.g., Random Forests, Neural Networks) [110] | Handles complex, non-linear relationships and high-dimensional data (e.g., genomics, medical imaging). | Identifying patient subgroups with differential treatment responses; analyzing complex multimodal data. [112] | High risk of overfitting without rigorous validation; requires large sample sizes. "Black box" nature can limit interpretability and clinical trust. [110] |
| Causal Machine Learning (CML) [112] | Aims to estimate cause-effect relationships from observational data using methods like doubly robust estimation. | Estimating real-world treatment effects; creating external control arms for clinical trials. | Requires explicit causal assumptions and advanced methods to mitigate confounding inherent in real-world data. [112] |
Performance and Validation Metrics
A model's journey from development to implementation hinges on a multi-faceted evaluation of its performance, which must assess both its statistical soundness and its potential for real-world impact.
Table 2: Key Metrics for Evaluating Clinical Prediction Models
| Evaluation Dimension | Key Metrics | Interpretation and Impact on Clinical Usefulness |
|---|---|---|
| Discrimination | C-statistic (Area Under the ROC Curve) | Measures how well the model separates patients with and without the outcome. A higher value indicates better predictive accuracy. [110] |
| Calibration | Calibration-in-the-large, Calibration slope | Assesses the agreement between predicted probabilities and observed outcomes. Good calibration is crucial for risk-based clinical decision-making. [110] |
| Clinical Utility | Net Benefit (from Decision Curve Analysis) | Quantifies the clinical value of using the model by balancing true positives and false positives, factoring in the relative harm of unnecessary interventions versus missed diagnoses. [110] |
Experimental Protocols for Model Validation
Robust validation is critical for assessing the real-world performance and stability of a clinical prediction model. The following protocols detail standard methodologies.
Protocol for Internal Validation via Bootstrapping
Bootstrapping is a robust internal validation technique used to estimate a model's likely performance on new data from the same underlying population and correct for overfitting. [110]
- Sampling: Generate a large number (e.g., 1000) of bootstrap samples by randomly selecting observations from the original development dataset with replacement. Each sample will be the same size as the original dataset.
- Model Development: Develop a model for each bootstrap sample using the exact same modeling procedure (e.g., variable selection, hyperparameter tuning).
- Performance Testing: Test the performance of each bootstrap-derived model on the original dataset.
- Calculate Optimism: For each bootstrap sample, calculate the difference between the performance on the bootstrap sample (optimistic) and the performance on the original dataset (closer to truth). This difference is the "optimism".
- Adjust Performance: Average all the optimism estimates and subtract this value from the apparent performance of the model developed on the original dataset to obtain an optimism-corrected performance estimate.
Protocol for External Validation
External validation is the strongest test of a model's generalizability and is essential before clinical implementation. [110]
- Data Acquisition: Obtain a completely new dataset, collected from a different location, time period, or population than the model development data.
- Predictor Application: Apply the exact same model (i.e., the original regression formula or saved ML algorithm) to this new dataset to generate predictions for each patient.
- Performance Assessment: Calculate the model's discrimination, calibration, and clinical utility metrics (as in Table 2) on this new dataset without any model retraining or updating.
- Interpretation: A model that maintains good performance upon external validation is considered transportable and is a stronger candidate for clinical use. Poor performance indicates the model may be overfitted or not generalizable.
Protocol for Causal Model Evaluation via Trial Emulation
For CML models aiming to estimate treatment effects from real-world data (RWD), a key validation method is emulating the results of a randomized controlled trial (RCT). [112]
- Target Trial Definition: Precisely define the protocol of the target RCT you wish to emulate, including eligibility criteria, treatment strategies, outcomes, and follow-up.
- Data Curation: Apply the eligibility criteria to the RWD (e.g., electronic health records, registries) to create a study cohort.
- Confounding Adjustment: Use advanced CML methods to control for confounding. For example, create a "digital twin" for each patient using prognostic matching, which models the outcome based on a large set of baseline covariates. [112]
- Effect Estimation: Compare outcomes between the treated and untreated groups after adjusting for residual confounding through techniques like propensity score matching or weighting within the prognostically matched sets.
- Validation Benchmarking: Compare the estimated treatment effect from the CML analysis on RWD with the results from the actual, published RCT. Close agreement between the two provides strong evidence for the validity of the CML approach. [112]
Workflow Visualization
The following diagram illustrates the key stages in the development and validation of a clinically useful prediction model, highlighting the iterative nature of the process and the critical role of validation.
Figure 1: Clinical Prediction Model Workflow
The Scientist's Toolkit: Research Reagent Solutions
The following table details key resources and methodologies essential for conducting rigorous development and validation of clinical prediction models.
Table 3: Essential Reagents and Resources for Predictive Model Research
| Item / Solution | Function / Purpose | Application in Validation |
|---|---|---|
| TRIPOD+AI Reporting Guideline [110] | A checklist for transparent reporting of multivariable prediction models that use AI. | Ensures all critical aspects of model development and validation are completely documented, enabling reproducibility and critical appraisal. |
| Real-World Data (RWD) Sources (e.g., EHRs, Claims Data, Patient Registries) [112] | Provides large-scale, longitudinal data on patient journeys, treatment, and outcomes outside of controlled trials. | Used for external validation of existing models and for developing/training new models (e.g., CML) where RCTs are infeasible. |
| Causal Machine Learning (CML) Algorithms (e.g., Doubly Robust Estimators, Targeted Maximum Likelihood Estimation) [112] | Advanced statistical methods designed to estimate causal treatment effects from observational data by mitigating confounding. | Core analytical tool for generating robust real-world evidence from RWD, such as estimating the effect of a drug in a specific patient subgroup. [112] |
| Statistical Software & Platforms (e.g., R, Python with scikit-learn, Azure Machine Learning) | Provides the computational environment and libraries for data preprocessing, model building, and validation. | Essential for implementing all validation techniques, from basic bootstrapping in R to deploying deep learning models on cloud platforms like Azure. |
| Digital Health Technologies (DHTs) (e.g., Wearables, Mobile Apps) [113] | Collects dense, real-time physiological and behavioral data from patients in their natural environment. | Serves as a source of novel, high-frequency predictors for model development and enables continuous monitoring of outcomes post-deployment. |
The clinical usefulness of a prediction model is determined not by its complexity but by the rigor of its validation and the demonstrable improvement it offers over current decision-making processes. A model's journey from concept to clinic depends on a structured pathway that prioritizes methodological soundness, transparent reporting, and robust evaluation across multiple datasets and settings. Frameworks like TRIPOD+AI are critical for ensuring this transparency. [110] Furthermore, the emergence of Causal Machine Learning applied to Real-World Data offers a powerful, complementary approach to traditional RCTs for generating evidence on treatment effects in diverse patient populations. [112] Ultimately, for a model to truly impact decision-making, its integration into clinical workflows must be planned from the outset, with ongoing monitoring to ensure its performance and utility are maintained over time.
Novel Approaches for Estimating External Performance with Limited Data
Estimating how a predictive model will perform on external data sources is a critical step in clinical prediction model development. Traditional external validation requires full access to patient-level data from external sites, which often presents significant practical barriers including data privacy concerns, regulatory hurdles, and resource constraints. Recent methodological advances have introduced novel approaches that can estimate external model performance using only summary statistics from target populations, dramatically reducing the data sharing burden. These approaches are particularly valuable in healthcare settings where data harmonization across institutions is challenging, yet understanding model transportability is essential for safe clinical implementation.
The importance of robust external validation has been highlighted by well-documented cases of performance deterioration when models are applied to new populations. For instance, the widely implemented Epic Sepsis Model demonstrated significant performance degradation when applied to external datasets, underscoring the limitations of internal validation alone [114]. Similarly, various stroke risk scores have shown inconsistent performance across different populations of atrial fibrillation patients [114]. These examples illustrate the critical need for methods that can reliably estimate how models will generalize before actual deployment.
Comparative Analysis of Validation Methods
Methodological Approaches
Table 1: Comparison of Validation Techniques for Predictive Models
| Method Type | Data Requirements | Key Advantages | Limitations | Ideal Use Cases |
|---|---|---|---|---|
| Internal Validation | Single dataset, resampling | Controls overfitting; Computationally efficient | Does not assess generalizability to new populations | Model development and feature selection |
| Traditional External Validation | Full patient-level data from external sources | Direct performance assessment in target setting; Gold standard | Resource-intensive; Regulatory and privacy challenges | Final validation before implementation when data sharing is feasible |
| Summary Statistic-Based Estimation | External summary statistics only | Privacy-preserving; Resource-efficient; Enables rapid iteration | Accuracy depends on relevance of statistics; May fail if characteristics cannot be matched | Early-stage transportability assessment; Multi-site collaboration planning |
| Internal-External Cross-Validation | Multiple similar datasets from different sources | Assesses performance heterogeneity; More robust than single external validation | Requires access to multiple external datasets | Understanding geographic or temporal performance variation |
Performance Metrics Comparison
Table 2: Key Performance Metrics for Model Validation
| Metric Category | Specific Metrics | Interpretation | Methodological Considerations |
|---|---|---|---|
| Discrimination | Area Under ROC Curve (AUC) | Ability to separate events from non-events; 0.5=random, 1.0=perfect | Most commonly reported; Insensitive to calibration |
| Calibration | Calibration-in-the-large, Calibration slope | Agreement between predicted and observed risks | "Achilles' heel" of prediction models; Critical for clinical utility |
| Overall Accuracy | Brier score, Scaled Brier score | Overall prediction accuracy considering both discrimination and calibration | Proper scoring rule; Sensitive to both discrimination and calibration |
| Clinical Utility | Net Benefit, Decision Curve Analysis | Clinical value considering tradeoffs between benefits and harms | Incorporates clinical consequences; Essential for implementation decisions |
Core Methodology and Workflow
The summary statistic-based estimation method represents a significant innovation in model validation methodology. This approach seeks weights that, when applied to the internal cohort, induce weighted statistics that closely match the external summary statistics [114]. Once appropriate weights are identified, performance metrics are computed using the labels and model predictions from the weighted internal units, providing estimates of how the model would perform on the external population.
The external statistics required for this method may include task-specific characteristics that stratify the target population by outcome value or more general population descriptors. These statistics can be specifically extracted for the validation purpose or obtained from previously published characterization studies and reports from national agencies [114]. This flexibility makes the method particularly valuable for rapid assessment of model transportability across diverse settings.
Experimental Protocol and Benchmarking
A comprehensive benchmark study evaluated this method using five large heterogeneous US data sources, where each dataset sequentially played the role of internal source while the remaining four served as external validations [114]. The study defined a target cohort of patients with pharmaceutically-treated depression and developed models predicting various outcomes including diarrhea, fracture, gastrointestinal hemorrhage, insomnia, and seizure.
The benchmarking protocol followed these key steps:
Model Development: For each internal data source, researchers trained prediction models using various algorithms including logistic regression and XGBoost with different feature set sizes.
Statistic Extraction: From each external data source, researchers extracted limited population-level statistics characterizing the target population.
Performance Estimation: The weighting algorithm was applied to estimate model performance on each external source using only the summary statistics.
Validation: Actual model performance was computed by testing models on the full external datasets, enabling direct comparison with estimated performance.
This rigorous evaluation demonstrated that the method produced accurate estimations across all key metrics, with 95th error percentiles of 0.03 for AUC, 0.08 for calibration-in-the-large, 0.0002 for Brier score, and 0.07 for scaled Brier score [114]. The estimation errors were substantially smaller than the actual differences between internal and external performance, confirming the method's utility for detecting performance deterioration during transport.
Performance Results and Methodological Considerations
Quantitative Performance Assessment
Table 3: Benchmark Results of Estimation Method Accuracy
| Performance Metric | 95th Error Percentile | Median Estimation Error (IQR) | Median Actual Internal-External Difference (IQR) |
|---|---|---|---|
| AUROC (Discrimination) | 0.03 | 0.011 (0.005-0.017) | 0.027 (0.013-0.055) |
| Calibration-in-the-large | 0.08 | 0.013 (0.003-0.050) | 0.329 (0.167-0.836) |
| Brier Score | 0.0002 | 3.2×10⁻⁵ (1.3×10⁻⁵-8.3×10⁻⁵) | 0.012 (0.0042-0.018) |
| Scaled Brier Score | 0.07 | 0.008 (0.001-0.022) | 0.308 (0.167-0.440) |
The results demonstrate that the estimation method provides substantially more accurate assessment of external performance than simply assuming performance will match internal validation results. For all metrics, the estimation errors were an order of magnitude smaller than the actual differences between internal and external performance [114]. This precision makes the method particularly valuable for identifying models that may appear promising during development but would deteriorate significantly in real-world settings.
Critical Implementation Factors
Feature Selection Strategy
The success of the weighting algorithm depends critically on the set of features used for matching internal and external statistics. Benchmark testing revealed that using feature sets aligned with the model's important predictors yielded the most accurate results [114]. Specifically:
- Model-Specific Features: Using features with substantial importance in the prediction model (e.g., coefficients ≥0.1 in linear models) produced optimal performance.
- Avoid Unrelated Features: Including features with low predictive importance or unrelated to the model decreased estimation accuracy and sometimes prevented algorithm convergence.
- Balance Comprehensiveness and Feasibility: While more features potentially provide better approximation of the joint distribution, excessively large feature sets make finding appropriate weights more challenging.
Sample Size Considerations
The method's performance is influenced by both internal and external sample sizes, though the impact of internal sample size is more pronounced [114]. Experimental results demonstrated:
- Internal Sample Size: Samples below 1,000 units frequently led to algorithm convergence failures. Reliability improved substantially with larger internal cohorts, with stable performance achieved at approximately 10,000 units for most outcomes.
- External Sample Size: The method showed reasonable robustness to external sample size, though very small external samples (<100) increased estimation variance.
- Outcome Prevalence: For rare outcomes, stratified sampling preserving outcome proportions improved performance with smaller sample sizes.
Research Toolkit for Implementation
Essential Methodological Components
Table 4: Research Reagent Solutions for External Performance Estimation
| Component | Function | Implementation Considerations |
|---|---|---|
| Weighting Algorithm | Assigns weights to internal cohort to match external statistics | Optimization constraints prevent negative weights; Convergence criteria must be predefined |
| Feature Selection Framework | Identifies optimal predictors for statistical matching | Should prioritize model-important features; Must balance comprehensiveness and feasibility |
| Performance Metric Calculator | Computes discrimination, calibration, and accuracy metrics | Should implement proper scoring rules; Must account for weighting in calculations |
| Bias Assessment Tool | Evaluates potential selection bias in external statistics | PROBAST tool adaptation recommended for systematic bias assessment [115] |
| Sample Size Planner | Determines minimum internal and external sample requirements | Particularly important for rare outcomes; Incorporates prevalence and effect size estimates |
Integration with Validation Frameworks
The summary statistic-based estimation method should be integrated within comprehensive validation frameworks such as TRIPOD (Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis) [9]. Recent extensions including TRIPOD-AI specifically address artificial intelligence and machine learning prediction models, providing reporting guidelines that enhance methodological rigor and transparency [9].
Additionally, the PROBAST (Prediction model Risk Of Bias Assessment Tool) provides a structured approach for evaluating potential biases in prediction model studies [115]. This tool assesses four key domains: participants, predictors, outcome, and analysis, helping researchers identify methodological weaknesses that could affect validation results [115].
The development of methods that can estimate external model performance using limited summary statistics represents a significant advancement in predictive model validation. These approaches address practical constraints in healthcare data sharing while providing accurate assessment of model transportability. Benchmark studies demonstrate that these methods can estimate external performance with errors substantially smaller than the actual performance differences between internal and external validation [114].
Future research directions include extending these methods to handle time-to-event outcomes, developing approaches for assessing model fairness across populations using summary statistics, and creating standardized protocols for reporting summary characteristics to facilitate broader adoption. As predictive models continue to play an increasingly important role in clinical decision-making, these efficient validation approaches will be essential for ensuring models perform reliably across diverse patient populations and healthcare settings.
Conclusion
The rigorous statistical validation of predictive models is paramount for their successful translation into clinical practice. This synthesis of core intents underscores that a robust validation framework must integrate the assessment of discrimination, calibration, and overall performance, while proactively addressing common challenges like overfitting and data imbalance. Moving forward, the field must embrace more dynamic model updating strategies, standardized reporting guidelines, and decision-analytic frameworks that explicitly evaluate clinical utility. For biomedical research, this evolution is critical to building trustworthy models that can genuinely enhance patient care, optimize drug development, and fulfill the promise of personalized medicine. Future efforts should focus on improving model interpretability, facilitating external validation with limited data, and demonstrating tangible impact on patient outcomes through prospective studies.
References
- 1. There is no such thing as a validated prediction model [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-02779-w]
- 2. Validation of the model - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK305598/]
- 3. Prediction models need appropriate internal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5578404/]
- 4. Predictive Model Validation [https://www.deepchecks.com/glossary/predictive-model-validation/]
- 5. What is Model Validation and Why is it Important? [https://www.geeksforgeeks.org/machine-learning/what-is-model-validation-and-why-is-it-important/]
- 6. Development and Internal-External Validation Models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12267828/]
- 7. Development and Spatial External Validation of a ... [https://www.jmir.org/2025/1/e71257]
- 8. Evaluating predictive performance, validity, and applicability of ... [https://bmcglobalpublichealth.biomedcentral.com/articles/10.1186/s44263-025-00184-4]
- 9. Statistical methods for validation of predictive models [https://www.sciencedirect.com/science/article/abs/pii/S1071358123007213]
- 10. How to Evaluate the Accuracy of Predictive Models [https://businessanalyticsinstitute.com/how-to-evaluate-the-accuracy-of-predictive-models/]
- 11. Discrimination and calibration performances of non-laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11815431/]
- 12. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 13. Reporting of Fairness Metrics in Clinical Risk Prediction ... [https://ojphi.jmir.org/2025/1/e66598]
- 14. Article When accurate prediction models yield harmful self ... [https://www.sciencedirect.com/science/article/pii/S2666389925000777]
- 15. Validation technique could help scientists make more ... [https://news.mit.edu/2025/validation-technique-could-help-scientists-make-more-accurate-forecasts-0207]
- 16. Weighted Brier Score - an Overall Summary Measure for ... [https://arxiv.org/html/2408.01626v2]
- 17. Brier Score: Definition, Examples [https://www.statisticshowto.com/brier-score/]
- 18. Brier score [https://en.wikipedia.org/wiki/Brier_score]
- 19. A Brief on Brier Scores | UVA Library [http://library.virginia.edu/data/articles/a-brief-on-brier-scores]
- 20. Interpreting the concordance statistic of a logistic regression ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-12-82]
- 21. The conservativeness of standard C statistics in ... [https://pubmed.ncbi.nlm.nih.gov/41243705/]
- 22. C-Statistic: Definition, Examples, Weighting and Significance [https://www.statisticshowto.com/c-statistic/]
- 23. A gentle introduction and visual exploration of calibration and ... [https://iclr-blogposts.github.io/2025/blog/calibration/]
- 24. Model Calibration, Explained: A Visual Guide with Code ... [https://towardsdatascience.com/model-calibration-explained-a-visual-guide-with-code-examples-for-beginners-55f368bafe72/]
- 25. How to be prepared for Pharmaceutical Validation in 2025 [https://www.gillsprocess.com/blog-1/2024/12/11/how-to-be-prepared-for-pharmaceutical-validation-in-2025]
- 26. Regulatory Science to 2025: An Analysis of Stakeholder ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7540226/]
- 27. Healthcare Predictive : Transforming Patient Outcomes 2025 [https://www.omdena.com/blog/predictive-healthcare-2025]
- 28. Principles of Clinical Development and Prediction Model Validation [https://pubmed.ncbi.nlm.nih.gov/40314596/]
- 29. : A Practical Approach to... | SpringerLink Clinical Prediction Models [https://link.springer.com/book/10.1007/978-3-030-16399-0]
- 30. A predictive approach to enhance time-series forecasting [https://www.nature.com/articles/s41467-025-63786-4]
- 31. Optimization and performance evaluation of machine ... [https://www.sciencedirect.com/science/article/abs/pii/S0926580525005102]
- 32. Frontiers | Applications and challenges of biomarker-based predictive ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1633487/full]
- 33. Assessing the performance of prediction models: a framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3575184/]
- 34. On the C-statistics for Evaluating Overall Adequacy of Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3079915/]
- 35. Calibration: the Achilles heel of predictive analytics [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-019-1466-7]
- 36. Brier Score: Understanding Model Calibration [https://neptune.ai/blog/brier-score-and-model-calibration]
- 37. On misconceptions about the Brier score in binary ... [https://arxiv.org/html/2504.04906v4]
- 38. Quantifying and Interpreting the Prediction Accuracy of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10660575/]
- 39. what does the “calibration slope” really measure? [https://www.sciencedirect.com/science/article/pii/S0895435619303579]
- 40. Comparison of standard and penalized logistic regression ... [https://www.sciencedirect.com/science/article/pii/S2666273622000286]
- 41. Decision curve analysis: a technical note - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6123195/]
- 42. A simple, step-by-step guide to interpreting decision curve ... [https://diagnprognres.biomedcentral.com/articles/10.1186/s41512-019-0064-7]
- 43. Decision Curve Analysis • dcurves [https://www.danieldsjoberg.com/dcurves/articles/dca.html]
- 44. Decision Curve Analysis - DCA: Homepage [https://mskcc-epi-bio.github.io/decisioncurveanalysis/]
- 45. A Comparison of Decision Curve Analysis with Traditional ... [https://www.fharrell.com/post/dca/]
- 46. Decision Curve Analysis Explained [https://www.medrxiv.org/content/10.1101/2025.08.16.25333820v1]
- 47. This Is How We Should Evaluate Our Survival Models [https://arxiv.org/html/2506.02075v1]
- 48. Evaluating Survival Models — scikit-survival 0.25.0 [https://scikit-survival.readthedocs.io/en/stable/user_guide/evaluating-survival-models.html]
- 49. The Intuition behind Concordance Index - Survival Analysis [https://towardsdatascience.com/the-intuition-behind-concordance-index-survival-analysis-3c961fc11ce8/]
- 50. Comparison of machine learning and deep ... [https://www.sciencedirect.com/science/article/pii/S2949820125000736]
- 51. Interpretable machine learning models to predict survival in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605121/]
- 52. A comparative analysis of parametric survival models and ... [https://www.nature.com/articles/s41598-025-15696-0]
- 53. Net reclassification improvement [https://en.wikipedia.org/wiki/Net_reclassification_improvement]
- 54. Net Reclassification Improvement (NRI) and IDI [https://www.uniqcret.com/post/nri-idi-explained]
- 55. Simpson's Paradox in the Integrated Discrimination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5726308/]
- 56. A Modified Net Reclassification Improvement Statistic - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10079138/]
- 57. The Net Reclassification Index (NRI): a Misleading ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4615606/]
- 58. Evaluating the Incremental Value of New Biomarkers With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3202159/]
- 59. Derivation and Internal Validation of Prediction Models for ... [https://elifesciences.org/reviewed-preprints/98169]
- 60. Net Reclassification Index and Integrated Discrimination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5837334/]
- 61. Evaluation of polygenic risk models using multiple ... [https://www.sciencedirect.com/science/article/pii/S1098360021046256]
- 62. 19 Residual-diagnostics Plots - Explanatory Model Analysis [https://ema.drwhy.ai/residualDiagnostic.html]
- 63. A comparison of residual diagnosis tools for diagnosing ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-020-01055-2]
- 64. Residuals and regression diagnostics: focusing on logistic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4885900/]
- 65. 2.4 Model Diagnostics and Residual Analysis [https://fiveable.me/modern-statistical-prediction-and-machine-learning/unit-2/model-diagnostics-residual-analysis/study-guide/mhd8Xv735HQgYYBi]
- 66. Everything to Know About Residual Analysis [https://www.6sigma.us/six-sigma-in-focus/residual-analysis/]
- 67. Influence Diagnostics in Gamma-Pareto Regression Model With ... [https://doaj.org/article/ee36669902a24e6d8642cd70d94bd5b3]
- 68. How to Fix Overfitting and Underfitting | by Tahir | Oct, 2025 [https://medium.com/@tahirbalarabe2/how-to-fix-overfitting-and-underfitting-4cf8f383ea96]
- 69. Understanding Overfitting: Strategies and Solutions [http://www.lyzr.ai/glossaries/overfitting/]
- 70. When to use regularization vs. cross validation [closed] [https://stats.stackexchange.com/questions/472202/when-to-use-regularization-vs-cross-validation]
- 71. Cross Validation in Machine Learning [https://www.geeksforgeeks.org/machine-learning/cross-validation-machine-learning/]
- 72. Comparative Analysis of Regularization Methods for ... [https://link.springer.com/chapter/10.1007/978-3-031-95365-1_5]
- 73. Comparative Deep Learning Analysis of Regularization ... [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.20944/preprints202511.0501.v1]
- 74. Development and validation of machine learning models ... [https://www.nature.com/articles/s41598-025-06998-4]
- 75. Development and validation of a machine learning model ... [https://www.sciencedirect.com/science/article/abs/pii/S0165032725019974]
- 76. Comparative Analysis of Resampling Techniques for Class ... [https://www.mdpi.com/2227-7390/13/13/2186]
- 77. Resampling approach for imbalanced data classification ... [https://www.sciencedirect.com/science/article/abs/pii/S0020025524014841]
- 78. The harm of class imbalance corrections for risk prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9382395/]
- 79. Examining characteristics of predictive models with ... [https://journalofbigdata.springeropen.com/articles/10.1186/s40537-019-0231-2]
- 80. Performance analysis of cost-sensitive learning methods ... [https://www.sciencedirect.com/science/article/pii/S235291482100174X]
- 81. Evaluation of Cost-Sensitive Learning Models in ... [https://www.mdpi.com/2227-7390/13/3/368]
- 82. Should You Use Imbalanced-Learn in 2025? [https://www.blog.trainindata.com/should-you-use-imbalanced-learn-in-2025/]
- 83. Distinction Between Outliers and High Leverage Observations [https://online.stat.psu.edu/stat462/node/170/]
- 84. Influential Observations, High Leverage Points, and ... [https://projecteuclid.org/journals/statistical-science/volume-1/issue-3/Influential-Observations-High-Leverage-Points-and-Outliers-in-Linear-Regression/10.1214/ss/1177013622.full]
- 85. Outliers, High-Leverage & Influential Points [https://www.savemyexams.com/ap/statistics/college-board/20/revision-notes/exploring-two-variable-data/scatterplots-and-regression/outliers-high-leverage-and-influential-points/]
- 86. 4.4.2. Outlier, Leverage, and Influential Points Unusual ... [https://www.theopeneducator.com/doe/Regression/outlier-leverage-influential-points]
- 87. Exploring Outliers, Leverage, and Influence [https://sabarevictor.medium.com/exploring-outliers-leverage-and-influence-33879dbbba9a]
- 88. Precise meaning of and comparison between influential point ... [https://stats.stackexchange.com/questions/65912/precise-meaning-of-and-comparison-between-influential-point-high-leverage-point]
- 89. Missing Data & Outliers in Biocomputational Analysis [https://sapient.bio/resources/biocomputational-analysis-addressing-outliers/]
- 90. Multiple Regression Residual Analysis and Outliers [https://www.jmp.com/en/statistics-knowledge-portal/what-is-multiple-regression/mlr-residual-analysis-and-outliers]
- 91. A machine learning regression model for the screening ... [https://link.springer.com/article/10.1007/s13721-021-00326-2]
- 92. Comparison of dynamic updating strategies for clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8647501/]
- 93. towards continual monitoring and updating of AI algorithms ... [https://www.nature.com/articles/s41746-022-00611-y]
- 94. Implementation and Updating of Clinical Prediction Models [https://www.sciencedirect.com/science/article/pii/S2949761225000355]
- 95. Machine Learning With Statistical Imputation for Predicting ... [https://hdsr.mitpress.mit.edu/pub/ct67j043]
- 96. Comparison of the effects of imputation methods for missing ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02173-x]
- 97. Comparative performances of machine learning algorithms ... [https://www.nature.com/articles/s41598-023-39738-7]
- 98. A Review of Feature Selection Methods for Machine Learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9580915/]
- 99. External validation and comparison of clinical prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482746/]
- 100. Benchmarking the Confidence of Large Language Models in ... [https://medinform.jmir.org/2025/1/e66917]
- 101. The DRAGON benchmark for clinical NLP - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12084576/]
- 102. Chapter 10 Model Validation | Introduction to Statistical ... [https://tjfisher19.github.io/introStatModeling/model-validation.html]
- 103. The Actual Difference Between Statistics and Machine ... [https://medium.com/data-science/the-actual-difference-between-statistics-and-machine-learning-64b49f07ea3]
- 104. A comparative analysis of machine learning and statistical ... [https://www.sciencedirect.com/science/article/abs/pii/S0360132324001100]
- 105. Machine Learning vs. Statistics: What's the Best Approach? [https://und.edu/blog/machine-learning-vs-statistics.html]
- 106. Statistics versus machine learning | Nature Methods [https://www.nature.com/articles/nmeth.4642]
- 107. A Comparative Study of Traditional Statistical Methods and ... [https://etamaths.com/index.php/ijaa/article/view/3700]
- 108. Assessing the accuracy of survival machine learning and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587511/]
- 109. Accuracy Comparison of Machine Learning Algorithms on ... [https://www.mdpi.com/2227-7390/13/7/1176]
- 110. Clinical prediction models using machine learning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506039/]
- 111. Top 9 decision-making tools for better organizational ... [https://www.1000minds.com/articles/decision-making-tools]
- 112. Real-World Data and Causal Machine Learning to Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579681/]
- 113. Artificial Intelligence for Drug Development [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 114. Extensive benchmarking of a method that estimates ... [https://www.nature.com/articles/s41746-024-01414-z]
- 115. Evaluating predictive performance, validity, and applicability of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288308/]